Abstract
Since the report from the national high blood pressure (BP) education program working group on BP in children and adolescents and the introduction of a new description called prehypertension many data have been provided on its rate of progression to hypertension, its prevalence and association with other cardiovascular (CV) risk factors and its therapy. Making a diagnosis of prehypertension in a child or adolescent identifies an individual at increased risk for early-onset CV disease who requires specific treatment. Thus, routine BP measurement is highly recommended at every health-care encounter beginning at 3 years of age. This review will present updated data on prehypertension in children and adolescents to increase awareness of health-care providers to the seriousness of this condition. Optimal BP measurement techniques as well as the evaluation and management of prehypertension will be discussed and preventive strategies to reduce the CV risk will be presented.
Keywords: Cardiovascular disease, children and adolescents, essential hypertension, pre-hypertension, prevention
INTRODUCTION
Childhood prehypertension is a common clinical problem facing both primary care clinicians and specialist. Considering the prevalence of prehypertension >30% in asymptomatic obese adolescents, its rate of progression to hypertension and association with cardiovascular (CV) risk factors, prehypertension should be considered a common long-term health problem inchildhood.[1,2,3]
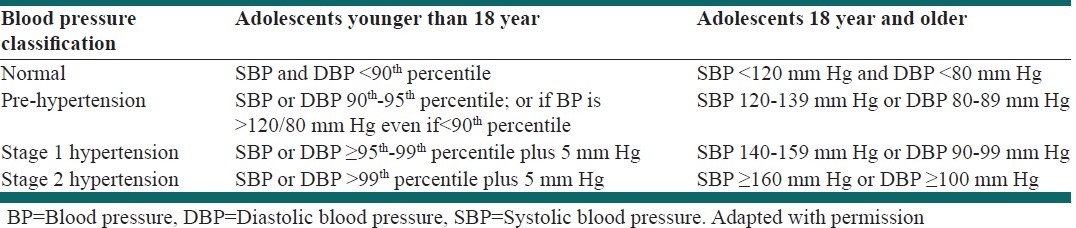
The National High Blood Pressure (BP) Education Program Working Group on High BP in children and adolescents defines hypertension as an average systolic and/or diastolic BP that is ≥the 95th percentile for sex, age and height on ≥3 occasions.[4] In 2004, the working group on high BP introduced a new term called “prehypertension” to designate children and adolescents whose BP levels were higher than normal, but did not reach the level of hypertension.[4] Children with systolic or diastolic BP between 90th and 95th percentile or adolescents with BP >120/80 mm Hg are now defined as prehypertension as opposed to the “high normal” classification that was used previously [Table 1]. The overall intent of this designation was to help identify children who were at the greatest risk for the development of hypertension over a lifetime as well as added risk of CV outcomes due to comorbidities such as obesity and diabetes and in whom therapeutic approaches to prevent or delay the onset of hypertension would be of value.
Table 1.
Classification of hypertension in adolescents
Since the 2004 report from the working group on BP in children and adolescents, advances in the ability to identify, evaluate and care for children and adolescent with prehypertension have led to an increased awareness of this serious medical condition.[1,2,3]
Prehypertension is usually asymptomatic and easily missed, even by health-care professionals.[5] The rate of progression of prehypertension to hypertension can be relatively rapid, particularly in those whose BP lie in the upper portion of the prehypertension range.[1,3] Prehypertension in children as in adults, is commonly associated with obesity, metabolic syndrome and dyslipidemia.[6,7,8,9] The risk ratio for chronic kidney disease (CKD) and CV event are also greater in prehypertensive than hypertensive persons.[10,11,12,13]
Microalbuminuria is also more common in pre-hypertension than normotension as are abnormalities in circulating markers of inflammation, like C-reactive proteins.[14] The national high BP education program working group on BP in children and adolescents report has recommended the adoption of healthy life-styles to achieve BP goals except in prehypertensive subjects with diabetes or chronic renal disease in whom drug treatment is also advocated.[4] The decision to use antihypertensive drug treatment in pre-hypertensive subjects in the absence of diabetes or chronic renal disease should be based on global CV risk rather than on specific levels of BP alone.
