Abstract
Background.
Low muscle mass and weakness are common and potentially disabling in older adults, but in order to become recognized as a clinical condition, criteria for diagnosis should be based on clinically relevant thresholds and independently validated. The Foundation for the National Institutes of Health Biomarkers Consortium Sarcopenia Project used an evidence-based approach to develop these criteria. Initial findings were presented at a conference in May 2012, which generated recommendations that guided additional analyses to determine final recommended criteria. Details of the Project and its findings are presented in four accompanying manuscripts.
Methods.
The Foundation for the National Institutes of Health Sarcopenia Project used data from nine sources of community-dwelling older persons: Age, Gene/Environment Susceptibility-Reykjavik Study, Boston Puerto Rican Health Study, a series of six clinical trials, Framingham Heart Study, Health, Aging, and Body Composition, Invecchiare in Chianti, Osteoporotic Fractures in Men Study, Rancho Bernardo Study, and Study of Osteoporotic Fractures. Feedback from conference attendees was obtained via surveys and breakout groups.
Results.
The pooled sample included 26,625 participants (57% women, mean age in men 75.2 [±6.1 SD] and in women 78.6 [±5.9] years). Conference attendees emphasized the importance of evaluating the influence of body mass on cutpoints. Based on the analyses presented in this series, the final recommended cutpoints for weakness are grip strength <26kg for men and <16kg for women, and for low lean mass, appendicular lean mass adjusted for body mass index <0.789 for men and <0.512 for women.
Conclusions.
These evidence-based cutpoints, based on a large and diverse population, may help identify participants for clinical trials and should be evaluated among populations with high rates of functional limitations.
Key Words: Aging, Sarcopenia, Muscle, Outcomes, Weakness.
The term “sarcopenia” originally referred solely to the loss of muscle mass with age, and as such, is an almost universal phenomenon (1,2). Although the term “sarcopenia” has become widely used in the literature, definitions vary, due to greater insights into the relationships between muscle mass, muscle quality, muscle strength, and function. Recent literature suggests that the role of muscle mass in function and health appears to be indirect. Although not entirely consistent, the weight of evidence in community-dwelling older adults suggests that (i) low muscle mass is associated with weakness (3), (ii) weakness (now often referred to as “dynapenia”) (4) is strongly associated with function and disability (5,6), but (iii) low muscle mass alone is weakly or not associated with function and disability (7,8). Because of these findings, current “sarcopenia” definitions incorporate not only muscle mass but also elements such as strength and function.
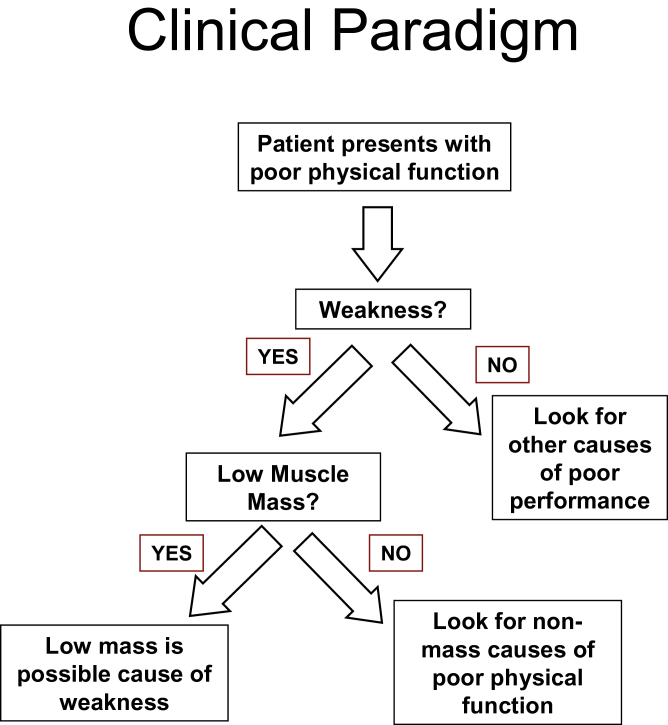
It is clear that we can no longer assume that there is a direct and strong causal pathway from mass to strength to function. On the other hand, there does appear to be a population of adults who have functional limitations because they are weak, and they are weak in part because they have low muscle mass. One conceptual and analytic strategy to identify this population is to take the approach of a clinician making a “differential diagnosis.” The clinician understands that there are many causes of reduced physical function, one of which is weakness. Similarly, low lean mass, an indicator of muscle mass based on imaging, may be considered one of many contributing factors in the development of weakness (Figure 1). Thus, it would be reasonable to identify individuals with low lean mass contributing to weakness because these individuals may benefit from interventions that are specifically designed to address muscle mass. Persons without low muscle mass as a cause of their weakness may require different interventions.
Figure 1.
Clinical paradigm.
The original criteria for low lean mass, which have largely been carried forward into all proposed definitions, were based on distributional characteristics in modest sized populations, rather than on potential clinical relevance in large, diverse populations. Thus, a key gap in knowledge remains: What degree of low lean mass is clinically relevant, when it is empirically grounded to its relationship to strength and function?
To determine critical thresholds for low lean mass that are based on its relationship to strength and function, the Foundation for the National Institutes of Health (FNIH) Biomarkers Consortium, a public–private partnership composed of representatives from the National Institute of Aging, National Institute of Arthritis and Musculoskeletal and Skin Diseases, Center for Drug Evaluation and Research/Food and Drug Administration, several prominent academic institutions, and six pharmaceutical companies, approved support for an initiative entitled, “The FNIH Sarcopenia Project.” The project’s goal was to use multiple existing data sources to identify criteria for clinically relevant weakness and low lean mass. In 2009, the FNIH released a Request for Proposals (RFP) to participate in a Consortium that would address the following major goals: using mobility impairment as the clinically relevant state of function (i) define a clinically relevant degree of muscle weakness; (ii) define a clinically relevant degree of low lean mass associated with muscle weakness; (iii) determine, among those without current mobility limitations, whether these weakness and low lean mass criteria predict future mobility limitations; and (iv) compare these criteria for weakness and low lean mass to other proposed criteria. The Request for Proposals eligibility requirements included: (i) existing data set; (ii) longitudinal cohort or clinical trial study design with data at a minimum of two time points; (iii) inclusion of older adults; (iv) available measures of body composition, strength, and physical performance; and (v) willingness to share data and analysis plans with other investigators. Investigators from nine sets of studies participated in an initial planning meeting in March 2010, where they agreed to: (i) use mobility impairment, assessed by physical performance measures, as the criterion for a clinical state of physical function that is relevant to muscle; (ii) define mobility impairment from clinically relevant thresholds of physical performance tests such as slow walking or inability to rise from a chair; and (iii) apply clinically relevant analytic strategies, including classification and regression tree analysis and receiver operating characteristic curves. At a later time, a decision was made to increase statistical power by pooling the original data rather than meta-analyze individual study results. Finally, due to current confusion related to the meaning of the word “sarcopenia,” we decided to avoid using the term itself and consistently employ only the terms “low lean mass” and “weakness.”
