Abstract
The adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs) on the upper gastrointestinal (GI) tract and small intestine are well established. The effect of such therapy on the large intestine, so called NSAID-induced colopathy, is less well described. NSAID-induced colopathy usually involves the right colon due to a higher concentration of the drug at this site, but the rectum may also be involved. NSAIDs possibly damage the normal large intestine, which presents as ulceration, colitis and stricture. Even though several studies found that NSAIDs can cause diverticular bleeding and perforation, flare-up of inflammatory bowel disease ,and play a role as an etiologic factor in lymphocytic colitis. Inflammatory bowel diseases , malignancy and infectious colitis must be ruled out before establishing the diagnosis of NSAID –induced colopathy. Discontinuation of the offending drug is mandatory. Here, we have reported the case of a 43-year-old female, NSAID user due to low back pain, who was admitted to the hospital with painless hematochezia.
Keywords: NSAID, NSAID-induced colopathy, Gastrointestinal bleeding
INTRODUCTION
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely recognized for their ability to cause gastroduodenal ulceration. Adverse effects of NSAIDs upon the small and large intestine are frequently recognized. Erosions, superficial and deep ulcerations, strictures and diaphragm-like narrowing in the distal intestine and proximal colon have been identified as complications of chronic use of NSAIDs, particularly the slow release forms.1, 2
CASE REPORT
A 43-year-old female, known to have lumbar disc herniation and severe low back pain, was admitted to the hospital because of painless hematochezia, since one day prior to admission. She had no history of abdominal pain, altered bowel habits, fever, anorexia, weight loss or previous gastrointestinal (GI) bleeding.
Current medications were: extended release Alfen-X (oral diclofenac, 100 mg bid), Gabapentine (300 mg qd), Baclofen (10 mg qd) and intermittent usage of ibuprofen and indomethacin, for four months, due to chronic low back pain. On physical exam, the vital signs was stable and she was afebrile. Abdomen was soft, non-tender,and with normal bowel sound.
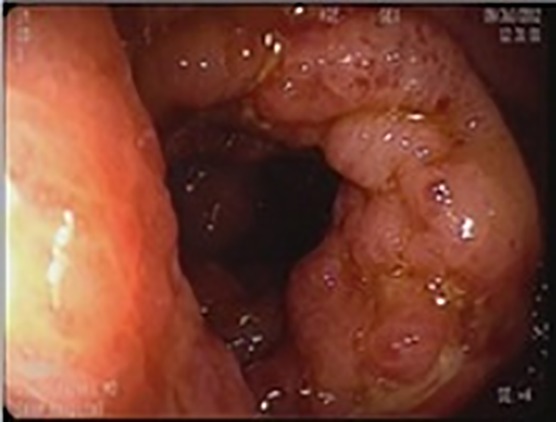
Lab tests showed white blood cells count of 9.8 x 103/μL, hemoglobin of 9.5 g/dL, and MCV of 79fL,a normochrom-normocytic anemia which was probably due to acute blood loss. ESR, CRP, LFT, Bun and Cr were within normal limits. Colonoscopy revealed multiple ulcers with clot and fibrin exudates on it in the ascending colon, cecum and terminal ileum respectively (Figure 1a,b,c), and a few small superficial ulcerations in the transverse, descending colon.
Fig.1a.

Ascending colon: ulcerations with fibrin and clot.
Fig.1b.

Cecum: ulcerations with fibrin and clot.
Fig.1c.
Terminal Ileum: ulcerations with fibrin and clot.
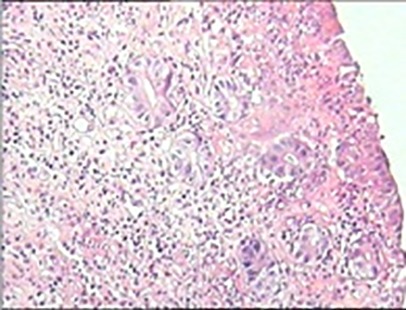
Biopsies from ascending colon, cecum and terminal ileum showed edema, an intense inflammatory cells (lymphocyte and neutrophils) infiltration between glands and ulceration and without evidence of granuloma, fibrosis, crypt abscess, dysplasia and malignancy.(Figure 2a,b,c)
Fig.2a, 2b,2c .
