Abstract
There are limited data evaluating the relationship between influenza treatment and hospitalization duration. Our purpose assessed the association between different treatments and hospital stay among Korean pediatric influenza patients. Total 770 children ≤ 15 yr-of-age hospitalized with community-acquired laboratory-confirmed influenza at three large urban tertiary care hospitals were identified through a retrospective medical chart review. Demographic, clinical, and cost data were extracted and a multivariable linear regression model was used to assess the associations between influenza treatment types and hospital stay. Overall, there were 81% of the patients hospitalized with laboratory-confirmed influenza who received antibiotic monotherapy whereas only 4% of the patients received oseltamivir monotherapy. The mean treatment-related charges for hospitalizations treated with antibiotics, alone or with oseltamivir, were significantly higher than those treated with oseltamivir-only (P < 0.001). Influenza patients treated with antibiotics-only and antibiotics/oseltamivir combination therapy showed 44.9% and 28.2%, respectively, longer duration of hospitalization compared to those treated with oseltamivir-only. Patients treated with antibiotics, alone or combined with oseltamivir, were associated with longer hospitalization and significantly higher medical charges, compared to patients treated with oseltamivir alone. In Korea, there is a need for more judicious use of antibiotics, appropriate use of influenza rapid testing.
Graphical Abstract
Keywords: Influenza, Human; Hospitalizations; Oseltamivir; Therapeutics; Child
INTRODUCTION
Influenza viruses are common respiratory pathogens among all age groups and are major causes of excess respiratory disease-associated hospitalizations, mortality, and costs during annual epidemics and pandemics (1, 2). Children with underlying medical conditions and younger age, especially ≤ 5 yr olds, are at high risk for severe influenza-associated outcomes (3, 4, 5). Furthermore, pediatric influenza exerts a considerable socioeconomic burden in terms of direct and indirect costs, and excess health-care utilization (6, 7, 8). Children also serve as a reservoir for household transmission of influenza, causing secondary illness in the family (8, 9).
Currently available neuraminidase inhibitors are effective in reducing influenza-associated illness duration, severity, complication risks, influenza-related mortality and even antibiotic use (10, 11, 12). Often patients hospitalized with influenza-related illnesses are inappropriately treated with antibiotics as prophylactic and empiric therapy, as indicated by increased antibiotic prescriptions during the influenza season (10, 13). The emergence of drug resistance and over-prescription of antibiotics are growing public health issues, as well as increased healthcare costs without reductions in illness duration (14, 15, 16).
Republic of Korea (ROK) has a relatively high influenza vaccination coverage rate of nearly 40% in the general population (17) and this is higher than the vaccination rate among children hospitalized with acute respiratory infection in the US (18) and similar to that of healthy Ontario children in Canada (19). Nonetheless, Korea still suffers from considerable disease burden of influenza in children, where 20% of viral respiratory disease hospitalizations are due to influenza virus infection (20). This study is the first to address treatment patterns in influenza-associated hospitalizations among Korean children. To address existing gaps in knowledge regarding childhood influenza in Korea, we evaluated the association between hospitalization duration and treatment type, using clinical and epidemiological data from children hospitalized with laboratory-confirmed influenza. We also described the economic burden by calculating medical charges incurred during hospitalization by treatment type.
MATERIALS AND METHODS
Study hospital and cohort
A retrospective review of medical records for patients admitted or treated from February 2004 through June 2007 was conducted at three academic, tertiary-care hospitals. Ansan, Anam, and Guro Hospitals, affiliated with Korea University (KU), serve the communities of Ansan city (a neighboring city of Seoul), and districts of Anam and Guro in Seoul, respectively. At these KU hospitals, nasal aspirate specimens were systematically collected from patients presenting with acute respiratory symptoms and routinely tested to identify adenovirus, parainfluenza, respiratory syncytial virus (RSV) and influenza A/B with virus. Additionally, selected patients were tested for influenza A/B and RSV by rapid antigen detection (Directigen EZ Flu A+B Test Kit, Becton-Dickinson, NJ, USA) at the clinicians' discretion.
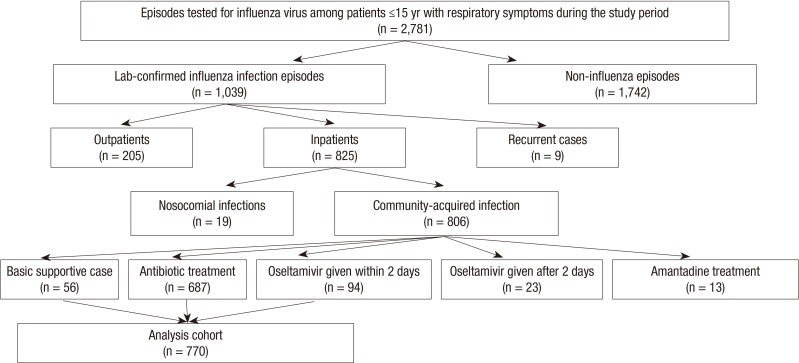
For this study, we included patients who: a) presented with respiratory symptoms at one of the KU hospitals, b) were ≤15 yr-of-age at the time of admission, and c) had laboratory-confirmation of influenza A/B. Children with mixed viral infections (with following viruses; influenza, RSV, parainfluenza, or adenovirus) and with recurrent episodes with the same virus type who returned to the hospital within two weeks from the date of the previous discharge or clinic visit were excluded from our analysis. Assembly of the study patient cohort is outlined in Fig. 1. During the 41 months, 1,039 episodes of laboratory-confirmed influenza were identified from the outpatient and inpatient departments of the three hospitals.
Fig. 1.
Flow chart describing the ascertainment of the patient cohort with hospitalization identified during the study period of February 2004-June 2007.
Virus detection
Viral culture had been performed using an enhanced cell culture method with fluorescent antibody detection. Specimens (200 µL) were inoculated onto R-Mix Ready Cells (Diagnostic Hybrids, NY, USA), and vials were centrifuged at 700×g for 60 min at room temperature. After overnight incubation at 35℃ in a CO2 incubator, cell monolayers were washed with phosphate-buffered saline, fixed with acetone, and stained with a respiratory virus fluorescent antibody pool, D3 DFA (Diagnostic Hybrids). When virus specific fluorescence was noted, virus identification was performed by using individual monoclonal antibodies (Diagnostic Hybrids). The presence of three or more cells per well with specific apple-green fluorescence was considered positive identification. Screenings were done on day 1 and 3. Additionally, selected patients were tested for influenza A/B and RSV by rapid antigen detection (Directigen EZ Flu A+B Test Kit, Becton-Dickinson) at the clinicians' discretion.