A key step in the process of developing these criteria was to obtain feedback on preliminary findings of the FNIH Sarcopenia Project from representatives from academia, professional organizations, government, and the private sector who have an interest in the area of aging and muscle. Therefore, a conference was held in May 2012 to elicit priorities and perspectives, provide feedback on the progress of the FNIH Sarcopenia Project team, and make recommendations for next steps. This manuscript summarizes the findings from the Conference, the results of final analyses, and identifies key next steps.
The purpose of this first manuscript of a set of five, derived from the work of the FNIH Sarcopenia Project, is twofold. First, to present the characteristics of the participating studies, including study design, sample size, demographics, baseline status of key indicators of physical function, strength, and body composition, and additional indicators of health and disease. Second, we summarize the recommendations from the Conference that led to the final set of analyses presented in this series of articles. The second manuscript in the series focuses on developing clinically relevant criteria for weakness based on grip strength (9); the third on criteria for low muscle mass (10); the fourth on longitudinal predictions based on the weakness and muscle mass criteria (11); and the fifth presents comparisons between the FNIH Project findings and previously published operational definitions for sarcopenia (12). We hope that these findings can support further development of a robust and well-validated clinical definition of “sarcopenia” that would aid in critical appraisal of existing literature, help guide eligibility and measurement in future studies, support the assessment of interventions, either as a target group for treatment or as part of an endpoint, and eventually be used to help develop diagnostic criteria and indications for clinical treatments in practice.
Methods
Overview
This Methods section has two goals; our first goal is to present the study design, population sample, and key measures from the nine participating studies. Because the goals of the cross-sectional analyses required that there be sufficient cases of mobility impairment, for some cohorts, we selected a wave and study time point that optimized the prevalence of mobility impairment and sample size. Our second goal is to summarize the methods we used to obtain feedback during the conference in May 2012.
For the purpose of defining our primary outcome, mobility impairment, we selected a usual gait speed ≤ 0.8 m/s because it predicts reduced overall survival (13), disability (14), and has been recommended by other experts (15). In addition, we planned sensitivity analyses using other cutpoints for gait speed (0.6 and 1.0 m/s). We considered inability to rise from a chair as an alternate definition of mobility impairment because it is potentially more strongly related to muscle strength compared with gait speed and has also been recommended by expert panels (15). Grip strength was used as the primary measure of muscle strength because it was widely available in all nine studies, whereas lower extremity strength measures varied greatly and were available in only a few studies. Written informed consent had been obtained from each participant and each study was approved by the institutional review boards at each institution.
Collaborating Studies
Age, Gene/Environment Susceptibility-Reykjavik Study.
In 2002–2006, adults aged ≥65 years who originally participated in the Reykjavik Study (1967–1997) were recruited to participate in an interdisciplinary genetic epidemiology study of the musculoskeletal, body composition, neurocognitive, and vascular systems including assessment of function by both self-report and performance (16). The objective of the study was to identify shared biological pathways for disease and to test gene–environment interactions. Participants were seen approximately 5 years later in 2007–2011 for follow-up. Data on body composition and/or physical performance from the baseline visit were available in 5,764 participants (2,438 men and 3,326 women).
Boston Puerto Rican Health Study.
In 2004–2007, 1,505 men and women aged 45–75 years and living in Massachusetts were recruited to examine the relationships between life stressors and physical and psychosocial health (17). Data on body composition and/or physical performance from the baseline visit were available in 249 participants (63 men and 186 women) aged ≥65 years.
Clinical Trials.
This study included data from six different clinical trials conducted at the University of Connecticut. Recruitment and enrollment criteria varied. Participants were randomized to active or placebo group with various interventions including testosterone, estradiol, omega-3, exercise, and dehydroepiandrosterone with Yoga or aerobics (18–23). The study duration ranged between 6 and 36 months. Data on body composition and/or physical performance from the randomization visits were available in 651 participants (184 men and 467 women).
Framingham Heart Study.
In 1948, the Framingham Heart Study (FHS) Original cohort recruited two thirds of the population sample from Framingham, Massachusetts, to evaluate risk factors of heart disease (24). In 1971, adult children of the FHS Original cohort were recruited to the FHS Offspring cohort to understand familial risk factors of heart disease (25). This study includes data from the FHS Original cohort and FHS Offspring cohort. Participants were seen at 2- to 4-year intervals. Data on body composition and/or physical performance were available in 469 participants (151 men and 318 women) from the FHS Original cohort (exam cycle 22, 1992–1993) and in 1,175 participants (558 men and 617 women) from the FHS Offspring cohort (exam cycle 6 and 7, 1996–2001).
Health, Aging, and Body Composition Study.
In 1997–1998, 3,075 men and women aged 70–79 years who reported no difficulty walking 0.25 mile and climbing a flight of stairs and were free of disability in activities of daily living were recruited at two clinical centers (Memphis, Tennessee and Pittsburgh, Pennsylvania) to evaluate whether change in body composition is a common pathway contributing to disability (26). The study oversampled for African Americans and was 42% black and 48% men. Participants were seen yearly for the first 6 years and then every other year until the 10th year with continuing follow-up by examination and phone contact. Because the FNIH Sarcopenia Project focused on more disabled older adults, data at Year 6 for 2,580 participants (1,198 men and 1,382 women) aged 76–85 were utilized as the baseline in these analyses.
Invecchiare in Chianti.
In 1998–1999, 1,154 men and women aged 65 and older were recruited from population-based registries in two Italian towns (Bagno a Ripoli in Tuscany and Greve in Chianti) to study subsystems affecting walking ability (27). The study oversampled for adults aged 90+. In 2001–2002, 836 participants (365 men and 471 women) aged ≥68 years were followed up and had data on body composition and/or physical performance were used for these analyses.
Osteoporotic Fractures in Men Study.
In 2000–2002, 5,994 men who were aged ≥65 years, able to walk independently, and did not report bilateral hip replacements were recruited at six U.S. clinical centers (Birmingham, Alabama; Minneapolis, Minnesota; Palo Alto, California; Monongahela Valley, near Pittsburgh, Pennsylvania; Portland, Oregon; and San Diego, California) to evaluate the epidemiology of osteoporosis and fractures (28,29). In clinic follow-up visits occurred approximately every 2–3 years. Data on body composition and/or physical performance from the baseline visit were available in 5,993 men.
Rancho Bernardo Study.
In 1972, 6,728 men and women aged 30–79 years were recruited from a southern California community (Rancho Bernardo, California) to evaluate the risk factors for heart disease (30). Starting in 1988, participants returned to clinic every 4 years for body composition and physical performance assessments. Data on body composition and/or physical performance from exam cycle 7, 1992–1996, were available in 1,238 participants (477 men and 761 women).
Study of Osteoporotic Fractures.
