Abstract
We report the cases of two patients diagnosed with Morgagni hernia who presented with nonspecific abdominal symptoms. Both underwent laparoscopic surgery that used a dual-sided mesh, polyvinylidene fluoride (PVDF; Dynamesh IPOM®). The procedures were successful and both patients were discharged with no complications. There was no recurrence in 18 months of follow up.Herein is the report of these cases and a literature review.
Keywords: Morgagni hernia, Laparoscopic repair, Dual-sided mesh
INTRODUCTION
Impaired fusion or muscularization of the pleuroperitoneal membrane located on the anterior side of the body will result in a triangular defect between the sternum and right-side ribs. This defect is called the foramen of Morgagni.
Omental or visceral herniation through the foramen of Morgagni is more common in females and obese individuals1 , 2 The prevalence of a Morgagni hernia is rare, comprising only 3%-4% of all diaphragmatic hernias.3
In symptomatic cases, chronic gastrointestinal (GI) symptoms occur such as pain and constipation due to intermittent partial obstruction of the colon. Complications such as intermittent gastric volvulus, small intestine obstruction, incarceration and strangulation of the hernia are rare.
Cardiopulmonary symptoms such as dyspnea and palpitations are infrequent and occur less frequently than GI symptoms.1
One-third of Morgagni hernia cases are asymptomatic and may be incidentally diagnosed during an evaluation for other diseases.1
Diagnosis of a Morgagni hernia is made on the basis of clinical and imaging findings.
Laparoscopic surgical approach is based on the intraperitoneal positioning of the mesh without the necessity for abdominal wall separation4 Until now, expanded polytetrafluoroethylene (e-PTFE)-derived meshes, which have been used for laparoscopic repair of hernias are the most common meshes described in the literature.5
Dynamesh IPOM® is a new mesh structure with large pores made of polyvinylidene fluoride (PVDF), which contains a small amount of polypropylene located on the parietal side. PVDF Dynamesh IPOM® is an inert mesh material which does not adhere to abdominal structures.6 In this report, we have discussed two cases of Morgagni hernia that were treated laparoscopically using a PVDF-based dual-sided mesh.
CASE PRESENTATION
A 75-year-old woman with vague epigastric pain from one year prior was admitted to the Emam Khomeyni hospital. Her epigastric pain worsened with large meals and was associated with nausea, vomiting, and constipation. Symptoms were exacerbated since one month prior to admission. No sweating, palpitation, dyspnea, anorexia, early satiety, weight loss, dysphagia, and odynophagia were detected. The patient had a history of hypertension and hyperlipidemia for which she was under treatment with antihypertensive drugs and lipid lowering agents. A chest X-ray (CXR) revealed the presence of a hypodense mass in the proximity of the right lung base. Consequently, thoracic CT scan was performed. After complete clinical and imaging evaluations, the patient was sent for surgical repair of the Morgagni hernia. Preoperative risk assessments that included an ECG, echocardiography, cardiologist consult, routine laboratory analyses, ABG, PFT, and anesthesiologist consult were performed. She had an Left Ventricular Ejection Fraction(LVEF) of 55% and mild Mitral Regurgitation(MR).
The second patient was an 80-year-old woman who suffered from dyspnea at rest and orthopnea since two weeks before admission that was associated with vomiting after heavy meals, generalized vague abdominal pain, dysphagia, regurgitation, epigastric fullness, constipation, sweating, and cough. Clinical and diagnostic imaging that included CXR and a spiral thoraco-abdominal CT scan was indicative of a Morgagni hernia.
For the laparoscopies, both patients were placed in the supine position with their arms at their sides. A Foley catheter was inserted under general anesthesia. CO2 insufflations were performed by Veress needle. One, 10-mm trocar port was inserted above the umbilicus and a camera (30o angulated optic) was introduced into the abdominal cavity through this port. After primary evaluation in both patients, the Morgagni hernia was located and a segment of transverse colon and omentum was seen in the hernia sac. After insertion of two 10-mm and 5-mm trocar ports from the right and left upper abdominal quadrants (RUQ, LUQ), respectively, the colon and omentum were reduced back into the abdominal cavity. Subsequently, patients’ positions were changed to perform a reverse Trendelenburg; the anesthesiologist manually inflated the lungs to ensure positive pressure in order to facilitate the reduction of the sac contents. The hernia sac was excised( Figure 1) and the falciform ligament was divided by LigaSure. The size of the defect was 6 x 7 cm in the first patient and 5 x 6 cm in the second patient.
Fig. 1.
