Abstract
BACKGROUND
Ulcerative colitis (UC), as the prototype of inflammatory bowel disease of the large bowel, is increasing in Iran and other developing countries. There are few studies that discuss the properties of this disease Iran. The result of this review may provide a general consensus about the epidemiological features of UC in Iran.
METHODS
This was a qualitative, systematic review that investigated the incidence, prevalence, and demographic properties of UC in Iran. We evaluated all published studies in the PubMed database, IranMedex, Magiran, and Scientific Information Database (SID) that pertained to the epidemiology and demographic features of UC in Iran from January 1987 to January 2012. After searching with defined keywords and implementing the inclusion and exclusion criteria, 11 case series and 2 case-control studies fulfilled the criteria for inclusion.
RESULTS
The estimated prevalence of UC is 15 per 105 persons, and the reported incidences were 3.04 and 3.25 per 105 persons in two Iranian provinces. The disease was more commonly observed in women and people in their fourth decade of life. Cigarette smoking conferred protection and familial association seemed to be similar to developed countries. UC did not appear to be more common among the higher socioeconomic class. In addition the proximal colon and rectum were less commonly involved.
CONCLUSION
Although the data is limited, the prevalence and incidence of UC in Iran shows an increasing pattern similar to other countries in the region. There is no clear association with socioeconomic status. Milder forms of the disease are common in Iran. A comprehensive nationwide data bank is needed for a better definition of the disease characteristics.
Keywords: Ulcerative colitis, Prevalence, Incidence, Demography, Iran
INTRODUCTION
Ulcerative colitis (UC) is a chronic immune-mediated inflammatory disorder of the large bowel that usually affects young people, greatly impacting their health and activity levels.1,2 The pathogenesis of this disease is unknown, however inappropriate interactions between genetic, immunological, and environmental factors have an important effect. Affected patients may present with chronic blood and passage of mucous in the stool in mild forms of the disease to severe bloody diarrhea, abdominal distension, fever, weight loss, and toxic megacolon in severe cases.3 Unpredictable remissions and exacerbations are typical and extraintestinal involvement is common in affected patients. UC is more common in developed countries, especially in northern Europe and America,4 traditionally it has rarely been seen in developing countries. A gradual increase in the incidence and prevalence of this disease in developing countries has coincided with an improvement in health, sanitation, and a more Western life style in nations such as India,5 Japan,6-8 and South Korea.9 The Iranian people have rapidly improved their health status over the previous three decades, which coincides with reports of an increasing burden of this disease. However, due to wide geographical and ethnic variation, the pattern of epidemiological characteristics and risk factors are not clearly defined. The purpose of this study is to evaluate and interpret all published evidence that relate to the epidemiological, clinical presentation, and risk factors of UC in Iran during the last 25 years.
MATERIALS AND METHODS
This research was a qualitative systematic review on the epidemiology and risk factors of UC in Iran. All English and Persian language articles published from January 1987 to January 2012 in PubMed, IranMedex, Magiran, and Scientific Information Database (SID) were surveyed through a comprehensive search. UC studies were determined using the following terms:
(“Ulcerative colitis”[Text Word]) OR (“Colitis, Ulcerative” [Text Word]) OR (“Inflammatory Bowel Diseases”[Text Word]) OR (“Mortality”[Text Word]) OR (ʺ incidenceʺ [Text Word]) OR (“Age of onset”[Text Word]) OR (ʺPrevalenceʺ [Text word]) OR (“Mortality risk ratio”[Text word]) OR(“Mortality relative risk”[text word] OR (ʺrecurrenceʺ[Text Word]) OR (“Mortality RR” [Text Word]) OR(“Remission, Spontaneous”[Text Word]) OR (“natural history”[Text word]) OR (“Mortality”[MesH]) OR (“Incidence”[MesH]) OR (“Prevalence”[MesH]) OR (“Recurrence”[MesH]) OR(“Remission, Spontaneous”[MesH]) OR (“Colitis, Ulcerative”[MesH]) OR (“Inflammatory Bowel Diseases”[MesH]) OR (“Natural History”[MesH]) OR (“ disease duration”[Text Word]) OR (“Incidence”[MesH]) OR (ʺincidenceʺ [Text Word]) OR (ʺPrevalenceʺ [Text Word]) OR (“Prevalence”[MesH]) (ʺduration ʺ [Text Word]) AND (ʺIranʺ [Text Word]) in PubMed. The search study was limited to adult humans. For Persian language articles, the search terms included Persian translations of UC and epidemiology as suggested by the Persian Language and Culture Academy.