In 1986–1988, 9,704 white women aged ≥65 years were recruited at four U.S. clinical centers (Baltimore, Maryland; Portland, Oregon; Pittsburgh, Pennsylvania; and Minneapolis, Minnesota) to evaluate the epidemiology of osteoporosis and fractures (31). Recruitment was initially limited to white women due to low incidence of fractures in other populations. In 1997–1998, 662 African American women were additionally recruited (32). Participants returned to clinic every 2–3 years for repeat assessments. Data on body composition and/or physical performance were available in 7,008 white women from Visit 6 and 662 African American women from Visit 1 for these analyses.
Measures
Physical performance and strength.
Gait speed was defined as the length of the walking course divided by the time it took subjects to walk the course at their usual pace. If more than one walking test was administered, the average gait speed (m/s) was used. Except for the Boston Puerto Rican Health Study (BPRHS) and Clinical Trials studies, the walking courses were 4 or 6 m long and were considered equivalent. Walking courses that were longer or shorter were converted to a speed that would have been achieved on a 4- or 6-m course using previously published equations (33). Gait speed was not measured in Rancho Bernardo. Participants were asked to rise once from a standard chair without using their arms. If able to rise once successfully, participants were then asked to complete five chair stands and the time to complete the chair stands was recorded in seconds. Chair stand was not measured in Age, Gene/Environment Susceptibility-Reykjavik Study. Grip strength was measured by a handheld dynamometer, and the maximum value from either hand was analyzed. Most studies used a Jamar dynamometer (Sammons Preston Rolyan, Bolingbrook, IL) (34).
Body composition.
Total body fat mass and total bone-free lean mass (kg) were acquired from total body scans using fan-beamed dual-energy x-ray absorptiometry (Hologic, Waltham, MA or Lunar, Madison, WI) using standardized protocols (35,36). Appendicular lean mass (ALM) was the sum of lean mass from both arms and legs. Participants missing lean mass measurements for an arm or leg were excluded. The validity and reproducibility of dual-energy x-ray absorptiometry have been reported previously. In Invecchiare in Chianti, body composition was measured using peripheral quantitative computed tomography of the calf. For Invecchiare in Chianti, estimated ALM was available only in men and was derived from equations from Osteoporotic Fractures in Men Study that included height, weight, waist circumference, fat area, muscle area, and muscle density. In Age, Gene/Environment Susceptibility-Reykjavik Study, body composition was measured with bioelectrical impedance (Xitron Hydra ECF/ICF Bio-Impedance Spectrum Analyzer).
Covariates.
Height (cm) was measured on Harpenden stadiometers and weight (kg) was measured on standard balance beam or digital scales using standard protocols with participants wearing light clothing without shoes. Body mass index was calculated as weight divided by height2 (kg/m2). Chronic diseases including diabetes, congestive heart failure, chronic obstructive pulmonary disease, and cancer were collected where possible. The definition of these diseases was study specific and dichotomized as present or absent.
The FNIH Conference.
The three and a half day conference began with an overview of the issues and perspectives of experts from organizations with an interest in aging and muscle. Subsequent sessions presented participant characteristics of the studies that contributed data to the pooled analyses, the rationale and methodological approaches to analyses, preliminary cutpoints for clinically relevant weakness and low lean mass, and their predictive validity. After that, breakout groups and panels commented on strengths, limitations, and need for further work based on these preliminary findings. On the last day, panels addressed unresolved issues related to clinical trial design to test novel agents that have the potential to benefit older persons with weakness and low lean mass. Also, representatives from professional organizations provided feedback and recommendations. Conference attendees were asked to respond to a survey regarding level of agreement with key statements related to the work of the FNIH Project. The conference agenda and key presentations can be found at http://biomarkersconsortium.org/sarcopenia_pdfs.html.
Statistical Analysis
We present descriptive analyses for categorical and continuous variables. All descriptions and subsequent analyses are presented separately by gender because body composition and strength differ greatly by gender.
Results
A total of 30,772 participants participated in the nine sets of studies. However, 3,633 were <65 years old and 515 participants with inaccurately measured gait speed were excluded, leaving 26,625 participants (11,427 men and 15,198 women) who were included the pooled data sample.
Baseline characteristics by gender and study are shown in Tables 1 and 2. The average age was 75.2 (±6.1 SD) and 78.6 (±5.9) years for men and women, respectively. Men had a higher prevalence of diabetes and cancer than women. The prevalence of obesity was high in both genders, although men were on average heavier than women. Men had greater lean mass (both appendicular and leg) and grip strength, walked faster, and completed the five chair stands faster. About 5% men and 10% women were unable to rise from a chair without the use of their arms. Of the participants with gait speed measurements, 10% of men and 31% of women had gait speed ≤ 0.8 m/s.
Table 1.
Baseline Characteristics by Study for Men