DEFINING PREHYPERTENSION
Hypertension in children and adolescent less than 18 years is defined as an average systolic and/or diastolic BP that is ≥95th percentile for sex, age and height on ≥3 occasions.[4] In the 2004, the working group replaced the term “high normal BP” with the term “prehypertension” to designate all children and adolescents whose BP levels were higher than normal, but did not reach the level of hypertension [Table 1].[4] The aim of this designation was to help identify children who were at the greatest risk for the development of hypertension over a lifetime as well as added risk of CV outcomes due to comorbidities such as obesity and diabetes and in whom therapeutic approaches to prevent or delay the onset of hypertension would be of value.
Data on the prevalence of prehypertension in children and adolescents varies with the study population and patient ethnicity. Recent data from large samples of healthy adolescents show that the rates of hypertension and prehypertension in adolescents are increasing.[1,3] One study of nearly 14,000 healthy children from well child clinic visit in the United States noted that 3.4% of the population had prehypertension[5] while a data reported by McNiece et al. and associates on high school students put the figure at 15.7%.[2] Recent data also indicate that obesity-associated hypertension and prehypertension in adolescence is a major public health problem and a condition that is likely to contribute substantially to future CV disease.[6,7,8,9] A data from the National Health and Nutrition Examination Surveys (NHANES) studies examined BP levels in children and adolescents and identified a significant increase in both systolic and diastolic BP level.[8] A subsequent study on the same two NHANES databases detected an overall increase in the prevalence of childhood hypertension from 2.7% in the 1988-1994 survey to 3.7% in the 1999-2002 survey periods.[9] Both reports verified that the increase in BP level and prevalence of hypertension in adolescents is largely due to the increasing prevalence of obesity.
WHY TARGET PREHYPERTENSION?
Evidence indicates that BP measured in adolescence predicts future BP.[14,15,16] There are also reports that link prehypertension in childhood with hypertension in early adulthood.[5] Among adolescents with prehypertension, 14% developed hypertension 2 years later and among adolescents with prehypertension and obesity combined, 68% of boys and 43% of girls had hypertension 2 years later.[17]
Many of the factors associated with the development of hypertension, particularly obesity, as well as male gender and black race, are also associated with prehypertension.[18,19] It has been shown patients with prehypertension are at increased risk of developing hypertension and CV event.[10,11,12,13,20]
Elevated serum uric acid level has also been considered a risk factor for development of hypertension and CV risk.[21] Results from animal models suggest that uric acid induces vasoconstriction by activation of the renin-angiotensin system and reduction of nitric oxide, which can be revered by lowering uric acid.[22] Overtime, uric acid uptake into the vascular muscle cells causes cellular proliferation and secondary arteriosclerosis.[23] Consistent with the animal data, clinical trials performed in adolescents with prehypertension[24] and newly diagnosed essential hypertension demonstrate that reduction of uric acid can mitigate BP elevations.[25,26,27] These data suggest that uric acid plays a significant role, in the pathogenesis of early-onset primary hypertension.[21,22,23,24,25,26,27]
In the trial of preventing hypertension (TROPHY) study, investigators found that nearly two-thirds of participants who had been in the placebo (e.g., untreated) arm, all whom fit the clinical description of prehypertensive, progressed to stage 1 hypertension.[28] Furthermore, hypertension is considered to be a self-accelerating condition in that ongoing structural changes, including arteriolar hypertrophy and endothelial dysfunction, contribute to increased vasoconstriction. These have been seen in prehypertensive patients and are hallmarks of the transition from prehypertension to hypertension.[27]
Compared with normotensive patients, those with prehypertension are more likely to experience higher cholesterol levels, obesity or overweight as measured by body mass index (BMI) and diabetes.[28,29] However, the increased CV risk associated with prehypertension cannot be explained entirely by an increased prevalence of other CV factors and is likely also to be related to BP elevation per se.[20,27] Inflammatory markers such as microalbuminuria, C-reactive proteins, interleukin 6 and tumor necrosis factor-α are also more common in prehypertensive and hypertensive patients than in those with normal BP levels.[14,30,31]
In addition patients with prehypertension face a higher risk of CV mortality as their BP levels rise. Assadi reported that treating microalbuminuria in children with primary hypertension with renoprotective therapy was associated with left ventricular hypertrophy regression.[32] A meta-analysis involving more than 1 million adults showed that in individuals 40-69 years of age, every increase of 20/10 mm Hg starting at a normal level of 115/75 mm Hg doubled the risk of stroke death and cardiac death.[33] Thus, the prehypertensive patients already face a higher risk of CV death, even though they are not yet classified as being hypertensive.[33,34]
SCREENING FOR HYPERTENSION RISK
Risk factors associated with the development of both prehypertension and hypertension include, excess body weight; excessive sodium intake; insufficient physical activity; inadequate consumption of fruits, vegetables and potassium; and excessive alcohol consumption. Parikh et al. have designed a risk stratification scheme using the measures easily obtainable in a doctor's office. These authors, suggested that age, gender, BMI, family history of hypertension, cigarette smoking, systolic blood pressure (SBP) and diastolic blood pressure (DBP), BMI, were associated with the higher incidence of hypertension.[35]
It is shown that the following life-style modifications can help reduce SBP [Table 2]:[35,36]
Table 2.
