Abstract
We evaluated the clinical course of subchondral insufficiency fracture of the femoral head (SIFFH) and its characteristic findings with special regard to joint space narrowing (JSN). Thirty-one cases of SIFFH of mean age 68.9 yr initially underwent limited weight-bearing conservative treatment. During the follow-up period, the patients with intractable pain underwent total hip arthroplasty (THA). For radiographic evaluation, lateral center-edge angle, JSN and femoral head collapse (FHC) were documented, and the extent of FHC was classified as mild (<2 mm), moderate (2-4 mm), and severe (>4 mm). The progression or new development of FHC more than 2 mm was evaluated on sequential plain radiographs. The relationship between radiographic parameters and clinical outcomes were evaluated. THAs were performed in 15 cases (48.4%). There was no significant correlation between clinical outcomes and the extent of initial FHC. However, a significantly larger proportion of patients that underwent THA showed JSN and FHC progression compared to the symptom improvement group. The risk factor significantly associated with failed conservative treatment was JSN (P=0.038; OR, 11.8; 95% CI, 1.15-122.26). Clinical results of conservative treatment for SIFFH in elderly patients are relatively poor. The patients with JSN are at higher risk of failed conservative treatment.
Graphical Abstract
Keywords: Hip, Fractures, Bone, Risk Factors, Outcome Assessment (Health Care)
INTRODUCTION
Subchondral stress fracture of the femoral head can occur as two types; fatigue-type and insufficiency-type. Of them, subchondral insufficiency fracture of the femoral head (SIFFH) is caused by normal or physiological stress without antecedent trauma and usually occurs in elderly patients with poor bone quality. Since it has been reported not only in osteoporotic patients without underlying disease, but also in patients who were treated with corticosteroids for systemic lupus erythematosus and organ (kidney or liver) transplantation, most authors emphasize the importance of differentiating SIFFH from osteonecrosis (1, 2, 3, 4). SIFFH is known as a rare condition. But the number of cases of SIFFH in the literature is increasing on the basis of characteristic findings from magnetic resonance image (MRI) such as subchondral fractures and bone marrow edema patterns which are distinct from those of osteonecrosis (5, 6, 7, 8, 9). However, most cases were reported as case reports and the number of case series studies is very limited.
Unlike fatigue-type subchondral fracture of the femoral head which occurs in healthy adults with good bone quality after sudden increases in activity, joint space narrowing has been observed in some hip joints affected by SIFFH. However, the cause and clinical significance of the joint space narrowing are unknown.
The purpose of current study was to evaluate the clinical course of SIFFH and its characteristic findings with special regard to joint space narrowing.
MATERIALS AND METHODS
Thirty one hips with SIFFH were diagnosed and treated at a single institution from December 2000 to May 2011. The average age was 68.9 yr (range, 53.0 to 90.3 yr). There were 26 women and five men with 15 right and 16 left hips. All patients presented with acute hip pain during daily activity without precedent trauma. None of them had concomitant metabolic disease worsening bone quality except for osteoporosis. A sixty-two-year-old female patient had radiation therapy over the area of the left ilium and ischium for metastatic lesions of recurring rectal cancer twenty years ago. While only one patient was a regular drinker (≥400 mL of alcohol weekly), others had no predisposing factors for osteonecrosis of the femoral head such as alcohol consumption and corticosteroid treatment.
Radiographic evaluation
Diagnosis was confirmed with characteristic MR findings which were distinctive for osteonecrosis of the femoral head (10), as well as with plain radiographs and bone scans. On plain radiographs, the lateral center-edge (CE) angle was measured as well as the presence of femoral head collapse (FHC), joint space narrowing (JSN) and linear patch sclerotic changes in the superior portion of the femoral head were identified. The extent of the FHC was measured using concentric circles and classified as mild (<2 mm), moderate (2-4 mm), and severe (>4 mm) (Fig. 1). The progression or new development of the FHC was defined when there was >2 mm increase in extent as compared with the initial radiograph, and then it was serially evaluated on sequential plain radiographs. The joint space width was measured on standard anteroposterior radiograph of the hip by the same method as described in our previous paper (11). Joint space narrowing was defined when there was >a 0.5 mm decrease in width as compared with the contralateral hip on the radiograph. Bone scans were performed in seven patients with a high suspicion of SIFFH even though their plain radiographs showed no definite abnormal findings. The characteristic MR features of bone marrow edema patterns, subchondral fracture lines and their locations were recorded in all patients.