| MrOS | InChianti | RCT | BPRHS | RBS | FHS Orig | FHS Off | AGES | HABC | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| N = 5,993 | N = 365 | N = 184 | N = 63 | N = 477 | N = 151 | N = 558 | N = 2,438 | N = 1,198 | N = 11,427 | |
| Age, y | 73.7±5.9 | 76.1±6.7 | 77.4±5.9 | 70.0±3.6 | 77.0±6.8 | 85.0±3.5 | 71.1±4.6 | 77.0±5.7 | 78.6±2.9 | 75.2±6.1 |
| Weight, kg | 83.2±13.3 | 73.1±11.3 | 79.5±13.6 | 84.3±17.9 | 77.9±11.7 | 75.9±11.7 | 82.6±16.0 | 82.6±13.4 | 80.3±13.4 | 82.1±13.5 |
| Height, m | 1.7±0.1 | 1.7±0.1 | 1.7±0.1 | 1.7±0.1 | 1.7±0.1 | 1.7±0.1 | 1.7±0.1 | 1.8±0.1 | 1.7±0.1 | 1.7±0.1 |
| White race, % | 89.8 | 100 | 98.4 | N/A | 100 | 100 | 100 | 100 | 66.1 | 90.5 |
| BMI, kg/m2 | 27.4±3.8 | 26.0±3.2 | 26.6±3.8 | 31.0±6.0 | 25.9±3.4 | 26.6±3.4 | 27.6±5.0 | 26.8±3.8 | 27.1±4.1 | 27.1±3.9 |
| BMI < 25, % | 27.4 | 36.8 | 35.3 | 11.8 | 45.1 | 32.5 | 25.3 | 32.8 | 29.8 | 29.9 |
| BMI 25 to <30, % | 51.2 | 53.2 | 46.7 | 38.2 | 45.5 | 51.0 | 47.5 | 48.5 | 49.5 | 50.0 |
| BMI ≥ 30, % | 21.4 | 10.0 | 17.9 | 50.0 | 9.5 | 16.6 | 27.3 | 18.8 | 20.7 | 20.2 |
| Walking speed, m/s | 1.3±0.2 | 1.1±0.3 | 1.0±0.2 | 0.7±0.2 | — | 0.8±0.2 | 1.1±0.2 | 1.0±0.2 | 1.1±0.3 | 1.2±0.3 |
| Walking speed ≤ 1.0 m/s, % | 14.4 | 35.6 | 45.1 | 96.6 | — | 83.3 | 48.8 | 56.2 | 27.2 | 28.7 |
| Walking speed ≤ 0.8 m/s, % | 3.7 | 13.5 | 19.8 | 78.0 | — | 45.5 | 12.1 | 20.3 | 8.5 | 9.7 |
| Walking speed ≤ 0.6 m/s, % | 0.8 | 5.9 | 6.2 | 25.4 | — | 8.3 | 0.3 | 4.6 | 2.0 | 2.2 |
| Grip strength, kg | 41.6±8.5 | 39.8±10.3 | 27.6±8.2 | 30.9±8.0 | 33.9±7.7 | 28.8±7.4 | 37.2±9.2 | 39.1±9.5 | 37.0±8.5 | 39.7±9.2 |
| Unable to rise from a chair, % | 2.7 | 14.6 | 3.2 | 6.8 | 0.8 | 19.9 | 7.0 | — | 12.0 | 5.1 |
| Five chair stand time, s | 11.1±3.3 | 11.3±3.5 | 13.8±5.3 | 12.0±3.2 | — | 16.5±5.2 | 12.4±3.2 | — | 14.6±4.2 | 11.7±3.7 |
| ALM, kg | 24.3±3.5 | 22.7±3.0 | 22.8±3.3 | 21.8±3.5 | 21.6±3.1 | — | 23.1±3.2 | 24.8±3.4 | 23.0±3.4 | 24.0±3.5 |
| ALM/ht2, kg/ht2 | 8.0±0.9 | 8.1±0.8 | 7.6±1.0 | 8.0±1.1 | 7.2±0.8 | — | 7.7±0.9 | 8.0±0.9 | 7.8±1.0 | 7.9±1.0 |
| LLM, kg | 17.8±2.5 | — | 16.5±2.4 | 15.5±2.7 | 16.0±2.3 | — | 16.5±2.2 | — | 16.6±2.5 | 17.4±2.6 |
| Diabetes, % | 10.9 | 15.9 | 10.6 | 46.8 | 8.7 | 21.0 | 18.7 | 16.8 | 22.8 | 12.2 |
| CHF, % | 5.3 | 13.4 | 37.4 | 12.7 | 4.8 | 10.6 | 2.9 | 6.4 | — | 6.4 |
| COPD, % | 10.7 | — | 4.5 | 30.2 | — | — | — | 3.2 | — | 8.6 |
| Cancer, % | 29.1 | 9.3 | 8.9 | 4.8 | 17.2 | — | — | 16.0 | 1.0 | 21.8 |
Notes: AGES = Age, Gene/Environment Susceptibility-Reykjavik Study; ALM = appendicular lean mass; ALM/ht2 = ratio of appendicular lean mass over height2; BMI = body mass index; BPRHS = Boston Puerto Rican Health Study; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; FHS = Framingham Heart Study; HABC = Health, Aging, and Body Composition Study; InChianti = Invecchiare in Chianti; LLM = leg lean mass; MrOS = Osteoporotic Fractures in Men Study; RBS = Rancho Bernardo Study; RCT = Clinical Trials. Data are presented as mean ± SD.
Table 2.
Baseline Characteristics by Study for Women
| SOF Whites | SOF AA | InChianti | RCT | BPRHS | RBS | FHS Orig | FHS Off | AGES | HABC | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 7,008 | N = 662 | N = 471 | N = 467 | N = 186 | N = 761 | N = 318 | N = 617 | N = 3,326 | N = 1,382 | N = 15,198 | |
| Age, y | 80.9±4.7 | 75.4±5.1 | 77.3±7.3 | 74.5±5.8 | 69.2±3.2 | 77.3±6.9 | 85.7±4.0 | 70.9±4.4 | 77.0±6.0 | 78.4±2.9 | 78.6±5.9 |
| Weight, kg | 65.5±12.9 | 76.2±16.4 | 64.6±11.5 | 67.9±13.1 | 74.7±16.4 | 61.8±11.0 | 61.8±12.8 | 68.4±15.6 | 70.1±13.3 | 68.9±14.7 | 67.5±13.8 |
| Height, m | 1.6±0.1 | 1.6±0.1 | 1.6±0.1 | 1.6±0.1 | 1.5±0.1 | 1.6±0.1 | 1.5±0.1 | 1.6±0.1 | 1.6±0.1 | 1.6±0.1 | 1.6±0.1 |
| White race, % | 100 | 0 | 100 | 83.9 | N/A | 100 | 100 | 100 | 100 | 55.7 | 89.9 |
| BMI, kg/m2 | 26.5±4.8 | 30.3±6.3 | 26.9±4.4 | 27.1±5.2 | 32.2±6.8 | 24.5±3.9 | 26.2±4.9 | 27.1±5.9 | 27.2±4.9 | 27.4±5.6 | 26.9±5.2 |
| BMI < 25, % | 42.4 | 20.3 | 36.8 | 40.1 | 10.4 | 60.9 | 43.4 | 38.5 | 34.5 | 36.6 | 39.2 |
| BMI 25 to <30, % | 36.2 | 32.6 | 41.2 | 34.6 | 33.9 | 30.7 | 37.4 | 34.9 | 40.6 | 34.6 | 36.7 |
| BMI ≥ 30, % | 21.4 | 47.1 | 21.5 | 25.3 | 55.7 | 8.4 | 19.2 | 26.6 | 24.9 | 28.8 | 24.1 |
| Walking speed, m/s | 0.9±0.2 | 0.8±0.2 | 0.9±0.3 | 1.0±0.2 | 0.7±0.2 | — | 0.7±0.21 | 1.1±0.2 | 0.9±0.2 | 1.0±0.3 | 0.9±0.2 |
| Walking speed ≤ 1.0 m/s, % | 70.1 | 80.3 | 60.9 | 39.8 | 83.9 | — | 91.5 | 58.5 | 68.1 | 44.2 | 66.5 |
| Walking speed ≤ 0.8 m/s, % | 33.6 | 41.6 | 30.4 | 12.3 | 82.1 | — | 63.0 | 14.2 | 29.0 | 17.9 | 31.0 |
| Walking speed ≤ 0.6 m/s, % | 12.6 | 13.9 | 12.7 | 2.4 | 38.5 | — | 28.1 | 0.8 | 7.6 | 5.2 | 10.5 |
| Grip strength, kg | 18.6±4.5 | 21.9±5.3 | 23.7±6.5 | 18.2±6.1 | 18.5±5.2 | 18.3±5.0 | 15.8±4.9 | 20.5±6.8 | 23.6±5.9 | 22.9±6.0 | 20.5±5.8 |
| Unable to rise from a chair, % | 7.8 | 4.5 | 18.2 | — | 8.9 | 0.5 | 36.1 | 6.6 | — | 15.8 | 9.8 |
| Five chair stand time, s | 13.6±5.5 | 15.5±6.8 | 13.1±4.5 | 13.8±4.5 | 13.0±4.0 | — | 17.4±6.4 | 12.8±3.5 | — | 15.4±4.6 | 13.9±5.4 |
| ALM, kg | 16.1±2.3 | 19.0±3.3 | — | 15.7±2.3 | 14.9±2.4 | 14.0±2.0 | — | 15.1±2.3 | 16.7±2.6 | 16.0±3.0 | 16.2±2.9 |
| ALM/ht2, kg/ht2 | 6.4±0.8 | 7.5±1.2 | — | 6.3±0.9 | 6.4±0.9 | 5.5±0.7 | — | 6.0±0.8 | 6.4±0.9 | 6.4±1.1 | 6.4±1.0 |
| LLM, kg | 12.1±1.8 | 14.1±2.5 | — | 11.7±1.7 | 10.8±1.9 | 10.7±1.6 | — | 11.1±1.5 | — | 12.0±2.3 | 11.9±2.2 |
| Diabetes, % | 5.7 | 17.2 | 13.6 | 8.4 | 51.6 | 5.8 | 11.7 | 12.5 | 10.2 | 1.1 | 8.3 |
| CHF, % | 4.3 | 10.7 | 14.4 | 5.9 | 15.7 | 2.6 | 9.4 | 0.8 | 3.9 | — | 5.0 |
| COPD, % | 8.7 | 14.2 | — | 5.7 | 42.2 | — | — | — | 3.9 | — | 8.0 |
| Cancer, % | — | 10.7 | 11.5 | 11.6 | 10.8 | 17.8 | — | — | 15.1 | 1.1 | 12.2 |