GBiopsy Secti
2a.
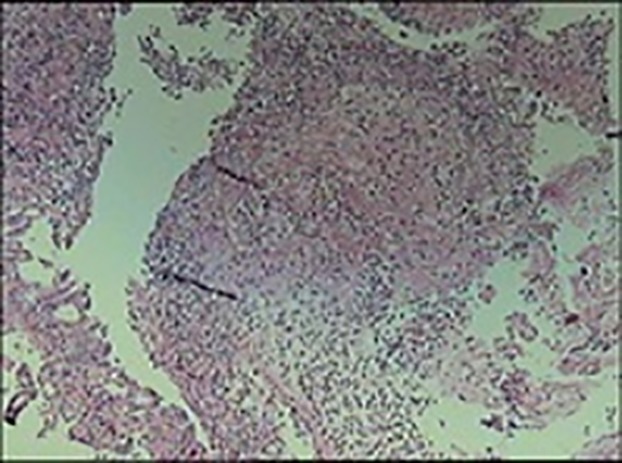
2b.
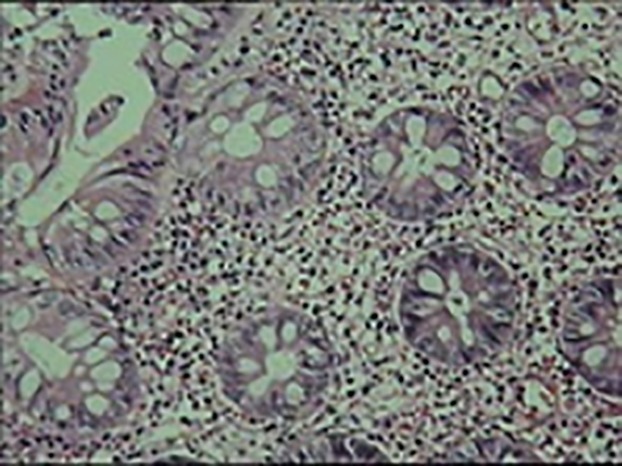
2c.
Bleeding stopped spontaneously one day after admission, and she was discharged four days later without any complications. Additional lab tests were negative for anti-saccharomyces cerevisiae antibody, and anti-neutrophil cytoplasmic antibodies; the stool culture was also negative. According to clinical, endoscopic, pathologic and laboratory data in addition to her history of excessive NSAIDs use, the preferred diagnosis was NSAID-induced colopathy. Alfen-x, ibuprofen and indomethacin were stopped and the patient was followed with a planned colonoscopy, 6-8 weeks later. Two months after discontinuation of NSAIDs, the second colonoscopy showed normal appearing colonic mucosa up to the level of the cecum.(Figure 3a,b,c,b,c). The patient had no GI complaint in serial follow-up.
Fig.3a.

Cecum
Fig.3b .

Ascending Colon
Fig.3c.