Inclusion criteria
We collected cross-sectional and case series studies in which the UC diagnosis was verified on the basis of clinical, endoscopic, radiological, and histological criteria by using the Lennard-Jones method.10 Two reviewers reviewed the articles for eligibility according to the above criteria. In cases of disagreement between the reviewers, inclusion of the article in question was resolved by consensus.
Data extraction
All data extracted by the two reviewers were entered on to a spreadsheet (Microsoft Excel XP Professional Edition; Microsoft Corp., Redmond, Washington). Discrepancies were resolved as previously mentioned.
Quality assessment
After data base searches, the quality of the studies was evaluated by a scoring system created according to predefined criteria (Table 1). This scoring system consisted of four variables: 1) clearance in general objects of the study, 2) sampling, 3) relevant scaling, and 4) data analysis. Two reviewers independently assessed the articles according to this system. If an article had more than 6 out of 12 points, it was entered into the study and the full text of the article was evaluated. We chose articles that evaluated the epidemiology, demographic character, and risk factors of UC with appropriate methodology.
Table 1. Assessment for article quality.
| Reviewer : 1 □ 2 □ | Articles | ||||
| 1 st step: Decision after reading the title and abstract. | 1 | 2 | 3 | 4 | 5 |
|
Reject □ Accept □ |
Reject □ Accept □ |
Reject □ Accept □ |
Reject □ Accept □ |
Reject □ Accept □ |
|
| 2 nd Step: Complete the following when the entire article is read. | |||||
| Research question | |||||
| Has the research aim been explained sufficiently and clearly? | |||||
| Has the population study been clearly defined? | |||||
| Have the outcomes been considered clearly? | |||||
| Are the time and location boundaries explained? | |||||
| Sampling | |||||
| Has the sample size been appropriately defined? | |||||
| Was random sampling performed? | |||||
| Do selected patient characteristics correspond to the defined population? | |||||
| Measurements | |||||
| Were valid and reliable tools used? | |||||
| Were identical tools used? | |||||
| Did a trained interviewer gather data? | |||||
| Analysis | |||||
| Was subgroup analysis performed? | |||||
| Was there a suitable analysis method? | |||||
| Total score | |||||
| Final decision |
Reject □ Accept □ |
Reject □ Accept □ |
Reject □ Accept □ |
Reject □ Accept □ |
Reject □ Accept □ |
If an article has a considered character, it will be assigned 1 point.
If an article has total score of more than 6, it will be accepted and entered in the next step.
RESULTS
The search identified 407 potentially relevant citations (Figure 1, Table 2). From these, we identified 11 case series studies that comprised 1882 individuals diagnosed with UC and 2 case-control studies. There was 80% agreement between the two reviewers (A.A.S. and M.S.F.) in assessing study eligibility. Fani,11 in a study conducted in Arak, Iran estimated the incidence of UC to be 3.04 per 105 individuals and Masoodi et al.12 in Hormozgan Province, Iran estimated the incidence of UC to be 3.25 per 105 individuals. The prevalence of UC in Arak in 2000 was estimated by Fani as 15.5 in 105.
Fig. 1.
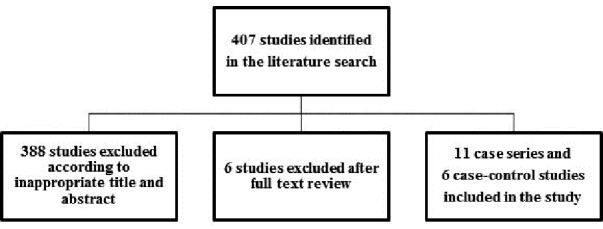
Flow diagram for assessing studies identified in the systematic review.