Data collection
Via medical chart reviews of 1,039 episodes of community-acquired laboratory-confirmed influenza, we extracted the following demographic and clinical variables from the KU hospital electronic medical information database: influenza virus type, dates of admission and discharge, diagnoses, signs and symptoms, body temperature, duration of fever, pre-existing medical conditions, vital signs, hematologic and radiologic test results, treatment information, and discharge status. Direct hospital medical charges were obtained from the hospital billing/registry office. Treatment-related fee was composed of charges for injection, medication, treatment material, physical therapy, surgery, anesthesia, and blood infusion. Testing fee consisted of charges for routine and specially-ordered laboratory and diagnostic tests. Hospital admission fee included admission, food, and room charges. They were summed for the total hospital charges incurred and currency was converted from Korean Won (KRW) to US dollar with the average exchange rate during study period of 1 KRW=0.0007 US$.
The diagnosis at admission was categorized by the primary clinical manifestation. Diagnoses of pneumonia, bronchitis, croup, and asthma were grouped as lower respiratory tract illness (LRTI), while acute pharyngitis, sinusitis, and laryngitis were grouped as upper respiratory illness (URI). Urinary tract infection, sepsis, and neurologic (e.g., convulsions, febrile seizure, Guillain-Barré Syndrome), gastrointestinal (e.g., diarrhea, acute gastroenteritis), and cardiovascular conditions were grouped as 'non-respiratory' diseases. An axillary (tympanic membrane) temperature≥37.5 (37.8)℃ was defined as fever. Fever duration included the febrile days prior to admission.
Variable construction and statistical analysis
The analysis examined the relationship between the length of hospital stay (LOS) and the different types of treatment administered during hospitalization, when adjusted for potential confounding factors. Nosocomial influenza episodes with virus detection≥7 days after the date of admission were excluded from the analysis sample. In accordance with current guidelines of influenza treatment, episodes treated with oseltamivir (Tamiflu®, Roche Pharmaceuticals, Basel, Switzerland) outside of the recommended two-day window after the onset of symptoms, and episodes treated with amantadine were excluded.
The mean peak body temperature for study patients measured during hospitalization, 38.6℃, was used as the cutoff value to create a dichotomous variable indicating elevated body temperature. Normal white blood cell (WBC) count was defined as WBC of 5,000-19,500/µL for children≤10 months-of-age; 6,000-17,500/µL for those 11 months-2 yr-of-age; 5,500-15,500/µL for children 3-7 yr-of-age; and 4,500-13,500 (11,500)/µL for children 8-13 (14-15) yr-of-age (21). Leukopenia and leukocytosis were below the lower and above the upper values of the normal WBC range, respectively. Complications that occurred during hospitalization were categorized into secondary bacterial pneumonia, other secondary bacterial infection, encephalitis, or exacerbation of the pre-existing medical conditions. Pre-existing medical conditions were congenital diseases and acquired diseases (e.g., asthma, and cancer). Binary variables were created for the presence or absence of complications and pre-existing conditions.
Influenza hospitalizations with complete data were divided into four treatment categories: oseltamivir-only, antibiotics-only, antibiotics-plus-oseltamivir, and supportive-care without antiviral or antibiotic treatment. Categorical pair-wise comparisons were made with reference to the oseltamivir-only group using chi-square or the Fisher's exact tests with significance at P<0.05. Comparison of continuous variables was performed using the Student's t-test. However, for hospital charges with skewed distributions, the Mann-Whitney test was used to make pair-wise comparisons with reference to the oseltamivir-only group. Bivariate analyses were performed to identify potential confounders and covariates of interest for the regression model, using SAS® version 9.0 (SAS Institute, Cary, NC, USA).
To adjust for variability in initial severity of illness, clinical parameters such as temperature measured at admission, presenting signs and symptoms (i.e., expectoration, diarrhea, headache, injected tympanic membrane, sore throat, vomiting, breathing difficulty, rales or wheezing), admission diagnosis, laboratory test results (i.e. WBC/neutrophil counts and chest infiltrates) were compared across treatment groups. Construction of the model with these variables allows statistical adjustment for initial variability in clinical presentation. As potential confounders, presence of underlying medical conditions and occurrence of complications during hospitalization, were included as dichotomous variables in the model to control for variations in disease presentation at admission and during clinical course that may have guided treatment-related decisions. Some variables that are closely related were assessed for multicollinearity and were limited for inclusion in the regression model. Multivariable linear regression was performed with the outcome as the log-transformed, hospitalization duration and categorical variable of influenza treatments as the main predictor. The β, % change in treatment-related charges, and 95% confidence intervals (CI) were reported.
Ethics statement
Study approvals were obtained from the institutional review boards of the KU Ansan Hospital (IRB No. ED0744) and the International Vaccine Institute (IRB No. 2007-008). The exemption of informed consent and assent forms was allowed by both IRBs because this study was based on a retrospective review and the patient IDs were removed from the DB provided by the hospital records office.
RESULTS
Patient characteristics
Of the 770 hospitalizations in our analysis sample, 77% were ≤ 5 yr-of-age (590/770) and there were twice more influenza A positive episodes than influenza B episodes (62% vs 34%), with few influenza A and B co-infections (Table 1). The distributions of hospitalizations by age and gender in the oseltamivir-only group were similar to those in other treatment groups. The distributions of influenza hospitalizations by virus type and admission diagnosis category were significantly different when treatment groups were compared to the oseltamivir-only group. The patients in the antibiotics-only, antibiotics-plus-oseltamivir, and supportive-care groups were more likely to be diagnosed at admission with LRTI than the oseltamivir-only group (57%, 42%, and 54% vs 19%, respectively).
Table 1.