Fig. 1.
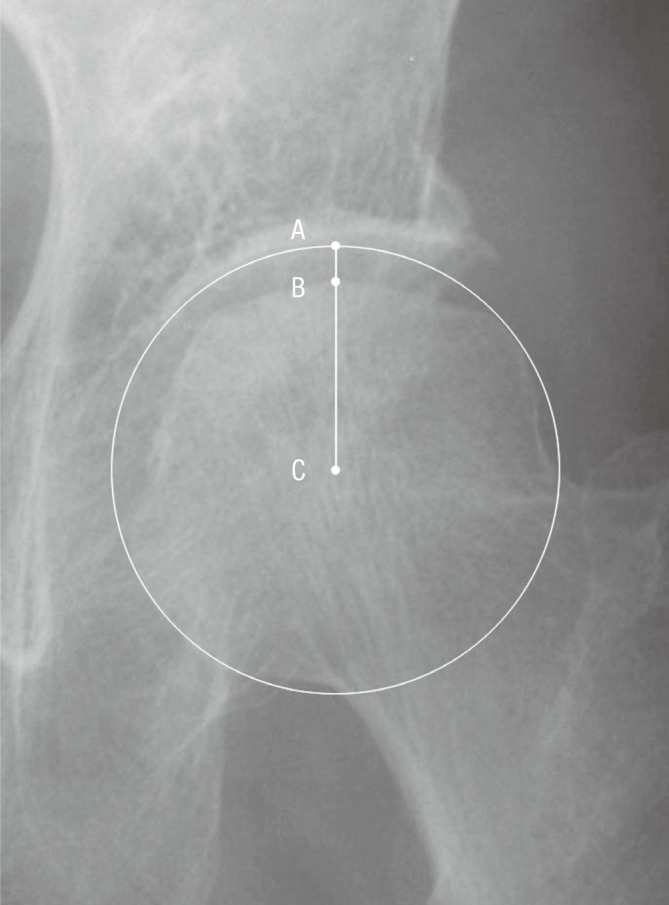
The extent of femoral head collapse (the distance between A and B) was measured using concentric circles (C, the center of the femoral head).
Clinical outcome evaluation
The severity of osteoporosis was estimated on the basis of a bone mineral density (BMD) measurement by dual-energy X-ray absorptiometry (DEXA) in eight patients and calculation of the Singh index score at the time of the onset of hip pain in all patients. Body mass index (BMI) was calculated as kg/m2.
Initially, non-weight bearing conservative treatment was planned, then the patients were allowed to bear weight as tolerated but crutches were used until the hip pain almost completely disappeared. During the follow-up period, the patients with intractable pain underwent total hip arthroplasty (THA). At baseline and the end of follow-up, clinical outcome assessments were performed using the Western Ontario and McMaster Universities (WOMAC) scores in patients who had symptom improvements without surgical treatment.
Statistical analysis
Data processing and statistical analyses were performed using IBM SPSS statistics software package (version 20; IBM, Chicago, IL, USA). To evaluate the relationship between radiographic parameters and clinical outcomes, a chi-square test or Fisher's exact test was used for analysis of categorical data such as presence of JSN and FHC progression. A Mann-Whitney U-test was used for parametric data between the symptom improvement group and THA group. To assess which variables were associated with failed conservative treatment, a multiple logistic regression was used. The parameters included in the model were selected using the univariate analysis (P<0.2). P values below 0.05 were considered statistically significant.