Table 2. Number of related articles in various indexes.
| Articles |
PubMed
(n) |
Iran Medex
(n) |
Magiran
(n) |
SID*
(n) |
| Primary search | 152 | 97 | 86 | 72 |
| Review of title and abstract | 13 | 13 | 5 | 3 |
| Review of full text | 5 | 7 | 4 | 2 |
There were overlaps between data base sources
*SID: Scientific Information Database
Patients’ demographic characteristics are shown in Table 3. There were 1039 female patients (F/M: 1.23). Patients’ mean age at the time of diagnosis was approximately 34 years. In all studies, with the exception of one study, patients’ mean ages were in the fourth decade of life One of the studies revealed a second peak.
Table 3. Demographic characteristics and risk factors of UC in 11 Iranian studies.
|
Case
(n) |
F/M ratio | Age/years (SD year) | Smoking (%) | Urban (%) |
Higher
education |
Familial (%) | |
| Dariani 15 | 200 | 1.22 | 27.4 (10.4) | 11 | NA† | 80 | 28 |
| Aghazade 16 | 401 | 1.25 | 31.9 (11.8) | 15.5 | 95.9 | 66 | 13.8 |
| Fani 11 | 97 | 1.1 | 39.3 (15.4) | NA | NA | NA | NA |
| Zahedi 17 | 85 | 1.25 | 33.3 (13.2) | 5.9 | NA | NA | NA |
| Keshavarz 18 | 85 | 0.8 | 34.1 (16.0) | NA | NA | NA | NA |
| Fakheri 19 | 265 | 1.15 |
34.5 (14) |
2.3 | 77.6 | 25.3 | 3.4 |
| Vahedi 20 | 293 | 1.4 |
37.2 (13.7) |
13.3 | 90 | 46.4 | 9.6 |
| Masjedi 21 | 166 | 1.3 | 38.6 (17.4) | 13 | NA | NA | 9 |
| Yazdanbod 22 | 105 | 1.38 | 33.5 (13.1) | 10.4 | 83.8 | NA | NA |
| Semnani 23 | 104 | 1.2 | 37.8 (15.1) | 15 | 34.6 | 83.3 | NA |
| Masoodi 12 | 79 | 1.25 |
32.8 (16) |
NA | NA | 12.4 | NA |
†Not available
Smoking was common in 2.3% to 15.5% of patients in seven studies. In the case-control studies, there was an inverse relation between smoking and the presence of UC (p ≤ 0.002, OR: 0.31921,13 and p<0.0001, OR: 0.214); cessation of smoking was accompanied by appearance of disease.15 In addition, the extension of UC wasn’t affected by cigarette smoking.13
City dwellers, which might have a higher socioeconomic status compared with villagers, comprised 34.5%-94% of UC patients. Another indicator of higher socioeconomic status was higher education level which was considered in five studies and varied from 12.4%-80% of the studied populations (Table 3).
The duration of symptoms at the time of diagnosis was assessed in nine studies with a mean of 8-13.9 months and appeared to have decreased in recently published articles (Table 4). Disease extension was assessed in all studies. In the most common forms, UC seemed to be limited to the left side of the colon (Table 4). Proctitis was the second most common form of UC. In the least common form, UC extended beyond the splenic flexure.
Table 4. Colonic extension and duration of symptoms in Iranian UC cases.
| Proctitis (%) | Left- sided colitis (%) |
Extensive colitis
(%) |
Duration (months) | |
| Dariani15 | 32 | 52 | 16 | 11.9 |
| Aghazade16 | 51.9 | 30 | 18.1 | 13.9 |
| Fani11 | 26.8 | 47.5 | 25.7 | *NA |
| Zahedi17 | 8.3 | 51.5 | 39.8 | 8.1 |
| Keshavarz18 | 23.5 | 57 | 8.23 | NA |
| Fakheri19 | 36.2 | 48.3 | 15.5 | 9.74 |
| Vahedi20 | 51 | 32 | 17 | 8 |
| Masjedi21 | 20.4 | 60 | 17.4 | 12 |
| Yazdanbod22 | 36.2 | 55 | 3.8 | 9 |
| Semnani23 | 32 | 52 | 16 | 11.9 |
| Masoodi12 | 51.9 | 30 | 18.1 | 13.9 |
*NA: Not available
Familial propensity to UC was evaluated in five studies and had an intense discrepancy that ranged from 3.4%-28%. Overall, approximately 10%-15% represented familial aggregation in other studies (Table 4). Four studies evaluated the consumption of oral contraceptive pills (OCP), which comprised approximately 6.5%-32% of UC cases (Table 5). These studies failed to show any relation between the duration of contraceptive use on the extension of the colonic involvement.
