Abstract
Adolescents in Northern Uganda are at risk of teenage pregnancies, unsafe abortions and sexually transmitted infections (STIs). There is silence on sex both at home and school. This cross sectional descriptive analytical study interviews a random sample of 827 students and 13 teachers on knowledge, perception and acceptability to a comprehensive adolescent sexual and reproductive health education in “O” and “A” level secondary schools in Gulu District. Quantitative data was analysed using SPSS 16.0. Directed content analysis of themes of transcribed qualitative data was conducted manually for common codes, sub-categories and categories. Of the 827 students; 54.3% (449) reported being in a sexual relationship especially those aged 15–17 years. Majority 96.1% (807) supported the teaching of a comprehensive ASRHE, citing no negative impact 71.5% (601). Majority 81.6% (686) agreed that such education could help prevention of STIs, abortions and teenage pregnancies, and that it should be taught by health workers 69.0% (580). Majority 76.6% (203) reported that ASRHE was not currently being taught in their schools. Students had low knowledge levels and misconceptions about ASRHE. ASRHE was highly acceptable though not being emphasized; its success in school settings requires multidisciplinary culturally sensitive approaches amongst which health workers should be frontiers.
Keywords: Acceptability, ASRHE, Knowledge, Perception
I. Introduction
Background Adolescents’ Sexuality and Reproductive Health Education (ASRHE), refers to instruction on issues relating to human sexuality including human sexual anatomy, sexual- reproduction, sexual intercourse, reproductive health, emotional relations, reproductive rights and responsibilities, abstinence, birth control, sexual orientation, values, decision making, communication, dating, sexually transmitted infections (STIs) and how to avoid them [1].
Today there are 1.8 billion youths, forming the largest segment of the world’s population[2]. 70% of 10–19 year olds live in developing nations [3]; nearly contributing half of Uganda’s population [2], but majority do not receive sexuality education both at home and at school although it is their right [4]. According to the adolescents and youth report [2], young people, particularly those living in poverty, have been virtually ignored in policies and programmes thus high prevalence of STIs, teenage pregnancies and abortions.
A. HIV/AIDS amongst Adolescents
As a result of lack of sexuality education, almost half of new HIV infections each day are among young people especially adolescents in Sub-Saharan Africa [5], due to early sexual initiation [6]. HIV prevalence in Uganda is increasing from 6.5% to 7.3%, as in [7]. Northern Uganda has the second highest HIV/AIDS prevalence in the country [8] and adolescents account for almost half of all new HIV infections, explaining the multi-dimensional effect of HIV on Northern Uganda’s economy [9]–[10]. This region is the poorest in the country [8]. Experiences show that HIV/AIDS programmes, including sexuality and reproductive health education that respect and involve young people, while being sensitive to their cultures, are more likely to succeed [11].
B. Pregnancy amongst Adolescents
As a result of deficiency in sexuality and reproductive health education, sixteen million adolescent girls become mothers worldwide every year, many of whom suffer consequences of unplanned pregnancy [2]. In Uganda, the girl-child is commonly looked at as a source of wealth and society expects or forces girls to marry at very young ages, explaining a high teen birth rate of 211 per 1,000. Up to 31% of adolescents, aged 15–19, are already mothers or pregnant with their first child and only 12% of this age group use contraceptives [12]-[13], yet maternal mortality among adolescent mothers is more than twice the rate in other age groups [14].
C. Abortions among Adolescents
There is also a high incidence of abortion among pregnant adolescents [14]. In Uganda, studies show that 78% of female adolescents know someone who has had an abortion and more than two-thirds of patients receiving care for abortion complications at local teaching hospitals in Uganda are aged 15–19-years [15].
D. Adolescents in Northern Uganda
According to Amone [16], the two decade war burden heavily crippled the social, economic, education and health of individuals and communities of Northern Uganda. About 1.7 million people were internally displaced at the peak of the insurgence. The youths in this region are now living in adverse poverty coupled with the post war psychological impacts of their experiences. The communities in this region, who were forced to crowd together in camps, experienced increased idleness which led to poverty; frequent out-breaks of illnesses, alcohol abuse, gender-based violence and sexual exploitation against women and girls, leading to concerns of the spread of HIV/AIDS. Adolescents in this region are now struggling to cope with the broken social, economic and health systems following resettlement.
Reference [9] shows that adolescent girls aged 13 to 17 years in Northern Uganda are most frequently reported as survivors of sexual violence. The report emphasizes that, nearly 40% of Gulu District adolescents aged 10–19 years living in IDP camp settings are sexually experienced, with median age of first sexual intercourse at 15 years and that childbearing and marriage are becoming increasingly unlinked yet abortions contribute 13.5% of the outcome of first pregnancy in this region.
E. Need for Sexuality Education
According to the report from World Population Foundation [17], over 50% of young people worldwide are sexually active by the time they are 17 years old. Many adolescents are curious and will wish to experience their sexuality [1]. Countries with conservative attitudes towards sex education have a higher incidence of STIs and teenage pregnancy [18]. Adolescents are resorting to pornographic magazines and media to obtain sexual information [19].
In Uganda, common avenues for sex education are parents or caregivers, formal school programs, and public health campaigns. Formal education is based on seven years of primary and six years of secondary education. Secondary education consists of 6 years divided into two levels the first level comprising grades 1–4 (ordinary level) and the second level, grades 5 and 6 (advanced level). The education system, particularly secondary education, is still centrally managed by the Ministry of Education and Sport (MoES). The Government of Uganda introduced Universal Secondary Education (USE) in 2007 to meet rising demand, increase access to secondary schools and improve on school education out comes (MoES, 2006). Knowledge, perceptions and negotiation skills are most efficiently influenced during secondary education schooling [20]-[21]. The increased access to secondary schools is a good opportunity to capture young stars for sexuality and reproductive health education. Policies of Uganda’s education strongly emphasize the importance of science education in national development. However there is increasing poor performance in mainly the science subjects including biology in some secondary schools especially those in Northern Uganda [22]. We therefore cannot entirely rely on adequacy of adolescent sexuality and reproductive health education as a component of biology subject. Besides, majority students do not offer sciences. Discussions on sexuality in the existing Ugandan primary and secondary school curriculum mainly include anatomy, changes during adolescence and fertilisation, leaving out important aspects like dealing with gender based violence and prevention of: sexually transmitted infections other than HIV, abortions and teenage pregnancy thus the need to bridge the existing gap. Straight talk foundation has had an input in Northern Uganda but there still challenges of sustainability and coverage of adolescents in remote areas. Some schools offer no sex education, since it remains a controversial issue especially with regard to the age at which children should start receiving such education and the amount of detail to be revealed. It is thought that an investigation in this area would shed light on the perceptions and factors influencing acceptability to a comprehensive adolescent sexual and reproductive health education amongst secondary schools and in particular knowledge on prevention of STIs, teenage pregnancies and abortions.
A survey conducted in Gulu and Amuru districts [23], rated sexuality education from families as a source of information at only 16% due to cultural factors. The report emphasised that in the case of Northern Uganda and Acholi sub region in particular, there has been no sustained reproductive health education to roll over improved behavioural and attitude change. Studies and interventions on Sexual and Reproductive Health Education in this region have been dwelling so much on abstinence-only and HIV/AIDS prevention programmes. Straight Talk Foundation [24], emphasizes its limited opportunities for children in respect to the sources of information dissemination and challenges it faces in strategically, firmly and regularly coordinating its activities in this region.
Reliance on traditional sources of sex information particularly from community elders and paternal aunts is weakening [15]. Social and cultural norms have largely prohibited parents and children from discussing sex. As a first step towards improving the options available to adolescents to protect their sexual and reproductive health, we need to understand; what lies behind this gap, whether and where adolescents go for health-related information and care, and how to make it easier for them to obtain the services they need.
According to a report from the Uganda Delivery of Improved Services for Health (Uganda DISH) [25], adolescents in Uganda especially Northern region, frequently do not have access to appropriate sexual and reproductive health services. Failure to respond to adolescents’ sexual and reproductive health needs and designing interventions that directly involve them in culturally acceptable manner is reflected in the emerging rates of sexual initiation during young adulthood that are rising globally and in many developing countries [26], [27], [28], [29]. This is also reflected in the emerging teenage pregnancies, mortality due to unsafe abortions, new HIV infections and other STIs that predominantly affect young people in Uganda [12], [13]. Studies in Northern Uganda [23], and elsewhere in the world have revealed ineffectiveness of abstinence-only sexual and reproductive health interventions and have recommended a comprehensive adolescent sexual and reproductive health education [30], [31], [32].
Teachers spend a considerable time with students, it is seemingly easier for them to execute and integrate such interventions in the existing curriculum. Determining what exactly teachers communicate and what challenges they face while teaching sexuality to their students is crucial, since effective student-teacher communication is associated with delayed sexual initiation [33]. Students’ openness to their teachers in such a setting is a big concern. Delivery of sexual education in schools is being dodged by teachers with claims that they lack appropriate training in teaching sexuality education as well as teaching aids [15], although it exists as a component of the biology syllabus. Teachers often feel uncomfortable and lack confidence to talk to their students about sexual issues as this goes against local traditions, viewing public discussion of sex as taboo subject. Protecting adolescents from STIs, Unsafe abortions and unwanted pregnancies calls for a concerted effort from parents, teachers, health workers, the community and the government.
With the relative peace prevailing in Northern Uganda since 2006, special attention is needed to restore the broken social fabric through multi-sectorial approach. Because most youth obtain at least some formal education under Universal Secondary School Education (USE), school-based programs appear to be a logical choice for which there is need to build capacity in offering a comprehensive sexual and reproductive health education, if we are to secure a healthy future for the adolescents in Northern Uganda. Determining perceptions and acceptability to such interventions is very crucial.
F. Problem Statement
There is silence on sex education both at home and school, with an assumption that our children are young. Only 34% of Ugandan girls and 22% boys aged 12–14 years receive sex education in schools [34]. At home, 71% girls and 64% boys never talk with parents about sex related matters.
According to the United Nations Human Development Indicators report [35], Uganda’s adult literacy rate is only 33.2%. This lowers the quality of sexuality and reproductive health education parents deliver to their children. Many adolescents in Gulu District cannot afford media channels often used for sexuality education due to high poverty levels and busy school academic schedules [36], [37]. There has been no sustained health education in Northern Uganda to effectively roll over improved attitude change [24]-[23]. It is the culture of most people in Northern Uganda, including teachers not to discuss sex education to their children [15]-[23], thus the information gap and need for an investigation in this field.
G. Justification
Because we do not give information doesn’t mean the youth do not have sex. Girls are getting pregnant at the age of 12 and 13 years resulting into complications. These complications can be avoided through access to both sexuality education and youth friendly services.