Notes: AA = African American; AGES = Age, Gene/Environment Susceptibility-Reykjavik Study; ALM = appendicular lean mass; ALM/ht2 = ratio of appendicular lean mass over height2; BMI = body mass index; BPRHS = Boston Puerto Rican Health Study; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; FHS = Framingham Heart Study; HABC = Health, Aging, and Body Composition Study; InChianti = Invecchiare in Chianti; LLM = leg lean mass; RBS = Rancho Bernardo Study; RCT = Clinical Trials; SOF = Study of Osteoporotic Fractures. Data are presented as mean ± SD.
Because recruitment criteria were different for each study, there were several characteristic differences between studies. For example, the prevalence of slow walking speed (gait speed ≤ 0.8 m/s) varied. In men, the Osteoporotic Fractures in Men Study and the Health, Aging, and Body Composition study had the lowest percentage of slow walkers, whereas BPRHS and FHS Original study had the highest. In women, FHS Offspring, Clinical Trials, and the Health, Aging, and Body Composition studies had the lowest percentage of slow walkers, whereas the BPRHS and FHS Original study had the highest percentage. Participants who were slow walkers (gait speed ≤ 0.8 m/s) had higher body mass index, lower grip strength, and higher prevalence of self-reported diabetes, congestive heart failure, and chronic pulmonary disease. There was a large difference in mean grip strength in men by study (range 27.6–41.6kg); men in the Clinical Trials, FHS Original, and BPRHS had lower grip strengths. In women, there was less variability in grip strength (range 15.8–23.7kg). Except for higher ALM in African American women in Study of Osteoporotic Fractures study (19kg) and lower ALM in Rancho Bernardo Study women (14kg), who had lower body mass index, the differences in mean ALM in women between studies were small.
Regarding the research findings from the Conference, participants who returned surveys (n = 66) reported the strongest level of agreement with a statement regarding the use of grip strength to initially assess weakness in a clinical setting (Supplementary Appendix Table 1). Other statements with moderately strong levels of agreement included the use of physical performance measures to identify persons at risk for disability and the proposed clinical scenario for sequential screening based on mobility performance, strength testing, and body composition assessment. The respondents reported lower levels of agreement with the use of absolute appendicular lean body mass as a criterion for low mass and preferred a measure that accounts for body mass. Respondents did not feel that lean mass cutpoints without adjustment for body mass were ready for clinical use. Respondents also commented on clinical relevance (Supplementary Appendix Table 2). Overall, there continues to be concern about how to use the term “sarcopenia.” On the other hand, there was broad support for the existence of a clinically important condition of low mass and weakness, that weakness is a clinically relevant state, and that mobility impairment by performance and self-report are clinically relevant outcomes that are likely related to low mass and weakness.
Recommendations for further analyses by the FNIH consortium (Supplementary Appendix Table 3) emphasized the need to more carefully examine (i) the influence of body mass, (ii) the potential influence of gender differences in gait speed on grip strength cutpoints, (iii) the relationship between lean mass and gait speed, and (iv) to compare the cutpoints derived from the FNIH Sarcopenia analyses to other proposed criteria available in the literature. Based on these recommendations, additional analyses were performed. Detailed findings are presented in the individual manuscripts, but the final cutpoints are summarized here (Table 3).
Table 3.
Recommendations for Cutpoints for Weakness and Low Lean Mass in Men and Women
| Cutpoint | Men | Women |
|---|---|---|
| Weakness | ||
| Recommended: grip strength (GSMAX) | <26 kg | <16 kg |
| Alternate: grip strength adjusted for BMI (GSMAXBMI) | <1.0 | <0.56 |
| Appendicular lean body mass | ||
| Recommended: ALM adjusted for BMI (ALMBMI) | <0.789 | <0.512 |
| Alternate: ALM | <19.75 kg | <15.02 kg |
Notes: ALM = appendicular lean mass; BMI = body mass index.
Finally, conference respondents made several recommendations regarding directions for future research (Supplementary Appendix Table 4). Among those most emphasized were the need to study these relationships in populations with a higher prevalence of mobility limitations and the need to develop criteria for low muscle quality.
Discussion
The FNIH Sarcopenia Project offers a unique opportunity to carry out a key next step toward a consensus definition of sarcopenia. In this series, we hope to provide detailed evidence about clinically relevant criteria for weakness and low muscle mass that are based on statistically sound methods. The Sarcopenia Project incorporates an exceptionally large, diverse, and well-characterized set of populations. The pooled sample represents both genders, diversity of race and ethnicity, multiple geographic regions, and a range of health and functional states. This diversity provides important support for the generalizability of our findings and permits evaluation of subgroup effects. From an analytic perspective, the very large sample size of both men and women creates the potential for adequate cell sizes for analyses based on a range of categories of strength and body composition. Because many participating studies included alternate measures of physical function, strength, and body composition, we are able to perform a range of sensitivity and supplementary analyses to evaluate whether findings would differ substantially using other cutpoints or measures. We envision that these findings will be used by experts as they continue to clarify and refine the terminology and develop consensus criteria for a clinical condition of sarcopenia.