Ethics statement
The design and protocol of this study were approved by the institutional review board in our hospital (IRB No. H-1201-069-394), and informed consent was obtained from each patient.
RESULTS
In all cases, magnetic resonance images revealed a serpentine low signal intensity line with surrounding bone marrow edema in the subchondral area of the femoral head. The bone-marrow-edema pattern extended to the subchondral area, but there was no additional abnormal signal intensity band representing the reactive margin of the necrotic area which is the characteristic finding of osteonecrosis of the femoral head. Subchondral fracture lines were observed at the anterosuperior aspect of the femoral head in thirty cases and at the posterosuperior aspect in one case. A bone scintigram was available for seven patients and they all showed increased radionuclide uptake in the affected femoral head.
Collapse of the femoral head at the anteosuperior portion was identified in 13 (41.9%) of 31 hips on initial radiograph assessment. The collapse was mild in five, moderate in five and severe three cases. When reevaluated on final follow-up of radiographs, progression of FHC more than 2 mm was observed in 10 of 13 hips with initial collapse. Three of 18 cases without FHC at the time of initial diagnosis showed development of collapse; however, there was no evidence of collapse in the remaining 14 cases until the final follow-up visit.
A total of 21 cases (67.7%) showed JSN of the affected hip on plain radiographs compared to the unaffected one. It was detected at the time of initial diagnosis in 16 cases and at 4-8 weeks after diagnosis in five cases (Fig. 2).
Fig. 2.
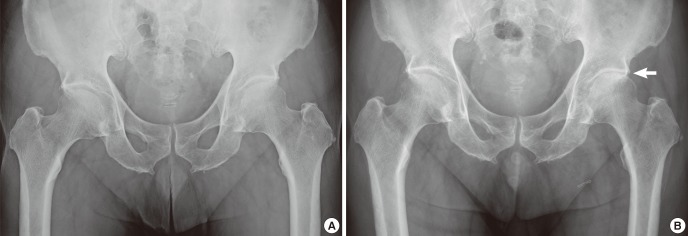
An anteroposterior radiograph of an 82-yr-old male patient with left hip pain showed no femoral head collapse and joint space narrowing initially (A). Radiograph made at eight weeks later shows joint space narrowing of the left hip (B).
The mean CE angle of the affected hip in all cases was 27.0 degrees (range, 16.0 to 39.7 degrees). The mean T-score of the affected proximal femur in eight patients was -3.7±0.5 and the mean Singh index score for all cases was 2.9 (range, 1 to 4). The mean BMI for all cases was 22.8 kg/m2 (range, 17.0 to 27.0 kg/m2).
The average duration of symptoms from onset to diagnosis was 2.1 months (range, 1 to 6 months). The initial treatment for all patients was limited weight-bearing walking (as much as possible), with a walking aid. It was followed by tolerable weight bearing, and full weight bearing was allowed after patients became pain-free and no further progression of femoral head collapse was confirmed on follow-up radiographs. In 16 cases, pain reduced and gradually disappeared almost completely by an average of 5 months (range, 4 to 6 months) after conservative treatment. Their mean WOMAC scores were significantly improved from 42.1 (range, 28 to 52) at baseline to 89.9 (range, 81 to 96) at the end of follow-up; the last follow-up averaged 15.9 months (range, 12 to 30.2 months).
THAs were performed in 15 cases (48.4%) due to intractable pain with or without remarkable progression of FHC during the follow-up period. The mean interval between initial diagnosis and THA was 5.6 months (range, 1.5 to 9.5 months). The cartilage of the femoral head was markedly damaged in these cases with JSN (Fig. 3, 4, 5, 6).
Fig. 3.