Adolescent sexual education could help reduce school drop outs. Adolescents who stay in school longer are less likely to engage in sexual risk behaviours [38].
Abstinence-only and the ABC (abstinence, be faithful, use condoms) focus of the last few years have not brought about the desired behavioural change[39]. There is need for a comprehensive sexual and reproductive health education [31]-[32]. This remains a priority for Northern Uganda as it transits from war to post conflict rehabilitation. Perceptions and acceptability to such a comprehensive sexual and reproductive health education beyond HIV prevention in a school setting had not been largely assessed in Uganda and in particular Northern Uganda.
G. Purpose
This study determines knowledge, perceptions and acceptability of students and teachers to a comprehensive adolescent sexual and reproductive health education in secondary school settings of Gulu District and therefore determines how best such interventions can be designed in the near future to meet the sexual and reproductive health needs of adolescents in this region.
The study highlights priority areas for programmes and policies aimed at improving the sexual and reproductive health education of the youth in secondary schools in Gulu District, to ensure that adolescents have adequate knowledge and tools to make informed and healthy choices concerning their sexual and reproductive health.
H. Objectives
1. Broad Objective
To determine knowledge, perceptions and acceptability to a comprehensive adolescents’ sexual and reproductive health education, how it should be conducted and who should deliver it, in secondary school settings of Gulu District.
2. Specific Objectives
To determine the proportion of respondents with sound knowledge about adolescent sexual and reproductive health education amongst secondary schools in Gulu District.
To determine respondents’ perceptions towards a comprehensive ASRHE in secondary school settings in Gulu District.
To assess the acceptability of a comprehensive ASRHE in secondary school settings in Gulu District.
To highlight priority areas for programmes and policies aimed at improving the sexual and reproductive health of adolescents in secondary schools in Gulu District
II. Literature Review
A. The Outcome of Implementation of ASRHE in Other Countries
Timor-Leste presents a unique successful case for implementing adolescents’ sexual and reproductive health education [40], in which teachers and students were involved in designing and implementing a new curriculum. In Nigeria, a randomized school-based intervention using nurses led to more favourable attitudes toward HIV prevention measures among students [41]. In a school-based intervention in Thailand, secondary students who were exposed to a comprehensive sexual and reproductive health education program had greater knowledge than other students, and were more likely to refuse sex and to decrease frequency of sex, although no change was seen in consistent condom use [42]. On the contrary, a study in the Dominican Republic showed that adolescents who received sexual education had higher rates of condom use and more knowledge of HIV prevention than those who did not [43]. These two studies reflect that there are other underlying factors that influence behaviour other than knowledge and perceptions, of which the degree of acceptability to such interventions is crucial. Studies in Mexico revealed that a school-based intervention led to more positive norms related to HIV-preventive behaviours [44]-[45]. On the other hand, early sexual initiation culminating into teenage pregnancies, abortions and STIs are consequences of lack of ASRHE. Countries with conservative attitudes towards sex education have a higher incidence of STIs and teenage pregnancy [18].
B. Acceptability and Perceptions to ASRHE
In a Tanzanian study [46], that assessed acceptability of parents and guardians of adolescents towards the introduction of sexual and reproductive health education in the community and schools, there was a mixed feeling on the introduction of sexual and reproductive health education in schools. Parents strongly supported that they should talk with their adolescents about sexuality and reproductive health (88.6%) but their culture prohibits them from doing so (76.7%). Also supported that condoms could protect against HIV/AIDS and sexually transmitted infections (82%), but strongly opposed the use of condoms to their adolescents because it would encourage promiscuity (78%), however such misconceptions have been disputed by other studies [47]. According to [46], the preferred source of information about sex education and reproductive health was from the parents (86%), religious leaders (70%), media (62%), health workers (61%) and school teachers (59%). They concluded that parents were willing to introduce sexual education and reproductive health in the community but the approach needed to be worked out carefully by taking into account of the cultural and religious factors. Although the most preferred source of information about sex in the above study were parents, on the contrary, [48] revealed that practically only 1.1% of parents discuss sexual aspects with adolescents.
In Tanzania, where it is considered a taboo for teachers and parents to talk with children about sexual matters including sexually transmitted diseases (STDs) in schools and at home because of cultural, religious barriers and political pressure, study [49] assessed the knowledge of STDs, and attitude towards sexual behaviour and STDs among secondary school students. Results showed that majority of students had poor knowledge about symptoms associated with STDs. Television and radio were the most commonly mentioned sources of information on STDs, whilst none of them cited parents as source of information (p<0.001). It was concluded that parents were a poor source of sexual education compared to media, but the extent and quality of the media content is still a question. Besides, media channels cannot be afforded by adolescents in Northern Uganda due to high poverty levels[36].
According to [50], assessment of the effectiveness of a school based “Adolescent Reproductive Sexual Health Education Package” in improving students’ knowledge on reproductive sexual health matters in Kerala; they observed that in the pre-intervention period, majority of adolescents were poorly informed about reproductive sexual health matters, particularly about contraceptives. As compared to boys, girls had much poorer knowledge about prevention of pregnancy and after intervention; there was a statistically significant increase in the knowledge in both boys and girls. They concluded that adolescent sexual and reproductive health education was feasible and effective in a school setting. However such feasibility may not be obvious in Northern Uganda settings due to cultural factors [15].
According to [47], evaluation of sex education and HIV prevention programmes world-wide, it was indicated that interventions that employed activities, instructional methods, and behavioural messages that were appropriate to the youth culture, developmental age, and sexual experience were more successful. In this report, several authors had concluded that there is evidence for a positive impact of curriculum and group-based sex education programs on behaviour for adolescents and young adults. The patterns of findings were similar irrespective of the social, economic and gender settings. Consistently, skill-based programs were more effective at changing behaviour than were knowledge-based programs. Just as importantly, however, “there was no evidence to suggest that such programs increased sexual behaviour”, as some parents have always feared [46]). “This concern had been used as a reason not to provide sexual-prevention information to youth”. It was recommended that programs targeting youth should be an important component of overall prevention strategies. The conclusion was that development of comprehensive reproductive health education and evaluation of strong adolescent and young-adult interventions have been deficient yet are needed, particularly in sub-Saharan Africa, where abortions and teen pregnancy rates are high and adolescents are becoming HIV-infected.
C. Knowledge Gap and Recommendations
A situation analysis of adolescent reproductive health in selected Pacific Island countries [51] revealed that adolescents were not adequately informed about family planning, reproductive and sexual health as well as services available for young people. They lacked negotiation skills for safe sex, had low motivation for preventing teenage pregnancies through contraceptive methods and sexuality education was going at a slow pace. Integration of a comprehensive sexual and reproductive health education services into the existing health care system was recommended. Such a recommendation may not be that feasible in post conflict Northern Uganda setting due to already constrained broken health care system under rehabilitation, following resettlement.
In an Indian study [52], to investigate the perception, knowledge and attitude of adolescent urban secondary school girls towards STIs, safer sex practice and sex education, it was found that more than one third of students in this study had no accurate understanding about the signs and symptoms of STIs other than HIV/AIDS. About 30% of respondents considered HIV/AIDS could be cured, 49% felt that condoms should not be available to youth, 41% were confused about whether the contraceptive pill could protect against HIV infection and 32% thought it should only be taken by married women. The author concluded that there was an immense need to implement gender-based sex education regarding STIs, safe sex options and contraceptives amongst schools in India.
A study conducted by the Valley research group [53], to determine reproductive health awareness, attitudes and behaviour of adolescents in Nepal revealed that Knowledge of RTIs and STDs was limited. Only 30.0 per cent of adolescents had heard of reproductive tract infections (RTIs), the authors highlighted the need for adequately designed education programmes that offer comprehensive reproductive health education and recommended Initiation of Reproductive Health education before the onset of puberty by including relevant topics even in lower secondary curriculum. The controversy is whether teachers in Africa, particularly Northern Uganda would take over such responsibility despite limitation by cultural influence [15]; since parents believe that it is their sole responsibility to offer sexuality education [46] although they are not doing it [48].
In Zimbabwe, a study [48] to assess parents’ and teachers’ attitude towards Adolescent Sexual and Reproductive Health Education (ASRHE) and to determine their opinion on the need, content and the appropriate person to provide (ASRHE) in a school setting, revealed that majority of parents had not discussed growth and development issues with their adolescents. Only 5.2% teachers and 1.1% parents discussed sexual aspects with adolescents. Majority of parents agreed that information on HIV/AIDS/STD should not be provided and more than 50% of parents were not sure whether information on topics like, safe sex, contraceptives, pregnancy, abortion and childcare should be provided to adolescents. Authors concluded that there was urgent need for introduction of reproductive health and sexual education in the school setting.
The above studies reflect that not only significant knowledge gaps exist amongst adolescents on sexual and reproductive health issues but also with in programs that target both knowledge and behaviour change in the sexual activities of adolescents. Programs need to go beyond HIV and focus on broader topics in sexual and reproductive health. Currently, in many programs; other STIs and pregnancy prevention are conspicuously absent. According to [39], it is evident that neither the abstinence-only nor the ABC (abstinence, be faithful, use condoms) focus of the last few years has brought about the desired outcomes for adolescent sexual and reproductive health. Given that no single educational or communication program appears to have yielded lasting behavioural change, a stronger focus on knowledge, perceptions and acceptability is crucial. Such studies have not been largely conducted in secondary school settings in Northern Uganda. The need for direct involementment of the vulnerable adolescents, determining their perceptions and acceptability to such interventions calls for this study.
III. Methodology
A. Study Design
This was a descriptive analytical cross sectional study with both quantitative and qualitative research methods of enquiry.
B. Study Scope
The study was carried out from April 2012 to April 2013, in Gulu District-Northern Uganda.
C. Study Site
The study was conducted in 5 secondary schools in Gulu District, all with “O” and “A” levels
D. Study Population
The study targeted students and teachers in secondary schools in Gulu District.
E. Sampling Procedure
According to the District Education Officer and School Guide Uganda, there were 42 secondary schools in Gulu District. Due to limited funds, 5 schools were selected purposively for convenience. Mixed and single Schools in Urban, peri-urban and rural settings were represented in the study.
F. Selection Criteria
Inclusion criterion
Students in Secondary Schools, Teachers in secondary Schools
Informed consent for study participants >18 years and assent for participants <18 years
Exclusion criterion
Those who did not consent/assent to the study were excluded
G. Sample Size
The total population in the sample schools was 3,664 students, meaning on average each class from senior one (S.1) to senior six (S.6) had a total of 122 students for each of the 5 schools. The study sample size was obtained by using the hypergeometric formula for calculating sample size in small population,
where
-
n is required sample size
N is population size, 3,664
z is value for the level of confidence, 1.96 since we are using a 95% confidence interval.
