Abstract
Objective: To determine the prevalence of eclampsia in Qatar, the associated maternal and perinatal outcomes for the period from January 1991 to December 2009 and to define any possible preventive measures to this potentially fatal complication. Methods: A retrospective case review was performed of all women with eclampsia admitted to the Women's Hospital and Obstetrics and Gynecology department at Al Khor Hospital for the period from January 1991 to December 2009. Details were collected by reviewing the files of the patients from the medical records. Data were analyzed by either X2 analysis or the unpaired student “t” test as appropriate. Results: During the period of the study there were 224,809 births. Seventy women developed eclampsia (0.31/1000 deliveries), 44.3% of them were antepartum, 31.4% postpartum and 24.3% intrapartum eclampsia. 34.3% of patients presented with fits, 38.5% presented with pre-eclampsia (PE) and 20% presented with severe pre eclampsia; 18.5% were mild PE and another 27.2% were admitted with different complaints. Symptoms of impending eclampsia were seen in 22.9% of the PE patients. Thirty percent had no antenatal care (ANC). Antihypertensive therapy was given to 72% of cases. Antiepileptic therapy was administered to 48% of cases and 58.5% received magnesium sulfate. Eclampsia was associated with increased rate of cesarean section (CS) (64.2%). There was one maternal death, and the rate of major maternal complications was 20%. The perinatal mortality rate was 12.8%. Conclusion: The incidence of eclampsia in Qatar is 0.31 per 1000 deliveries. Although rare, this condition is associated with increased maternal morbidity and perinatal mortality. However our result is lower than reported worldwide. Improvement of obstetric care by having high index of suspicion even with apparently low risk patients, using magnesium sulfate prophylaxis for all cases of severe pre-eclampsia, in addition to community based approach to improve community health, education and prenatal care, all can be effective measures for the decrease incidence of this fatal condition although eclampsia cannot be entirely prevented.
Introduction
Eclampsia is an obstetric condition, which can present both to general and women's hospitals emergency departments.
Eclampsia is the occurrence of one or more generalized convulsions and/or coma not caused by any co-incidental neurological disease, such as epilepsy, in a pregnant woman whose condition also meets the criteria of pre-eclampsia (sustained protein uric hypertension with edema from 20 weeks gestation to the puerperium).
Pre-eclampsia/eclampsia remains the second most common cause of maternal death in the United States (US) and United Kingdom (UK) after thrombo-embolic disease. 1,2 Eclampsia accounts for 50,000 maternal deaths per year worldwide. 3
Eclampsia is rare before 20 weeks gestation, which should raise the possibility of an underlying molar pregnancy or antiphospholipid syndrome. It is associated with high incidence of perinatal morbidity and mortality, which is mainly related to prematurity. 4
The incidence of eclampsia is relatively stable in 4 to 5 cases/10,000 live births in developed countries and 6 to 100 cases/10,000 live births in developing countries. 5,6 Pathogenesis remains unknown, possibly due to cerebral vasospasm with local ischemia, hypertensive encephalopathy, vasogenic edema and endothelial damage. 7 This study was conducted to detect the incidence of eclampsia in the state of Qatar and the associated maternal and fetal outcomes, with the evaluation of any possible avoidable measures to decrease this incidence.
Materials and Methods
A retrospective study was conducted at the Women's Hospital and Al Khor Hospital Obstetrics and Gynecology department by reviewing the medical record files of all women diagnosed to have eclampsia admitted during the period of the study, from January 1991 to December 2009.
The total annual delivery rate during the study period ranged from 9452 to 15,952 deliveries. The total number of births during the period of the study was 224,809. Parameters checked from the files were maternal age, nationality, parity, gestational age, number of antenatal visits, number of fits, symptoms of impending eclampsia, coma, diagnosis at admission, medications used, mode of delivery, maternal and fetal outcomes. Eclampsia was diagnosed by the occurrence of convulsions during pregnancy, labour or in the first 10 days postpartum with or without hypertension (a systolic blood pressure (BP) of ≥ 140 mmHg and a diastolic of ≥ 90 mmHg and proteinuria (at least +1 or more in a random urine sample or ≥ 0.3 g in a 24 hour collection), after excluding all other causes of fits.
The management of eclampsia at this hospital is directed towards stabilizing the mother, stopping convulsions, prevention of further fits, (by the use of anticonvulsants), controlling BP (by antihypertensives), and delivering the fetus regardless of gestational age.