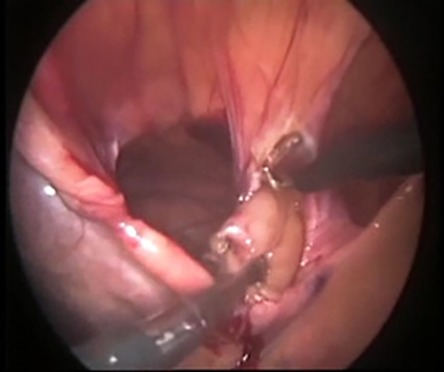
Excision of hernia sac
Dual-sided mesh (15 x 20 cm) was inserted into the abdominal cavity through the 10 mm port in the LUQ. Mesh was expanded over the defect( Figure 2 ) and fixed to the anterior abdominal wall and edge of the diaphragmatic defect in the posterior part with spiral tacks (Protack®, Covidien, Mansfield, MA, USA) ( Figure 3 ).
Fig. 2.
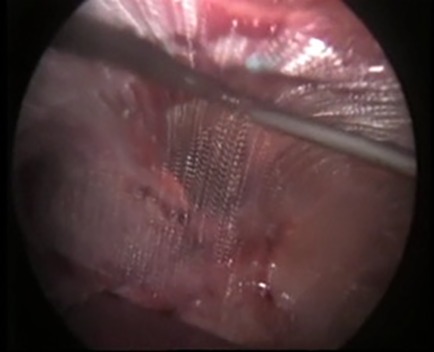
Expansion of Dual-sided mesh over the defec
Fig. 3.
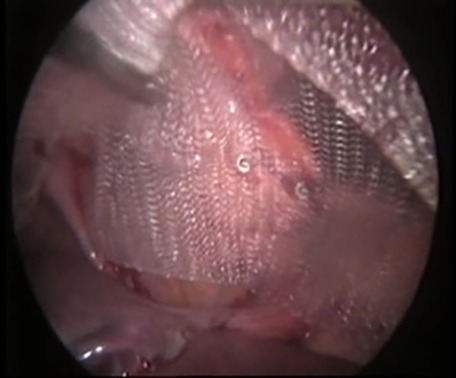
Tacking for fixation of mesh
Application of spiral tacks at the diaphragm carries the risk of life-threatening complications such as cardiac tamponade.7
After removal of the trocars under direct visualization, the fascia at the 10 mm trocar sites were closed and incisions repaired. Patients were admitted to the SICU for the first postoperative day and discharged 72 hours after surgery. Both were discharged ambulatory and were on soft diets.
There was no complication or recurrence during 18 months of follow up for either patient.
DISCUSSION
Morgagni, an Italian anatomist, in 1761 described a hernia that was located through a defect in the diaphragm just behind the sternum.8 Morgagni hernia is a rare type of diaphragmatic hernia in which herniation of the intra-abdominal viscerae into the thorax through the foramen of Morgagni (parasternal hiatus) leads to the formation of a well-defined mass in the right costophrenic angle.2
Morgagni hernia should be treated, even when asymptomatic. This hernia may cause complications such as incarceration, strangulation and intestinal obstruction. Consequently, all patients should undergo surgical repair of the hernia, which is the ultimate.9 Exceptions to surgery include the elderly and asymptomatic patients who do not tolerate open or laparoscopic repair due to severe underlying diseases.
Different surgical approaches that include transabdominal, transthoracic and laparoscopic (minimal invasive surgery) procedures have been described.
An open transabdominal approach (laparotomy by upper midline or paramedian or subcostal incision) is the method of choice in patients with obstruction, incarceration, strangulation or perforation. Both sides can be evaluated by a midline incision.9 The transthoracic approach provides an excellent view for repair of the hernia. Although repair is simple through this procedure, however evaluation of the other side is not possible.
Laparoscopic repair is a safe, effective procedure 3 and has been mentioned as the gold standard and the initial step for repair of a Morgagni hernia.9
Excellent bilateral view, less tissue damage, a short hospital stay and rapid return to normal life are the stated benefits of laparoscopic repair for Morgagni hernia.10 Primary repair is recommended with tension-free suturing using 0-gauge nonabsorbable surgical fiber for smaller defects (<3 cm) and a prosthesis for larger defects.9
Most surgeons recommend the use of a prosthesis to repair a hernia defect, even in cases of small hernias. Polypropylene mesh, expanded polytetrafluoroethylene (e-PTFE), hydrophilic resorbable film, dual-sided e-PTFE, and new double-layer meshes are the typical prostheses that have been used.11 As the risk of adhesion to the prosthesis is less for the dual-sided mesh, it is the prosthesis of choice.12
Most patients described in the literature have been treated with e-PTFE-derived meshes.5 The visceral side is as smooth as possible and the parietal side is rough or covered with polypropylene to induce strong adhesions to the diaphragm and abdominal wall. Using meshes made by polypropylene or polyester covered with an anti-adhesion barrier on the visceral side represents another approach.6 , 13
PVDF is an inert material that has long been used as suture material. Its long-term stability is better than that of polypropylene meshes.6, 10 It has been shown that PVDF induces less inflammatory process at the cellular level and lower amounts of fibrotic tissue compared to e-PTFE and covered polypropylene meshes.4, 6, 10 Its anti-adhesive properties seem to be comparable to covered polypropylene.