Table 5. Risk factors for UC in Iranian studies.
*Not available
OCP: Oral contraceptive pill
Over 83% of patients in three studies were breast fed during infancy, but the duration of breast feeding and the use of formula milk or whole milk in non-breast fed individuals was not determined (Table 5). Case control studies also revealed that breast-feeding did not prevent the development of UC.
DISCUSSION
The first report of inflammatory bowel disease (IBD) from Iran presented UC as a rare disorder.24 An estimation of the incidence and prevalence of UC in Iran has limitations. First, there is no national data bank for registration of all patients. Second, there are only a few studies that evaluate the prevalence or incidence of this disease. It seems that the absence of systematic registration and the limited access to medical care and diagnostic tools have a significant role in the inaccuracy of the present epidemiological data.
There were two reports on UC incidence in Iran, one by Fani conducted in Arak (Central Iran, in a cold region)11 and the other conducted in Hormozgan Province (Southern Iran, in a warm region) by Masoodi et al.12.Fani reported an incidence of 3.04 out of 105 individuals and Masoodi et al. reported an incidence of 3.25 out of 105 individuals. However, this might be an underestimation of the incidence. Due to the low case fatality and mortality rate for UC, the estimated prevalence in the Fani study has increased in recent years. These data are similar to the reports on the incidence of UC in neighboring Middle Eastern countries, such as Turkey (4.4 in 105) 25 and Kuwait (2.8 in 1005).26
Sood et al.5 in a population based study from Punjab, India have reported the highest incidence (6.02 in 105) for UC in Asia. This is much higher than both Japan6 and Korea.9 Industrialization, which is discussed as a coincident factor, began in Japan, South Korea and Iran prior to its onset in India. These differences should be evaluated more precisely before reaching any definite conclusion, but rapidity and the time of industrialization start-up which differs in these countries may be a cause for the discrepancies.27 Genetic background in association with environmental changes (dietary, psychosocial, and immunological) in the Indian immigrant community in the UK and Canada increased the incidence of UC more than residents India.28 It seemed that the absence of systematic national registration and limited access to medical care and diagnostic tools in some areas, had a significant role in the inaccuracy of epidemiological data from Iran and India.
There were several differences in the clinical characteristics of ulcerative colitis compared to the western population. There was an overall female predominance (F/M = 1.23:1), that is different from westeren population,which had equal or slightly female predominance(Table 3).4,29 This finding is close to the M/F ratio (0.78) in a pooled analysis of UC in Iran by Derakhshan et al.30 Female predominance has also been observed in other Middle Eastern countries and in some parts of the Pacific as well.31 This figure is not entirely related to earlier referrals to physicians or more disturbing symptoms in women; it may be related to ethnic and other environmental factors. In Iran, 6.55-32% of females with UC were oral contraceptive users, that isn’t an acceptable description for this finding. In spite of that Turkey,25 Saudi Arabia,32 and India5 have a male predominance of UC. This figure is not entirely related to earlier referrals to physicians or more disturbing symptoms in women; it may be related to ethnic and other environmental factors. In Iran, 6.55-32% of females with UC were oral contraceptive users, that isn’t an acceptable description for this finding.
The mean age of the patients at first presentation is approximately 34 years. However, the mean age of patients at time of diagnosis in Western countries is in the third decade of life, with another peak reported in the fifth to seventh decades of life, which has not been reported in published data from Iran. This has also been observed in the Indian subcontinents. A second peak has been reported in the Turkish population,25 as seen with Western countries.