P and q are population proportions, p-proportion intending to accept a comprehensive adolescents’ sexual and reproductive health education in the secondary school setting and q is (1-p), since these proportions were unknown we assumed 50%(0.5) for each.
Eis the value setting accuracy of our sample proportion, +/−3% = 0.03
- Therefore,
- Then sample size was 827 students. For equal representation, proportion (P) depending on school population was calculated as
Thus 22.6% of each school’s population was studied, meaning a total of 170 students from St. Joseph Layibi College, 90 from Graceland Girls’ College, 252 from Gulu High School, 170 from Awere SS and 146 from Awach SS. In each individual school, efforts were made to equally represent all classes S1–S6 by 10 students per class for focussed group discussions and the rest of students for self-administered questionnaires. These students were selected in such a way that half of the study participants are boys and the other half girls in all the respective sessions so as to balance both sexes in mixed school settings.
H. Study Variables
The study variables included both dependent and independent. In this study perceptions and acceptability to a comprehensive ASRHE in secondary school setting were likely to depend on the respondents’ prior knowledge about the topic, thus knowledge being the independent variable.
I. The Outcome Variables
Perception and acceptability of respondents, who feel that a comprehensive adolescent sexual and reproductive health education should be taught in secondary schools, were measured in percentages. Percentages were calculated for a number of respondents who feel that ASRHE in a school setting should be taught by; teachers, health workers, parents or peer/friends. Respondents’ perceptions on the content of ASRHE and its likely negative impacts in a school setting were qualitatively analysed.
J. Other Variables
Data on factors influencing perception, attitudes and acceptability such as sex, age, level of education, nature of school and previous exposure to sexual and reproductive health education and state of emotional relationships were obtained.
K. Study Procedure
The selection of study subjects was done by the research team members through recruitment of the respondents until the required sample size per class was obtained. The recruitment was done at the respective schools during evening time for co-curricular activities in order not to interfere with routine class work. Researchers conducted the recruitment with the aid of class lists obtained from school administrators so as to ensure that no respondent was recruited more than once.
Every respondent was explained to the purpose of the study and consented/assented to participate. A self-administered research questionnaire was then administered to the selected number of students per class and atleast 2 selected teachers per school in charge of reproductive health as key informants. Questionnaires were answered with guidance of the researchers to avoid misinterpretation of concepts. A 45 minutes focused-group discussion (FGD) was held with 10 randomly selected students per class in each of the 5 schools. Students who were recruited for FGDs were not recruited for questionnaires. Each focused group discussion was conducted by two researchers; one asking questions and the other counting and tallying respondents’ opinion by show of hands and recording any other responses from the respondents. Each respondent was availed with a focussed group discussion guide. These discussions were conducted in class rooms or an environment with privacy after formal class teaching with female respondents approached by female researchers and male respondents approached by male researchers.
L. Data Collection
Data collection was carried out using a pre-tested questionnaire designed in simple English by the research team. Both qualitative and quantitative data was obtained using the self-administered questionnaires that was filled at the spot as this had been a successful method in similar studies done elsewhere. The questionnaires had both closed and open ended questions covering variables that were selected basing on the problem statement and study objectives. Data collection was be done by the research team, headed by the Principle Investigator. Other qualitative data was obtained from the focussed group discussions using focussed group discussion guides, tape recorders and manila papers to ensure that none of the verbal deliberations were missed.
M. Data Analysis
Data sorting, coding, entry and analysis was done by the research team with the help of a biostatician and technical supervision by the faculty mentors. Quantitative data was analysed using SPSS 16.0 statistical package programme. Directed content analysis of themes of transcribed qualitative data was conducted manually for common codes, subcategories and categories.
N. Data Management and Presentation
Descriptive statistics that include frequencies, proportions/percentages, means, medians, standard deviations was computed and presented in form of tables and graphs as appropriate. Multivariate analysis, categorisation of variables, linear regression and chi-square testing was conducted to determine factors that significantly influenced knowledge, perceptions and acceptability to teaching an integrated adolescent sexual and reproductive health education in the secondary schools.
O. Ethical Considerations
The study followed the National Institute of Health guidelines on research involving use of human subjects and ethical approval was obtained from Gulu University Faculty of Medicine Institutional Research Committee (IRC). Permission to execute the study was sought from the District Education Officer (D.E.O), Chief Administrative Officer (C.A.O) and from administrators of the respective schools. Study participants indicated their consent/assent by endorsing pre-designed consent/assent forms using their signatures in the presence of the investigators. The respondents had the right to refuse to participate or withdraw from the study at any time if they so wished. Their confidentiality and privacy were highly observed. Tape records were destroyed at the end of the study duration to avoid retrieval by members outside the research team. Data was kept in password protected files until dissemination.
P. Study Limitations
Being a cross-sectional study, it may not give us the future perception and attitude of respondents. Perceptions of parents and religious leaders that are part and key partners in delivering sexual education was beyond the scope of this study.
Q. Quality Control
Each school had a defined schedule day and received a notice at least 2 days prior to the school visit on receipt of acceptance from school administration to voluntarily participate.
Pre-coded questionnaires in English were pre-tested in a similar study population by the research team in order to minimize errors. Proper identification of the respondents by use of class lists was emphasized to avoid any double recording. All questionnaires were re-checked for completeness by research team before leaving the site. Questionnaires were stored centrally to ensure safety of the items. All collected data that was entered in the computer was protected by a password to prevent access by unauthorized individuals.
R. Dissemination of Results
Study findings will be presented in scientific conferences and published in peer review journals. A copy of findings in the final bound report will be submitted to MESAU-MEPI secretariat, Gulu University IRC and to authorities including the D.E.O, C.A.O of Gulu District.
IV. Results
A. Socio-Demographic Characteristics
A total of 840 respondents were interviewed, 827 students and 13 teachers. Of the 840 respondents, majority 58.3% (n = 490) of them were aged between 15–17 years, 52.9% (n = 444) were females and 47.1% (n = 396) were males. Majority of respondents, 68.3% (n = 574) were from schools with in municipality (urban) setting and 31.7% (266) from rural setting.
Of the 540 respondents who answered self-administered questionnaires, 13.3% (n = 72) had ever been abducted, a total of 28 (5.2%) reported having children of which 3.5% (n = 19) were students, mostly in senior one and two. (See table II)
TABLE II.
Showing Respondents’ Socio-Demographic Characteristics
| Age (years) | Frequency | Valid Percent |
|---|---|---|
| 12–14 | 159 | 18.9 |
| 15–17 | 490 | 58.3 |
| 18–20 | 159 | 18.9 |
| > 20 | 32 | 3.8 |
| Total | 840 | 100 |
| Class of respondents | Frequency | Valid Percent |
|---|---|---|
| S.1 | 234 | 27.9 |
| S.2 | 203 | 24.2 |
| S.3 | 162 | 19.3 |
| S.4 | 118 | 14.0 |
| S.5 | 86 | 10.2 |
| S.6 | 24 | 2.9 |
| Teachers | 13 | 1.5 |
| Total | 840 | 100 |
| Nature of school | Frequency | Valid Percent |
|---|---|---|
| Single girls | 185 | 22.0 |
| Single boys | 147 | 17.5 |
| Mixed boys and girls | 508 | 60.5 |
| Total | 840 | 100 |
| Settings | Frequency | Valid Percent |
|---|---|---|
| Within municipality (urban) | 574 | 68.3 |
| Outside municipality (rural) | 266 | 31.7 |
| Total | 840 | 100 |
| Emotional relationship | Frequency | Valid Percent |
|---|---|---|
| In a boyfriend/girlfriend sexual relationship | 451 | 53.7 |
| Married | 33 | 3.9 |
| Not in any sexual relationship | 356 | 42.4 |
| Total | 840 | 100 |
| Psycho-traumatic experience | Frequency | Valid Percent |
|---|---|---|
| Ever been abducted | 72 | 13.3 |
| Never been abducted | 468 | 86.7 |
| Total | 540 | 100 |
| Parenthood | Frequency | Valid Percent |
|---|---|---|
| Have children | 28 | 5.2 |
| Have no children | 512 | 94.8 |
| Total | 540 | 100 |
During assessment of status of emotional relationship, of the 827 students, 54.3% (n = 449) reported being involved in sexual boyfriend/girlfriend relationships, majority of which were aged 15–17 years 62.6% (n = 281). A total of 2.8% (n = 23) students reported to be married of which 6 were senior one students aged 12–14 years while 42.3% (n = 355) were not involved in any emotional relationship. Table 2 summarises status of emotional relationship of respondents in different classes and age groups.
B. Acceptability to a Comprehensive Adolescents’ Sexual and Reproductive Health Education
Of the 840 respondents, majority 96.1% (n = 807) felt that a comprehensive adolescents’ sexual and reproductive health education should be taught in secondary school settings while 3.9% (n = 33) felt it should not be taught. In response to the question “Is ASRHE currently being taught in your school?”, of the 300 students in focussed group discussions, 67.6% (n = 203) reported that it was not being taught while 32.3% (n = 97) reported some components of adolescents’ sexual and reproductive health education were currently being taught in their schools.
C. Perceptions about a Comprehensive Adolescents’ Sexual and Reproductive Health Education in Secondary School Setting
A total of 71.5% (n = 601) respondents believed that teaching students such education is not likely to cause any negative impacts, 21.5% (n = 181) believed that teaching ASRHE could promote promiscuity, 3.0% (n = 25) felt that teaching ASRHE in a secondary school setting will be time wasting at the expense of other subjects while 3.9% (n = 33) expressed worries related to breach of cultural norms.
Of the 840 respondents, 4.9% (n = 41) had not been exposed to any form of sexual and reproductive health education while 95.1% (n = 799) had ever been exposed of which majority had been taught by: teachers; 26.9% (n = 226), health workers; 25.8% (n = 217), parents; 21.9% (n = 184). Minority had been exposed to sexuality education through their friends 7.5% (n = 63), a considerable number 11.9% (n = 100) reported having been taught by all the above while 1.1% (n = 9) reported other sources especially media.
When asked on whether teaching a comprehensive ASRHE would help reduce STIs, abortions, teenage pregnancy and school drop outs; 26.5% (n = 223) strongly agreed, 55.1% (n = 463) agreed, 10.4% (n = 87) disagreed while 8.0% (n = 67) strongly disagreed.
When asked their opinion on who should teach ASRHE in secondary schools; majority of respondents felt it should be taught by health workers on school visits 69.0% (n = 580), 14.0% (n = 118) preferred parents during visiting days, 10.7% (n = 90) preferred teachers, 3.8% (n = 32) preferred friends while 2.4% (n = 20) felt that it should be taught by all the above.