Characteristics of the analysis cohort of hospitalizations with laboratory-confirmed influenza identified during February 2004-June 2007 in Republic of Korea
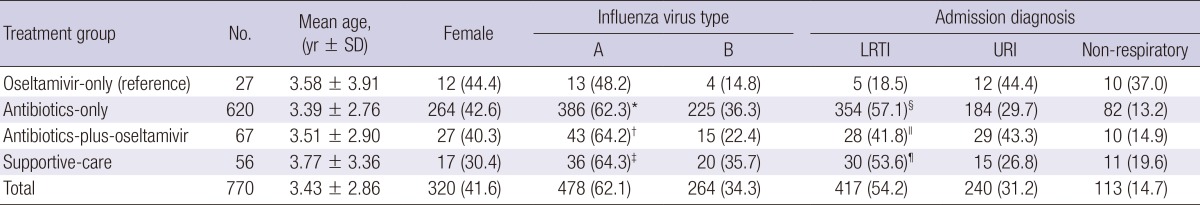
Values are No. (%) unless otherwise noted. *P<0.001, for comparison between the antibiotics-only vs oseltamivir-only treatment groups; †P=0.050, for comparison between the antibiotics-plus-oseltamivir vs oseltamivir-only treatment groups; ‡P<0.001, for comparison between the supportive-care vs oseltamivir-only treatment groups; §P<0.001, for comparison between the antibiotics-only vs oseltamivir-only treatment groups; ∥P=0.025, for comparison between the antibiotics-plus-oseltamivir vs oseltamivir-only treatment groups; ¶P=0.010, for comparison between the supportive-care vs oseltamivir-only treatment groups. LRTI, lower respiratory tract illness; URI, upper respiratory illness.
Clinical characteristics
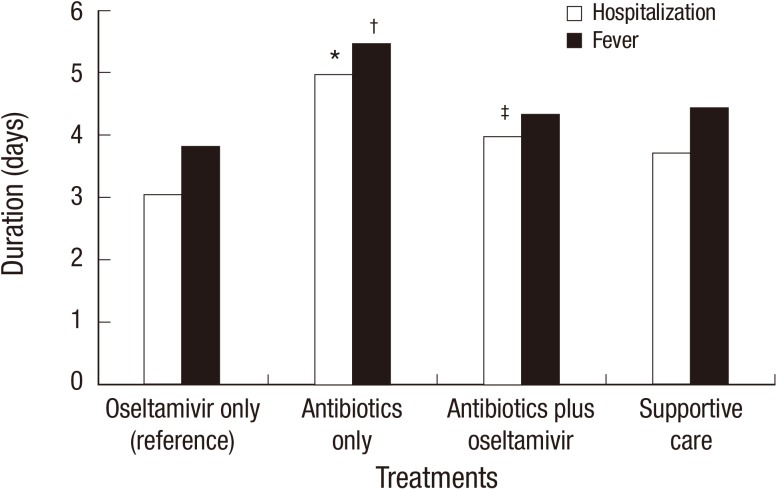
Among the total of 770 patients, 27 were treated with oseltamivir-only, 620 were treated with antibiotics-only, 67 received antibiotics-plus-oseltamivir and 56 patients received supportive-care. The mean LOS for patients in the antibiotics-only and antibiotics-plus-oseltamivir groups were significantly longer compared to the oseltamivir-only group (5.0 and 4.0 vs 3.0 days, respectively) (Fig. 2). The mean fever duration was significantly longer in the antibiotics-only group compared to the oseltamivir-only group (5.5 vs 3.8 days). Patients in the oseltamivir-only group were more likely to have received influenza rapid diagnostic tests (IRDT) than the antibiotics-only, antibiotics-plus-oseltamivir, and supportive-care groups (82% vs 3%, 55%, and 16%, respectively) (Table 2). Patients who presented with rales/wheezing were found more commonly in those three treatment groups than in the oseltamivir-only group (38%, 37%, and 41% vs 7%). Patients presenting with pharyngeal injection were significantly less common in the antibiotics-only group, compared to the oseltamivir-only group (73% vs 93%). Overall, 12% of patients (n=96/770) suffered from complications during hospitalization, and 45% (n=43/96) developed secondary bacterial pneumonia or other bacterial infection with few cases of neurologic problems (e.g. encephalitis) and exacerbation of pre-existing medical conditions (data not shown).
Fig. 2.
Mean length of hospital stay and duration of fever in days for 770 hospitalizations with laboratory-confirmed influenza by the treatment type, February 2004-June 2007. *P < 0.001, for comparison of the mean duration of hospital stay in antibiotics-only (5.0 days the oseltamivir-only treatment groups (3.0 days); †P < 0.001, for comparison of the mean fever duration in antibiotics-only (5.5 days) vs the oseltamivir-only treatment groups (3.8 days); ‡P = 0.012, for comparison of the mean duration of hospital stay in antibiotics-plus-oseltamivir (4.0 days the oseltamivir-only treatment groups (3.0 days).
Table 2.
Clinical characteristics of the 770 hospitalizations with laboratory-confirmed influenza treated with antiviral or antibiotic medication from February 2004 to June 2007
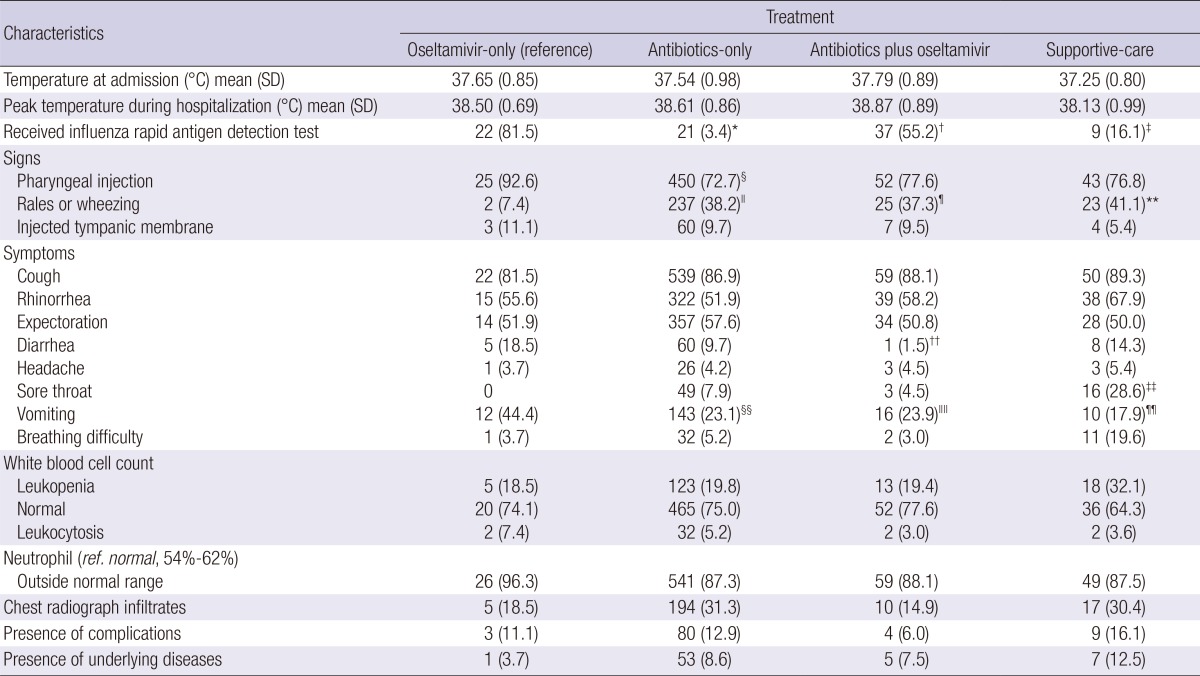
Values are No. (%) unless otherwise noted. The 95% confidence intervals (95% CI) were reported. *P<0.001, for comparison between the antibiotics-only vs oseltamivir-only treatment groups; †P=0.017, for comparison between the antibiotics-plus-oseltamivir vs oseltamivir-only treatment groups; ‡P<0.001, for comparison between the supportive-care vs oseltamivir-only treatment groups; §P=0.022, for comparison between the antibiotics-only vs oseltamivir-only treatment groups; ∥P=0.001, for comparison between the antibiotics-only vs oseltamivir-only treatment groups; ¶P=0.004, for comparison between the antibiotics-plus-oseltamivir vs oseltamivir-only treatment groups; **P=0.002, for comparison between the supportive-care vs oseltamivir-only treatment groups; ††P=0.002, for comparison between the antibiotics-plus-oseltamivir vs oseltamivir-only treatment groups; ‡‡P=0.002, for comparison between the supportive-care vs oseltamivir-only treatment groups; §§P=0.011, for comparison between the antibiotics-only vs oseltamivir-only treatment groups; ∥∥P=0.049, for comparison between the antibiotics-plus-oseltamivir vs oseltamivir-only treatment groups; ¶¶P=0.010, for comparison between the supportive-care vs oseltamivir-only treatment group.