Cigarette smoking is a known protective factor in UC and observed in 2.3% to 15.5% of patients,15-17,19-23, Case control studies have shown this inverse relation13,14and cessation of cigarette smoking has induced UC. These studies have failed to show that extension of UC can be affected by smoking.
The family history of UC was seen in a diverse range (3.4% to 28%) of affected patients.16,19-21 This difference might be due to inappropriate case selection in these studies. Overall familial association was seen in over 10% of patients, which approximated the previously pooled analysis by Darakhshan et al.30 and was similar to Western countries. Familial association was noted in about 2.2% of UC subjects in Sri Lanka,31 but this issue was observed in about 10%-20% of Saudi Arabian subjects.32 Considering the interfamily marriage in our country, as with Saudi Arabia and particularly in some ethnic areas, a familial association might be increased.
There was more UC among the higher socioeconomic classes in Europe and the US.29 In Iran, the higher socioeconomic status might be defined by higher education and residence in urban areas. Higher education varied in Iranian UC subjects, from 12.4%-83% (Table 3). This variation might be explained by differences in education levels where the studies were performed. A case control study did not report that more educated individuals were likely to have UC.13
Another index, urban residence, varied from 34.6% to 95.9% in Iranian studies (Table 3). These differences in part, might be related to the study population and availability of medical facility in cities. In addition, a case-control study did not show any relation to birthplace (villages or cities) and presence of UC.13
Several studies did not show an inverse association between UC and breast feeding, but increased episodes of diarrhea in infancy, which were more frequent in non-breast feed infants seemed to be associated with UC. More than 83% of UC patients were breast fed as infants in three of these studies (Table 5). There was no report regarding the duration of breast feeding in breast fed infants and type of formula in non-breast fed infants. Because the proportion of nursing mothers in the native population has not been clearly defined, a more appropriate conclusion regarding breast milk consumption could not be substantiated. Rahimi et al. have revealed that breast milk could not prevent subsequent UC.13 Proximal involvement of the colon, such as cecum and transverse colon, have been reported in 3.4%-25% of studies (Tables 4), which might denote prediction of a less severe course for UC among Iranian patients. Fulminant disease is mentioned in one study and was seen in 0.37%,19 which might be an indicator of lower frequency of severe disease. The interval between symptom onset until diagnosis of UC was greater than eight months, but appears to have decreased in more recent studies (Table 3). This earlier diagnosis might be related to increased awareness of people and physicians, improved diagnostic facilities and more access to gastroenterologists.
There are few well-designed reports regarding epidemiological data of UC in Iran. The available data shows the incidence of UC between 3.04 and 3.25 per 105 individuals, which is in the range of other Middle East countries. There is a trend for increasing occurrence of UC, as with other developing countries. The F/M ratio is 1.23 and most patients present in the fourth decade of life. Although ex-smokers are prone to disease presentation, the extent of disease is not affected by cigarette smoking. Most patients have a mild form of UC and left-sided colitis. We propose the establishment of a nationwide comprehensive data bank for to more aptly define UC disease characteristics.
ACKNOWLEDGMENT
The authors thank Professor Reza Malekzadeh for his scientific support. The article is supported by Research institute for Infectious Disease of Digestive System (RIDD) in Ahvaz Jundishapour University of Medical Science (AJUMS) and Digestive Disease Research Center (DDRC) in Tehran University of Medical Science (TUMS).
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as:
Shayesteh AA, Saberifirozi M, Abedian S, Sebghatolahi V. Epidemiological, Demographic, and Colonic Extension of Ulcerative Colitis in Iran: A Systematic Review. Middle East J Dig Dis 2013;5:29-36.