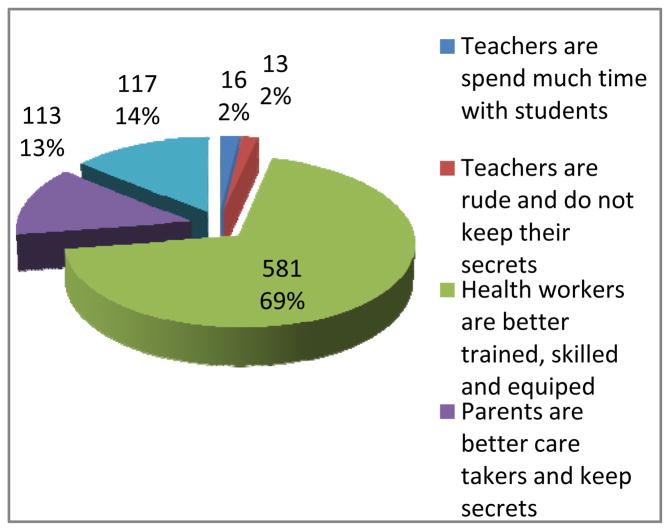
When asked to give one reason for their choice on who should teach ASRHE in secondary schools, majority of students who preferred health workers believed that they are better trained, skilled and equipped 69.0% (n = 581), while a considerable number of students entrust their friends other than their teachers whom they report to be rude and unapproachable, well as teachers and a few students believed that since they spend much time together at school and that since teachers are professionally trained to teach, they would be in a better position to teach ASRHE. (See Fig 1)
Fig. 1.
Pie chart showing respondents’ reasons for who should teach ASRHE in secondary school setting
D. Priority Areas for Policies and Programmes Aimed at Improving ASRHE in Secondary Schools
When asked the major barrier to accessing ASRHE information in secondary schools, majority of respondents reported that students feel shy to share and learn such information from their teachers 55.6% (n = 467), 19.2% (n = 161) reported having no textbooks and information education and communication (IEC) materials in their libraries, 13.1% (110) reported that ASRHE was not taught at all by their teachers while 12.1% (n = 102) reported that teachers feel shy to teach ASRHE.
When asked the best intervention that can be done to improve on ASRHE in schools, of the 840 respondents, majority 50.5% (n = 424) suggested that it should be taught by health workers on school visits other than teachers, 26.4% (n = 222) suggested that ASRHE should be taught as a separate subject in the secondary school curriculum, 19.9% (n = 167) suggested that teaching aids like textbooks should be availed to teachers and accessible in the libraries while minority, 3.2% (n = 27) suggested organising conferences on ASRHE in schools and use of media channels.
In response to suggestions on what priority topics to be emphasised in teaching ASRHE in secondary schools, majority 75.6% (n = 635) felt that a comprehensive package on prevention of: STIs, teenage pregnancy and abortions should be emphasised, 14.2% (n = 119) suggested prevention off STIs only, 10.0% (n = 84) suggested prevention of; teenage pregnancy and abortions only, while 0.2% (n = 2) cited teaching of good morals and responsible conduct.
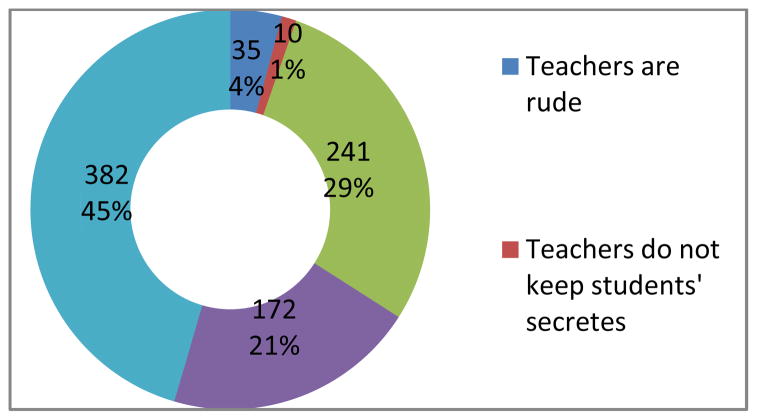
In response to the question “where do adolescents feel comfortable to seek reproductive health attention”, majority 47.7% (n = 401) preferred government hospitals and facilities, 29.9% (n = 251) preferred private hospitals, 18.6% (n = 156) preferred seeking reproductive health attention from private clinics while 3.8% (n = 32) preferred drug shops and pharmacies. Majority of respondents who preferred government facilities believed they are cheap 47% (n = 398), although some believe there is no privacy in government hospitals 16.0% (n = 132) and that they are discouraged by over waiting while at these facilities, 7.0% (n = 59). A considerable number of respondents believed that private hospitals offer better services 26.0% (n = 218). Those who preferred private clinics and drug shops was because of easy accessibility 4.0% (n = 33). A summary of respondents’ reasons is provided here in Fig. 2.
Fig. 2.
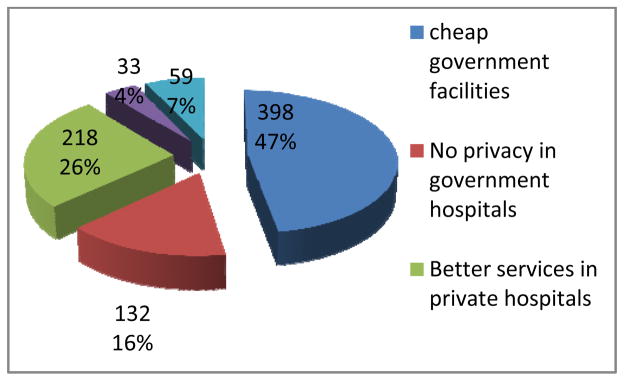
Pie chart showing respondents’ reasons for their choice of health facility from which seek reproductive health attention
In response to the question “As an adolescent, who do you feel comfortable telling first to seek help in case you got pregnant”, majority 43.1% (n = 362) would prefer discloser to their peer because they believe they are more approachable and trust worthy, 29.9% (n = 251) would disclose to health workers whom they believe have professional skills, 21.8% (n = 183) would disclose to their parents while only 5.2% (n = 44) would disclose to their teachers, whom other respondents mistrusted for reasons related to secrecy and rudeness (See Fig. 3).
Fig. 3.
Doughnut showing respondents’ reasons for choice of person they would disclose to if they got pregnant
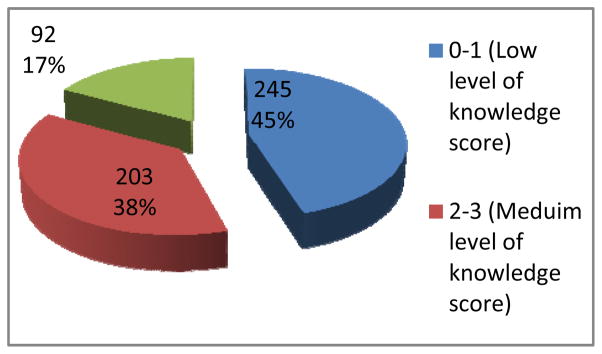
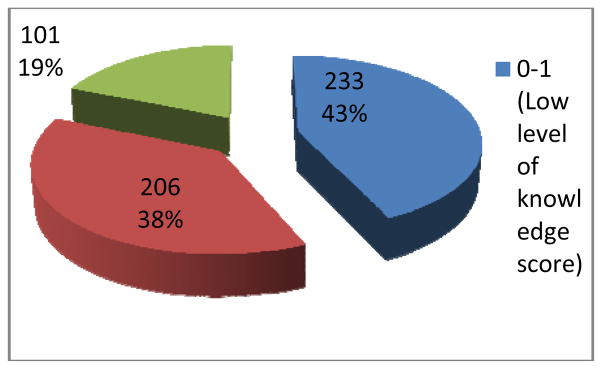
E. Knowledge on ASRHE, Prevention of STIs and Teenage Pregnancies
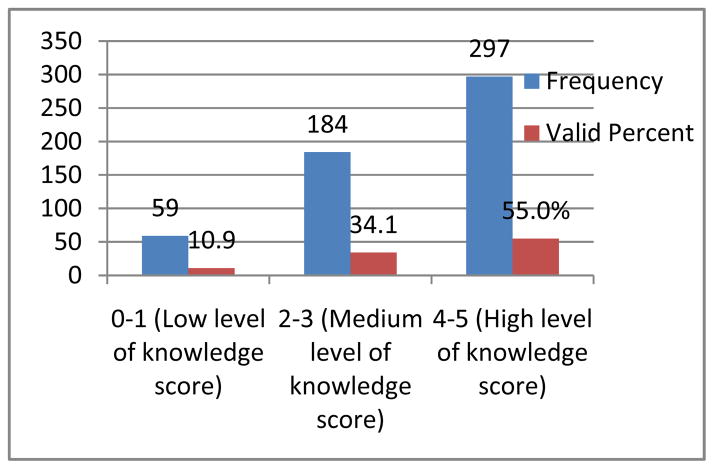
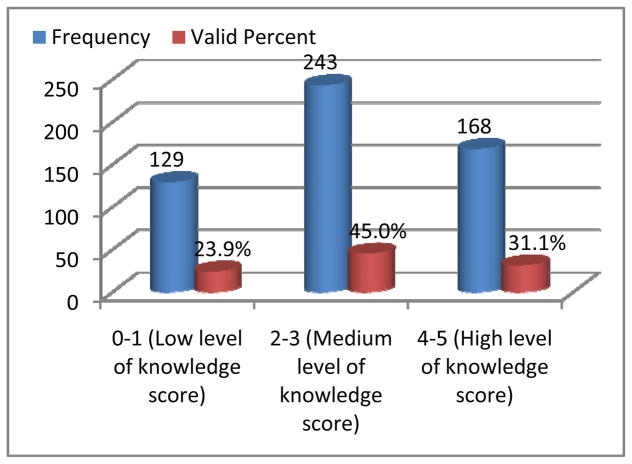
Participants recruited for self-administered questionnaire (n = 540) were asked to rate themselves on their current level of knowledge about different components of a comprehensive adolescents’ sexual and reproductive health education by ticking a score of 0–1 for low level of knowledge, 2–3 for medium level of knowledge and 4–5 as the maximum score representing a high level of knowledge about a given topic. The results are provided here in figures
Majority of participants 65.2% (n =352) reported high level of knowledge about the role of good hygiene in an adolescent as summarised in the Table IV.
TABLE IV.
