Abstract
Background:
Mosquito borne diseases (MBDs) are major public health problem in India. State of Delhi is endemic for dengue and other MBDs. The increasing incidence of MBDs in Delhi in recent years warrants a pro-active approach for their prevention. Knowledge and use of personal protective measures (PPMs) presents an effective strategy for prevention and control of MBDs.
Aim:
The present study was conducted to assess the knowledge and use of PPMs against MBDs in an urban resettlement colony of Delhi.
Subjects and Methods:
It was a cross-sectional study carried out in a resettlement colony of Delhi. A total of 100 families were selected by systematic random sampling. Data was collected using semi-structured questionnaire and supplemented by spot survey by the investigator in the community. The results were analyzed in SPSS version 16.0 (Chicago Illinios, USA).
Results:
Out of the 100 respondents, 65% (65/100), 58%(58/100) and 13% (13/100) had heard about dengue, malaria and chikungunya, respectively. Nearly, one-fifth (20/100; 20%) of the participants reported incorrect breeding sites for mosquitoes. The knowledge regarding PPMs was very high (93/100; 93%) and about (90/100; 90%) families were actually using at least one of the PPMs. However, very few families were using them correctly (1/90; 1.1%) and adequately (5/90; 5.6%). The most common PPM being used by the study population was liquid vaporizers (54/90; 60%). Nearly one-third (29/90; 32.2%) of the participants reported side-effects due to PPMs with irritation to smell being the most common reported side-effect. On house visit, adult mosquitoes were seen in 67% (67/100) of the houses, while potential mosquito breeding sites were found in and around 56% (56/100) houses.
Conclusions:
There were crucial gaps in knowledge and practices of participants with regard to prevention and control of MBDs. Thus, there is a need to intensify efforts toward creating public knowledge and mobilizing community about correct use of preventive measures against MBDs.
Keywords: Chikungunya, Delhi, Dengue, Malaria, Mosquito borne diseases, Personal protective measures
Introduction
In recent years, mosquito borne diseases (MBDs) have emerged as a serious public health concern in India. Many of these, particularly dengue fever, Japanese encephalitis and malaria now occur in epidemic proportions almost on an annual basis causing considerable morbidity and mortality.[1] Though, the confirmed cases of malaria have decreased from 75 million in 1950's to 1.49 million in year 2010,[2] approximately 65% of the population at risk of becoming infected with malaria in South-East Asia is still residing in India.[3] Recently, it has been suggested that malaria incidence is between 9 times and 50 times greater than reported with approximately 13 fold under estimation of malaria related mortality.[4] On the other hand, changing epidemiology of dengue fevers in terms of strains, severity and geographic distribution is a growing concern in Indian subcontinent. Over the last 10-15 years recurrent outbreaks of dengue fever have occurred in different parts of the country. Delhi, the capital city of India, has experienced nine major outbreaks of dengue fever from 1967 to 2010. Thus, it is evident that malaria and dengue have already established their endemicity in Delhi.[5] The failure to cap the resurgence of malaria and the continuing increased incidence of other MBDs is warranting a more pro-active approach for their prevention.
Vector is an important link in transmission of MBDs and thus, protection from vector serves as one of the best strategies for prevention in population. Personal protective measures (PPMs) serve as critical action in this regard. A variety of PPMs are available including-repellent creams, mosquito nets (plain or insecticide treated), mosquito coils, liquid repellents, electric rackets, mats, smokeless coils, Incense sticks and naphthalene balls. Under national vector borne disease control program, government has introduced insecticide treated nets for the malaria endemic communities.[6] Considering the increasing problem of MBDs, it is important that people should be aware about various measures available and how to use them correctly. Success of these measures largely depends on the access, acceptability and proper usage by the target population.[7] Further, role of community participation in vector control is imminent. Community participation in turn depends on people's awareness and knowledge towards the disease and its prevention.[8] Therefore, for designing evidence based effective prevention strategies, it is pertinent to study the existing knowledge of the population regarding the disease.
Thus, the present endeavor was undertaken with the objective to study the knowledge about the MBDs in the community, assess the various measures taken by the families to prevent them and to explore reasons for choice of various PPMs used against MBDs by them.