Results
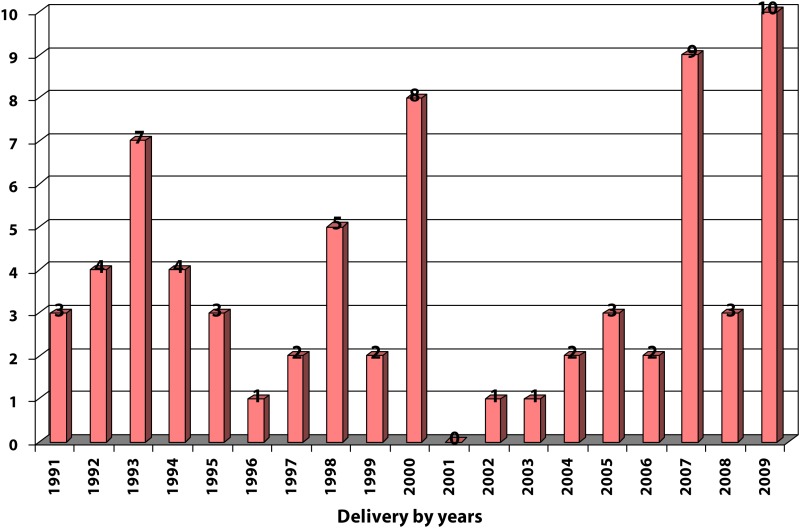
The total number of deliveries was 224,809 during the period of the study from January 1991 to December 2009. Eclampsia was detected in 70 women with an incidence of 0.31/1000 deliveries (details in Table 1).
Table 1.
Prevalence of eclampsia in Qatar.
| Year | Number of deliveries | Eclampsia | Ratio |
| 1991 | 9452 | 3 | 0.31/1000 |
|
| |||
| 1992 | 10150 | 4 | 0.39/1000 |
|
| |||
| 1993 | 10515 | 7 | 0.66/1000 |
|
| |||
| 1994 | 10239 | 4 | 0.39/1000 |
|
| |||
| 1995 | 10092 | 3 | 0.29/1000 |
|
| |||
| 1996 | 10052 | 1 | 0.09/1000 |
|
| |||
| 1997 | 10188 | 2 | 0.19/1000 |
|
| |||
| 1998 | 10500 | 5 | 0.47/1000 |
|
| |||
| 1999 | 10587 | 2 | 0.18/1000 |
|
| |||
| 2000 | 10999 | 8 | 0.72/1000 |
|
| |||
| 2001 | 11734 | 0 | 0.00/1000 |
|
| |||
| 2002 | 11821 | 1 | 0.08/1000 |
|
| |||
| 2003 | 12620 | 1 | 0.07/1000 |
|
| |||
| 2004 | 12838 | 2 | 0.15/1000 |
|
| |||
| 2005 | 13258 | 3 | 0.22/1000 |
|
| |||
| 2006 | 13953 | 2 | 0.14/1000 |
|
| |||
| 2007 | 14586 | 9 | 0.61/1000 |
|
| |||
| 2008 | 15273 | 3 | 0.19/1000 |
|
| |||
| 2009 | 15952 | 10 | 0.62/1000 |
|
| |||
| Total = | 224809 | 70 | 0.31/1000 |
|
| |||
| |||
The timing of fits was 44.3% ante partum (31 cases), 24.3% intra partum (17 cases) and 31.4% postpartum (22 cases) (Figure 1). Thirty-four patients (48.5%) were < 25 years old and 13 patients (18.5%) were teenagers.
Figure 1.
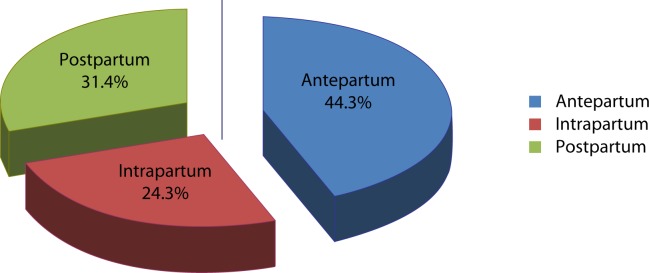
Timing of fits.
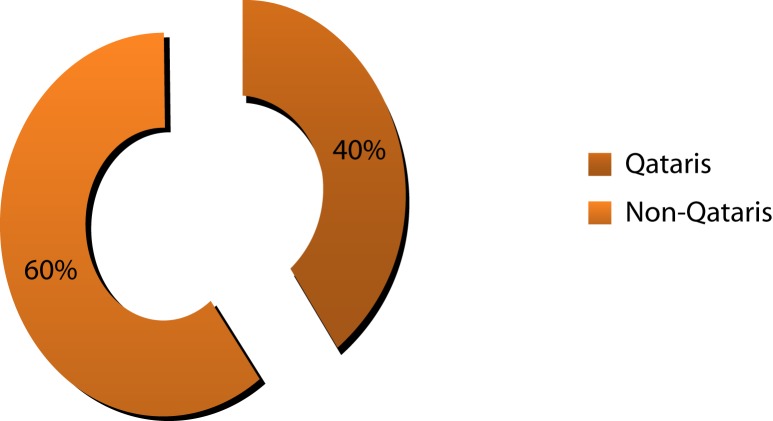
Thirty-two women presented with a gestational age of ≥ 37 weeks (45.7%) and 38 women (54.2%) were < 37 weeks (Figure 2). Further, 65.7% of the patients were primiparous (46 cases) and 34 .3% were multiparous (24 cases). Twenty-eight cases (40%) were Qataris and 42 cases (60%) were non-Qataris (Figure 3). Of the patients, 54.2% were under the age of 25 years and 18.5% were teenagers.