Showing Participants’ Self-Rating on Understanding the Role of Good Hygiene amongst Adolescents and Youth
| Frequency | Percent | |
|---|---|---|
| 0–1 (Low level of knowledge) | 49 | 9.1 |
| 2–3 (Medium level of knowledge) | 139 | 25.7 |
| 4–5 (High level of knowledge) | 352 | 65.2 |
| Total | 540 | 100 |
V. Discussion
A. Socio-Demographic Characteristics
Of the 827 respondents, majority; 54.3% (n = 449) reported being involved in sexual boyfriend/girlfriend relationships while 2.8% (n = 23) students reported to be married. Majority off students who were married 52.2% (n = 12) and those involved in sexual relationships 62.6% (n = 281) were aged between 15 – 17 years of which majority were in senior two (95% CI, x2=1.586, p = 0.000). Of the 540 respondents who answered self-administered questionnaires a total of 19 (3.5%) students reported having children of which majority were in senior one and two aged 15–17 years. These findings highlight the need to emphasise sexuality education amongst adolescents in this age group to guide them in their relationships.
B. Acceptability to a Comprehensive Adolescents’ Sexual and Reproductive Health Education
Although ASRHE was highly acceptable at 96.1% (n = 807) in a secondary school setting, in focussed group discussions, majority of respondents, 67.6% (n = 203) reported that it was not currently being taught in their schools. The proportion of respondents that reported receiving sexuality education schools in the present study 32.4% (n = 97) is similar to that reported by Guttmacher Institute [34]. During Focussed group discussions, students who reported ASRHE as being currently taught in their schools cited major components as normal changes during adolescence and prevention of STIs especially HIV. Components like prevention of teenage pregnancies, role off emergence contraceptives, and dealing with gender based violence, sexuality violence and adolescence crisis, role of safe male medical circumcision had not been discussed by their teachers. The idea of comprehensiveness and diversity in adolescents’ sexual and reproductive health is still lacking and calls for special attention given the fact that adolescents are moving away from sexual relationships to getting married and bearing children while in a school setting. There was a significant association between acceptability to ASRHE and; age, sex, class of respondents, nature of school (mixed or single), previous exposure to ASRHE, and status of emotional relationship. There was no statistically significant association between acceptability to ASRHE and; school settings, parenthood and psycho-traumatic experience. Table V below summarises acceptability of ASRHE cross tabulated with independent variables.
TABLE V.
Chi Square Table (95% CI)
| Independent variable | Df | Pearson Chi-square (X2) | P value (2-sided asymp. Sig) | Likelihood ratio |
|---|---|---|---|---|
| Age | 3 | 40.578 | 0.000 | 31.587 |
| Sex | 1 | 11.287 | 0.001 | 11.690 |
| Class of respondents | 6 | 33.673 | 0.000 | 36.394 |
| Nature of school | 2 | 19.229 | 0.000 | 15.528 |
| School settings | 1 | 1.735 | 0.188 | 1.861 |
| Emotional relationship | 2 | 15.278 | 0.001 | 14.251 |
| Psycho-traumatic experience | 1 | 0.011 | 0.915 | 0.011 |
| Parenthood | 1 | 0.112 | 0.738 | 0.101 |
| Previous exposure to ASRHE | 1 | 32.539 | 0.001 | 18.003 |
C. Perceptions about a Comprehensive Adolescents’ Sexual and Reproductive Health Education in Secondary School Setting
Majority of respondents, 71.5% (n = 601) believed that teaching students such education is not likely to cause any negative impacts, 21.5% (n = 181) believed that teaching ASRHE could promote promiscuity. Such misconceptions have been cited in similar settings in East Africa [46], but have been disputed by other studies that have evaluated sex education programs worldwide [47]. Respondents who were not involved in any sexual relationship were more likely to reject ASRHE (95% CI, x2=13.278, p = 0.001) A few respondents, 3.0% (n = 25) felt teaching ASRHE in a secondary school setting will be time wasting at the expense of other subjects while 3.9% (n = 33) expressed worries related to breach of cultural norms. Other surveys in Uganda show similar [15]. This is of particular concern thus introduction of such education should be in a manner that is culturally acceptable to adolescents and their community.
Of the 840 respondents, 4.9% (n = 41) had not been exposed to any form of sexual and reproductive health education while 95.1% (n = 799) had been exposed. There was a significant association between previous exposure and acceptability to ASRHE (95% CI, x2= 32.539, p = 0.000). Majority of exposed respondents had been taught by: teachers; 26.9% (n =226), health workers; 25.8% (n =217), parents; 21.9% (n =184). Minority had been exposed to sexuality education through their friends 7.5% (n = 63), a considerable number 11.9% (n = 100) reported having been taught by all the above while 1.1% (n = 9) reported other sources especially media.
Although the previous source of exposure to sexuality and reproductive health education had been majorly teachers, when asked their opinion on who should teach ASRHE in secondary schools; majority of respondents felt it should be taught by health workers on school visits 69.0% (n = 580), whom they believe to be well trained, skilled and equipped. Only 10.7% (n= 90) preferred teachers, 3.8% (n = 32) preferred friends whom they believe to be trustworthy and approachable other than their teachers whom they report to be rude, unapproachable and that they do not keep secrets although their counter parts 2% (n = 16) believed that since teachers spend much time with students at school, together with their professional training would be in a better position to teach ASRHE. Studies elsewhere in East Africa have consistently reported teachers as least preferred source of sexuality education [46], revealing the need to shift to a multisectoral approach in teaching reproductive health in schools amongst which health workers should be frontiers. Although considerable proportion of students, 14.0% (n = 118) preferred to be taught sexuality education at school by parents during visiting days just like parents were the most preferred source in a Tanzanian study [46], Studies elsewhere in the world have cited parents as poor source of sexuality information [49] and that practically only 1.1% of parents discuss sexual aspects with their adolescents [48], particularly due to cultural factors. Other surveys in Northern Uganda [15]-[23] and Uganda in general have reported similar [34].
Despite the fact that adolescents who stay in school longer are less likely to engage in sexual risk behaviours [38], when asked on whether teaching a comprehensive ASRHE in schools would help reduce STIs, abortions, teenage pregnancy and school drop outs; 26.5% (n = 223) strongly agreed, 55.1% (n = 463) agreed, 10.4% (n = 87) disagreed while 8.0% (n = 67) strongly disagreed.
D. Priority Areas for Policies and Programmes Aimed at Improving ASRHE in Secondary Schools
Despite the fact that effective student-teacher communication is associated with improved behavioural changes like delayed sexual initiation [33], when asked the major barrier to accessing ASRHE information in secondary schools, majority of respondents reported that students feel shy to share and learn such information from their teachers 55.6% (n = 467), 13.1% (n = 110) reported that ASRHE was not taught at all by their teachers while 12.1% (n = 102) reported that teachers feel shy to teach ASRHE. Students’ openness to their teachers was a big concern that needs to be addressed. This probably explains why most students preferred ASRHE to be taught by health workers. In response to this same question, 19.2% (n = 161) respondents reported having no textbooks and lacked information education and communication (IEC) materials in their libraries. This complaint had been raised by earlier surveys that involved teachers [15]
When asked the best intervention that can be done to improve on ASRHE in schools, of the 840 respondents, majority 50.5% (n = 424) suggested that it should be taught by health workers on school visits other than teachers, 26.4% (n = 222) suggested that ASRHE should be taught as a separate subject in the secondary school curriculum while 19.9% (n = 167) suggested that teaching aids like textbooks should be availed to teachers and accessible in the libraries. Minority, 3.2% (n = 27) suggested organising conferences on ASRHE in schools and use of media channels. Earlier studies had underscored use of media channels on grounds that they are not affordable to most adolescents in Northern Uganda due to high poverty levels, this region being the poorest in the country [36]-[37]. Therefore evidence-based sex education must be a major strategy in school-based programs, with user friendly resources readily available to students.
In response to suggestions on what priority topics to be emphasised in teaching ASRHE in secondary schools, majority 75.6% (n = 635) felt that a package comprising of prevention of: STIs, teenage pregnancy and abortions should be emphasised, 14.2% (n = 119) suggested prevention of STIs only, 10.0% (n = 84) suggested prevention of; teenage pregnancy and abortions only, while 0.2% (n = 2) cited teaching of good morals and responsible conduct.
Majority of respondents supported a comprehensive adolescents’ sexual and reproductive health education package in this regard.
In response to the question “where do adolescents feel comfortable to seek reproductive health attention”, majority 47.7% (n = 401) preferred government hospitals and facilities which they believed are cheap 47% (n = 398), although some believe there is no privacy in government hospitals 16.0% (n = 132) and that they are discouraged by over waiting while at these facilities 7.0% (n = 59). Because most adolescents in Uganda cannot pay for reproductive health services [25], empowering government facilities with youth friendly reproductive health services would attract adolescents but young people’s fear of seeking reproductive health services in settings without privacy was a big concern. Next preferred were private hospitals 29.9% (n = 251) and private clinics 18.6% (n = 156) which they believe offer better services 26.0% (n = 218) though expensive while 3.8% (n = 32) preferred drug shops and pharmacies because of easy accessibility 4.0% (n = 33) even in rural areas.
In response to the question “who do adolescents feel comfortable telling first to seek help in case they got pregnant”, majority 43.1% (n = 362) would prefer discloser to their peer because they believe they are more approachable and trust worthy, 29.9% (n = 251) would disclose to health workers whom they believe have professional skills, 21.8% (n = 183) would disclose to their parents while only 5.2% (n = 44) would disclose to their teachers, whom their counterparts mistrusted for reasons related to secrecy and rudeness. “I cannot tell my teacher when I get pregnant because I will be expelled from school. We have lost two bright candidate class mates who conceived during second term holidays. I rather tell my parents who are likely to keep it secret because they know if they don’t, the loss is theirs, having paid school fees for nothing after my expulsion from school”, says 18 year old senior four female candidate. Empowering peer educators through skill- based programs conducted by health workers in schools could be of help otherwise advice exchanged between peers when they get pregnant may not be appropriate. In the above scenario, the student’s primary interest is not solving the reproductive health problem but to stay in school which may be the parent’s interest as well.