Life-style interventions to prevent and manage hypertension
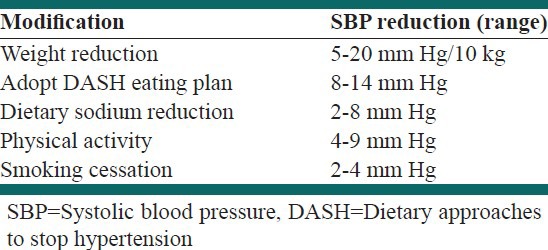
Achieving a normal body weight (BMI 18.5-24.0 kg/m2) may reduce SBP as much as 20 mm Hg
Adopting the dietary approaches to stop hypertension (DASH) diet (rich in fruits, vegetables and low-fat dairy products) could result in a drop in SBP as great as 14 mm Hg
Keeping stress levels down also can help prevent progression of prehypertension to full-blown hypertension. Analysis of data from the atherosclerosis risk in communities trial showed that among men with higher levels of anger, there was a modest association with progression to hypertension.[37] Thus, a healthy, reduced-stress life-style can produce significant benefits and may reduce or prevent the need for pharmacological treatment if their prehypertension progresses. The effectiveness of the complete package of life-style interventions recommended by Joint National Committee 7 (JNC-7),[38] was supported by the results of the PREMIER trial.[39]
HOW TO BEST MANAGE PREHYPERTENSION?
The medical treatment of prehypertension has been the subject of recent debate since the report of Working Group on High BP in Children and Adolescents was released in 2004. The JNC-7 report has recommended the adoption of healthy life-styles to achieve BP goals except in prehypertensive subjects with diabetes or chronic renal disease in whom drug treatment is also advocated.[38]
Is there a role for antihypertensive drug treatment in prehypertensive subjects in the absence of diabetes or chronic renal disease? The answer is yes, for at least one group, African American, according to the International Society on Hypertension in Blacks (ISHIB).[40] The ISHIB report recommends that for primary prevention of hypertension in blacks, medical therapy should be initiated at 135/85 mm Hg and at 130/80 mm Hg in adult subjects with preclinical CV disease, and/or a history of CV disease.[40] The statement further recommends monotherapy with a diuretic or calcium channel blocker in those patients whose BP is ≤10 mm Hg above target and combination therapy in patients with a BP >10 mm Hg above target.
Beyond targets for the black population, some investigators are looking at whether implementing pharmacotherapy in prehypertensives in general can help prevent progression of the disease. In TROPHY, patients considered prehypertensive were randomized to either the angiotensin receptor blocker (ARB) candesartan or placebo for 2 years and all patients were followed for an additional 2 years.[28] Use of the ARB significantly suppressed progression to hypertension at both 2- and 4-year follow-up; although the magnitude of the reduction in new-onset hypertension was attenuated (16% vs. 66% during the active treatment phase) once antihypertensive therapy was discontinued. In another study using the angiotensin-converting enzyme inhibitor ramipril, the agent significantly reduced progression to hypertension in prehypertensives compared with the placebo, with no increase in adverse CV or cerebrovascular events.[41]
It has been argued recently that the decision to use antihypertensive drug treatment should be based on global CV risk rather than on specific levels of BP alone.[42] However, adequate clinical trial data are not available as yet to justify such an approach in contrast to the extensive evidence regarding specific BP levels.
A new multicenter, randomized study from the National Institutes of Health called the systolic blood pressure intervention trial is studying patients with prehypertension to test whether reducing SBP levels below the currently recommended goal will reduce the risk of cardiovascular disease and CKD.[43,44] The study is expected to help answer questions not only about the need for aggressive therapy in patients with hypertension, but also about whether prehypertensive patients will reduce their risk and benefit from pharmacotherapy as well.
