Abstract
The case control study was conducted to quantify the amount of the carcinogenic tobacco specific nitrosamine in smokeless tobacco users and smokers in patients with oral leukoplakia and also to emphasize the role of tobacco-specific nitrosamine in the incidence of oral leukoplakia. The study was conducted on 30 patients. The urine samples were obtained from smokeless tobacco users with oral leukoplakia, smokers with oral leukoplakia and non-tobacco users (i.e. people who do not use tobacco in any form). The collected samples were processed by gas chromatography-mass spectrometry. A highly significant difference of NNAL[4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol] in smokeless tobacco users than tobacco smokers P = 0.0002 (Table 1) was obtained. This significant difference shows smokeless tobacco is more carcinogenic than smoked tobacco. This study confirmed that NNAL is a potent biomarker for calculating the risk of occurrence of carcinoma in smokeless tobacco users and smokers, and that smokeless tobacco is more harmful than smoked tobacco.
Keywords: Urinary biomarker NNAL, Leukoplakia, Oral cancer
Introduction
Oral cancer is one of the ten most common cancers in the world. In spite of this, there are over one billion smokers in the world and millions of people use smokeless tobacco products [1]. World health organization (WHO) has reported that about 90 % of oral cancer in South-East Asia is attributed to the usage of tobacco. Premalignant lesions of the oral cavity represent an important target for cancer prevention. A significant proportion of oral squamous cell carcinomas develop from premalignant lesions such as leukoplakia, erythroplakia or erythroleukoplakia which have a strong etiologic factor of tobacco products [2].
WHO, defined leukoplakia as a white patch or plaque that cannot be characterized clinically or pathologically as any other disease. As such, leukoplakia should be used only as a clinical term. It has no specific histopathological connotation and should never be used as a microscopic diagnosis [3]. Consumption of tobacco is through smoking and chewing. Smoked forms of tobacco are cigarette, beedi, chutta, chevroots, hookli, hooka, dhumti and chillum. Even reverse smoking habit is in use. Reverse smoking is a type of smoking in which the glowing end of the tobacco product is kept inside the mouth. Smokeless forms of tobacco are betel quid, pan masala, mawa and khaini [4].
Among the smoked forms of tobacco chevroots are rolls made from tobacco leaves. A chutta is a type of chevroot made at home. Dhumti is made by rolling a tobacco leaf with the leaf of another plant, forming a conical cigar like stick. Cigars are made of air-cured fermented tobacco. Chevroot is a roll made from tobacco leaves. Chuttas are coarsely prepared chevroots. Hookah is an Indian water pipe in which the tobacco smoke passes through water. Chillum is a straight, conical pipe made of clay, 10–14 cm long, held vertically and used for smoking opium and other narcotics.
Among the smokeless tobacco products pan masala is a commercial preparation containing areca nut, slaked lime, catechu and condiments, with or without powdered tobacco. Mawa contains thin shavings of arecanut with the addition of some tobacco and slaked lime. Khaini is a mixture of sun-dried tobacco and slaked lime. Swedish snuff called snus is available in teabag-like pouches. The pouch can be kept in the buccal or labial groove and sucked. Mishri is a roasted, powdered preparation made by baking tobacco on a hot metal plate until it is uniformly black [4].
Tobacco-specific nitrosamines, a group of carcinogens formed from tobacco alkaloids such as 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) play a significant role in the initiation of oral cancer and hence quantifying NNAL might help to assess the incidence of oral cancer [5].
Urinary NNAL 4-(methylnitrosoamino)-1-(3-pyridyl)-1-butanol has been widely used as a biomarker of exposure to the carcinogen, NNK 4-(methylnitrosoamino)-1-(3-pyridyl)-1-butanone in tobacco products [5].