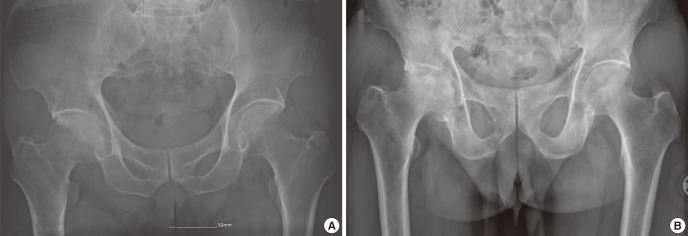
The initial radiograph of a 76-yr-old male patient shows joint space narrowing of the right hip joint (A). Radiograph five months later shows progression of joint space narrowing and femoral head collapse (B).
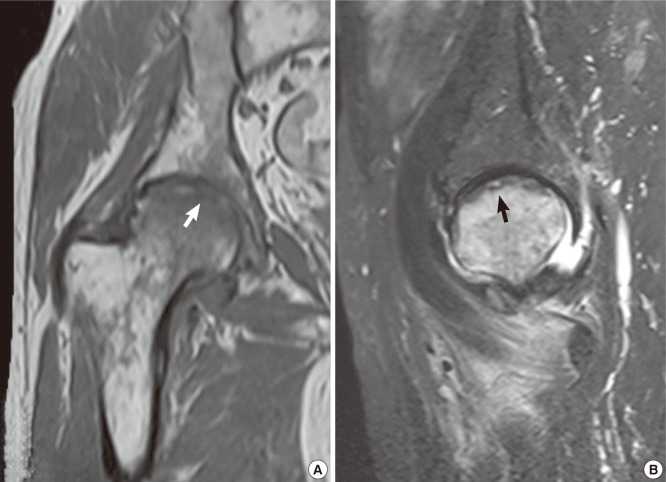
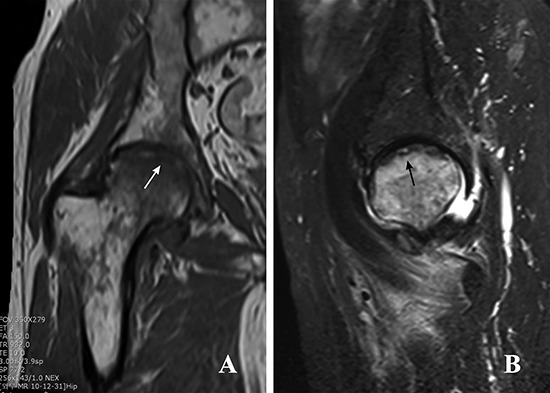
Fig. 4.
MR images of the same patient in Fig. 3. (A) T1- and (B) T2-weighted signal intensity images show a subchondral fracture (arrows) and the bone-marrow-edema pattern extending to the subchondral area.
Fig. 5.

Gross photograph of the resected femoral head of the same patient in Fig. 3 showed a markedly destroyed articular cartilage.
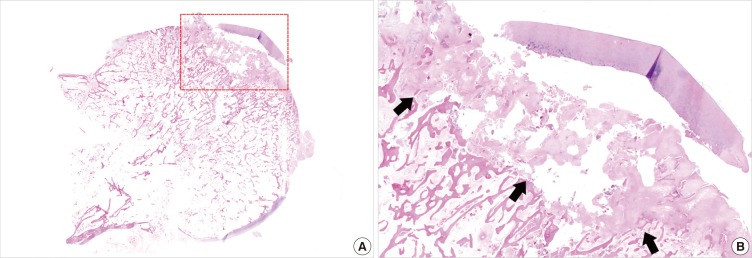
Fig. 6.
Histology of the superior portion (dotted read rectangle) of the resected femoral head of the same patient in Fig. 3, showing fracture callus formation (arrows) and granulation tissue (H&E, ×40 [A], ×100 [B]).
There was no significant correlation between clinical outcomes and the extent of initial FHC. However, a significantly larger proportion of patients who underwent THA showed JSN and FHC progression compared to the symptom improvement group (P=0.006 and 0.048, respectively, Table 1). The risk factor significantly associated with failed conservative treatment was JSN (P=0.038; OR, 11.8; 95% CI; 1.15-122.26, Table 2). There was a significant difference between the mean age of cases with JSN (71.3±8.5 yr) than those cases without JSN (63.8±6.8 yr; P=0.025, Table 3).