The rationale and conceptual framework underlying our work is based on the growing consensus of experts about the clinical and functional consequences of age- and disease-related changes in muscle. The central functional role of muscle is to provide force for body movements and actions, so a treatment that addresses muscle dysfunction should improve body movements and actions. Mobility is one way to assess impairments due to clinical states of function that are related to muscle and is an important component of functional independence and disability. Mobility can be measured reliably using performance measures (33). In addition, mobility is a useful and possibly cardinal indicator of function because decreases in mobility often precede more advanced forms of disability such as dependence in self-care (33). Mobility as a primary indicator of functional ability is also more closely linked to muscle function and less confounded by factors such as cognitive impairment than is a global indicator like dependence in self-care.
We believe that criteria for reduced lean mass should be reevaluated because those in current use have significant limitations. The original definition of sarcopenia based on reduced muscle mass alone was designed to parallel the definition of reduced bone mass, in that “abnormal” is defined in relation to the distribution of bone mass in the population. The definition proposed for sarcopenia was a ratio of muscle mass to height 2 SDs below the mean found in healthy young persons drawn from the Rosetta Stone project (37). Whereas low bone mass has consistently been associated with risk of future fracture, low muscle mass alone is not consistently associated with adverse outcomes, but rather appears to become a problem only when it is associated with weakness. Therefore, we believe that criteria for low muscle mass should be determined based on the risk of weakness. Thus, we believe that our overarching approach is well justified in that it is based on using mobility impairment as the clinically relevant functional state to determine meaningful weakness and then linking lean mass to the relationship with weakness.
We believe that our operational choices of physical performance cutpoints for analysis are reasonable. First, we provide evidence that our primary indicator, a usual gait speed of less than 0.8 m/s, is associated with reduced survival, increased disability, and is recommended by experts (15). Second, we evaluate alternate cutpoints and indicators of mobility disability. Third, we note that many widely accepted markers of a condition or disease, for example, blood pressure to diagnose hypertension, blood sugar to diagnose diabetes, or cholesterol level to diagnose hyperlipidemia, are all actually arbitrary cutpoints representing expert opinion of what is actually a continuous, graded relationship with serious adverse events. In fact, for all three of the examples (blood pressure, blood sugar, and cholesterol level), the cutoff values have evolved over time (38–40). Thus, we feel that we have attempted to select a justifiable initial cutpoint and recognize that future research may evolve toward a higher or lower value.
Although longitudinal analyses are superior to cross-sectional analyses for questions related to causation and prognosis, we note that cross-sectional analyses as used here for our work on grip strength and lean mass cutpoints (9,10) are most appropriate for establishing clinical diagnostic cutpoints based on concurrent clinical presentation and laboratory findings. We emphasize that we are not looking for cross-sectional associations, but rather for optimal diagnostic cutpoints using approaches such as classification and regression tree analysis and diagnostic test characteristics such as sensitivity and specificity.
Conference attendees generally supported the appropriateness of measures of grip strength and physical performance. Based on the feedback from conference participants, we refined and extended our analyses. With our existing resources, we were able to address all but one of the recommended additional analyses (Supplementary Appendix Table 2). Specifically, because of concerns regarding the influence of body mass on the relationships among performance, strength, and lean mass, we performed multiple additional analyses to clarify the need to adjust or stratify lean mass estimates for body mass (9–11). In addition, as recommended by the conference participants, we examined alternative cutpoints for gait speed and performed a series of analyses comparing our findings to other recommended criteria (12).
The findings reported in this series represent our best current estimates for cutpoints for clinically relevant weakness and low lean mass. We note that our final recommendation is to use unadjusted grip strength and body mass–adjusted ALM. Overall, we found that, in men, body mass adjustment had little effect on the relationships between walking speed and strength, or between strength and lean mass, but had noticeable effects in women (see (9,10) for details). These effects in women were present for both strength and mass but had only modest impact on model fit for grip strength (9), whereas the effects were larger for lean mass (10). In addition, we felt that unadjusted grip strength might be simpler to use clinically and, because it seemed less reasonable to adjust both strength and lean mass, we recommend body mass adjustment for lean mass but not strength. Also, the combination of unadjusted grip strength and body mass–adjusted lean mass had the least heterogeneity of future associations with incident mobility limitations across different study samples in women (11).
This work has numerous strengths, including sample sizes that are by far the largest to ever be applied to this topic, broad representation of community-dwelling older persons, an explicit conceptual framework, extensive use of sensitivity, and cross-validation analyses and supplemental analyses based on recommendations from multiple experts. We envision that these criteria might be used to plan prevention studies in which older persons with weakness and low lean mass receive interventions designed to reduce the incidence or increase the time to onset of mobility impairment. Alternatively, these criteria might be used to identify candidates for treatment studies of persons who already have mobility impairment, weakness, and low lean mass.
We faced numerous challenges in our efforts to pursue this work. It became obvious early on that mobility impairment is not common among older adults who participate in research studies and that persons with baseline weakness and mobility impairment are more likely to have missing data and a higher risk of loss to follow-up. It is possible that relationships among function, weakness, and mass are different and perhaps more robust among more vulnerable or frail individuals. Also, our participating studies for the most part provide longitudinal follow-up at intervals of years. Although this interval is entirely appropriate for examining some outcomes important to aging, the time interval may be too long to examine effects of acute changes in health, nutrition, and activity on body composition. Data harmonization was also a challenge. For example, studies used more than one brand and more than one generation of dual-energy x-ray absorptiometry machines to measure body composition, more than one type of hand-grip dynamometer, and more than one distance for calculating gait speed. For each of these harmonization issues, we performed sets of analyses, described in the subsequent manuscripts, to try to evaluate the impact of these variations.
Other challenges of this work included weighing the advantages and disadvantages of several different approaches to criteria that emerged from our analyses. For example, we found two sets of grip strength cutoffs and chose to use the more stringent cutoff in order to limit false positives and to pursue our overall strategy of a conservative set of criteria. We also found challenges when dealing with differences in optimal types of criteria for men and women. Although simple indicators of lean mass appear to work well in men, obesity appeared to have a strong modifying effect on the impact of lean mass on gait slowness in women. For consistency, we chose to propose the same types of indicators (eg, ALMBMI) in both men and women. However, it is possible that the effects of body composition on function are truly different by gender. If further research supports a gender difference, it is possible that future criteria may incorporate different types of indicators for men than women. Because there may be differences in the relationship between lean mass, strength, and function within important subgroups, we had hoped to perform subanalyses stratified by race and ethnicity. However despite our efforts to involve multiple studies with diverse populations, we did not have sufficient sample sizes among populations of African Americans or Hispanics to perform these planned analyses. Many unanswered questions remain but there are many exciting directions for future work (Supplementary Appendix Table 4). With involvement of the participating studies, the comprehensive data set that we created could potentially be used to address some of these questions, whereas others would require the use of additional existing data sets or even new research planning. Important gaps in knowledge that could be pursued in the next few years include evaluating the impact of weakness and low lean mass on the incidence of other important outcomes such as hospitalization, self-reported disability, and quality of life. It would also be useful to assess the incidence of new weakness and low lean mass over time and evaluate factors that contribute to it. Although we chose to base our weakness indicator on the more severe degree of “very low” grip strength (9), it might be informative to evaluate the clinical implications of the less stringent indicator of weakness with and without low lean mass. In the longer term, clinical trials of interventions based on pharmacologic agents, exercise, and nutrition, separately and even together, can help determine issues related to the responsiveness of individuals with various degrees of weakness and low lean mass. Such trials can also assist in building knowledge about criteria for clinically meaningful change in relevant outcomes. Using the findings here as well as other developments in the field, professional organizations and expert panels might make refined recommendations regarding terminology, criteria, and help prioritize further work. We hope that our efforts will provide a resource to the field as we attempt to identify, prevent, and treat this important contributor to disability in late life.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
Funding support for the conference and the work of the consortium was provided by the National Institute on Aging (1U13AG041583 and P30 AG024827), the Food and Drug Administration, and through grants from the Foundation for the National Institutes of Health, made possible by funding from Abbott Nutrition, Amgen, Eli Lilly, Merck, Novartis, and The Dairy Research Institute.