Materials and Methods
This case control study was conducted in the outpatient Department of Oral Medicine and Radiology. 30 samples of urine were collected from (1) ten smokeless tobacco users with oral leukoplakia, (2) ten smokers with oral leukoplakia and (3) ten non-tobacco users (people who do not use tobacco in any form) as control. Permission from the Institutional Ethical Committee and informed consent from patients to participate in the study were obtained. The selected patients were given 3.5 l amber coloured bottle to collect 24 h urine. (Amber coloured bottle contains 20 % ammonium sulfamate in 3.6 n H2SO4). From the urine that was collected for 24 h, 15 ml was transferred to 4-oz amber coloured bottle by using pipette and stored at −80 °C temperature in the laboratory. The sample was placed in room temperature for 5 h before processing. All the batches of samples were processed at the same time.
For processing the sample was transferred to a conical glass centrifuge tube and centrifuged at 1,500 rpm for 3 min. A solution of glucuronidase (12,000 units) in 1 ml of H2O was added to the centrifuged sample. The sample was incubated at 37 °C overnight. Then the sample was transferred to a micro vial and heated at 50 °C for 60 min. After that the sample was injected into a GC column. The GC machine was programmed to keep the flow rate of helium through the column at a constant rate of 0.8 ml/min. Initially the GC machine temperature was at 80 °C for 2 min, then it was increased to 180 °C for 1 min, then to 210 °C for 1 min and then to 250 °C for 5 min. Then the readings were recorded through mass spectrometry detectors and this data was collected in the computer.
Results
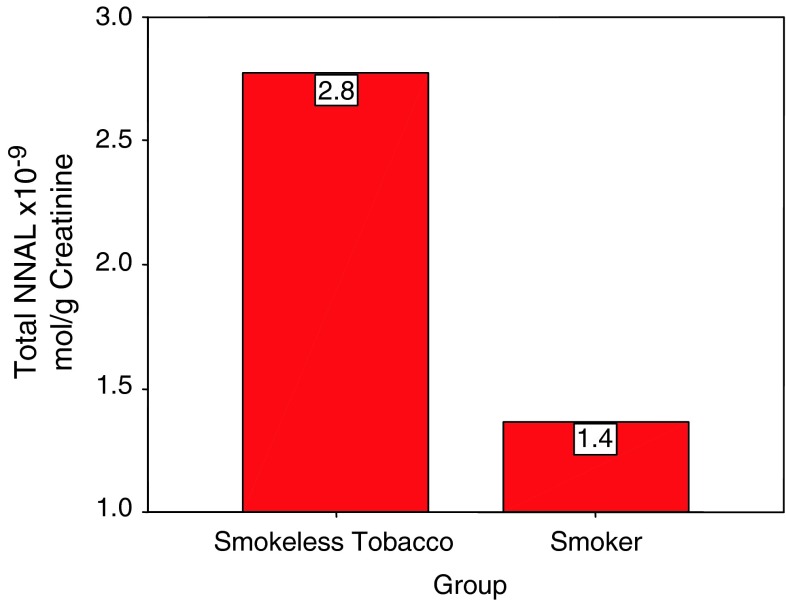
When the NNAL of ten samples of smokeless tobacco users with oral leukoplakia and ten samples of smokers with oral leukoplakia were compared with that of ten samples of control who did not use tobacco in any form, the control samples did not show even a trace of NNAL. Results were statistically analyzed by using unpaired and paired t test and it showed that smokeless tobacco users are more prone for cancer than smokers and a P value of 0.0002 (Table 1) (Graph 1) was obtained.
Table 1.
Showing the comparative result of NNAL in independent t-test
| Group | Independent samples t-test | |||||||
|---|---|---|---|---|---|---|---|---|
| Smokeless tobacco (N = 10) | Smoker (N = 10) | |||||||
| Mean | SD | SE | Mean | SD | SE | t | Sig. | |
| Total NNAL ×10−9 (mol per g creatinine) | 2.7740 | 0.3232 | 0.1022 | 1.3650 | 0.3047 | 0.0964 | 10.031 | 0.000 |
Graph 1.