Table 1.
Univariate analysis comparing symptom improvement group and THA groups*
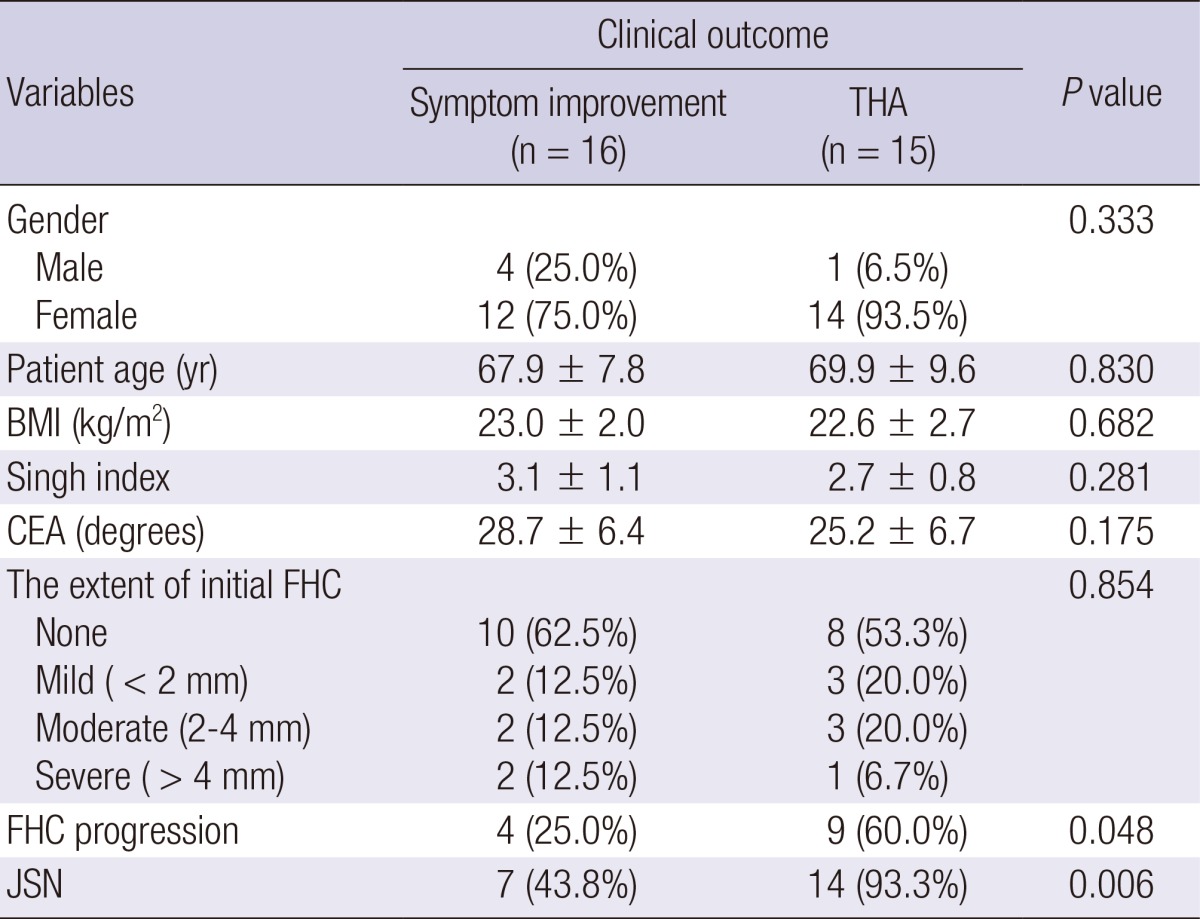
*Data represent the mean±standard deviation. BMI, body mass index; CEA, center-edge angle; FHC, femoral head collapse; JSN, joint space narrowing; THA, total hip arthroplasty.