Rectum
DISSCUSSION
Despite the beneficial effects associated with their long-term use such as the decrease in colorectal cancer risk and regression of existing polyps. NSAIDs have numerous deleterious effects on the colon. NSAID- induced colopathy is not a rare condition; however, the current case is also unique. Severe lower GI bleeding due to NSAID-induced colopathy is a rare diagnosis. In this case, the endoscopic findings were predominantly detected in the distal small intestine and right colon, the most susceptible sites for the deleterious effects of NSAIDs in the small intestine and large bowel. It appears that these findings are the result of direct drug toxicity due to higher drug concentration, in particular extended –release medication, in the proximal colon.1, 3, 4
NSAID- induced colopathy is clinically important and not just a benign endoscopic finding. There are reports of the development of NSAID-induced fibrous diaphragms of the bowel which can progress to significant strictures upon long-term NSAID use of usually more than one year duration. These lesions may necessitate therapeutic intervention in the form of an endoscopic balloon dilatation and even a segmental colectomy.1, 5, 6
In one study, Tanner et al. have found that approximately 10% of newly diagnosed colitis might be related to NSAID use.2 In 2006, in a case control study, the prevalence of NSAID-induced colitis mong long-term(1to 30 years) NSAID users was 3%; of these, 60% were taking aspirin.7 This side effect of NSAIDs was probably not dose-related. However the duration of treatment was highly associated with the spectrum of endoscopic findings in NSAID-induced colopathy.8
Long-term drug use is not a requirement for the development of NSAID-induced colopathy. Short-term therapy can be just as significant and colitis can occur even after a few days of NSAID use.9, 10 NSAIDs given in both the oral and parenteral forms have been found to cause colonic ulcerations.11 Colonic perforation, as an adverse effect of NSAIDs, has been reported in sporadic cases in the literature.12, 13 Rectal involvement has been also defined as proctitis, ulcerations and/ or strictures with suppository forms of NSAIDs (10-30% with ibuprofen suppositories).14
Sign and symptoms of NSAID-induced colopathy include a change in bowel habits, weight loss or anorexia, GI bleeding, positive occult blood, iron deficiency anemia and abdominal pain. Diagnosis is made by the history of NSAID therapy and endoscopic findings of a non-specific colitis which resolves partially or completely within the six to eight weeks of NSAID withdrawal, although strictures do not regress.15 Whether colonic strictures develop de-novo or are a sequel to ulceration is still unknown. Both direct and indirect mechanisms of damage are believed to be involved in the pathogenesis.16
Increasing awareness of the clinical presentation of NSAID-induced colopathy causes high level of suspicion for this diagnosis in vulnerable cases; other diagnosis such as inflammatory bowel disease should be ruled out. The list of differential diagnosis in a case of colitis with the same presentation are numerous and include infections, inflammatory bowel disease (Crohn’s or ulcerative colitis), ischemic , allergic, collagenous, pseudomembranous, radiation–induced and uremic colitis.17 A diagnosis of NSAID- induced colitis should always be considered in the differentiation of indeterminate colitis.15 Our patient’s clinical presentation along with endoscopic and laboratory findings, and response to drug withdrawal excluded the above mentioned differential diagnoses. We narrowed the diagnosis to an NSAID-induced colopathy.
This would lead to the suitable management and cessation of the offending drug, thereby avoiding potential adverse effects of other unnecessary treatments.8
There is no obvious evidence for the effectiveness of medical treatment in NSAID-induced colopathy. In some case reports, steroids have been used in the treatment of NSAID colonic stricture which failed to resolve after discontinuation of the offending drug,18 In another case report, it has been suggested that a prednisone taper of 40 mg daily, with a 5mg taper each week for two months, might promote healing of colonic ulcerations and prevent re-stricturing.19 Gibson et al. have proposed the use of steroids as a more aggressive treatment for stricture formation.20 However the use of steroids in the treatment of NSAID-induced colopathy cannot be advised until additional studies prove its efficacy.
Faucheron and Bjarnason et al. recommend the use of metronidazole and/or sulphasalazine in the management of NSAID colitis.21- 23 Patients with NSAID-induced colopathy should be discouraged from using these medications at any time in the future, as relapses can occur even after complete recovery.24 COX-2 inhibitors that are used widely, lack some common side effects of the traditional NSAIDs, but there is little available evidence on their possible side effects on colon.25 Freitas et al. have reported a case of acute hemorrhagic colitis after five days rofecoxib therapy, which resolved after the drug was stopped.26 Additional information should be gathered about the effects of COX-2 inhibitors on the colon; in the meantime clinicians should be warned of the potential for COX-2 inhibitor side-effects on the small intestine and large bowel. Misoprostol may decrease the risk of small bowel lesions but this preventive effect has not been well studied. A small study has found a protective benefit with enteric coated low-dose aspirin consumption, but placebo-controlled trials are needed to document the protective effects.27
NSAID-induced colitis is an important entity of which gastroenterologists should be well aware. Its course is usually benign and cessation of the drug is mandatory. Using COX-2 inhibitors as an alternative to non-selective NSAIDs might be effective but their safety is not yet established.