E. Knowledge on ASRHE, prevention of STIs and Teenage Pregnancies
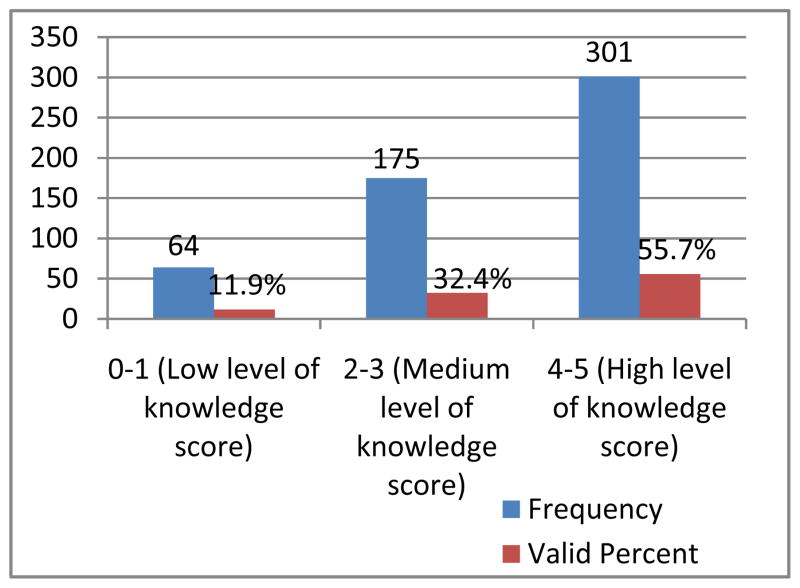
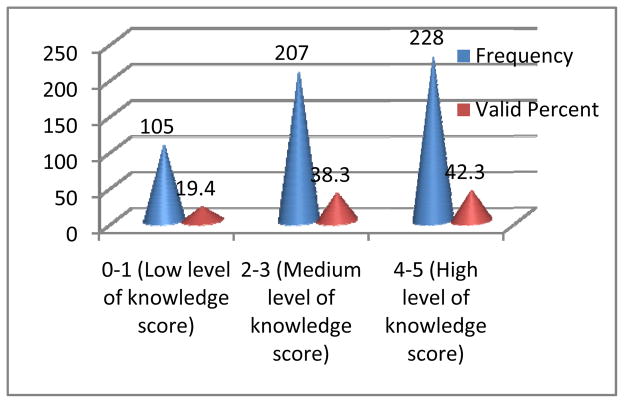
Majority of adolescents, 55.0% (n = 297) rated themselves having high knowledge about normal changes during adolescence. Only 31.1% (n = 168) rated themselves high on describing adolescence crisis although 34.4% (n= 186) reported high knowledge level on its prevention. Majority of respondents scored themselves highly on the role of good hygiene in an adolescent 65.2% (n = 352). Majority 55.7% (n = 301) rated themselves having high level of knowledge on knowing information about prevention of HIV however a fewer number 42.2% (n = 228) reported high level of knowledge on prevention of other STIs other than HIV, clearly indicating the need to design programs that target STIs beyond HIV. Some areas still needed special attention. Approximately half of the adolescents 45% (n = 245) in this study reported having low level of knowledge about ability to deal with gender-based violence and how they would advise such a colleague and only 17% (n =92) reported having high level of knowledge on ability to deal with sexuality violence. This is clearly an area that requires attention as it is not uncommon adolescents being victims of sexual violence in Northern Uganda [9].
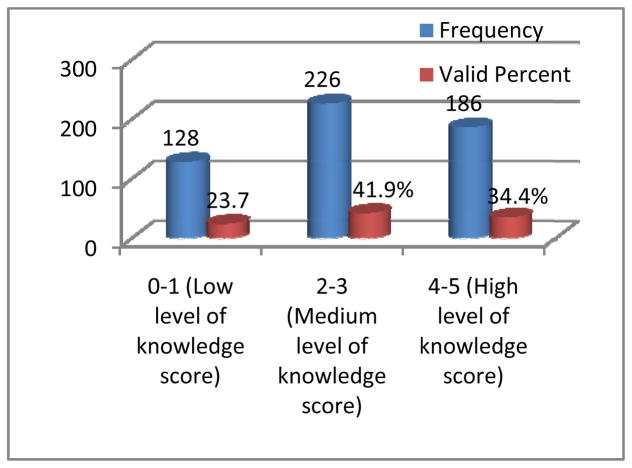
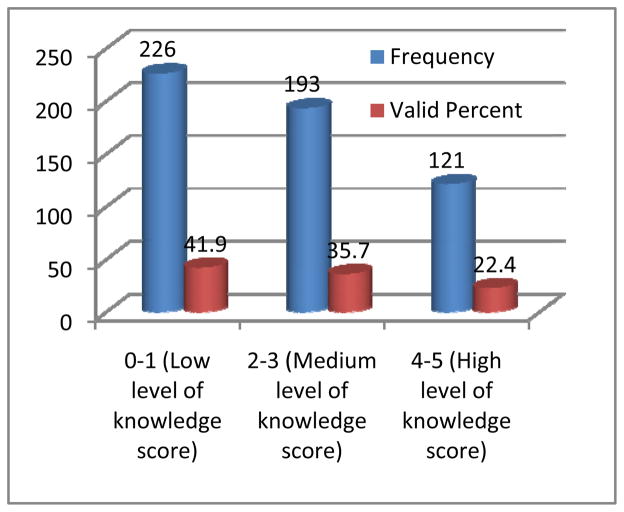
It is important to note that among the school course elements that have generated most controversy and debate in Uganda are discussions about contraceptive use and information on the options of safer sex, including condom use despite the fact that contemporary literature reveals that oral contraceptives are safe for adolescents. Bridging the gap between knowledge and practice, particularly with respect to the use of contraceptives, condom use and safe male medical circumcision which is perceived as a cultural norm in some communities, has emerged as a major behaviour change communication challenge to reducing adolescents’ vulnerability to STIs, abortions and unwanted teenage pregnancies. Studies have shown that safe male medical circumcision helps in prevention HIV infection by up to 60% in conjunction with other HIV prevention packages (WHO/UNAIDS, 2007; Uganda MoH SMMC policy, 2010). The present survey showed majority 41.9% (n = 226) of respondents reported low level of knowledge about the role of safe male medical circumcision in partial prevention of STIs like HIV. In response to the question “safe male medical circumcision could help in partial prevention of some STIs including HIV”, of the 840 respondents, only 38.3% (n = 322) said this was true, 26.5% (n = 223) said that this was not true while 35.1% (n = 295) were unsure. This is of concern as HIV prevalence in Uganda is increasing from 6.5% to 7.3% with Northern Uganda having the second highest prevalence in the country yet adolescents contribute to almost half of the new infections [8]-[7], leaving this region with an economic burden [37].
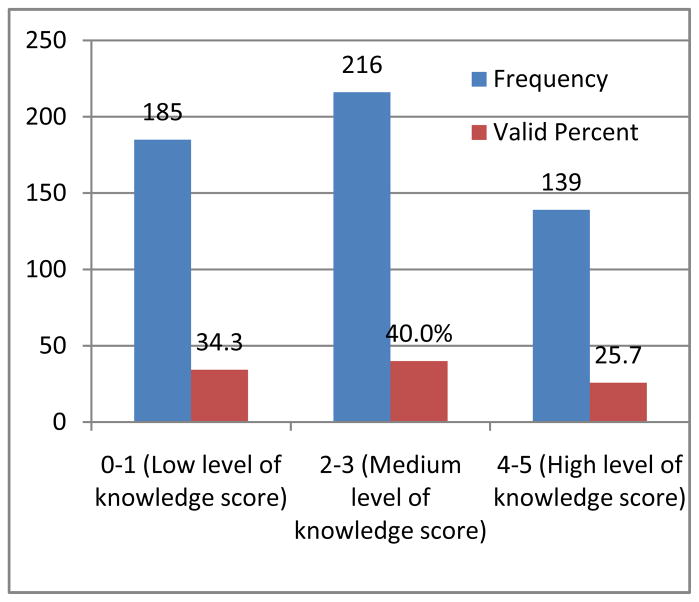
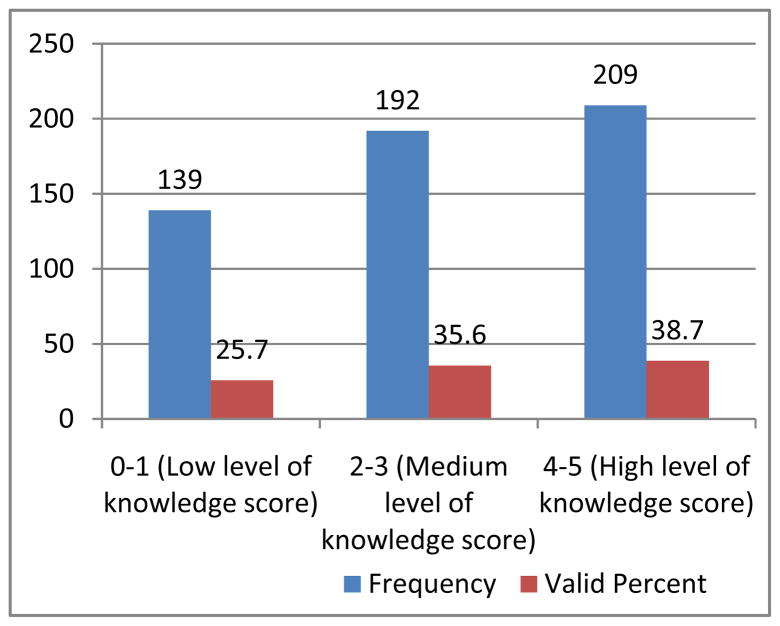
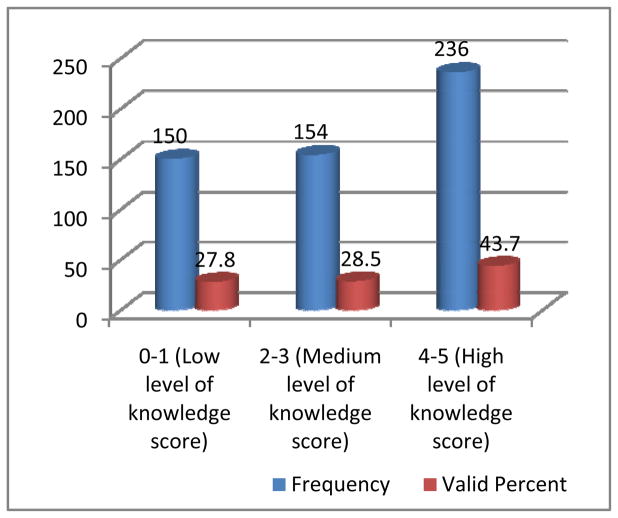
In this present study, only 25.7% (n = 139) of respondents felt that they had high knowledge on understanding the role of emergence contraceptives in prevention of teenage pregnancy despite the fact that majority 38.7% (n = 209) and 43.7% (n = 236) reported high level of knowledge on understanding complications of teenage pregnancy and abortions respectively.