Importantly, meshes have a tendency to shrink. Shrinkage has been found to be most pronounced in e-PTFE-derived meshes, which lost about 50% of their original size. PVDF-derived meshes lost only 19% of their original size, which was in the same order of magnitude or slightly better than covered polypropylene meshes.4 , 6, 14 Resistance against infection is another important property of PVDF-based meshes.5, 6 Consequently, experimental data have clearly supported the successful use of PVDF-based meshes for abdominal hernia repair.6
Morgagni hernia should be considered in the differential diagnosis of patients with chronic GI symptoms such as vague abdominal pain or constipation, or in cases with cardiopulmonary symptoms (dyspnea or palpitations). Surgical repair is advised for all cases of Morgagni hernia. For this type of hernia, laparoscopy is considered to be the procedure of choice.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as:
Godazandeh Gh, Mortazian M. Laparoscopic Repair of Morgagni Hernia using Polyvinylidene Fluoride (PVDF) Mesh. Middle East J Dig Dis 2012;4:232-5.
References
- 1.Berardi RS, Tenquist J, Sauter D. An update on the surgical aspects of Morgagni hernia. Surg Rounds. 1997;2:370–6. [Google Scholar]
- 2.Loong TP, Kocher HM. Clinical presentation and operative repair of hernia of Morgagni. Postgrad Med J. 2005;81:41–4. doi: 10.1136/pgmj.2004.022996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puglisi F, Capuano P, Iambrenghi OC, Armenise N, Carlucci F, MemeoM MemeoM. et al. Laparoscopic repair of Morgagni hernia in an adult: use of a porcine small intestine submucosa biocompatible prosthesis. ChirItal. 2009;61:351–6. [PubMed] [Google Scholar]
- 4.Nguyen T, Eubanks PJ, Nguyen D, Klein SR. The laparoscopic approach for repair of Morgagni hernias. JSLS. 1998;2:85–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Carlson MA, Frantzides CT, Shostrom VK, Laguna LE. Minimally invasive ventral herniorrhaphy: an analysis of 6,266 published cases. Hernia. 2008;12:9–22. doi: 10.1007/s10029-007-0286-4. [DOI] [PubMed] [Google Scholar]
- 6.Berger D, Bientzle M. Polyvinylidene fluoride: a suitable mesh material for laparoscopic incisional and parastomal hernia repair! A prospective, observational study with 344 patients. Hernia. 2009;13:167–72. doi: 10.1007/s10029-008-0435-4. [DOI] [PubMed] [Google Scholar]
- 7.Adhesion formation of a polyvinylidenfluoride/polypropylene mesh for intra-abdominal placement in a rodent animal model. Surg Endosc. 2009;23:327–33. doi: 10.1007/s00464-008-9923-y. [DOI] [PubMed] [Google Scholar]
- 8. Morgagni GB. In: Millar A, Cardell T, eds. Seats and Causes of Diseases. Vol. 3. London:1769:205.
- 9.Pironi D, Palazzini G, Arcieri S, Candioli S, Manigrasso A, PanareseA PanareseA. et al. Laparoscopic diagnosis and treatment of diaphragmatic Morgagni herniaCase report and review of the literature. Ann Ital Chir. 2008;79:29–36. [PubMed] [Google Scholar]
- 10.Klinge U, Klosterhalfen B, Ottinger AP, Junge K, Schumpelick V. PVDF as a new polymer for the construction of surgical meshes. Biomaterials. 2002;23:3487–93. doi: 10.1016/s0142-9612(02)00070-4. [DOI] [PubMed] [Google Scholar]
- 11.Marín-Blazquez AA, Candel MF, Parra PA, Méndez M, Ródenas J, Rojas MJ. et al. Morgagni hernia: repair with a mesh using laparoscopic surgery. Hernia. 2004;8:70–2. doi: 10.1007/s10029-003-0145-x. [DOI] [PubMed] [Google Scholar]
- 12.Junge K, Binnebösel M, Rosch R, Jansen M, Kämmer D, Otto J. et al. Adhesion formation of a polyvinylidenfluoride/polypropylene mesh for intra-abdominal placement in a rodent animal model. Surg Endosc. 2009;23:327–33. doi: 10.1007/s00464-008-9923-y. [DOI] [PubMed] [Google Scholar]
- 13.Chelala E, Thoma M, Tatete B, Lemye AC, Dessily M, Alle JL. The suturing concept for laparoscopic mesh fixation in ventral and incisional hernia repair: Mid-term analysis of 400 cases. Surg Endosc. 2007;21:391–5. doi: 10.1007/s00464-006-9014-x. [DOI] [PubMed] [Google Scholar]
- 14.Conze J, Junge K, Weiss C, Anurov M, Oettinger A, KlingeU KlingeU. et al. New polymer for intra-abdominal meshes--PVDF copolymer. J Biomed Mater Res B Appl Biomater. 2008;87:321–8. doi: 10.1002/jbm.b.31106. [DOI] [PubMed] [Google Scholar]