Figure 2.
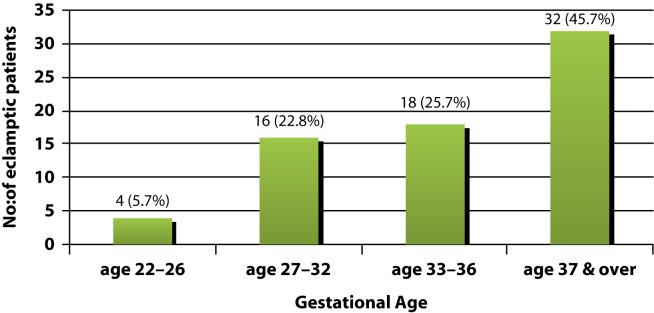
Gestational age distribution for eclamptic patient.
Figure 3.
Nationality of eclamptic patients.
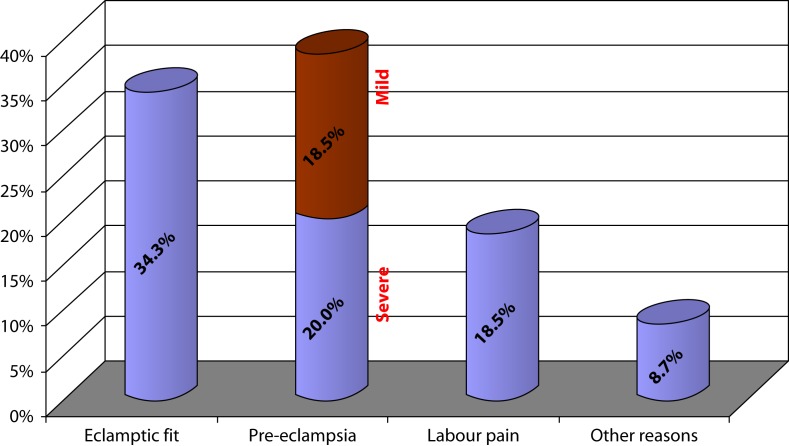
Diagnosis on admission was eclamptic fits in 34.3% of the cases (24 women), 13 of them were referred from the general emergency room; 38.5% of the women were admitted with the diagnosis of pre-eclampsia (27 cases)—14 of them had severe pre-eclampsia (20%) and 13 had mild pre-eclampsia (18.5%). Sixteen cases of PE (22.9%) were admitted with symptoms of impending eclampsia. Ten cases of eclamptic fit (14.3%) had normal blood pressure on admission < 130/80 mmHg. Thirteen women were admitted with labour pains (18.5%), 8.7% of patients were admitted for different reasons; of them 2 with upper respiratory tract infection and two with pre-term labour pain. One patient was admitted with ante-partum hemorrhage and one patient was admitted for suspicion of spontaneous rapture of membranes (Figure 4). Twenty-one patients (30%) had no antenatal visits.
Figure 4.
Diagnosis on admission.
Forty-five cases (64%) were delivered by Cesarean section (CS) and 25 patients (36%) were delivered vaginally. Of the vaginal deliveries, seven cases were delivered by vacuum (10%), which were done for intrapartum eclampsia. Seventeen cases underwent normal vaginal delivery (24%), and one case underwent assisted breech delivery (Figure 5). Of those who delivered vaginally (25 patients), 14 of them had post-partum eclampsia (20%) and only three had ante-partum eclampsia who were induced at 25, 27 and 29 weeks gestation and delivered.
Figure 5.
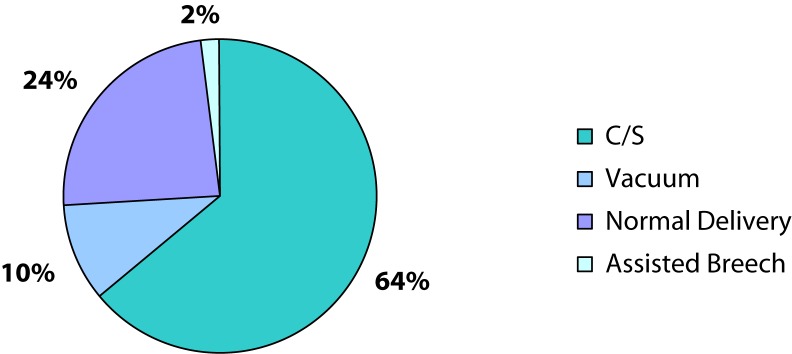
Mode of delivery.