CONCLUSIONS
The definition of prehypertension is the same in adolescents of all ages, namely a BP reading >120/80 mm Hg. Prehypertension children and adolescents plus other metabolic risk factors are at high risk for accelerated CV disease. Thus, the danger of prehypertension warrants early detection and appropriate life-style modifications including weight loss increased physical activity, use of DASH diet and drug therapy if target-organ damage is present.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Redwine KM, Daniels SR. Prehypertension in adolescents: Risk and progression. J Clin Hypertens (Greenwich) 2012;14:360–4. doi: 10.1111/j.1751-7176.2012.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr. 2007;150:640–4. doi: 10.1016/j.jpeds.2007.01.052. 644.e1. [DOI] [PubMed] [Google Scholar]
- 3.Redwine KM, Falkner B. Progression of prehypertension to hypertension in adolescents. Curr Hypertens Rep. 2012;14:619–25. doi: 10.1007/s11906-012-0299-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76. [PubMed] [Google Scholar]
- 5.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874–9. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 6.Sorof J, Daniels S. Obesity hypertension in children: A problem of epidemic proportions. Hypertension. 2002;40:441–7. doi: 10.1161/01.hyp.0000032940.33466.12. [DOI] [PubMed] [Google Scholar]
- 7.Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. The relationship of body mass index and blood pressure in primary care pediatric patients. J Pediatr. 2006;148:195–200. doi: 10.1016/j.jpeds.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 8.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–13. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 9.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–96. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 10.Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291–7. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 11.Qureshi AI, Suri MF, Kirmani JF, Divani AA, Mohammad Y. Is prehypertension a risk factor for cardiovascular diseases? Stroke. 2005;36:1859–63. doi: 10.1161/01.STR.0000177495.45580.f1. [DOI] [PubMed] [Google Scholar]
- 12.Hsia J, Margolis KL, Eaton CB, Wenger NK, Allison M, Wu L, et al. Prehypertension and cardiovascular disease risk in the Women's Health Initiative. Circulation. 2007;115:855–60. doi: 10.1161/CIRCULATIONAHA.106.656850. [DOI] [PubMed] [Google Scholar]
- 13.Assadi F. Strategies to reduce the incidence of chronic kidney disease in children: Time for action. J Nephrol. 2013;26:41–7. doi: 10.5301/jn.5000157. [DOI] [PubMed] [Google Scholar]
- 14.Assadi F. Relation of left ventricular hypertrophy to microalbuminuria and C-reactive protein in children and adolescents with essential hypertension. Pediatr Cardiol. 2008;29:580–4. doi: 10.1007/s00246-007-9153-4. [DOI] [PubMed] [Google Scholar]
- 15.Gidding SS. Measuring children›s blood pressure matters. Circulation. 2008;117:3163–4. doi: 10.1161/CIRCULATIONAHA.108.787168. [DOI] [PubMed] [Google Scholar]
- 16.Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: The Bogalusa Heart Study. Am J Hypertens. 1995;8:657–65. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 17.Fuentes RM, Notkola IL, Shemeikka S, Tuomilehto J, Nissinen A. Tracking of systolic blood pressure during childhood: A 15-year follow-up population-based family study in eastern Finland. J Hypertens. 2002;20:195–202. doi: 10.1097/00004872-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Falkner B, Gidding SS, Portman R, Rosner B. Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics. 2008;122:238–42. doi: 10.1542/peds.2007-2776. [DOI] [PubMed] [Google Scholar]
- 19.Franklin SS, Pio JR, Wong ND, Larson MG, Leip EP, Vasan RS, et al. Predictors of new-onset diastolic and systolic hypertension: The Framingham Heart Study. Circulation. 2005;111:1121–7. doi: 10.1161/01.CIR.0000157159.39889.EC. [DOI] [PubMed] [Google Scholar]
- 20.Toprak A, Wang H, Chen W, Paul T, Ruan L, Srinivasan S, et al. Prehypertension and black-white contrasts in cardiovascular risk in young adults: Bogalusa Heart Study. J Hypertens. 2009;27:243–50. doi: 10.1097/hjh.0b013e32831aeee3. [DOI] [PubMed] [Google Scholar]
- 21.Julius S, Nesbitt S, Egan B, Kaciroti N, Schork MA, Grozinski M, et al. Trial of preventing hypertension: Design and 2-year progress report. Hypertension. 2004;44:146–51. doi: 10.1161/01.HYP.0000130174.70055.ca. [DOI] [PubMed] [Google Scholar]
