Abstract
Primary hepatic lymphoma is a rare malignancy usually presenting with symptoms of fever, hepatomegaly, jaundice and weight loss. This picture mimics infectious and inflammatory disorders and thus delays the diagnosis. Here, we present a 47-year old man with prolonged fever who underwent several investigations and, in the meantime, developed fulminant hepatic failure before the diagnosis could be reached.
Keywords: Diffuse Large B-Cell Lymphoma, Fulminant Hepatic Failure, Fever of Unknown Origin
INTRODUCTION
Primary hepatic lymphoma (PHL) is a rare malignancy usually presenting with abdominal pain, anorexia, hepatomegaly and jaundice. Diffuse hepatic involvement is exceedingly rare with only few cases of fulminant hepatic failure (FHF) due to PHL reported in the literature.1- 5
Here, we present a case with prolonged fever who underwent several investigations and, in the meantime, developed hepatic failure before the diagnosis could be reached.
CASE REPORT
A 47-year old man was referred with a history of fever and jaundice for two months. The fever (oral temperature = 38.5°C without chills) and jaundice persisted despite the fact that two weeks ago, he had undergone cholecystectomy in another center for cholelithiasis. The patient was admitted to our center and a full work-up for sepsis was performed, including blood and urine cultures and chest radiography. Laboratory studies revealed abnormal liver enzymes (ALT=80; AST=60; ALP=1,100) and abnormal liver function tests (PT=18”; aPTT=40”; Hb=11; MCV=90; WBC=12,000; Plt=121,000). Serologic evaluations for brucellosis, leishmaniasis, borreliosis, and bone marrow aspiration and biopsy all returned normal. Chest and abdominal CT scans were normal (no mass lesion or lymphadenopathy), except for mild hepatomegaly (Figure 1). Magnetic resonance cholangiopancreatography was also performed, yielding a normal result. A liver biopsy, performed after correction of prothrombin time with fresh frozen plasma, revealed diffuse large B-cell lymphoma (Figure 2). Immunohistochemical assessments indicated the expression of CD20 and Bcl2 on blast, while CD10 was negative. The cells were negative for TdT, excluding a precursor lymphoid neoplasm. Few T-cells (CD5) were intermingled. There was no EBV-association (EBER in-situ hybridization). The proliferative capacity (Ki67) reached 60-70%.
Fig.1.
Hepatomegaly was evident on CTscan.
Fig.2.
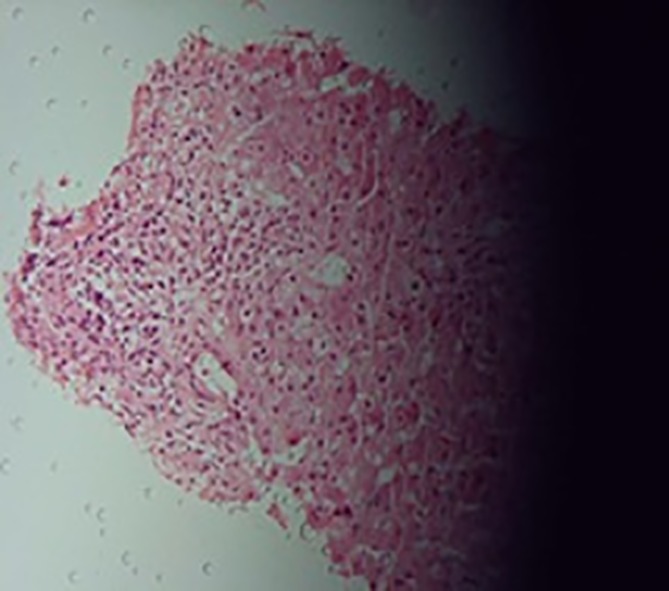
Nodular infiltration of the liver by a diffuse large B-cell lymphoma (centroblastic subtype
In the meantime, the patient expired as a result of fulminant hepatic failure.
DISCUSSION
PHL is associated with a poor prognosis, with a median survival of 8 to 16 months and low rate of complete remission (<20%). Very rare cases of PHL presenting with FHF have almost always been fatal because of the ambiguous features and rapid progression, with most cases diagnosed on autopsy with an average survival of 10.7 days from diagnosis.1
Few cases have been reported to survive FHF caused by hematologic malignancies involving the liver. Cameron et al. reported a patient with FHF from PHL, who underwent urgent orthotopic liver transplantation.4 Saló et al. reported the case of a woman who developed FHF due to infiltration by a non-Hodgkin’s lymphoma. In this case, rapid administration of chemotherapy resulted in complete recovery.6 Finally, Shehab reported a patient with FHF due to Richter’s transformation of CLL who was successfully treated with a CHOP regimen.7 The key to successful treatment in all these cases was early diagnosis by prompt liver biopsy.