The indications of CS were ante-partum eclampsia in 26 cases (37%), intra-partum eclampsia in four cases (57%), non-reassuring cardiotocography in 10 cases (14.2%) and severe pre-eclampsia in 5 cases (7%). Eleven cases (15.7%) had post-partum eclampsia after CS, six of them had their first fit after the cesarean; three had a previous ante-partum fit and one case had a previous intra-partum fit.
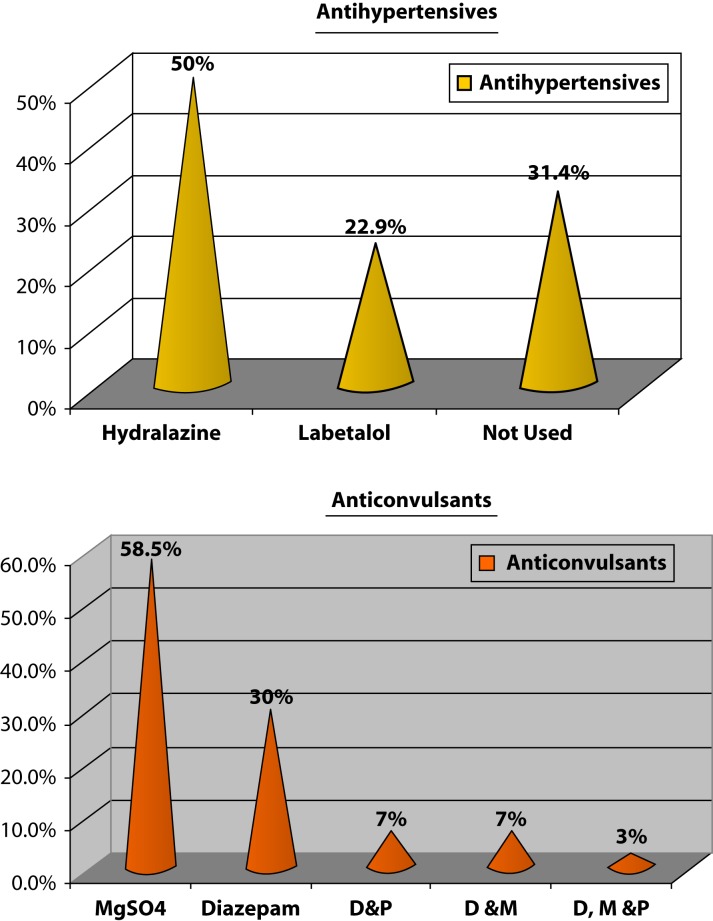
The medications used included anticonvulsants and anti-hypertensives. Forty-one cases (58.5%) of the women were given magnesium sulfate, 21 cases (30%) received diazepam, five cases (7%) diazepam and phenytoin, five cases (7%) used diazepam and magnesium sulfate and two cases (3%) diazepam, magnesium sulfate and phenytoin. The antihypertensives used were hydralazine in 35 cases (50%) and labetalol in 16 cases (22.9%). Antihypertensive therapy was not used in 22 cases (31.4%) of the women because their BP was normal or mildly elevated (Figure 6). Recurrent fits occurred in 17 cases (24.3%), 12 of them received diazepam.
Figure 6.
Medication used D&P = Diazepam&Phenytoin; D&M = Diazepam&MgSO4; D,M &P = Diazepam, MgSO4 & Phenytoin.
All women were admitted to the high dependency area at the Women's Hospital or intensive care unit (ICU) in Al Khor Hospital, with multidisciplinary care as required. There was one maternal mortality during the 19-year study period. The maternal mortality case was for a gravida 4 para 3 Pakistani woman who presented with sever pre-eclampsia at 32 weeks gestation, had one intra-partum fit and delivered by cesarean section for non-reassuring cardiotocography. She was complicated by severe HELLP (haemolysis, elevated liver enzymes and low platelets) syndrome and massive cerebrovascular accident (CVA). The patient had no antenatal care, and her baby was delivered with an Abgar score of 8 and 10 in the first and fifth minute, respectively, but admitted to the neonatal intensive care unit (NICU) for low birth weight (LBW).