Showing the NNAL distribution in smokeless tobacco users and smokers
Discussion
In India, oral cancer is highly prevalent, due to the habit of tobacco chewing in the form of betel quid that is commonly observed in the population [4]. Smoking of tobacco like cigarettes, cigars, pipes etc. also causes oral cancer [6]. Several reports have suggested the association of high risk of oral cancer with greater amounts of tobacco used and longer duration of use [7]. Tobacco-specific nitrosamines, a group of carcinogens formed from tobacco alkaloids during the curing and processing of tobacco, are present in both unburnt tobacco and tobacco smoke, and are likely to play a significant role in cancer induction by tobacco products [8]. The most carcinogenic of the commonly occurring tobacco-specific nitrosamines is 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL). Cumulative NNAL are believed to play an important role in oral cancer induction by smokeless tobacco products. The first report of the role of NNAL was published in 1978 [9].
Previous literature states that a person who smokes more than one pack of cigarettes a day is 24 times more likely to develop oral cancer than people who do not use either substance [10]. The high incidence of oral cancer in India is linked with smokeless tobacco habit than smoking tobacco in various forms for a longer duration [11].
In this study, among smokeless tobacco users NNAL was found to be more in pan masala than betel leaf and areca nut and a P value of 0.005 was obtained (Table 2). The previous literature, states that pan masala, the major form of chewing tobacco used in India, is a commercial mixture of tobacco, lime, spices, and areca nut [10]. Its use in India has been growing steadily, and it is often used by teenagers and young adults. It has been shown to form high levels of carcinogenic N-nitroso compounds to induce cytogenetic damage [12].
Table 2.
Showing NNAL distribution in types of smokeless tobacco chewers (paired t-test)
| Types of smokeless tobacco chewers | N | Mean | SD | Std. error mean | t | Sig. | |
|---|---|---|---|---|---|---|---|
| Total NNAL ×10−9 (mol/g creatinine) | Pan masala | 6 | 2.9767 | 0.18833 | 0.07688 | 3.901 | 0.005 |
| Betal leaf and arecanuts | 4 | 2.4700 | 0.22106 | 0.11053 |
Among tobacco smokers, NNAL was found to be more in beedi smokers than cigarette smokers and the P value of 0.009 (Table 3) was obtained. The previous literature states that beedis contain much higher levels of phenol, hydrogen cyanide, benzo(a)pyrene and flavouring agents than conventional cigarettes and it may produce carcinogens other than those commonly found in tobacco [10]. Flavouring agents added to beedis are not rigidly controlled and so the composition may vary [13].
Table 3.
Showing NNAL distribution in types of tobacco smokers (paired t-test)
| Types of tobacco smokers | N | Mean | SD | Std. error mean | t | Sig. (2-tailed) | |
|---|---|---|---|---|---|---|---|
| Total NNAL ×10−9 (mol/g creatinine) | Cigarette | 6 | 1.1833 | 0.19755 | 0.08065 | −3.410 | 0.009 |
| Beedi | 4 | 1.6375 | 0.22021 | 0.11010 |
The study shows the highly significant difference of NNAL in smokeless tobacco users than tobacco smokers. This study also shows that users of pan masala, beedi are highly prone for cancer than betel leaf, arecanut and cigarette users. Our study further confirms, the urinary biomarker of NNAL to be associated with the presence of leukoplakia, which provides biochemical support for the role of smokeless and smoked tobacco products as a cause of oral leukoplakia. NNAL is precipitated in very small amount in a 24 h urine sample. Previous data shows 35–45 fold increase in the relative risk of tobacco induced oral cancer, when total NNAL range elevated constantly over 5 pmol/mg Cr/day urine [14].
This study is in concurrence with the study done by Kresty et al. in 1996 [5] who analyzed the metabolites of a tobacco-specific nitrosamine, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK), in the urine of smokeless tobacco users, to find the relationship between urinary biomarker and oral leukoplakia.
Conclusion
In this case control study, we have confirmed that NNAL is a potent biomarker for calculating the risk of occurrence of carcinoma in smokers, smokeless tobacco users and that smokeless tobacco is more harmful than smoked tobacco. Urinary NNAL estimation is a safe, non invasive method of estimation that can be effectively used for screening large population, who have the habit of using tobacco in smoked or smokeless form and are prone for oral cancer.