NSAID-induced colitis and ulceration is an important entity of which gastroenterologists should be well aware off. The course is usually benign and cessation of the drug is the rule. Using COX-2 inhibitors as an alternative to non-selective NSAIDs might be effective but their safety is not established yet.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as:
Mokhtare M, Valizadeh SM, Emadian O. Lower gastrointestinal bleeding due to Non-steroid Anti-inflammatory Drug-induced Colopathy Case Report and Literature Review. Middle East J Dig Dis 2013;5:107-11.
References
- 1.Geramizadeh B, Taghavi AR, Banan B. Clinical, endoscopic and pathologic spectrum of non-steroidal anti-inflammatory drug-induced colitis. Indian J Gastroenterol. 2009;28:150–3. doi: 10.1007/s12664-009-0053-9. [DOI] [PubMed] [Google Scholar]
- 2.Tanner AR, Raghunath AS. Colonic inflammation and non-steroidal anti-inflammatory drug administrationAn assessment of the frequency of the problem. Digestion. 1988;41:116–20. doi: 10.1159/000199740. [DOI] [PubMed] [Google Scholar]
- 3.Byrne MF, McGuinness J, Smyth CM, Manning DS, Sheehan KM, Bohra SG. et al. Non-steroidal anti-inflammatory drug-induced diaphragms and ulceration in the colon. Eur J Gastroenterol Hepatol. 2002;14:1265–9. doi: 10.1097/00042737-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Aloysius MM, Kaye PV, Lobo DN. Non-steroidal anti-inflamatory drug (NSAID)-induced colonic strictures and perforation: a case report. Dig Liver Dis. 2006;38:276–8. doi: 10.1016/j.dld.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Gopal DV, Katon RM. Endoscopic balloon dilation of multiple NSAID-induced colonic strictures: case report and review of literature on NSAID-related colopathy. Gastrointest Endosc. 1999;50:120–3. doi: 10.1016/s0016-5107(99)70362-7. [DOI] [PubMed] [Google Scholar]
- 6.Smith JA, Pineau BC. Endoscopic therapy of NSAID-induced colonic diaphragm disease: two cases and a review of published reports. Gastrointest Endosc. 2000;52:120–5. doi: 10.1067/mge.2000.105979. [DOI] [PubMed] [Google Scholar]
- 7.Ohkusa T, Terai T, Abe S. Colonic mucosal lesions associated with long-term administration of non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2006;24(Suppl 4):88–95. [Google Scholar]
- 8.Aftab AR, Donnellan F, Zeb F, Kevans D, Cullen G, Courtney G. NSAID-induced colopathyA case series. J Gastrointestin Liver Dis. 2010;19:89–91. [PubMed] [Google Scholar]
- 9.Hebuterne X, Dreyfus G, Fratini G, Rampal P. Non-steroidal anti-inflammatory drug-induced colitis and misoprostrol. Dig Dis Sci. 1996;41:520–1. doi: 10.1007/BF02282331. [DOI] [PubMed] [Google Scholar]
- 10.Crosby JC, Ross GJ, Auchenbach RC, McCafferty MH. Non-steroidal anti-inflammatory drug-induced cecal ulceration diagnosed on barium enema. J Clin Gastroenterol. 1998;26:154–5. doi: 10.1097/00004836-199803000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Halter F, Weber B, Huber T, Eigenmann F, Frey MP, Ruchti C. Diaphragm disease of the ascending colonAssociation with sustained-release diclofenac. J Clin Gastroenterol. 1993;16:74–80. doi: 10.1097/00004836-199301000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Aloysius MM, Kaye PV, Lobo DN. Non-steroidal anti-inflammatory drug (NSAID)-induced colonic strictures and perforation : a case report. Dig Liver Dis. 2006;38:276–8. doi: 10.1016/j.dld.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Robinson MH, Wheatley T, Leach IH. Non-steroidal anti-inflammatory drug-induced colonic strictureAn unusual cause of large bowel obstruction and perforation. Dig Dis Sci. 1995;40:315–9. doi: 10.1007/BF02065416. [DOI] [PubMed] [Google Scholar]