Acknowledgments
This manuscript was submitted for publication on behalf of the FNIH Sarcopenia Consortium with the following additional members:
From The Private Sector
Olivier Benichou, MD, Eli Lilly
Julie Chandler, MD, Merck Research Labs
Shao-Lee Lin, MD, Amgen
Suzette Pereira, PhD, Abbott Nutrition
Daniel S. Rooks, ScD, Novartis
Jeff Zachwieja, PhD, The Dairy Research Institute
From Government
Rosaly Correa-de-Araujo, MD, MSc, PhD, NIA/NIH
Chhanda Dutta, PhD, NIA/NIH
Melissa Garcia, MPH, IRP/NIA/NIH
Evan Hadley, MD, NIA/NIH
Judy Hannah, PhD, NIA/NIH
Lenore J. Launer, PhD, MSc
Karen Mahoney, PhD, CDER/FDA
Ali Mohamadi, PhD, CDER/FDA
Eleanor Simonsick, PhD, IRP/NIA/NIH
From Academia
Katherine L. Tucker, PhD, Northeastern University, Boston, Massachusetts
Stefania Bandinelli, MD, Azienda Sanitaria di Firenze
Paolo Caserotti, PhD, University of Southern Denmark, Odense, Denmark
Elizabeth Barrett-Connor, MD, University of California San Diego, San Diego, California
Steven R Cummings, MD, California Pacific Medical Center Research Institute, San Francisco, California
Alyssa B. Dufour, PhD, Institute for Aging Research, Hebrew SeniorLife, Boston, Massachusetts and Harvard Medical School, Boston, Massachusetts
Gudny Eiriksdottir, MS, Icelandic Heart Association, Reykjavik, Iceland
Vilmundur Gudnason, MD, PhD, Icelandic Heart Association, Reykjavik, Iceland
Marian T. Hannan, DSc, MPH, Institute for Aging Research, Hebrew SeniorLife, Boston, Massachusetts and Harvard Medical School, Boston, Massachusetts
Greg Hicks, PhD, University of Delaware, Newark, Delaware
James O. Judge, MD, University of Connecticut Health Center, Farmington, Connecticut
Annemarie Koster, PhD, University of Maastricht, Maastricht, Netherlands
Alison Kleppinger, MS, University of Connecticut Health Center, Farmington, Connecticut
George A. Kuchel, MD, University of Connecticut Health Center, Farmington, Connecticut
Joanne M. Murabito, MD, ScM, The National Heart, Lung, and Blood Institute’s Framingham Heart Study, Framingham, Massachusetts and Boston University School of Medicine, Boston, Massachusetts
Anne B. Newman, MD, MPH, University of Pittsburgh, Pittsburgh, Pennsylvania
Eric S. Orwoll, MD, Oregon Health and Sciences University
Karen M. Prestwood, University of Connecticut Health Center, Farmington, Connecticut
Suzanne Satterfield, MD, DrPH, University of Tennessee Health Science Center, Memphis, Tennessee
Carmen Castaneda-Sceppa, MD, Northeastern University, Boston, Massachusetts
Kristin Siggeirsdottir, MS, Icelandic Heart Association, Reykjavik, Iceland
Sigurdur Siggurdson, MS, Icelandic Heart Association, Reykjavik, Iceland
Qian-Li Xue, PhD, Johns Hopkins University, Baltimore, Maryland
Data contributed to this project was derived from the following studies, which were generously supported by funding as described:
SOF
The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, and R01 AG027576.
MrOS
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140.
Framingham
National Heart, Lung and Blood Institute’s Framingham Heart Study at the National Institutes of Health (grant number N01-HC-25195) and the National Institute of Arthritis Musculoskeletal and Skin Diseases and National Institute on Aging (grant number R01 AR/AG41398), Friends of Hebrew SeniorLife
UConn clinical trials
MO1-RR06192, R01-AG18887, NNG04GK63G, 5P60AG13631, Patrick and Catherine Donaghue Medical Research Foundation, American Federation on Aging Paul Beeson Faculty Scholar Program
Boston Puerto Rican Health Study
P01AG023394, R01AG027087, and P50HL105185
Rancho Bernardo Study
National Institutes of Health/National Institute on Aging grants AG07181 and AG028507 and the National Institute of Diabetes and Digestive and Kidney Diseases, grant DK31801
InChianti
Italian Ministry of Health and U.S. National Institute on Aging (NIA) supported the InCHIANTI Study as a targeted project (ICS 110.1 RS97.71; Contracts N01-AG-916413, N01-AG-821336, 263 MD 9164 13, and 263 MD 821336); this research was supported in part by the Intramural Research Program of the National Institute on Aging.
Health ABC
National Institute on Aging (NIA) Contracts N01-AG-6-2101, N01-AG-6-2103, N01-AG-6-2106; this research was supported in part by the Intramural Research Program of the National Institute on Aging.
AGES-Reykjavik
National Institutes of Health (N01-AG-12100); Hjartavernd (Icelandic Heart Association); Althingi (the Icelandic Parliament); this research was supported in part by the Intramural Research Program of the National Institute on Aging.