The results of the study demonstrated that there is significant uptake of carcinogenic nitrosamines in smokeless tobacco users and such products are not harmless alternative cigarettes. Further, it is emphasized that this study has to be continued on a larger sample.
Acknowledgments
Authors would like to thanks Innovis Lab, SRMCH&RI, Porur, Chennai, India.
References
- 1.Thomas G, Hashibe M, Jacob BJ. Risk factors for multiple oral premalignant lesions. Int J Cancer. 2003;107:285–291. doi: 10.1002/ijc.11383. [DOI] [PubMed] [Google Scholar]
- 2.Scully C, Hopper C. Oral cancer: current and future diagnostic techniques. Am J Dent. 2008;21:199–209. [PubMed] [Google Scholar]
- 3.Neville BW, Day TA. Oral cancer and precancerous lesions. CA Cancer J Clin. 2002;52:195–215. doi: 10.3322/canjclin.52.4.195. [DOI] [PubMed] [Google Scholar]
- 4.Nair U, Bartsch H. Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: a review of agents and causative mechanisms. J Mutagen. 2004;19(4):251–262. doi: 10.1093/mutage/geh036. [DOI] [PubMed] [Google Scholar]
- 5.Kresty LA, Carmella SG, Borukhova A, Akerkar SA, Gopalakrishnan R, Harris R, et al. Metabolites of a tobacco specific nitrosamine, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (nnk), in the urine of smokeless tobacco users: relationship between urinary biomarkers and oral leukoplakia. J Cancer Epidemiol Biomarkers Prev. 1996;5:521–525. [PubMed] [Google Scholar]
- 6.Stepanov I, Hecht SS. Glucuronides in the urine of smokers and smokeless tobacco-specific nitrosamines and their pyridine-N tobacco users. J Cancer Epidemiol Biomarkers Prev. 2005;14:885–891. doi: 10.1158/1055-9965.EPI-04-0753. [DOI] [PubMed] [Google Scholar]
- 7.Pagare SS, Sachdev PD. Ablation of oral leukoplakia with CO2 laser: a clinical study. Sci J. 2009;III:89–95. [Google Scholar]
- 8.Bouquot JE, Suarez P. Oral precancer and early cancer detection in the dental office—review of new technologies. J Implant Adv Clin Dent. 2010;9:44–47. [Google Scholar]
- 9.Liu W, Wang Y-F. Malignant transformation of oral leukoplakia: a retrospective cohort study of 218 Chinese patients. J BMC Cancer. 2010;10:685–688. doi: 10.1186/1471-2407-10-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trock B. Out of the mouths of babes: oral premalignant lesions and use of alternative tobacco products. J Cancer Epidemiol Biomarkers Prev. 2000;9:637–638. [PubMed] [Google Scholar]
- 11.Ramakrishnan S, Gupta PC. Tobacco-specific nitrosamines in smokeless tobacco products marketed in India. Int J Cancer. 2005;116:16–19. doi: 10.1002/ijc.20966. [DOI] [PubMed] [Google Scholar]
- 12.Patel JB, Shukla SN. Utility of urinary biomarkers in oral cancer. Asian Pacific J Cancer Prev. 2007;8:229–235. [PubMed] [Google Scholar]
- 13.Hecht SS, Carmella SG, Murphy SE, Riley WT, Le C, et al. Similar exposure to a tobacco-specific carcinogen in smokeless tobacco users and cigarette smokers. J Cancer Epidemiol Biomarkers Prev. 2007;16:1567–1572. doi: 10.1158/1055-9965.EPI-07-0227. [DOI] [PubMed] [Google Scholar]
- 14.Elswick RK, Jr, Alzyoud S. Differences between urinary and plasma biomarkers of tobacco smoke exposure among cigarette smokers. J Tobacco Use Insights. 2001;2:12–20. [Google Scholar]