Hospitalization-associated medical charges
The mean treatment-related charges (US$171 and $111 vs $67, P<0.001 and <0.001, respectively) and the hospital admission charges (US$287 and $240 vs $176, P<0.001 and 0.017, respectively) were significantly higher in the groups treated with antibiotics-only and antibiotics-plus-oseltamivir, compared to the group treated with oseltamivir-only (Table 3). The mean total charges for hospitalizations treated with antibiotics-only and antibiotics-plus-oseltamivir were significantly higher than charges for hospitalizations treated with oseltamivir-only (US$753 and $623 vs $508, P<0.001 and 0.059, respectively).
Table 3.
Hospital charges (mean, SD) of patients with laboratory-confirmed influenza by treatment type, February 2004-June 2007
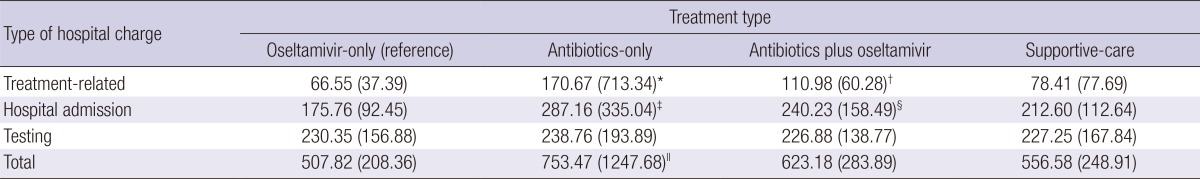
Mean values and standard deviation (in parenthesis) are reported in US$ with exchange rate of 1 KRW=0.0007 US$. *P<0.001, for comparison of the mean treatment-related fees in antibiotics-only vs the oseltamivir-only treatment groups; †P<0.001, for comparison of the mean treatment-related fees in antibiotics-plus-oseltamivir vs the oseltamivir-only treatment groups; ‡P<0.001, for comparison of the mean hospital admission charges in antibiotics-only vs the oseltamivir-only treatment groups; §P=0.017, for comparison of the mean hospital admission charges in antibiotics-plus-oseltamivir vs the oseltamivir-only treatment groups; ∥P<0.001, for comparison of total hospital charges in antibiotics-only vs the oseltamivir-only treatment groups.
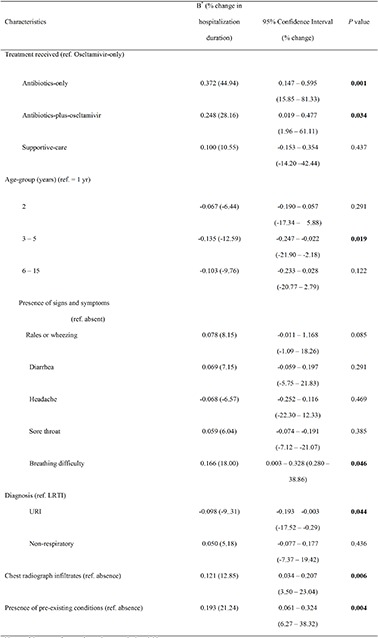
Predictors of increased hospital stay
Compared with the oseltamivir-only group, children treated with antibiotics-only showed 44.9% longer hospitalization compared to those who received oseltamivir-only (95% CI, 15.85-81.33; P value=0.001) (Table 4) in multivariate analysis. Treatment with antibiotics-plus-oseltamivir also showed a significantly longer LOS, compared to the oseltamivir-only group, by 28.2% (95% CI, 1.96-61.11; P value=0.034). From the univariate analysis, patients who received the antibiotics-only therapy showed 55.8% longer hospitalization compared to those who received oseltamivir-only (95% CI, 27.99-89.66; P value<0.001) (data not shown). Patients who received antibiotics-plus-oseltamivir therapy also showed a significantly longer LOS by 28.5%, compared to the oseltamivir-only group (95% CI, 2.24-61.48; P value=0.032).
Table 4.