- 14.Alsalameh S, al-Ward R, Berg P, Aigner T, Ell C. Rectal stricture associated with the long-term use of ibuprofen suppositories. Z Rheumatol. 2000;59:348–51. doi: 10.1007/s003930070058. [DOI] [PubMed] [Google Scholar]
- 15.Malone G, Kaushik VY, Morris JA. Non-steroidal anti-inflammatory drug colopathy. JR Coll Physicians Ednib. 2004;34:32–6. [Google Scholar]
- 16.Gopal DV, Katon RM. Endoscopic balloon dilation of multiple NSAID-induced colonic strictures : case report and review of literature on NSAID-related colopathy. Gastrointest Endosc. 1999;50:120–3. doi: 10.1016/s0016-5107(99)70362-7. [DOI] [PubMed] [Google Scholar]
- 17.El Hajj I, Hawchar M, Sharara A. NSAID-induced colopathy : Case report and review of the literature. J Med Liban. 2009;57:274–6. [PubMed] [Google Scholar]
- 18.Penner RM, Williams CN. Resolution of multiple nonsteroidal anti-inflammatory drug-induced colonic strictures with prednisone therapy : a case report and review of the literature. Can J Gastroenterol. 2003;17:497–500. doi: 10.1155/2003/306498. [DOI] [PubMed] [Google Scholar]
- 19.Weinstock LB, Hammoud Z, Brandwin L. Non-steroidal anti-inflammatory drug-induced colonic stricture and ulceration treated with balloon dilatation and prednisone. Gastrointest Endosc. 1999;50:564–6. doi: 10.1016/s0016-5107(99)70085-4. [DOI] [PubMed] [Google Scholar]
- 20.Gibson GR, Whitacre EB, Ricotti CA. Colitis induced by non-steroidal anti-inflammatory drugs. Arch Intern Med. 1992;152:625–32. [PubMed] [Google Scholar]
- 21.Faucheron JL. Toxicity of non-steroidal anti-inflammatory drugs in the large bowel. Eur J Gastroenterol Hepatol. 1993;11:382–92. doi: 10.1097/00042737-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Bjarnason I, Hopkinson N, Zanelli G, Prouse P, Smethurst P, Gumpel JM. et al. Treatment of non-steroidal anti-inflammatory drug induced enteropathy. Gut. 1990;31:777–80. doi: 10.1136/gut.31.7.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bjarnason I, Hayllar J, Smethurst P, Price A, Gumpel MJ. Metronidazole reduces inflammation and blood loss in NSAID enteropathy. Gut. 1992;33:1204–8. doi: 10.1136/gut.33.9.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kurahara K, Kurahara KMatsumoto T, Lida M, Honda K, Yao T, Fujishima M. Clinical and endoscopic features of non-steroidal anti-inflammatory drug-induced colonic ulcerations. Am J Gastroenterol. 2001;96:473–80. doi: 10.1111/j.1572-0241.2001.03530.x. [DOI] [PubMed] [Google Scholar]
- 25.Wight NJ, Gottesdiener K, Garlick NM, Atherton CT, Novak S, Gertz BJ. et al. Rofecoxib, a COX-2 inhibitor, does not inhibit human gastric mucosal prostaglandin production. Gastroenterology. 2001;120:867–73. doi: 10.1053/gast.2001.22432. [DOI] [PubMed] [Google Scholar]
- 26.Freitas J, Farricha V, Nascimento I, Borralho P, Paramés A. Rofecoxib; a possible cause of acute colitis. J Clin Gastroenterol. 2002;34:451–3. doi: 10.1097/00004836-200204000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Watanabe T, Sugimori S, Kameda N, Machida H, Okazaki H, Tanigawa T. et al. Small bowel injury by low-dose enteric –coated aspirin and treatment with misoprostol:a pilot study. Clin Gastroenterol Hepatol. 2008;6:1279–82. doi: 10.1016/j.cgh.2008.06.021. [DOI] [PubMed] [Google Scholar]