References
- 1.Hoivik ML, Moum B, Solberg IC, Cvancarova M, Hoie O, Vatn MH. et al. Health-related quality of life in patients with ulcerative colitis after a 10-year disease course: Results from the IBSEN study. Inflamm Bowel Dis. 2011;14:250–7. doi: 10.1002/ibd.21863. [DOI] [PubMed] [Google Scholar]
- 2.Graff LA, Vincent N, Walker JR, Clara I, Carr R, Ediger J. et al. A population-based study of fatigue and sleep difficulties in inflammatory bowel disease. Inflamm Bowel Dis. 2012;17:1882–9. doi: 10.1002/ibd.21580. [DOI] [PubMed] [Google Scholar]
- 3.Rao SS, Holdsworth CD, Read NW. Symptoms and stool patterns in patients with ulcerative colitis. Gut. 1988;29:342. doi: 10.1136/gut.29.3.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–17. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 5.Sood A, Midha V, Sood N, Bhatia A S, Avasthi G. Prevalence of ulcerative colitis in Punjab, North India. Gut. 2003;52:1587–90. doi: 10.1136/gut.52.11.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morita N, Toki S, Hirohashi T, Minoda T, Ogawa K, Kono S. et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995;30:1–4. [PubMed] [Google Scholar]
- 7.Yoshida Y, Murata Y. Inflammatory bowel disease in Japan: studies of epidemiology and etiopathogenesis. Med Clin North Am. 1990;74:67–90. doi: 10.1016/s0025-7125(16)30587-9. [DOI] [PubMed] [Google Scholar]
- 8.Higashi A, Watanabe Y, Ozasa K, Hayashi K, Aoike A, Kawai K. Prevalence and mortality of ulcerative colitis and Crohn’s disease in Japan. Gastroenterol Jpn. 1988;23:521–6. doi: 10.1007/BF02779483. [DOI] [PubMed] [Google Scholar]
- 9.Yang SK, Hong WS, Min YI, Kim HY, Yoo JY, Rhee PL. et al. Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong District, Seoul,Korea, 1986-97. J gastroenterol Hepatol. 2000;15:1037–42. doi: 10.1046/j.1440-1746.2000.02252.x. [DOI] [PubMed] [Google Scholar]
- 10.Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–6. doi: 10.3109/00365528909091339. [DOI] [PubMed] [Google Scholar]
- 11.Fani A. A study on the patteren of prevalence of inflamatory bowel disease and its clinical presentation in Arak. Rahavard Danesh Journal of Arak University of Medical Sciences. 2002;18:28–33. [Google Scholar]
- 12.Masoodi M, Agah S, Faghihi Kashani AH, Eghbali H. Estimation of Ulcerative Colitis Incidence in Hormozgan Province, Southern Iran. Govaresh. 2012;16:265–9. [Google Scholar]
- 13.Rahimi HO, Vahedi H, Isfahani F, Malekzadeh R. Are Breast feeding and measeles vaccination in infancy increase Inflamatory Bowel Disease later? Govaresh. 2008;13:81–8. [Google Scholar]
- 14.Firouzi F, Bahari A, Aghazadeh R, Zali MR. Appendectomy, tonsillectomy, and risk of inflammatory bowel disease: a case control study in Iran. Int J Colorectal Dis. 2006;21:155–9. doi: 10.1007/s00384-005-0760-3. [DOI] [PubMed] [Google Scholar]
- 15.Ebrahimi Dariani N, Mohamadi HR, Airamloo M. Clinical and epidemiological chacteristics in Ulcerative Colitis patients Reffered to Imam Hospital 1995-2000. The Journal of Tehran Faculty of Medicine. 2001;4:85–90. [Google Scholar]
- 16.Aghazadeh R, Zali MR, Bahari A, Amin K, Ghahghaie F, Firouzi F. Inflammatory bowel disease in Iran: a review of 457 cases. J Gastroenterol Hepatol. 2005;20:1691–5. doi: 10.1111/j.1440-1746.2005.03905.x. [DOI] [PubMed] [Google Scholar]