Multivariate regression analysis of association between treatment type received and hospitalization duration among 770 hospitalizations with laboratory-confirmed influenza in Republic of Korea, February 2004 through June 2007
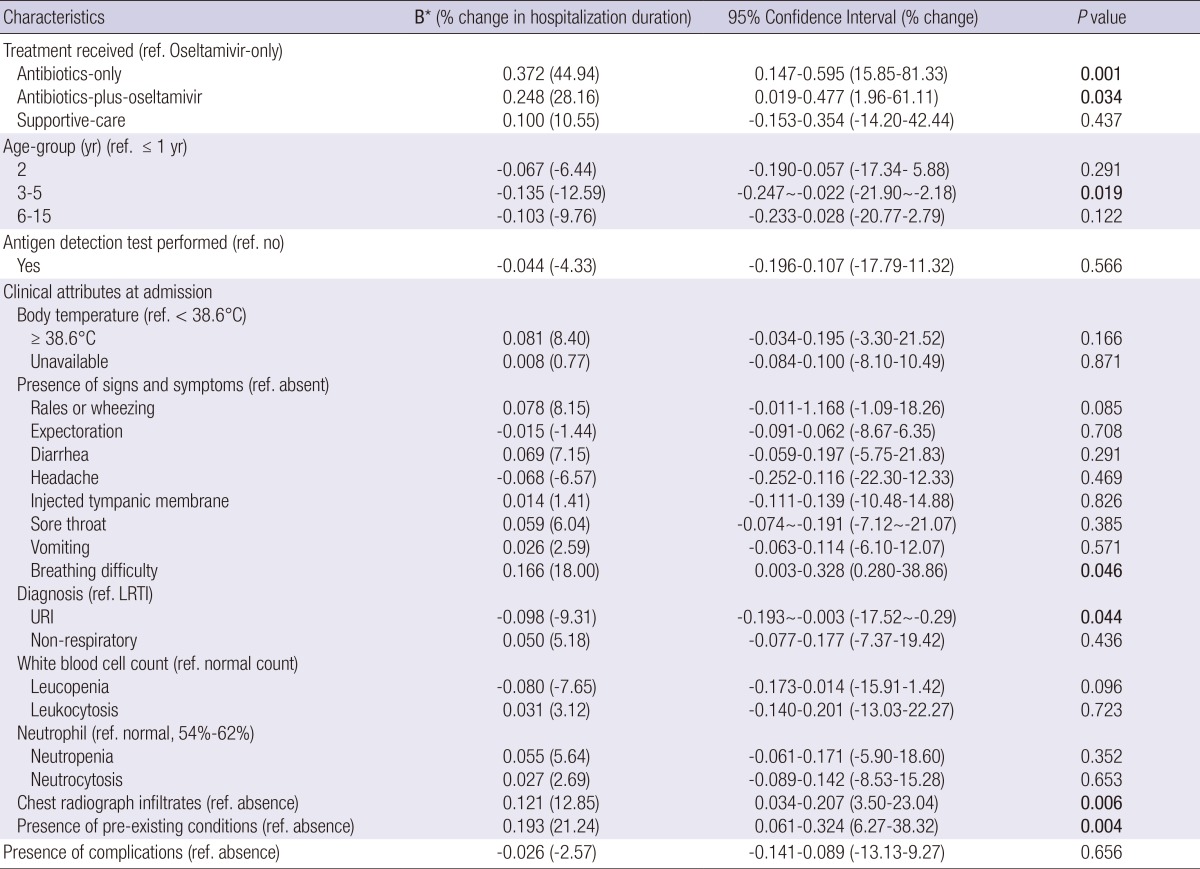
Note. ref denotes reference for each categorical variable. *In addition to the variables listed in the table, the multivariate analysis was adjusted for sex, influenza season, presence of signs/symptoms (chills, rales/wheezing, cough, expectoration, rhinorrhea, diarrhea, sore throat, pharyngeal injection, rhonchi, and headache).
Children in the 3-5 yr-old groups showed to have 12.6% shorter LOS, compared to infants≤1 yr old (95% CI, -21.9~-2.18; P value=0.019). Patients with dyspnea had 18.0% longer LOS compared to those without dyspnea (95% CI, 0.28-38.86; P value=0.046), while those children with admission diagnosis categorized as URI showed 9.3% shorter LOS compared to those with LRTI (95% CI, -17.52~-0.29; P value=0.044). Also, the presence of chest radiograph infiltrates and pre-existing medical conditions were significant indicators of lengthened hospitalization by 12.9% and 21.3%, respectively (95% CI, 3.50-23.04 and 6.27-38.32, respectively).
DISCUSSION
This is the fir st study to compare influenza treatments in relation to hospitalization-associated outcomes among Korean children. Our findings suggest that antibiotic therapy, alone or in combination with oselatmivir, is associated with longer hospitalization, compared to oseltamivir monotherapy, among children with laboratory-confirmed influenza. Also, our data showed that the lowest mean total hospital charges, as well as hospital admission and treatment-related charges, occurred among patients treated with oseltamivir-only among different influenza treatment options. In our sample of influenza hospitalizations, 81% of patients received antibiotic-only while only 4% received oseltamivir-only. Patients who received oseltamivir monotherapy were more likely to be laboratory-confirmed with IRDT in addition to culture tests than patients who received other treatments.
Our results are consistent with findings from Kaiser et al. and Gums et al. that demonstrated the effectiveness of oseltamivir in reducing the length of hospitalization (10, 22); and Sato, et al. that showed a significantly shorter duration of fever in oseltamivir-treated influenza A patients (12). Our data showed a significantly longer mean LOS for patients in the antibiotics-only and antibiotics-plus-oseltamivir groups compared to the oseltamivir-only group. Less timely onset of antibiotic therapy could play a role in increased LOS, however, 99% (n=683) of 687 antibiotics-treated patients received antibiotics within 3 days of admission in our data, indicating the timing of antibiotic therapy was unlikely the cause of observed association. In the antibiotics-plus-oseltamivir group, 59 patients out of 67 had received antibiotics before oseltamivir in our data. While this may be explained by the fact that these patients may have had clinical indications of bacterial pneumonia or other secondary infections, this antibiotic prescription preceding oseltamivir treatment could have led to delayed onset of oseltamivir therapy and consequently lengthening the patients' LOS.
Several factors, indicating severe clinical course (e.g., complication) and initial differences in clinical presentation of illness, could have potentially influenced treatment-related decisions and were taken into account in our multivariate modeling. It is possible that additional confounding variables that were not measured in this study may explain the relationship. However, the observed strength of the relationship of oseltamivir-only compared to antibiotics-only and antibiotics-plus-oseltamivir groups (i.e., 45% and 28% increases in LOS with the P value of 0.001 and 0.034, respectively) makes it unlikely that our findings are a result of residual confounding not controlled for in our models. While these findings are consistent with several reports of reduced hospitalization associated with oseltamivir treatment (10, 22), no previous studies have shown that antibiotic treatments, compared to oseltamivir therapy, is associated with longer LOS in children with laboratory-confirmed influenza.