References
- 1. Abellan van Kan G. Epidemiology and consequences of sarcopenia. J Nutr Health Aging. 2009;13:708–712 [DOI] [PubMed] [Google Scholar]
- 2. Visser M, Schaap LA. Consequences of sarcopenia. Clin Geriatr Med. 2011;27:387–399. 10.1016/j.cger.2011.03.006 [DOI] [PubMed] [Google Scholar]
- 3. Newman AB, Kupelian V, Visser M, et al. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51:1602–1609. 10.1046/j.1532-5415.2003.51534.x [DOI] [PubMed] [Google Scholar]
- 4. Clark BC, Manini TM. Sarcopenia =/= dynapenia. J Gerontol A Biol Sci Med Sci. 2008;63:829–834 [DOI] [PubMed] [Google Scholar]
- 5. Schaap LA, Koster A, Visser M. Adiposity, muscle mass, and muscle strength in relation to functional decline in older persons. Epidemiol Rev. 2012. 10.1093/epirev/mxs006 [DOI] [PubMed] [Google Scholar]
- 6. Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60:324–333. 10.1093/gerona/60.3.324 [DOI] [PubMed] [Google Scholar]
- 7. Newman AB, Kupelian V, Visser M, et al. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci. 2006;61:72–77 [DOI] [PubMed] [Google Scholar]
- 8. Visser M, Kritchevsky SB, Goodpaster BH, et al. Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc. 2002;50:897–904. 10.1046/j.1532-5415.2002.50217.x [DOI] [PubMed] [Google Scholar]
- 9. Alley DE, Shardell M, Peters KW, et al. Grip strength cutpoints for the identification of clinically relevant weakness. J Gerontol A Biol Sci Med Sci. 2014;5:559–566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cawthon PM, Peters KW, Shardell MD, et al. Cut-points for low appendicular lean mass that identify older adults with clinically significant weakness. J Gerontol A Biol Sci Med Sci. 2014;5:567–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McLean RR, Peters KW, Shardell MD, et al. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the Foundation for the National Institutes of Health (FNIH) Sarcopenia Project. J Gerontol A Biol Sci Med Sci. 2014;5:576–583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dam TL, Peters KW, Fragala M, et al. An evidence-based comparison of candidate criteria for the presence of sarcopenia. J Gerontol A Biol Sci Med Sci. 2014;5:584–590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. 10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881–889. 10.1007/s12603-009-0246-z [DOI] [PubMed] [Google Scholar]
- 15. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–423. 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris TB, Launer LJ, Eiriksdottir G, et al. Age, Gene/Environment Susceptibility-Reykjavik Study: multidisciplinary applied phenomics. Am J Epidemiol. 2007;165:1076–1087. 10.1093/aje/kwk115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tucker KL, Mattei J, Noel SE, et al. The Boston Puerto Rican Health Study, a longitudinal cohort study on health disparities in Puerto Rican adults: challenges and opportunities. BMC Public Health. 2010;10:107. 10.1186/1471-2458-10-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hutchins-Wiese HL, Kleppinger A, Annis K, et al. The impact of supplemental n-3 long chain polyunsaturated fatty acids and dietary antioxidants on physical performance in postmenopausal women. J Nutr Health Aging. 2013;17:76–80. 10.1007/s12603-012-0415-3 [DOI] [PubMed] [Google Scholar]
- 19. Judge JO, Kleppinger A, Kenny A, Smith JA, Biskup B, Marcella G. Home-based resistance training improves femoral bone mineral density in women on hormone therapy. Osteoporos Int. 2005;16:1096–1108. 10.1007/s00198-004-1816-x [DOI] [PubMed] [Google Scholar]
- 20. Kenny AM, Biskup B, Robbins B, Marcella G, Burleson JA. Effects of vitamin D supplementation on strength, physical function, and health perception in older, community-dwelling men. J Am Geriatr Soc. 2003;51:1762–1767. 10.1046/j.1532-5415.2003.51561.x [DOI] [PubMed] [Google Scholar]
- 21. Kenny AM, Boxer RS, Kleppinger A, Brindisi J, Feinn R, Burleson JA. Dehydroepiandrosterone combined with exercise improves muscle strength and physical function in frail older women. J Am Geriatr Soc. 2010;58:1707–1714. 10.1111/j.1532-5415.2010.03019.x [DOI] [PubMed] [Google Scholar]
- 22. Kenny AM, Prestwood KM, Gruman CA, Marcello KM, Raisz LG. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels. J Gerontol A Biol Sci Med Sci. 2001;56:M266–M272. 10.1111/j.1532-5415.2010.02865.x [DOI] [PubMed] [Google Scholar]
- 23. Prestwood KM, Kenny AM, Kleppinger A, Kulldorff M. Ultralow-dose micronized 17beta-estradiol and bone density and bone metabolism in older women: a randomized controlled trial. JAMA. 2003;290:1042–1048. 10.1001/jama.290.8.1042 [DOI] [PubMed] [Google Scholar]
- 24. Dawber TR, Meadors GF, Moore FE., Jr Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health. 1951;41:279–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979;110:281–290 [DOI] [PubMed] [Google Scholar]
- 26. Newman AB, Haggerty CL, Goodpaster B, et al. Strength and muscle quality in a well-functioning cohort of older adults: the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003;51:323–330. 10.1046/j.1532-5415.2003.51105.x [DOI] [PubMed] [Google Scholar]
- 27. Ferrucci L, Bandinelli S, Benvenuti E, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc. 2000;48:1618–1625 [DOI] [PubMed] [Google Scholar]
- 28. Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS). Contemp Clin Trials. 2005;26:557–568. 10.1016/j.cct.2005.05.005 [DOI] [PubMed] [Google Scholar]
- 29. Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study–a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–585. 10.1016/j.cct.2005.05.006 [DOI] [PubMed] [Google Scholar]
- 30. Castillo EM, Goodman-Gruen D, Kritz-Silverstein D, Morton DJ, Wingard DL, Barrett-Connor E. Sarcopenia in elderly men and women: the Rancho Bernardo study. Am J Prev Med. 2003;25:226–231. 10.1016/S0749-3797(03)00197-1 [DOI] [PubMed] [Google Scholar]
- 31. Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–773. 10.1056/NEJM199503233321202 [DOI] [PubMed] [Google Scholar]
- 32. Cauley JA, Lui LY, Ensrud KE, et al. Bone mineral density and the risk of incident nonspinal fractures in black and white women. JAMA. 2005;293:2102–2108. 10.1001/jama.293.17.2102 [DOI] [PubMed] [Google Scholar]
- 33. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. 10.1093/gerona/55.4.M221 [DOI] [PubMed] [Google Scholar]
- 34. Härkönen R, Piirtomaa M, Alaranta H. Grip strength and hand position of the dynamometer in 204 Finnish adults. J Hand Surg Br. 1993;18:129–132 [DOI] [PubMed] [Google Scholar]
- 35. Salamone LM, Fuerst T, Visser M, et al. Measurement of fat mass using DEXA: a validation study in elderly adults. J Appl Physiol (1985). 2000;89:345–352 [DOI] [PubMed] [Google Scholar]
- 36. Visser M, Fuerst T, Lang T, Salamone L, Harris TB. Validity of fan-beam dual-energy X-ray absorptiometry for measuring fat-free mass and leg muscle mass. Health, Aging, and Body Composition Study–Dual-Energy X-ray Absorptiometry and Body Composition Working Group. J Appl Physiol (1985). 1999;87:1513–1520 [DOI] [PubMed] [Google Scholar]
- 37. Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–763 [DOI] [PubMed] [Google Scholar]
- 38. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 39. Genuth S, Alberti KG, Bennett P, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–3167. 10.2337/diacare.26.11.3160 [DOI] [PubMed] [Google Scholar]
- 40. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. 10.1161/01.CIR.0000133317.49796.0E [DOI] [PubMed] [Google Scholar]