Table 2.
Multiple logistic regression results
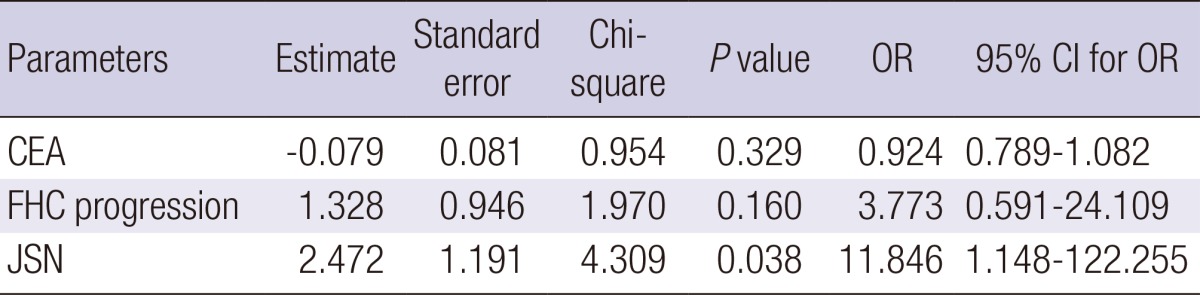
OR, odds ratio; CI, confidence interval; CEA, center-edge angle; FHC, femoral head collapse; JSN, joint space narrowing.
Table 3.
Univariate analysis comparing the patients with and without joint space narrowing*
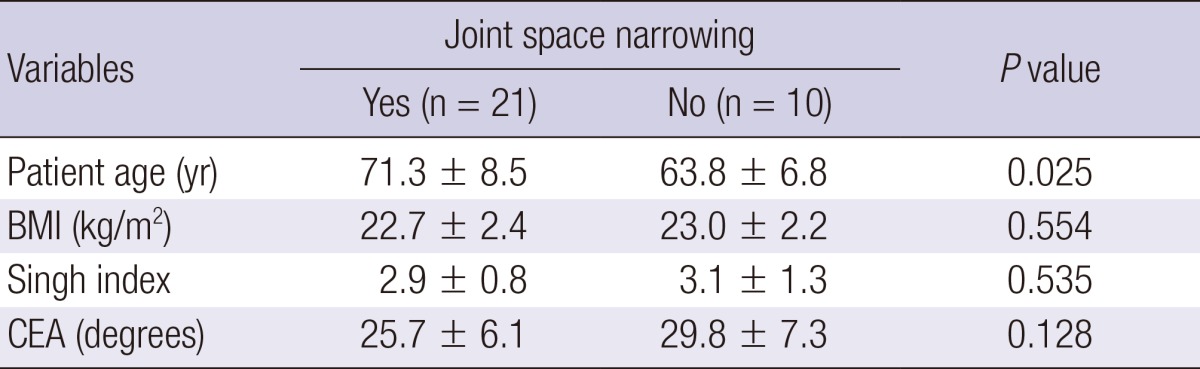
*Data represent the mean±standard deviation. BMI, body mass index; CEA, center-edge angle.
DISCUSSION
In the current study, 15 cases (48.4%) of SIFFH underwent THA because the conservative, limited weight-bearing treatment was not satisfactory. The risk for failure of conservative treatment was substantially higher in the patients with JSN.
These results are markedly different from those of fatigue-type subchondral fractures of the femoral head, which is another type of stress fracture of the femoral head that occurs in healthy people with good bone quality, frequently after a sudden increase in activity (12, 13). Clinical results of fatigue-type fractures have been reported to be very satisfactory with conservative treatment even with some collapse of the femoral head (12, 13, 14). Furthermore, no joint space narrowing has been reported in fatigue-type fractures.