Our finding that hospital charges were lowest among oseltamivir-only treated children also corresponds with previous studies reporting that unnecessary costs may incur among influenza-like illness (ILI) patients treated with antibiotics (13, 16, 23) while oseltamivir is the cost-effective choice of influenza treatment (24). The cost of influenza-related hospitalization in our data was shown to be lower than previously estimated in other countries (6, 7, 25). This is explained by the fact that ROK has universal population coverage by the National Health Insurance that subsidizes physician fees, hospital and prescription drugs charges via a compulsory healthcare plan (26). Despite the number of studies that have previously reported an indiscriminant and inappropriate use of antibiotics (16, 27, 28), antibiotics were demonstrated to still be a primary treatment option for children hospitalized with influenza in ROK. Observed treatment patterns may be explained, in part, by the absence of standardized treatment guidelines for seasonal influenza in ROK.
In addition to the absence of the treatment guidelines, infrequent use of the IRDT during the study period could lead to observed treatment patterns. Without test for viral pathogen, the uncertainty of diagnosis of children with influenza-like illness frequently leads clinicians to prescribe antibiotics to the children with lower respiratory symptoms and signs. Our data showed that the oseltamivir-treated children were more likely to have been tested with IRDT compared to the children treated with antibiotics or supportive-care. Although all of our study subjects were ultimately proven to have laboratory-confirmed influenza, children who were treated with antibiotics or only supportive-care may have been initially suspected of having bacterial infection or non-viral respiratory illness. Such children were less likely to undergo testing by IRDT than those oseltamivir-treated, who were more likely to be confirmed with influenza on admission with IRDT. Our results as well as previous studies support the notion that IRDT are an important tool for guiding influenza treatment decision-making (29, 30). Distinguishing influenza from other respiratory diseases in children as well as identifying influenza with atypical clinical presentations is a well-recognized clinical challenge (31). As a result, increased accessibility of IRDT is a recognized priority among clinicians in ROK and elsewhere that is likely to improve patient treatment regimens and clinical outcomes, as well as potentially reduce antibiotic usage and additional laboratory testing (29, 30, 32).
In our study, we adjusted for clinical characteristics in our multivariable analysis that were previously linked to higher influenza viral load, prolonged hospitalization, secondary pneumonia, as well as other viral or bacterial complications (33, 34, 35, 36, 37, 38). We found no consistent treatment-related patterns with respect to disease severity of illness when compared clinical presentation by treatment type. For example, rales/wheezing were more commonly present among patients treated with antibiotics-only, antibiotics-plus-oseltamivir, and even supportive-care, compared to those treated with oseltamivir-only, Also, chest infiltrate, which may suggest bacterial pneumonia (39), was not significantly more common in antibiotics or antibiotics-plus-oseltamivir groups compared to the oseltamivir-only group. There was no currently available and validated severity of illness index for pediatric influenza.
In this retrospective study, our data extraction was limited to the information available on medical charts. Due to the observational nature of our study, we cannot conclude that oseltamivir shortened the LOS among hospitalized patients with influenza. Although lengthened hospitalization practically directly reflects the burden of influenza requiring hospitalization, clinical data may not entirely capture the influenza disease burden. In clinical practice at KU hospitals, the hospitalizations diagnosed with mild conditions (e.g., pharyngitis) were less likely to be treated with antibiotics, while those with more severe findings, such as rales or chest infiltrate that prompt clinicians to suspect bacterial pneumonia, were often treated with antibiotics. Thus, variability in illness severity at admission influencing clinical diagnosis was the most important confounder of this relationship and various clinical attributes were controlled for in the analysis.
Despite these limitations, a robust analysis of the treatment type was possible due to: 1) three complete and consecutive viral seasons; 2) a relatively large sample of laboratory-confirmed influenza hospitalizations; 3) the geographic and patient mix of patients from community and academic hospitals in different parts of ROK, providing a representative sample for greater generalizability of results; and 4) no oseltamivir resistance in the viral strains during our study period in ROK (anecdotal reports), minimizing the influence of oseltamivir resistance on the study outcomes. Prescription patterns could differ by clinician and facility, but the three hospitals under the umbrella of KU had highly uniform standards in patient management and treatment regimen. Moreover, all subjects were culture-confirmed, in addition to some that had undergone IRDT, ensuring uniformity in the levels of sensitivity and specificity of influenza diagnostics. Considering the lack of data from direct comparison between antibiotic and oseltamivir treatments, our study provides a realistic illustration of influenza treatment in relation to increased hospitalization by comparing treatment options used in clinical practice in ROK. As suggested by Falagas et al., there is a need for comparative and randomized studies (40), our study findings will serve as a platform for further assessment of different influenza treatment options in clinical practice.
In ROK, the predominantly circulating strains were A/H3N2 in 2004-05, A/H1N1 in 2005-06, and A/H3N2 in 2006-07 and there were no reported oseltamivir-resistant strains of influenza during the study period of 2004-07. Notably, in the January 2011 issue of the U.S. Centers for Disease Control and Prevention's Morbidity and Mortality Weekly Report, either oseltamivir or zanamivir was recommended for use in patients hospitalized with suspected or confirmed influenza, whether it is 2009 H1N1 virus, influenza A (H3N2) virus, or influenza B virus or when the influenza virus type or influenza A virus subtype is unknown (41). In ROK, there is limited number of oseltamivir treatment guidelines or recommendations for seasonal influenza. Also, IRDT is not routinely used in decision-makings of patient management, despite its well-known benefits (23, 32, 37). Lately, real time RT-PCR is used more often in many facilities in ROK, which means influenza infection could be detected in earlier stage of illness with better accuracy.
Recognizing that laboratory-confirmation of influenza at an earlier point of the course of hospitalization may be particularly important in pediatric influenza treatment (29, 42), our study suggests the need for appropriate use of IRDT and RT-PCR for seasonal influenza in ROK so that more vigilant and judicious antibiotics prescription could be practiced in the clinical setting.
ACKNOWLEDGMENTS
We thank the doctors and laboratory staff of Korea University's Ansan Hospitals for their participation in the retrospective pediatric influenza study in ROK. We thank collaborators at Myung Moon Pediatrics for their support, Dr. Betsy Foxman (School of Public Health at the University of Michigan, Ann Arbor), Dr. Bill Letson (Pediatric Dengue Vaccine Initiative), Ms. Sunheang Shin, and Ms. Deborah Hong, as well as the statisticians and administrative staff at the International Vaccine Institute for their helpful comments during the analysis and preparation of this manuscript.
Footnotes
This study was supported by funding from the Korean Center for Disease Control and Prevention (grant #: 2007-S2-E-003), as well as from the governments of Kuwait, Sweden, and the Republic of Korea.
The authors have no relevant financial relationships or potential conflicts of interest to disclose regarding the material discussed in this manuscript.