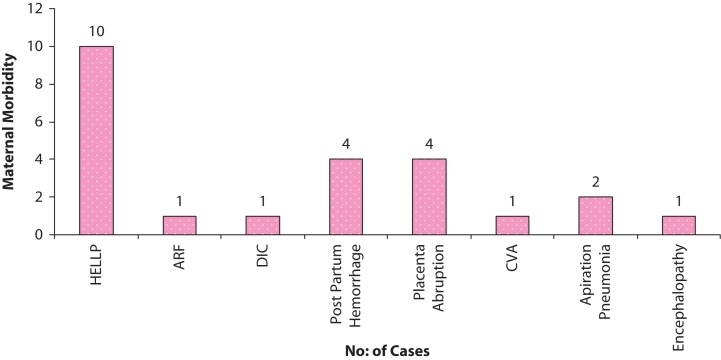
Maternal morbidity was present in 33% 8 cases, including 10 cases (14.3%) that were complicated by HELLP syndrome. One case involved acute renal failure (ARF), one case featured disseminated intravascular coagulation (DIC), four cases involved post-partum hemorrhage, four cases had placenta abruption, one case had CVA, two cases had aspiration pneumonia and one case had encephalopathy. All of these complications were reversible except for the CVA case, which needed rehabilitation for a long time. Fifteen women (21.5%) fell into a coma and post-eclamptic fits, but these were not prolonged and saw no focal neurological signs (Figure 7).
Figure 7.
Maternal morbidity
The perinatal outcome included a perinatal mortality of nine cases (13%). Six of them were stillbirths, one infant died in less than 24 hour of birth, two infants died less than 48 hour of birth. The still birth rate (SB) was 0.026/1000 total births and the perinatal mortality rate (PNM) was 12.8%. These are shown in Table 2.
Table 2.
Perinatal Mortality.
| GA/WEEKS | WT./GMS | TIMING OF DEATH | MODE OF DELIVERY | CAUSE OF DEATH |
| 24 | 470 | Stillbirth | C/S-Eclampsia | Eclampsia-hypoxia |
|
| ||||
| 25 | 550 | Stillbirth | Vaginal | Eclampia,hypoxia |
|
| ||||
| 27 | 640 | Stillbirth | Assisted breech delivery | Eclampsia-hypoxia |
|
| ||||
| 28 | 980 | Stillbirth | C/S-severe PE | Abruption |
|
| ||||
| 29 | 754 | < 24 hours | Vaginal | LBW,RDS |
|
| ||||
| 35 | 2500 | 48 hours | C/S-Eclampsia | Asphyxia |
|
| ||||
| 37 | 3140 | Stillbirth | Vacuum extraction | Abruption |
|
| ||||
| 38 | 1800 | 48 hours | C/S for non reassuring CTG | IUGR, Asphyxia |
|
| ||||
| 39 | 3690 | Stillbirth | Vaginal | abruption |
LBW: Low Birth Weight. RDS: Respiratory Distress syndrome. IUGR: Intrauterine growth restriction.
Low birth weight (LBW of < 2.5 Kg) was found in 48.6% of the cases34 all were admitted to the neonatal intensive care unit (NICU). Four more cases were admitted to NICU for other reasons (RDS, IUGR).
Discussion
The incidence of eclampsia in Qatar is low, 0.31/1000 deliveries. Similar incidence was reported in Canada-Nova Scotia, of about 0.27/1000 deliveries. 9
The incidence is stable in the UK and developed countries, about 0.4–0.5/1000 deliveries. 5 It was reported to be significantly higher in developing countries to reach 0.6–10/1000 deliveries. 6,10
Most of our eclamptic women were primiparous (46 cases 65.7%), the same was reported by Rosalyn et al. & Warden et al. in 2002. 11,12
Of the studied patients, 54.2% were 25 years old and 18.5% were teenagers—66.9% teenage eclamptics was reported by others. 10
Twenty-one cases (30%) did not have any antenatal visits, and 49 women (70%) had antenatal visits; 69.2% of unbooked eclampsia was reported by El Nafaty. 10
Thirty-one cases (44.2%) of eclampsia was ante-partum and 22 cases (31.4%) were postpartum. This was similar to what was reported earlier in the UK. 5 Lower post partum eclampsia was reported earlier (26%) by Lee et al. in 2004, and 10.6% by El Nafaty. 9,10
The majority of post-partum eclampsia (22 cases) had their first fit within 2 to 72 hour post-partum, 75% post vaginal delivery and 25% post CS. This was similar to what was reported by Douglas & Redman. 5 Twenty-seven women (38.6%) had severe pre-eclampsia, and magnesium sulfate prophylaxis was not used except for in two cases.