Because of the rare incidence of SIFFH, most of the reported cases have been case reports or small series reports (1, 2, 3, 4, 5, 9, 15, 16, 17). Of these limited number of cases, many were reported to be treated by THA. Yamamoto and Bullough (16) reported ten cases of SIFFH on histopathologic basis which had been previously diagnosed as osteonecrosis. All patients had failed initial conservative therapy and they eventually undergone THA between 2 and 13 months from the onset of hip pain. Buttaro et al. (5) reported four cases of SIFFH. All cases showed progressive femoral head collapse and three of them were treated with THA after 4-12 months of conservative treatment. Recently, Miyanishi et al. (18) reported the largest case series of 27 patients with SIFFH. Thirteen cases (48%) underwent THA. Femoral head collapse was observed much more frequently in the THA group than in the conservative treatment group, but only age was a statistically significant risk factor for THA with the cut-off value of 71 yr.
In the current study, patient age was not directly associated with failure of conservative treatment, while JSN of the affected hip on plain radiographs compared to the unaffected one was the only significant risk factor for a poor outcome. Joint space narrowing was observed in many cases reported in the literature and some authors suggested that this finding is an early sign of rapidly destructive arthrosis of the hip joint (2, 9, 15, 17, 19). However, there are no studies documenting JSN as a prognostic factor of SIFFH. We hypothesized that JSN is a factor for poor prognosis because it has not been reported in fatigue-type subchondral stress fractures of the femoral head which showed very satisfactory results with conservative treatment, in spite of FHC. And our hypothesis was supported by the results of statistical analyses. A univariate analysis proved that a significantly larger proportion of patients that underwent THA showed JSN compared to the symptom improvement group (P=0.006), and JSN was the significant risk factor for failure of conservative treatment according to the result of the multiple logistic regression analysis (P=0.038; OR, 11.8; 95% CI, 1.15-122.26). The mechanism of the development of JSN in SIFFH is unknown. In our study, the mean age of cases with JSN (71.3±8.5 yr) was significantly older than that of cases without JSN (63.8±6.8 yr; P=0.025).
In summary, conservative treatment failed in 15 cases (48.4%), and during the average follow-up period of 15.9 months, pain resolved to a tolerable level in 16 cases, even though there was FHC and JSN on radiographs in some of these cases at last follow-up. This may be due to low-demand activity in older patients and the symptoms in these patients may deteriorate with a longer follow-up. Clinical results of conservative treatment for SIFFH in older patients are relatively poor compared to those for fatigue-type subchondral fracture of the femoral head. The patients with JSN are at higher risk of failed conservative treatment.
ACKNOWLEDGMENT
We thank Sohee Oh from Seoul National University Boramae Hospital for statistical advice.
Footnotes
This study was supported by a grant (06-03-063) from the Seoul National University Hospital Research Fund.
The authors declare no potential conflicts of interest.
References
- 1.Ikemura S, Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Iwamoto Y. Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: a case report. Arthritis Rheum. 2005;52:1293–1296. doi: 10.1002/art.20994. [DOI] [PubMed] [Google Scholar]
- 2.Yamamoto T, Schneider R, Iwamoto Y, Bullough PG. Subchondral insufficiency fracture of the femoral head in a patient with systemic lupus erythematosus. Ann Rheum Dis. 2006;65:837–838. doi: 10.1136/ard.2005.041095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iwasaki K, Yamamoto T, Nakashima Y, Mawatari T, Motomura G, Ikemura S, Iwamoto Y. Subchondral insufficiency fracture of the femoral head after liver transplantation. Skeletal Radiol. 2009;38:925–928. doi: 10.1007/s00256-009-0706-x. [DOI] [PubMed] [Google Scholar]