References
- 1.Molinari NA, Ortega-Sanchez IR, Messonnier ML, Thompson WW, Wortley PM, Weintraub E, Bridges CB. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25:5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 2.Newall AT, Scuffham PA. Influenza-related disease: the cost to the Australian healthcare system. Vaccine. 2008;26:6818–6823. doi: 10.1016/j.vaccine.2008.09.086. [DOI] [PubMed] [Google Scholar]
- 3.Neuzil KM, Wright PF, Mitchel EF, Jr, Griffin MR. The burden of influenza illness in children with asthma and other chronic medical conditions. J Pediatr. 2000;137:856–864. doi: 10.1067/mpd.2000.110445. [DOI] [PubMed] [Google Scholar]
- 4.Neuzil KM, Zhu Y, Griffin MR, Edwards KM, Thompson JM, Tollefson SJ, Wright PF. Burden of interpandemic influenza in children younger than 5 years: a 25-year prospective study. J Infect Dis. 2002;185:147–152. doi: 10.1086/338363. [DOI] [PubMed] [Google Scholar]
- 5.Bhat N, Wright JG, Broder KR, Murray EL, Greenberg ME, Glover MJ, Likos AM, Posey DL, Klimov A, Lindstrom SE, et al. Influenza-associated deaths among children in the United States, 2003-2004. N Engl J Med. 2005;353:2559–2567. doi: 10.1056/NEJMoa051721. [DOI] [PubMed] [Google Scholar]
- 6.Ampofo K, Gesteland PH, Bender J, Mills M, Daly J, Samore M, Byington C, Pavia AT, Srivastava R. Epidemiology, complications, and cost of hospitalization in children with laboratory-confirmed influenza infection. Pediatrics. 2006;118:2409–2417. doi: 10.1542/peds.2006-1475. [DOI] [PubMed] [Google Scholar]
- 7.Keren R, Zaoutis TE, Saddlemire S, Luan XQ, Coffin SE. Direct medical cost of influenza-related hospitalizations in children. Pediatrics. 2006;118:e1321–e1327. doi: 10.1542/peds.2006-0598. [DOI] [PubMed] [Google Scholar]
- 8.Neuzil KM, Hohlbein C, Zhu Y. Illness among schoolchildren during influenza season: effect on school absenteeism, parental absenteeism from work, and secondary illness in families. Arch Pediatr Adolesc Med. 2002;156:986–991. doi: 10.1001/archpedi.156.10.986. [DOI] [PubMed] [Google Scholar]
- 9.Heikkinen T, Silvennoinen H, Peltola V, Ziegler T, Vainionpaa R, Vuorinen T, Kainulainen L, Puhakka T, Jartti T, Toikka P, et al. Burden of influenza in children in the community. J Infect Dis. 2004;190:1369–1373. doi: 10.1086/424527. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser L, Wat C, Mills T, Mahoney P, Ward P, Hayden F. Impact of oseltamivir treatment on influenza-related lower respiratory tract complications and hospitalizations. Arch Intern Med. 2003;163:1667–1672. doi: 10.1001/archinte.163.14.1667. [DOI] [PubMed] [Google Scholar]
- 11.Nicholson KG, Aoki FY, Osterhaus AD, Trottier S, Carewicz O, Mercier CH, Rode A, Kinnersley N, Ward P. Efficacy and safety of oseltamivir in treatment of acute influenza: a randomised controlled trial: Neuraminidase Inhibitor Flu Treatment Investigator Group. Lancet. 2000;355:1845–1850. doi: 10.1016/s0140-6736(00)02288-1. [DOI] [PubMed] [Google Scholar]
- 12.Sato M, Saito R, Sato I, Tanabe N, Shobugawa Y, Sasaki A, Li D, Suzuki Y, Sato M, Sakai T, et al. Effectiveness of oseltamivir treatment among children with influenza A or B virus infections during four successive winters in Niigata City, Japan. Tohoku J Exp Med. 2008;214:113–120. doi: 10.1620/tjem.214.113. [DOI] [PubMed] [Google Scholar]
- 13.Neuzil KM, Mellen BG, Wright PF, Mitchel EF, Jr, Griffin MR. The effect of influenza on hospitalizations, outpatient visits, and courses of antibiotics in children. N Engl J Med. 2000;342:225–231. doi: 10.1056/NEJM200001273420401. [DOI] [PubMed] [Google Scholar]
- 14.Carrat F, Schwarzinger M, Housset B, Valleron AJ. Antibiotic treatment for influenza does not affect resolution of illness, secondary visits or lost workdays. Eur J Epidemiol. 2004;19:703–705. doi: 10.1023/b:ejep.0000036807.40105.97. [DOI] [PubMed] [Google Scholar]
- 15.Chidiac C, Maulin L. Using antibiotics in case of influenza. Med Mal Infect. 2006;36:181–189. doi: 10.1016/j.medmal.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Cao B, Li R, Liu YM, Cao ZX, Geng XQ, Lau LT, Lu J, Wu L, Cui SF, Bai RT, et al. The impact of antibiotic treatment in patients with influenza-like illness. Zhonghua Jie He He Hu Xi Za Zhi. 2008;31:483–487. [PubMed] [Google Scholar]
- 17.Kee SY, Lee JS, Cheong HJ, Chun BC, Song JY, Choi WS, Jo YM, Seo YB, Kim WJ. Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J Infect. 2007;55:273–281. doi: 10.1016/j.jinf.2007.04.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poehling KA, Edwards KM, Weinberg GA, Szilagyi P, Staat MA, Iwane MK, Bridges CB, Grijalva CG, Zhu Y, Bernstein DI, et al. The underrecognized burden of influenza in young children. N Engl J Med. 2006;355:31–40. doi: 10.1056/NEJMoa054869. [DOI] [PubMed] [Google Scholar]
- 19.Moran K, Maaten S, Guttmann A, Northrup D, Kwong JC. Influenza vaccination rates in Ontario children: implications for universal childhood vaccination policy. Vaccine. 2009;27:2350–2355. doi: 10.1016/j.vaccine.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 20.Kim YK, Nyambat B, Hong YS, Lee CG, Lee JW, Kilgore PE. Burden of viral respiratory disease hospitalizations among children in a community of Seoul, Republic of Korea, 1995 - 2005. Scand J Infect Dis. 2008;40:946–953. doi: 10.1080/00365540802398937. [DOI] [PubMed] [Google Scholar]
- 21.Pee SY, Choi Y, Lee BC, Lee HJ, An HS, Hwang TJ, Lee SY, Seo JG, Oh SH, Hwang YS. Hongchangeui textbook of pediatrics. 8th ed. Seoul: Korean Textbook Press; 2004. [Google Scholar]