Pre-eclmapsia was present in 27 cases (38.5%) of eclamptic cases and severe pre-eclampsia complicated nearly half of the cases of eclampsia. Severe PE was reported to complicate 33.8% of the cases of eclampsia in Nigeria, 10 and 88.8% was reported by Onwuhafua et al. 13
Hydralazine or labetalol were the antihypertensives used in cases of severe PE. Most investigators recommend aggressive antihypertensive therapy for sustained diastolic pressures of 105–110 mmHg or higher and systolic BP of 160 mmHg or higher. 14
Two cases (3%) of cerebrovascular accident (CVA) were reported in our series; one of them ended by maternal death. Cerebrovascular accident accounts for 15–20% of deaths in eclampsia and correlates directly to the degree of BP elevation. 15 Anti-hypertensives were not used in 22 cases (31.4%) of our series, being that they were normotensives or had mild PE. The use of antihypertensive agents to control mildly elevated BP in the setting of PE did not show any alteration in the course of the disease nor did it diminish perinatal mortality (PNM) or morbidity. 16–18 Nine eclamptic women (12.8%) were normotensives with no protein detected in urine. Coetzee et al. reported in 1998 that non-proteinuric hypertension complicated only 0.1% of cases of eclampsia. 19
Symptoms of impending eclampsia were present in only 16 cases (22.9%), which made prediction and prevention difficult. The majority of eclamptic women had one or more antecedent symptom in the hours prior to an eclamptic fit, such as prodromal headache, visual disturbances or epigastric pain. 5,10
Forty-five cases (64%) of our series had CS, and the rest delivered vaginally, of which seven cases (10%) delivered by vacuum extraction. Lower CS rates were reported by El Nafaty. 10 Higher CS rates were reported (79%) by Lee et al. 9 Most CS were done due to eclampsia, unfavorable cervix and time ahead of term. We had only five inductions of labour for antepartum eclampsia. One needed CS for nonreassuring CTG. The rest delivered vaginally. Cervical ripening agents can be used to induce labour although less than one-third of women will successfully deliver vaginally, and long inductions should be avoided. 20,21
The anticonvulsant used was Magnesium Sulfate in 46 cases (58.5%) and Diazepam in 21 cases (30%). Recurrent fits were present in 17 cases (24.3%), 12 of them were given diazepam (17.19%), and three patients experienced recurrent fits while using magnesium sulfate. The drug of choice for the prevention of subsequent fits is magnesium sulfate, which is superior to diazepam and phenytoin with no significant differences in maternal or PNM. 22–24 Additional advantages of magnesium dulfate include safety, low cost, ease of administration and reduced sedation than with diazepam and phenytoin. It also increases cerebral blood flow and oxygen consumption in women with pre-eclampsia. 8 Therefore, magnesium sulfate appears to be substantially more effective than diazepam and phenytoin for the treatment of eclampsia. 25,26
Only 23 women (33%) in our series had major maternal complications including HELLP syndrome, DIC, ARF and CVA. They were all managed conservatively and were reversible except for the cases of CVA, in which one patient expired and the other needed rehabilitation. This indicated our relatively good high dependence area care and multidisciplinary involvement.
Maternal mortality and severe morbidity are lowest among women receiving regular prenatal care, managed by an experienced physician in tertiary centers. 27,28 Maternal complications were reported to be higher (32%) in Nova Scotia by Lee et al. 9 , and 70% by Lopez-Lleera 29 such as DIC, HELLP syndrome, ARF, CVA, hepatocelular injury and cardio-respiratory arrest. 9,29 There was one maternal death in our series due to a massive CVA and HELLP syndrome. Maternal mortality rate was thus reported to be 0.14%. 5,10,29
The most common cause of death was reported to be cerebral hemorrhage and cerebral venous thrombosis in autopsy of eclamptic mortalities. 30 The perinatal mortality was reported in our series to be 12.8% (9 cases). This result is better than that reported in developed countries. 9 The PNM was reported to be up to 14% in the US and UK. 5,10,29 The main cause of PNM was prematurity and LBW (46.6%) and intrauterine fetal death in 50% of cases. Similar reasons were reported by others. 10
Severe PE complicated 20% of our cases, magnesium sulfate was only used for prophylaxis in two cases. Anticonvulsant therapy should be administered to prevent a first seizure in women with severe PE. 19,31,32
The Magpie Trial (magnesium sulfate for prevention of eclampsia trial—a randomized placebo-controlled trial-published in 2002) concluded that magnesium sulfate significantly reduced the risk of eclamptic convulsions in pre-eclampsia. To prevent one convulsion, 63 women with severe PE and 109 women with mild PE would need to be treated. This was associated with reduction in the rate of maternal mortality.33 Magnesium sulfate is the anticonvulsant of choice as it is more effective than phenytoin and diazepam for the prevention and treatment of eclampsia. 23–26 33
The World Health Organization (WHO), The American College of Obstetricians & Gynecologists (ACOG), The Royal College of Obstetricians & Gynecologists (RCOG), Federation Internationale de Gynecologie et de Obstetrique, and The International Society for the Study of Hypertension in Pregnancy recommend the use of magnesium sulfate for prevention and treatment of eclampsia.