- 22.Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. 2008;359:1811–21. doi: 10.1056/NEJMra0800885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mazzali M, Hughes J, Kim YG, Jefferson JA, Kang DH, Gordon KL, et al. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension. 2001;38:1101–6. doi: 10.1161/hy1101.092839. [DOI] [PubMed] [Google Scholar]
- 24.Mazzali M, Kanellis J, Han L, Feng L, Xia YY, Chen Q, et al. Hyperuricemia induces a primary renal arteriolopathy in rats by a blood pressure-independent mechanism. Am J Physiol Renal Physiol. 2002;282:F991–7. doi: 10.1152/ajprenal.00283.2001. [DOI] [PubMed] [Google Scholar]
- 25.Soletsky B, Feig DI. Uric acid reduction rectifies prehypertension in obese adolescents. Hypertension. 2012;60:1148–56. doi: 10.1161/HYPERTENSIONAHA.112.196980. [DOI] [PubMed] [Google Scholar]
- 26.Feig DI. Hyperuricemia and hypertension. Adv Chronic Kidney Dis. 2012;19:377–85. doi: 10.1053/j.ackd.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Assadi F. Coadministration of allopurinol enhances blood pressure lowering effect of enalapril in children with hyperuricemic essential hypertension. J Nephrol. 2014 doi: 10.1007/s40620-013-0009-0. DOI 10.1007/s40620-013-0009-0. [DOI] [PubMed] [Google Scholar]
- 28.Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:1685–97. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 29.Assadi F. The growing epidemic of hypertension among children and adolescents: A challenging road ahead. Pediatr Cardiol. 2012;33:1013–20. doi: 10.1007/s00246-012-0333-5. [DOI] [PubMed] [Google Scholar]
- 30.Flynn JT, Falkner BE. Obesity hypertension in adolescents: Epidemiology, evaluation, and management. J Clin Hypertens (Greenwich) 2011;13:323–31. doi: 10.1111/j.1751-7176.2011.00452.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.King DE, Egan BM, Mainous AG, 3rd, Geesey ME. Elevation of C-reactive protein in people with prehypertension. J Clin Hypertens (Greenwich) 2004;6:562–8. doi: 10.1111/j.1524-6175.2004.03577.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Assadi F. Effect of microalbuminuria lowering on regression of left ventricular hypertrophy in children and adolescents with essential hypertension. Pediatr Cardiol. 2007;28:27–33.32. doi: 10.1007/s00246-006-1390-4. [DOI] [PubMed] [Google Scholar]
- 33.Chrysohoou C, Pitsavos C, Panagiotakos DB, Skoumas J, Stefanadis C. Association between prehypertension status and inflammatory markers related to atherosclerotic disease: The ATTICA Study. Am J Hypertens. 2004;17:568–73. doi: 10.1016/j.amjhyper.2004.03.675. [DOI] [PubMed] [Google Scholar]
- 34.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 35.Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, et al. A risk score for predicting near-term incidence of hypertension: The Framingham Heart Study. Ann Intern Med. 2008;148:102–10. doi: 10.7326/0003-4819-148-2-200801150-00005. [DOI] [PubMed] [Google Scholar]
- 36.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 37.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 38.Player MS, King DE, Mainous AG, 3rd, Geesey ME. Psychosocial factors and progression from prehypertension to hypertension or coronary heart disease. Ann Fam Med. 2007;5:403–11. doi: 10.1370/afm.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 40.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: Main results of the PREMIER clinical trial. JAMA. 2003;289:2083–93. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 41.Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH, Jr, et al. Management of high blood pressure in Blacks: An update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56:780–80. doi: 10.1161/HYPERTENSIONAHA.110.152892. [DOI] [PubMed] [Google Scholar]
- 42.Lüders S, Schrader J, Berger J, Unger T, Zidek W, Böhm M, et al. The PHARAO study: Prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: A prospective, randomized, controlled prevention trial of the German Hypertension League. J Hypertens. 2008;26:1487–96. doi: 10.1097/HJH.0b013e3282ff8864. [DOI] [PubMed] [Google Scholar]
- 43.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 44.Systolic Blood Pressure Intervention Trial (SPRINT). Clinical trials.gov identifier: Clinical trial identifier NCT01206062. [Last accessed on 2013 May 17]. Available from: http://clinicaltrials.gov .