- 4.Miyanishi K, Hara T, Hamada T, Maekawa M, Tsurusaki S, Moro-oka TA, Kamo Y, Jingushi S, Torisu T. Co-occurrence of subchondral insufficiency fracture of the femoral head and contralateral femoral neck fracture in a rheumatic patient receiving steroid treatment. Mod Rheumatol. 2008;18:619–622. doi: 10.1007/s10165-008-0093-5. [DOI] [PubMed] [Google Scholar]
- 5.Buttaro M, Della Valle AG, Morandi A, Sabas M, Pietrani M, Piccaluga F. Insufficiency subchondral fracture of the femoral head: report of 4 cases and review of the literature. J Arthroplasty. 2003;18:377–382. doi: 10.1054/arth.2003.50092. [DOI] [PubMed] [Google Scholar]
- 6.Uetani M, Hashmi R, Ito M, Okimoto T, Kawahara Y, Hayashi K, Enomoto H, Shindo H. Subchondral insufficiency fracture of the femoral head: magnetic resonance imaging findings correlated with micro-computed tomography and histopathology. J Comput Assist Tomogr. 2003;27:189–193. doi: 10.1097/00004728-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Cabarrus MC, Ambekar A, Lu Y, Link TM. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am J Roentgenol. 2008;191:995–1001. doi: 10.2214/AJR.07.3714. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto T, Iwamoto Y, Schneider R, Bullough PG. Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis. 2008;67:150–153. doi: 10.1136/ard.2006.066878. [DOI] [PubMed] [Google Scholar]
- 9.Miyanishi K, Hara T, Kaminomachi S, Maeda H, Watanabe H, Torisu T. Contrast-enhanced MR imaging of subchondral insufficiency fracture of the femoral head: a preliminary comparison with that of osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2009;129:583–589. doi: 10.1007/s00402-008-0642-6. [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto T. Subchondral insufficiency fractures of the femoral head. Clin Orthop Surg. 2012;4:173–180. doi: 10.4055/cios.2012.4.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoon PW, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Joint space widening in synovial chondromatosis of the hip. J Bone Joint Surg Am. 2011;93:303–310. doi: 10.2106/JBJS.J.00473. [DOI] [PubMed] [Google Scholar]
- 12.Kim JW, Yoo JJ, Min BW, Hong SH, Kim HJ. Subchondral fracture of the femoral head in healthy adults. Clin Orthop Relat Res. 2007;464:196–204. doi: 10.1097/BLO.0b013e3181577212. [DOI] [PubMed] [Google Scholar]
- 13.Song WS, Yoo JJ, Koo KH, Yoon KS, Kim YM, Kim HJ. Subchondral fatigue fracture of the femoral head in military recruits. J Bone Joint Surg Am. 2004;86-A:1917–1924. doi: 10.2106/00004623-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Lee YK, Yoo JJ, Koo KH, Yoon KS, Min BW, Kim HJ. Collapsed subchondral fatigue fracture of the femoral head. Orthop Clin North Am. 2009;40:259–265. doi: 10.1016/j.ocl.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Niimi R, Hasegawa M, Sudo A, Uchida A. Rapidly destructive coxopathy after subchondral insufficiency fracture of the femoral head. Arch Orthop Trauma Surg. 2005;125:410–413. doi: 10.1007/s00402-005-0831-5. [DOI] [PubMed] [Google Scholar]
- 16.Yamamoto T, Bullough PG. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum. 1999;42:2719–2723. doi: 10.1002/1529-0131(199912)42:12<2719::AID-ANR31>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto T, Takabatake K, Iwamoto Y. Subchondral insufficiency fracture of the femoral head resulting in rapid destruction of the hip joint: a sequential radiographic study. AJR Am J Roentgenol. 2002;178:435–437. doi: 10.2214/ajr.178.2.1780435. [DOI] [PubMed] [Google Scholar]
- 18.Miyanishi K, Ishihara K, Jingushi S, Torisu T. Risk factors leading to total hip arthroplasty in patients with subchondral insufficiency fractures of the femoral head. J Orthop Surg (Hong Kong) 2010;18:271–275. doi: 10.1177/230949901001800302. [DOI] [PubMed] [Google Scholar]
- 19.Davies M, Cassar-Pullicino VN, Darby AJ. Subchondral insufficiency fractures of the femoral head. Eur Radiol. 2004;14:201–207. doi: 10.1007/s00330-003-1998-1. [DOI] [PubMed] [Google Scholar]