Among the subjects in our study, 30% did not have any antenatal visits before. A higher percentage (69.2%) was reported earlier. 10 Community-based approaches to improve community health, education and prenatal care is required. Counseling women about the recurrence risk of sever PE and eclampsia and encourage early and regular antenatal care all can be effective measures for the prevention of eclampsia.
Auditing can ensure the safe and effective introduction of seizure prophylaxis with magnesium sulfate in obstetric practice.34 Eclampsia drills (on site stimulation, evidence based eclampsia management protocols, eclampsia boxes, individual staff feedback and education) can identify and correct potential deficiencies in the care of eclamptic patients due to the infrequency of the condition.35 Still, many cases of eclampsia appear not to be preventable even among women receiving regular antenatal care, which can be due to the abrupt onset and late post-partum onset.36
Conclusion
Eclampsia is a rare obstetric complication in Qatar and it is associated with a slight increase in maternal morbidity, and the vast majority of cases were completely reversible. Perinatal morbidity was also increased, which was mainly related to prematurity and LBW.
Eclampsia cannot be completely prevented but can be minimized by improvement in obstetric care through having a high index of suspicion even in low-risk patients and initiation of seizure prophylaxis by magnesium sulfate for all cases of sever PE, together with community-based approaches to improve health and education. The use of hospital-based audit and eclampsia drills may improve level of care.
References
- 1.Department of health, Welsh Office, Scotish home and health department, Department of health and Social services Northern Ireland. Why Mothers die. Report on Confidential Enquiry into maternal deaths in the United Kingdom. 1997-1999. London: HMSO; 2000. [Google Scholar]
- 2.Rochat RW, Koonin LM, Atrash HK, Jewett JF. Maternal mortality in the /United states: report from the maternal mortality collaborative. Obstet Gynecol. 1988;72(1):91–97. [PubMed] [Google Scholar]
- 3.Duley L. Maternal Mortality associated with hypertensive disorders of pregnancy in Africa, Asia, Latin America & the Caibbean. Br J Obstet Gynaecol. 1992;99(7):547–553. doi: 10.1111/j.1471-0528.1992.tb13818.x. [DOI] [PubMed] [Google Scholar]
- 4.Cowther C. Magnesium Sulphate versus diazepam in the management of eclampsia: A randomized controlled trial. Br J Obstet Gynaecol. 1990;97:110–117. doi: 10.1111/j.1471-0528.1990.tb01735.x. [DOI] [PubMed] [Google Scholar]
- 5.Douglas KA, Redman CW. Eclampsia in the United Kingdom. BMJ. 1994;309:1395. doi: 10.1136/bmj.309.6966.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geographic variation in the incidence of hypertension in pregnancy. World Health Organization International Collaborative Study of Hypertensive Disorders of Pregnancy. Am J Obstet Gynecol. 1988;158:80–83. [PubMed] [Google Scholar]
- 7.Morriss MC, Twickler DM, Hatab MR, Clarke GD, Peshock RM, Cunningham FG. Cerebral blood flow and cranial magnetic resonance imaging in eclampsia and severe preeclampsia. Obstet Gynecol. 1997;89(4):561–568. doi: 10.1016/s0029-7844(97)00048-3. [DOI] [PubMed] [Google Scholar]
- 8.Belfort MA, Moise KJ., Jr Effect of magnesium sulfate on maternal brain blood flow in preeclampsia: a randomized, placebo-controlled study. Am J Obstet Gynecol. 1992;167(3):661–666. doi: 10.1016/s0002-9378(11)91567-1. [DOI] [PubMed] [Google Scholar]
- 9.Lee W, O'Connell CM, Baskett TF. Maternal & Perinatal Outcomes of Eclampsia: Nova Scotia 1981-2000. J Obstet Gynecol Can. 2004;26(2):119–123. doi: 10.1016/s1701-2163(16)30487-x. [DOI] [PubMed] [Google Scholar]
- 10.El Nafaty AU, Melah GS, Massa AA, Audu BM, Nelda M. The analysis of eclamptic Morbidity and Mortality in the Specialist Hospital Gombe, Nigeria. J Obstet gynaecol. 2004;24(2):142–147. doi: 10.1080/01443610410001645415. [DOI] [PubMed] [Google Scholar]
- 11.Rasaly S, Carson-Dewitt . Gale Encyclopedia of Medicine. Pre-eclampsia & eclampsia; pp. 23–40. [Google Scholar]
- 12. Warden M & Euerle B. Pre eclampsia (Toxaemia of pregnancy) emergency Medicine 2003, Updated on April 5 2002.