- 17.Zahedi MJ, Darvish-Moghadam S, Haiatbakhsh M, Dalirsani Z. Demographic and Clinical Features of Ulcerative Colitis Patients in Kerman City during 2005-2007. Journal of Kerman University of Medical Sciences. 2009;16:45–53. [Google Scholar]
- 18.Keshavarz A.A, Izadi B. Frequency of Colonic Extension by Colonoscopy in Ulcerative Colitis Patients in Kermanshah Province in the Years 2002-2005. Behbod. 1386;11:441–9. [Google Scholar]
- 19.Fakheri H. Inflamatory Bowel Disease in Sari, Northeren of Iran , Report of 302 cases. Govaresh. 2007;12:155–60. [Google Scholar]
- 20.Vahedi H, Merat S, Momtahen S, Olfati G, Kazzazi AS, Tabrizian T. et al. Epidemiologic characteristics of 500 patients with inflammatory bowel disease in Iran studied from 2004 through 2007. Arch Iran Med. 2009;12:454–60. [PubMed] [Google Scholar]
- 21.Masjedi zade AR, Haijiani E, Hashemi SJ, Azmi M, Shayesteh AA. Survey of Epidemiological Findings of Inflamatory Bowel Disease in Khozestan. Scientific Journal of Jundishapor University of Medical Sciences. 2007;6:54–63. [Google Scholar]
- 22.Yazdanbod A, Farazeneh E, Pourfarzi F, Azami A, Mostafazadeh B, Adiban V. et al. Epidemiological profile and clinical characteristics of ulcerative colitis in northwest of Iran: a 10 year review. Tropical Gastroenterology. 2010;31:308–11. [PubMed] [Google Scholar]
- 23.Semnani S, Azarhosh R, Abdolahi N, Besharat S, Roshandel GH, Jabbari A. et al. Inflamatory Bowel Disease(IBD) in Northeast of Iran. Journal of Clinical and Diagnostic Research. 2008;2:731–4. [Google Scholar]
- 24.Mir-Madjlessi SH, Forouzandeh B, Ghadimi R. Ulcerative colitis in Iran: a review of 112 cases. Am J Gastroenterol. 1985;80:862–6. [PubMed] [Google Scholar]
- 25.Tozun N, Atug O, Imeryuz N, Hamzaoglu HO, Tiftikci A, Parlak E. et al. Clinical characteristics of inflammatory bowel disease in Turkey: a multicenter epidemiologic survey. J Clin Gastroenterol. 2009;43:51–7. doi: 10.1097/MCG.0b013e3181574636. [DOI] [PubMed] [Google Scholar]
- 26.Al-Shamali MA, Kalaoui M, Patty I, Hasan F, Khajah A, Al-Nakib B. Ulcerative colitis in Kuwait: a review of 90 cases. Digestion. 2003;67:218–24. doi: 10.1159/000072060. [DOI] [PubMed] [Google Scholar]
- 27.Goh K, Xiao SD. Inflammatory bowel disease: A survey of the epidemiology in Asia. J Dig Dis. 2009;10:1–6. doi: 10.1111/j.1751-2980.2008.00355.x. [DOI] [PubMed] [Google Scholar]
- 28.Mangat BK, Evaschesen C, Lee T, Yoshida EM, Salh B. Ethnic variation in the annual rates of adult inflammatory bowel disease in hospitalized patients in Vancouver, British Columbia. Can J Gastroenerol. 2011;25:73–7. doi: 10.1155/2011/640920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt . Ulcerative Colitis. In: Sleisenger And Fordtran’s Gastrointestinal And Liver Disease :Pathophysiology/Diagnosis / Management. (2010; 2. Saunders Elsevier, Philadelphia.
- 30.Darakhshan F, Khojeini EV, Balaii H, Naderi N, Firouzi F, Farnood A. et al. Epidemiology of Inflammatory Bowel Disease in Iran:A review of 803 cases. Gastroenterology and Hepatology from bed to bench. 2008;1:19–24. [Google Scholar]
- 31.Niriella MA, De Silva AP, Dayaratne AH, Ariyasinghe MH, Navarathne MM, Peiris RS. et al. Prevalence of inflammatory bowel disease in two districts of Sri Lanka: a hospital based survey. BMC Gastroenterology. 2010;10:32. doi: 10.1186/1471-230X-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khawaja AQ, Sawan AS. Inflammatory bowel disease in the Western Saudi Arabia. Saudi Med J. 2009;30:537–40. [PubMed] [Google Scholar]