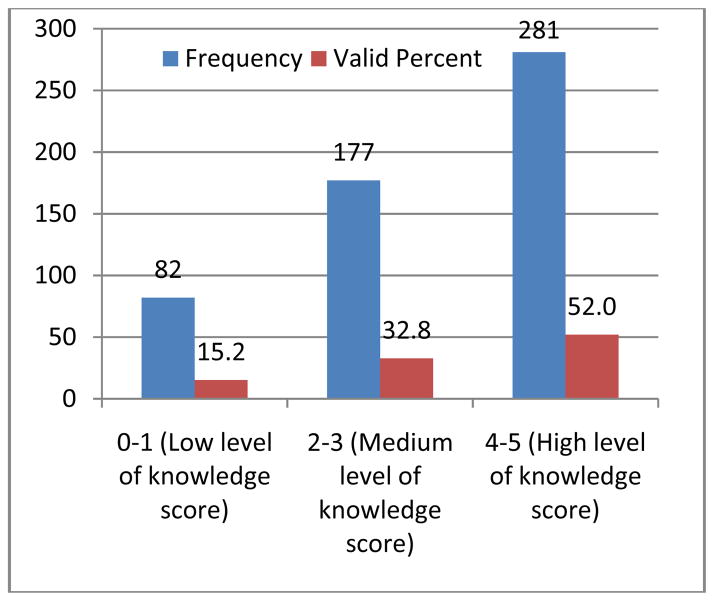
In Uganda, only 12% of adolescent girls use any form of contraceptives thus a high teenage pregnancy rate of 211 per 1000 [12]-[13] contributing to a high maternal mortality among adolescent mothers that is twice higher than other age groups [14]. In the current study in response to the question “emergence contraceptive pills are for married people only”, of the 840 respondents, 36.9% (n = 310) said this was true while 23.9% (n = 201) were unsure and only 39.2% (n = 329) disagreed. Studies elsewhere in the world like India have shown similar [52]. Adolescents’ attitude towards contraceptives, including emergence pills may be based on cultural and other beliefs that need specific investigation and educational efforts to change. Majority of respondents highly knew the role of girl child education in prevention of teenage pregnancy 52.0% (n = 281). Studies show that adolescents who stay in schools longer are less likely to engage in sexual risk behaviours [38]. In this current study of 840 respondents majority of respondents, 96.1% (n = 807) supported the teaching of a comprehensive ASRHE in secondary schools, citing no negative impacts 71.5% (n = 601) and majority 81.6% (n= 686) agreed that such education could help prevention of STIs, abortions and teenage pregnancies, especially if most preferably taught by health workers 69.0% (n = 580).
The opponents of sex education in schools say that ASRHE is not culturally sensitive, it has ambiguous material and could encourage students to experiment with sex, defeating the very purpose of the campaign and contributing to the spread of HIV/AIDS and other STIs and increment of abortions and unplanned teenage pregnancies. On the contrary, for example according to HIV/AIDS activists, sex education helps to make students cautious against the dangers of experimenting with sex at a young age, sensitising them and also warning them about the potential exposure to the deadly virus. Despite though, many parents at home and teachers at schools are hesitant to talk about sex with their teenage children. If schools agree to implement ASRHE further training in communication skills for peer educators, teachers and health personnel may be required. In addition, support of state and regional political leaders and health and education authorities is essential for ASRHE package to be effectively executed in secondary schools in Gulu district.
VI. Conclusion and Recommendations
Inspite of efforts over the past two decades in STIs, teenage pregnancy and abortions prevention, these burdens still presents a serious challenge to adolescents in societies around the world, including Northern Uganda. A comprehensive adolescents’ sexuality and reproductive health education is a crucial weapon in prevention of these burdens using school settings. Although highly acceptable in the present study, a number of studies, including the current study identified that this package is not emphasised in both school and home settings thus poor knowledge and reflected low levels of awareness of different components of a comprehensive ASRHE amongst adolescents. It is important to educate adolescents about safe sex, prevention of STIs, teenage pregnancies and abortions. The present strategy of this education in Uganda is simply not effective due to conservative cultural attitudes.
In summary, despite conservative cultures, there is an immense need for implementation of health worker-guided culturally sensitive comprehensive adolescents’ sexuality and reproductive health education package for appropriate age groups in secondary schools to cope up with the increasing vulnerability of adolescents, towards STIs, teenage pregnancies and abortions in Uganda. Standardised school-based programs across all levels of secondary schools in Northern Uganda will allow adolescents to make informed choices about protecting themselves from STIs, teenage pregnancies and abortions, especially when they decide to become sexually active.
Fig. 4.
Bar graph showing participants’ self-rating on knowledge about normal changes during adolescence
Fig. 5.
Clustered cylinder graph showing participants’ self-rating on ability to describe adolescence crisis
Fig. 6.
Cylinder graph showing participants’ self-rating on ability to describe prevention of adolescents’ crisis
Fig. 7.
Pie chart showing participants’ self-rating on ability to deal with sexuality violence
Fig. 8.
Pie chart showing participants’ self-rating on ability to deal with gender based violence
Fig. 9.
Bar chart showing participants’ self-rating on ability to provide information about prevention of HIV
Fig. 10.
Clustered cone graph showing participants self-rating on knowledge about other STIs other than HIV
Fig. 11.
Bar graph showing participants’ self-rating on understanding the role of girl child education in prevention of teenage pregnancy
Fig. 12.
Graph showing participants’ self-rating on understanding the role of safe male medical circumcision in prevention of HIV
Fig. 13.
Participants’ self-rating on understanding the role of emergence contraceptives in prevention of teenage pregnancy
Fig. 14.
Graph showing participants’ self-rating on understanding complications of teenage pregnancy
Fig. 15.
Graph showing participants’ self-rating on understanding complications of abortions
TABLE I.
Showing the Respective Total Students’ Population Basing On Academic Year 2011/2012, According to the Respective Head Teachers
| S/No. | Name of School | Setting | Total Population School |
|---|---|---|---|
| 1 | Gulu High School | Urban (mixed) | 1116 |
| 2 | St. Joseph’s college Layibi | Peri-Urban (single boys) | 750 |
| 3 | Graceland Girls’ College | Peri-Urban (single girls) | 400 |
| 4 | Awere SS | Rural (mixed) | 750 |
| 5 | Awach SS | Rural (mixed) | 648 |
TABLE III.
Showing Age*Class of Respondents*Emotional Relationship Cross Tabulation
| Class of respondents
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Emotional relationship | Age (Years) | S.1 | S.2 | S.3 | S.4 | S.5 | S.6 | Teachers | Total |
| In boyfriend-girlfriend sexual relationship | 12–14 | 25 | 15 | 1 | 0 | 0 | 0 | 0 | 41 |
| 15–17 | 42 | 96 | 87 | 41 | 13 | 2 | 0 | 281 | |
| 18–20 | 4 | 4 | 20 | 35 | 42 | 10 | 0 | 115 | |
| >20 | 0 | 0 | 0 | 2 | 3 | 7 | 2 | 14 | |
| Total | 71 | 115 | 108 | 78 | 58 | 19 | 2 | 451 | |
| Married | 12–14 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| 15–17 | 0 | 7 | 3 | 0 | 1 | 1 | 0 | 12 | |
| 18–20 | 0 | 0 | 0 | 1 | 3 | 0 | 0 | 4 | |
| >20 | 0 | 0 | 0 | 1 | 0 | 0 | 10 | 11 | |
| Total | 6 | 7 | 3 | 2 | 4 | 1 | 10 | 33 | |
| Not in any sexual relationship | 12–14 | 91 | 18 | 0 | 2 | 1 | 0 | 0 | 112 |
| 15–17 | 61 | 60 | 46 | 23 | 6 | 1 | 0 | 197 | |
| 18–20 | 5 | 3 | 5 | 12 | 12 | 3 | 0 | 40 | |
| >20 | 0 | 0 | 0 | 1 | 5 | 0 | 1 | 7 | |
| Total | 157 | 81 | 51 | 38 | 24 | 4 | 1 | 356 | |
Acknowledgments
This work was funded by the MEPI-MESAU under programmatic award number R24TW008886I from the Forgarty International Centre.
Footnotes
The content is solely the responsibility of the authors and does not necessarily reflect the official views of the Forgarty International Centre or the National Institute of Health.
Contributor Information
Lule Herman, Email: lule.herman@gmail.com, (Principal Investigator) (Medical Doctor) is with Gulu University faculty of medicine and Jinja Regional Referral Hospital.
E. Ovuga, Professor of Psychiatry and Mental Health and former Dean Faculty of Medicine-Gulu University. He now Heads supervision of research in Gulu University post graduate school
M. Mshilla, (PhD fellow) is senior lecturer of Medical Pharmacology and H.O.D Medical Entrepreneurship in Gulu University medical School
S. Ojara, (Medical Doctor) is with St. Mary’s Hospital Lacor
G. Kimbugwe, Medical student in Gulu University Medical School
A. P. Adrawa, Medical student in Gulu University Medical School
N. Mahuro, Medical student in Gulu University Medical School
References
- 1.Kearney 2008 http://www.doctors.am/en/announcments/Sex-education-and-human-sexuality/4821.
- 2.UNFPA-Adolescents and Youth. 2012 http://www.unfpa.org/public/adolescents/
- 3.United Nations Population Fund, UNFPA. State of the World Population: Investing Adolescents’ Health and Rights. New York: 2003. [Google Scholar]
- 4.The International Conference on Population and Development, ICPD. The ICPD POA, Para 7.37–7.47. Cairo: 1994. Identifying Sexuality education as a human right, essential to development and human well-being. [Google Scholar]
- 5.Joint United Nations Programme on HIV/AIDS, UNAIDS. Report on the Global AIDS Epidemic. 4. Geneva, Switzerland: 2004. HIV and young people: the threat for today’s youth; pp. 93–98. [Google Scholar]
- 6.Pettifor AE, Straten V, Ariane, Dunbar, Megan S, Shiboski, Stephen C, Padian, Nancy S. Early age of first sex: A risk factor for HIV infection among women in Zimbabwe. AIDS. 2004;18(10):1435–1442. doi: 10.1097/01.aids.0000131338.61042.b8. [DOI] [PubMed] [Google Scholar]
- 7.Uganda AIDS indicator survey. 2011 Available at news@ultimatemediaconsult.com.
- 8.Uganda Bureau of Statistics. Uganda National Household Survey Findings 2009/2010. UBOS Plot 9 Coleville Street, P.O. Box 7186, Kampala, Uganda: 2010. Telephone: (256-41) 706000; Fax: (256-41) 237553/230370; Email: ubos@ubos.org; Internet: www.ubos.org. [Google Scholar]
- 9.UNICEF . UNICEF Chulho Hyun. Communication Officer; UNICEF Uganda: 2005. Study highlights of rape in Northern Uganda’s largest IDP camp GULU, UGANDA, 15 JUNE 2005. +256 (0)77 222 347, chyun@unicef.org. [Google Scholar]
- 10.Chris Ocowun. Cited in the new vision Uganda. 2008. Jun Monday, 16th, [Google Scholar]
- 11.United Nations (UN) General assembly. Declaration of commitment on HIV/AIDS. Special session on HIV/AIDS; 25–27 June 2001.2001. [Google Scholar]
- 12.Alan Guttmacher Institute. Adolescent Sexual and Reproductive Health in Uganda: A Synthesis of Research Evidence. 2004 http://www.agiusa.org/pubs/2004/12/20/or14.pdf.