- 22.Gums JG, Pelletier EM, Blumentals WA. Oseltamivir and influenza-related complications, hospitalization and healthcare expenditure in healthy adults and children. Expert Opin Pharmacother. 2008;9:151–161. doi: 10.1517/14656566.9.2.151. [DOI] [PubMed] [Google Scholar]
- 23.Ciesla G, Leader S, Stoddard J. Antibiotic prescribing rates in the US ambulatory care setting for patients diagnosed with influenza, 1997-2001. Respir Med. 2004;98:1093–1101. doi: 10.1016/j.rmed.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 24.Reisinger K, Greene G, Aultman R, Sander B, Gyldmark M. Effect of influenza treatment with oseltamivir on health outcome and costs in otherwise healthy children. Clin Drug Investig. 2004;24:395–407. doi: 10.2165/00044011-200424070-00003. [DOI] [PubMed] [Google Scholar]
- 25.Hassan F, Lewis TC, Davis MM, Gebremariam A, Dombkowski K. Hospital utilization and costs among children with influenza, 2003. Am J Prev Med. 2009;36:292–296. doi: 10.1016/j.amepre.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 26.Jeong HS. Health care reform and change in public-private mix of financing: a Korean case. Health Policy. 2005;74:133–145. doi: 10.1016/j.healthpol.2004.12.017. [DOI] [PubMed] [Google Scholar]
- 27.Ploin D, Gillet Y, Morfin F, Fouilhoux A, Billaud G, Liberas S, Denis A, Thouvenot D, Fritzell B, Lina B, et al. Influenza burden in febrile infants and young children in a pediatric emergency department. Pediatr Infect Dis J. 2007;26:142–147. doi: 10.1097/01.inf.0000253062.41648.60. [DOI] [PubMed] [Google Scholar]
- 28.Low D. Reducing antibiotic use in influenza: challenges and rewards. Clin Microbiol Infect. 2008;14:298–306. doi: 10.1111/j.1469-0691.2007.01910.x. [DOI] [PubMed] [Google Scholar]
- 29.Noyola DE, Demmler GJ. Effect of rapid diagnosis on management of influenza A infections. Pediatr Infect Dis J. 2000;19:303–307. doi: 10.1097/00006454-200004000-00008. [DOI] [PubMed] [Google Scholar]
- 30.De La Rocque F, Lécuyer A, Wollner C, d'Athis P, Pecking M, Thollot F, Cohen R. Impact of influenza rapid diagnostic tests (IRDT) on the diagnosis of influenza and on the management of influenza in children in ambulatory pediatric setting. Arch Pediatr. 2009;16:288–293. doi: 10.1016/j.arcped.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Peltola V, Ziegler T, Ruuskanen O. Influenza A and B virus infections in children. Clin Infect Dis. 2003;36:299–305. doi: 10.1086/345909. [DOI] [PubMed] [Google Scholar]
- 32.Bonner AB, Monroe KW, Talley LI, Klasner AE, Kimberlin DW. Impact of the rapid diagnosis of influenza on physician decision-making and patient management in the pediatric emergency department: results of a randomized, prospective, controlled trial. Pediatrics. 2003;112:363–367. doi: 10.1542/peds.112.2.363. [DOI] [PubMed] [Google Scholar]
- 33.Eriksson M, Bennet R, Nilsson A. Wheezing following lower respiratory tract infections with respiratory syncytial virus and influenza A in infancy. Pediatr Allergy Immunol. 2000;11:193–197. doi: 10.1034/j.1399-3038.2000.00076.x. [DOI] [PubMed] [Google Scholar]
- 34.Heymann PW, Carper HT, Murphy DD, Platts-Mills TA, Patrie J, McLaughlin AP, Erwin EA, Shaker MS, Hellems M, Peerzada J, et al. Viral infections in relation to age, atopy, and season of admission among children hospitalized for wheezing. J Allergy Clin Immunol. 2004;114:239–247. doi: 10.1016/j.jaci.2004.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lahti E, Peltola V, Virkki R, Ruuskanen O. Influenza pneumonia. Pediatr Infect Dis J. 2006;25:160–164. doi: 10.1097/01.inf.0000199265.90299.26. [DOI] [PubMed] [Google Scholar]
- 36.Coffin SE, Zaoutis TE, Rosenquist AB, Heydon K, Herrera G, Bridges CB, Watson B, Localio R, Hodinka RL, Keren R. Incidence, complications, and risk factors for prolonged stay in children hospitalized with community-acquired influenza. Pediatrics. 2007;119:740–748. doi: 10.1542/peds.2006-2679. [DOI] [PubMed] [Google Scholar]
- 37.Daley AJ, Nallusamy R, Isaacs D. Comparison of influenza A and influenza B virus infection in hospitalized children. J Paediatr Child Health. 2000;36:332–335. doi: 10.1046/j.1440-1754.2000.00533.x. [DOI] [PubMed] [Google Scholar]
- 38.Ruiz Laiglesia F, Zubizarreta García J, Agud Aparicio J, Villasante Claudios F, Ayensa Dean C, Sánchez Nanclares M, Torrubia Pérez C. Febrile syndrome in hospitalized patients. An Med Interna. 1992;9:367–371. [PubMed] [Google Scholar]
- 39.Dawood FS, Fiore A, Kamimoto L, Nowell M, Reingold A, Gershman K, Meek J, Hadler J, Arnold KE, Ryan P, et al. Influenza-associated pneumonia in children hospitalized with laboratory-confirmed influenza, 2003-2008. Pediatr Infect Dis J. 2010;29:585–590. doi: 10.1097/inf.0b013e3181d411c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Falagas ME, Vouloumanou EK, Baskouta E, Rafailidis PI, Polyzos K, Rello J. Treatment options for 2009 H1N1 influenza: evaluation of the published evidence. Int J Antimicrob Agents. 2010;35:421–430. doi: 10.1016/j.ijantimicag.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 41.Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM Centers for Disease Control and Prevention (CDC) Antiviral agents for the treatment and chemoprophylaxis of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60:1–24. [PubMed] [Google Scholar]
- 42.Jennings LC, Skopnik H, Burckhardt I, Hribar I, Del Piero L, Deichmann KA. Effect of rapid influenza testing on the clinical management of paediatric influenza. Influenza Other Respir Viruses. 2009;3:91–98. doi: 10.1111/j.1750-2659.2009.00079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]