- 13. On Wuhafua.
- 14.Working group report on high blood pressure in pregnancy. Washington, DC: National Institutes of Health; 2000. [Google Scholar]
- 15.Lewingston S, Clarke R, Qizilbash N et al. Age specific relevance of usual blood pressure on stroke risk:a prospective observational study. Am J Epidemiol. 1995;142:1279. doi: 10.1093/oxfordjournals.aje.a117595. [DOI] [PubMed] [Google Scholar]
- 16.Sibai BM. Treatment of hypertension in pregnant women. N Engl J Med. 1996;335:257. doi: 10.1056/NEJM199607253350407. [DOI] [PubMed] [Google Scholar]
- 17.Von Dadelszen P, Ornstein MP, Bull SB et al. Fall in mean arterial pressure and fetal growth restriction in pregnancy hypertension: a meta-analysis. Lancet. 2000;355:87. doi: 10.1016/s0140-6736(98)08049-0. [DOI] [PubMed] [Google Scholar]
- 18.Magee LA, Ornstein MP, von Dadelszen P. Fortnightly review: management of hypertension in pregnancy. BMJ. 1999;318:1332. doi: 10.1136/bmj.318.7194.1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coetzee EJ, Dommisse J, Anthony T. A randomized controlled trial of intravenous magnesium sulhate versus placenbo in the management of women with severe pre eclampsia. Br J Obstet Gynaecol. 1998;105:300. doi: 10.1111/j.1471-0528.1998.tb10090.x. [DOI] [PubMed] [Google Scholar]
- 20.Alexander JM, Bloom SL, McIntire DD, Leveno KJ. Severe preeclampsia and the very low birth weight infant: is induction of labor harmful? Obstet Gynecol. 1999;93:485. doi: 10.1016/s0029-7844(98)00488-8. [DOI] [PubMed] [Google Scholar]
- 21.Nassar AH, Adra AM, Chakhtoura N, Gómez-Marín O, Beydoun S. Severe preeclampsia remote from term: labor induction or elective cesarean delivery? Am J Obstet Gynecol. 1998;179(5):1210–1213. doi: 10.1016/s0002-9378(98)70133-4. [DOI] [PubMed] [Google Scholar]
- 22.Which anticonvulsant for women with eclampsia? Evidence from the Collaborative Eclampsia Trial. Lancet. 1995;345:1455–1463. [PubMed] [Google Scholar]
- 23.Duley L, Henderson-Smart D. Magnesium sulphate versus diazepam for eclampsia. (Cochrane Library, issue 3, 2001.Oxford: update software) [Google Scholar]
- 24.Duley L, Henderson-Smart D. Magnesium sulphate versus phenytoin for eclampsia. (Cochrane Review). In Cochrane Library, issue 3, 2001.Oxford: update software. [Google Scholar]
- 25.Duley L, Henderson-Smart D. Magnesium sulphate versus diazepam for eclampsia. Cochrane Database Syst Rev. 2003;(4):CD000127. doi: 10.1002/14651858.CD000127. [DOI] [PubMed] [Google Scholar]
- 26.Duley L, Henderson-Smart D. Magnesium sulphate versus phenytoin for eclampsia. Cochrane Database Syst Rev. 2003;(4):CD000128. doi: 10.1002/14651858.CD000128. [DOI] [PubMed] [Google Scholar]
- 27.Sibai BM. Eclampsia. VI. Maternal-perinatal outcome in 254 consecutive cases. Am J Obstet Gynecol. 1990;163(3):1049–1054. doi: 10.1016/0002-9378(90)91123-t. [DOI] [PubMed] [Google Scholar]
- 28.Conde-Agudelo A, Kafury-Goeta AC. Case-control study of risk factors for complicated eclampsia. Obstet Gynecol. 1997;90(2):172–175. doi: 10.1016/S0029-7844(97)00219-6. [DOI] [PubMed] [Google Scholar]
- 29.López-Liera M. Main clinical types and subtypes of eclampsia. Am J Obstet Gynecol. 1992;166(1 Pt 1):4–9. doi: 10.1016/0002-9378(92)91816-s. [DOI] [PubMed] [Google Scholar]
- 30.Sheehan HL, Lynch JB. Pathology of toxaemia of pregnancy. Baltimore: Williams &Wilkins; 1973. [Google Scholar]
- 31.Robert JM, Villar J, Aruikumaran S. Peventing & treating eclamptic seizures. BMJ. 2002;325:609. doi: 10.1136/bmj.325.7365.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Diagnosis and management of preeclampsia and eclampsia. ACOG practice bulletin #33, American College of Obstetricians and Gynecologists, January 2002.