- 13.Macro International. Reproductive Health of Young Adults in Uganda. 2002 Available at http://www.measuredhs.com/pubs/pdf/OD23/OD23.pdf.
- 14.Myagmar E. Ulaanbaatar: s.n. 2000. Mongolian adolescents’ needs assessment survey report; p. 126. [Google Scholar]
- 15.Kibombo R, Neema S, Moore A, Humera AF. Occasional Report No. 35 February (2008) 2008. Adults’ Perceptions of Adolescents’ Sexual and Reproductive Health: Qualitative Evidence from Uganda. [Google Scholar]
- 16.Amone J. Reproductive health status of adolescents in the Internally Displaced People’s (IDP) camps in Gulu District, Uganda. Int Conf AIDS; International Conference on AIDS, 15th: 2004; Bangkok, Thailand. 2004 Jul 11–16; 15; 2004. abstract no. MoPeC3505. [Google Scholar]
- 17.World Population Foundation, WPF. Computer-based sexuality and life skills education in secondary schools in Indonesia, Thailand, Kenya and Uganda. 2003 http://schoolnetuganda.sc.ug/projects/on-goingprojects/theworldstartwithme.
- 18.Monibiot G. Joy of sex education: The Guardian. 2004 May 11 [Google Scholar]
- 19.Lauszus Finn Friis, Kloster Aiste Ozeraityte, Nielsen Jacob Lauesgaard, Boelskifte Jane, Falk Jørgen, Rasmussen Kjeld Leisgård. Gender-specific knowledge on sex. Arch Gynecol Obste. 2006;12:200, 66452. doi: 10.1007/s00404-009-1350-3. [DOI] [PubMed] [Google Scholar]
- 20.Lewin K, Caillords F. Financing secondary Education in Development 2001 [Google Scholar]
- 21.Nsubuga YKK. Development and examination of secondary school education in Uganda 2003 [Google Scholar]
- 22.Namirembe G. Status of education for rural people in Uganda Paper presented at the ministerial seminar on education for rural people in Africa. Addis Ababa, Ethiopia 2005 [Google Scholar]
- 23.Oyat C. The Challenges of Sustained HIV/AIDS Education in Uganda: A case study in Northern Uganda. Gulu University Medical Journal (GUMJ) 2009;4:13–18. 2008/2009. [Google Scholar]
- 24.Straight Talk Foundation. The straight talk foundation in Uganda: Impact of mass media initiatives (Full report) USAID; Kampala: 2007. p. 64. [Google Scholar]
- 25.Uganda DISH II- Research on Adolescent Sexual and Reproductive Health in Uganda. http://www.ugandadish.org/resource/aa/aa6.shtml.
- 26.Ali MM, Cleland J. Sexual and reproductive behaviour among single women aged 15–24 in eight Latin American countries: a comparative analysis. Social Science & Medicine. 2005;60(6):1175–1185. doi: 10.1016/j.socscimed.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 27.Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, Bajos N. Sexual behaviour in context: a global perspective. Lancet. 2006;368(9548):1706–1728. doi: 10.1016/S0140-6736(06)69479-8. [DOI] [PubMed] [Google Scholar]
- 28.Glasier A, Gülmezoglu AM, Schmid GP, Schmid GP, Moreno CG, Van Look Sexual and reproductive health: a matter of life and death. Lancet. 2006;368(9547):1595–1607. doi: 10.1016/S0140-6736(06)69478-6. [DOI] [PubMed] [Google Scholar]
- 29.Khan S, Mishra V. Youth Reproductive and Sexual Health, DHS Comparative Reports. Calverton, MD, USA: Macro International, Inc; 2008. p. 19. [Google Scholar]
- 30.DiCenso A, Gordon G, Willan A, Griffith L. Interventions to Reduce Unintended Pregnancies among Adolescents: Systematic Review of Randomized Controlled Trials. British Medical Journal. 2002;324:1426. doi: 10.1136/bmj.324.7351.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bersamin MM, Fisher DA, Walker S, Douglas LH, Joel WG. Defining virginity and abstinence: adolescents’ interpretations of sexual behaviours. Journal of Adolescent Health. 2007;41(2):182–188. doi: 10.1016/j.jadohealth.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Masatu MC, Kazaura MR, Ndeki S, Mwampambe R. Predictors of risky sexual behaviour among adolescents in Tanzania. AIDS and Behavior. 2009;13(1):94–99. doi: 10.1007/s10461-007-9292-x. (17.) [DOI] [PubMed] [Google Scholar]
- 33.Kawai K, Kaaya SF, Kajula L, Mbwambo J, Kilonzo GP, Fawzi WW. Parents’ and teachers’ communication about HIV and sex in relation to the timing of sexual initiation among young adolescents in Tanzania. Scandinavian Journal of Public Health. 2008;36(8):879–888. doi: 10.1177/1403494808094243. [DOI] [PubMed] [Google Scholar]
- 34.Guttmacher Institute. Protecting the next generation in Uganda: New evidence on Adolescent Sexual and Reproductive health needs 2008 [Google Scholar]
- 35.United Nations. Human Development Report. New York: 2008. [Google Scholar]
- 36.IOM. International Organization for Migration. Gulu District IDP Camps survey; Kampala: 2003. p. 30. [Google Scholar]
- 37.Nathan Okurut, Odwee Jonathan JAO, Adebua Asaf. The African Economic Research Consortium; Nairobi Kenya: 2002. Determinants of Regional Poverty in Uganda. http://www.aercafrica.org/documents/rp122.pdf. [Google Scholar]
- 38.Hargreaves JR, Morison LA, Kim JC, Bonell CP, Porter1 JDH, Watts C, Busza J, Phetla G, Pronyk PM. The association between school attendance, HIV infection and sexual behaviour among young people in rural South Africa. Journal of Epidemiology and Community Health. 2008;62(2):113–119. doi: 10.1136/jech.2006.053827. [DOI] [PubMed] [Google Scholar]
- 39.Bearinger LH, Sieving RE, Ferguson J, Sharma V. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. 2009;369(9568):1220–1231. doi: 10.1016/S0140-6736(07)60367-5. [DOI] [PubMed] [Google Scholar]
- 40.UNFPA Timor-Leste- Adolescent Sexual and Reproductive Health Curriculum for Tomor-Leste. http://countryoffice.unfpa.org/timorleste/2012/03/23/4725/adolescent_sexual_and_reproductive_health_carriculum_for_timor_leste/
- 41.Akpabio II, Asuzu MC, Fajemilehin BR, Ofi AB. Effects of school health nursing education interventions on HIV/AIDS-related attitudes of students in Akwa Ibom State, Nigeria. Journal of Adolescent Health. 2009;44(2):118–123. doi: 10.1016/j.jadohealth.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 42.Thato R, Jenkins RA, Dusitsin N. Effects of the culturally-sensitive comprehensive sex education programme among Thai secondary school students. Journal of Advanced Nursing. 2008;62(4):457–469. doi: 10.1111/j.1365-2648.2008.04609.x. [DOI] [PubMed] [Google Scholar]
- 43.Minaya J, Owen-Smith A, Herold J. The impact of sex education on HIV knowledge and condom use among adolescent females in the Dominican Republic. International Journal of Adolescent Medicine and Health. 2008;20(3):275–282. doi: 10.1515/ijamh.2008.20.3.275. [DOI] [PubMed] [Google Scholar]
- 44.Givaudan M, Leenen I, Fons JR, Van De V, Ype H, Poortinga PS. Longitudinal study of a school based HIV/AIDS early prevention program for Mexican adolescents, Psychology. Health and Medicine. 2008;13(1):98–110. doi: 10.1080/13548500701295256. [DOI] [PubMed] [Google Scholar]
- 45.Pick S, Givaudan M, Sirkin J, Ortega I. Communication as a protective factor: evaluation of a life skills HIV/AIDS prevention program for Mexican elementary-school students. AIDS Education and Prevention. 2007;19(5):408–421. doi: 10.1521/aeap.2007.19.5.408. [DOI] [PubMed] [Google Scholar]
- 46.Lumuli M, Kayombo JK. Assessing acceptability of parents/guardians of adolescents towards introduction of sex and reproductive health education in schools at Kinondoni Municipal in Dar es Salaam city. School of Medicine, Muhimbili University of Health & Allied Sciences (MUHAS), Dar es Salaam, Tanzania. East Afr J Public Health. 2008;5 (1):26–31. doi: 10.4314/eajph.v5i1.38973. 18669120 Cit:1. [DOI] [PubMed] [Google Scholar]
- 47.Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: their impact on sexual behaviors of young people throughout the world. Journal of Adolescent Health. 2007;40(3):206–217. doi: 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- 48.Nair MKC, Leena ML, Mini KP, Vijayan H, Babu G, Russell PS, Thankachi Y. Attitudes of parents and teachers towards adolescent reproductive and sexual health education. Indian J Pediatr. 2012;79(Suppl 1):S60–3. doi: 10.1007/s12098-011-0436-7. 21614606. [DOI] [PubMed] [Google Scholar]
- 49.Mwambete DK, Mtaturu Z. Knowledge of sexually transmitted diseases among secondary school students in Dar es Salaam, Tanzania. Afr Health Sci. 2006;6(3):165–169. doi: 10.5555/afhs.2006.6.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thankachi Y, Nair MKC, Paul Mini K, Leena ML, George Babu, Russell PS, Vijayan Pillai H. Effectiveness of a reproductive sexual health education package among school going adolescents. Indian J Pediatr. 2012;79(Suppl 1):S64–8. 21617909. doi: 10.1007/s12098-011-0433-x. [DOI] [PubMed] [Google Scholar]
- 51.Katoanga SF. Situation analysis of adolescent reproductive health in selected Pacific Island countries. Paper presented at the Inter-country Workshop on Adolescent Reproductive Health for East and South East and the Pacific Island Countries; 27 April to 3 May 2000; 2000. p. 20. [Google Scholar]
- 52.Alexandra McManus, Dhar Lipi. Knowledge, perception and attitude of adolescent girls towards STIs/HIV, safer sex and sex education: A cross sectional survey of urban adolescent school girls in South Delhi, India. 2008 doi: 10.1186/1472-6874-8-12. Published online 2008 July 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Valley Research Group. Reproductive health awareness, attitudes and behaviour of adolescents in Nepal. Kathmandu: UNFPA; 1999. p. 110. [Google Scholar]