The importance of liver biopsy in these patients is highlighted by another issue. While liver transplantation can be lifesaving in patients with FHF, it is imperative to perform a thorough evaluation to screen for potential contraindications. Dellon et al.8 reported a case of FHF in whom liver biopsy revealed natural killer (NK)-like T cell leukemia/ lymphoma to be the cause, thus obliterating liver transplantation once this diagnosis was made.
Patients with PHL have prominent “B” symptoms, including fever and weight loss, that mimic infectious and inflammatory disorders and therefore delay the diagnosis.9 In fact, we believe that the delay in appropriate diagnostic work-up led to the unfavorable outcome in our patient. Although the patient had mentioned no history of biliary pain, he was subjected to an unnecessary cholecystectomy for cholelithiasis that could not explain the initial clinical presentation. The resulting delay allowed the aggressive nature of the disease to ultimately progress to FHF, even though the initial presentation did not include hepatic failure.
A definite diagnosis of PHL is difficult to establish on clinical grounds. Metastasis from gastrointestinal tract (mostly colon) and hepatoma present similarly and are much more common. The standard approach to prolonged fever or fever of unknown origin in a patient with jaundice requires a liver biopsy following minimum diagnostic evaluations, including blood tests for infectious and inflammatory disorders and CT scans of the abdomen and chest.10
As in our case, the most frequent pathology for PHL is diffuse large B-cell followed by small lymphocytic, follicular and marginal B-cell lymphoma.9
PHL is a rare disease that may be neglected in patients with fever and jaundice or fever and hepatomegaly. Adherence to standard approaches to prolonged fever or fever of unknown origin and timely diagnostic workup without a need for a high index of suspicion for this rare condition may contribute to the correct diagnosis.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as:
Kheyri Z, Ali Asgari A, Zare Mehrjerdi A, Zamani F, Ajdarkosh H. Fulminant Hepatic Failure due to Primary Hepatic Lymphoma: a Case Report. Middle East J Dig Dis 2013;5:168-70.
References
- 1.Lettieri CJ, Berg BW. Clinical features of non-Hodgkin lymphoma presenting with acute liver failure: a report of five cases and review of published experience. Am J Gastroenterol. 2003;98:1641–6. doi: 10.1111/j.1572-0241.2003.07536.x. [DOI] [PubMed] [Google Scholar]
- 2.Haider FS, Smith R, Khan S. Primary hepatic lymphoma presenting as fulminant hepatic failure with hyperferritinemia: a case report. J Med Case Rep. 2008;2:279. doi: 10.1186/1752-1947-2-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Das A, Bhusnurmath SR, Sood GK, Chawla Y, Bambery P. Primary hepatic lymphoma mimicking fulminant hepatic failure. Indian J Gastroenterol. 1993;12:147–8. [PubMed] [Google Scholar]
- 4.Cameron AM, Truty J, Truell J, Lassman C, Zimmerman MA, Kelly BS Jr. et al. Fulminant hepatic failure from primary hepatic lymphoma: successful treatment with orthotopic liver transplantation and chemotherapy. Transplantation. 2005;80:993–6. doi: 10.1097/01.tp.0000173999.09381.95. [DOI] [PubMed] [Google Scholar]
- 5.Gargot D, Maitre F, Causse X, Goralski M, Festin D, Legoux JL. Primary liver non-Hodgkin’s lymphoma presenting as fulminant hepatic disease. Eur J Gastroenterol Hepatol. 1994;6:843–6. [Google Scholar]
- 6.Saló J, Nomdedeu B, Bruguera M, Ordi J, Ginès P, Castells A. et al. Acute liver failure due to non-Hodgkin’s lymphoma. Am J Gastroenterol. 1993;88:774–6. [PubMed] [Google Scholar]
- 7.Shehab TM, Kaminski MS, Lok AS. Acute liver failure due to hepatic involvement by hematologic malignancy. Dig Dis Sci. 1997;42:1400–5. doi: 10.1023/a:1018889904839. [DOI] [PubMed] [Google Scholar]
- 8.Dellon ES, Morris SR, Tang W, Dunphy CH, Russo MW. Acute liver failure due to natural killer-like T-cell leukemia/lymphoma: a case report and review of the literature. World J Gastroenterol. 2006;12:4089–92. doi: 10.3748/wjg.v12.i25.4089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lei KI, Chow JH, Johnson PJ. Aggressive primary hepatic lymphoma in Chinese patientsPresentation, pathologic features, and outcome. Cancer. 1995;76:1336–43. doi: 10.1002/1097-0142(19951015)76:8<1336::aid-cncr2820760807>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 10. Bor DH. Approach to the adult with fever of unknown origin. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA, 2013.