Subjects and Methods
Study settings and sampling
It was a cross-sectional study conducted in a resettlement colony of central Delhi from June 2011 to July 2011. Sample size was calculated as 94 using the level of knowledge regarding MBDs as 62% as reported in previous study,[9] with 10% precision at 95% confidence interval. There were 400 houses/families in that colony. A total of 100 families were selected by systematic random sampling method and informed consent was obtained before their inclusion into the study. This was carried out to ensure equal representation from whole of the study area. Sampling interval (SI) was calculated as four. A random number was chosen using random number table (n = 1, i.e., the first house) and by adding the SI to it, the next house was chosen (n + SI = 5 in this case). In case where the family refused to participate or those who could not be contacted or whose houses were found locked during the study period, the next house was included without disturbing the overall sampling procedure.
Study tool
A pre-tested, pre-designed, semi-structured questionnaire was used for data collection regarding socio-demographic profile Knowledge about MBDs, breeding sites of mosquitoes, PPMs and usage or non-usage of PPMs. The adequacy and correctness of use of PPMs were also assessed. Socio-economic status of the families was calculated using modified Kuppuswamy Scale.[10]
Key definitions
Adequacy and correctness of PPMs have been defined as follows:
-
Bed nets:
- Adequacy: Preferably every member of the house should sleep under the bed net
- Correctness: To be used every night, all year round, even if mosquitoes are not seen or heard. The net should be erected and supported in such a way so as to prevent contact of the net with the sleeping person. It should be installed before the dusk when mosquitoes become active.[11] Nets to be re-treated after washing 3 times or at least once a year.[12] (As it was a cross-sectional study, so the investigator only enquired about the date of last treatment of nets and number of washes they normally do in a year, for assessment of correctness).
-
Liquid vaporizers, mats and coils:
- Adequacy: Mats (containing allethrin and parallethrin) and coils (pyretheroids) to be changed every-day. Liquid vaporizers most commonly used in India (synthetic pyretheroids like transfluthrin 0.88%) come in 30, 60 and 90 day pack and have to be used daily preferably throughout the day
- Correctness: The heating machine/vaporizer is plugged into the ordinary household electric socket and heats up to an optimum temperature depending upon the mat and the heater.[13] The free end of the spiral of a coil should be lit and room should be closed and left, to return after 1-2 h.[14] The coil usually lasts for 6-8 h.
-
Sprays (with knockdown insecticide like pyrethrum and its related compounds):
- Adequacy: Multiple applications are particularly necessary for Aedes aegypti at intervals shorter than the extrinsic incubation period, but not < 8-10 days[15]
-
Creams (N, N diethyl benzamide, DEET-N, N-diethyl-meta-toluamide, N, N-diethyl-3 methyl benzamide):
- Adequacy: Re-application duration will vary with the amount of active ingredient, air temperature, amount of physical activity and perspiration, water exposure and other factors. Re-apply repellant creams according to label instructions
- Correctness: It must be applied on exposed skin of arms, forearms, legs, feet etc., and preferably before wearing anything so as to have protection against mosquito bites even through clothes. Should be applied in daytime also for protection against day biting mosquitoes.
(Adequacy of use of repellant creams was checked by asking the respondents about re-application duration and the answers were matched with the duration for re-application mentioned on the label of the cream).
Study methods
From the selected family, an adult person who was available at the time of survey and was willing to participate was contacted. In case, there were more than one adult present at the time of survey, simple random sampling was performed for selection. After explaining the purpose of this study, the requisite information was obtained through the questionnaire by interviewing the consenting participants. Data collection was further supplemented by spot survey by the investigator using an observation check-list at the study site regarding the presence of mosquitoes, presence of screened windows and mosquito breeding site in and around the selected house. After the interview, the study subjects were given health education about prevention of MBDs.
Statistical analysis
Data collected was entered in MS office excel and analyzed using Epi-info 2005 software of world health organization and SPSS version 16.0 (SPSS Inc., 233 South Wacker Drive, 11th Floor, Chicago, IL 60606-6412) The results were presented in proportions and any difference between two proportions in relation to particular factor was assessed by Chi-square (or fisher exact test if expected frequency in any of the cell was < 5) and was considered significant if probability of error was < 5%.
Ethical considerations
Informed written consent was taken from all the participants and privacy and confidentiality of information so provided by them was assured. The study was approved by the Institutional Ethics Committee, Maulana Azad Medical College.
Results
Sociodemographic profile of the participants
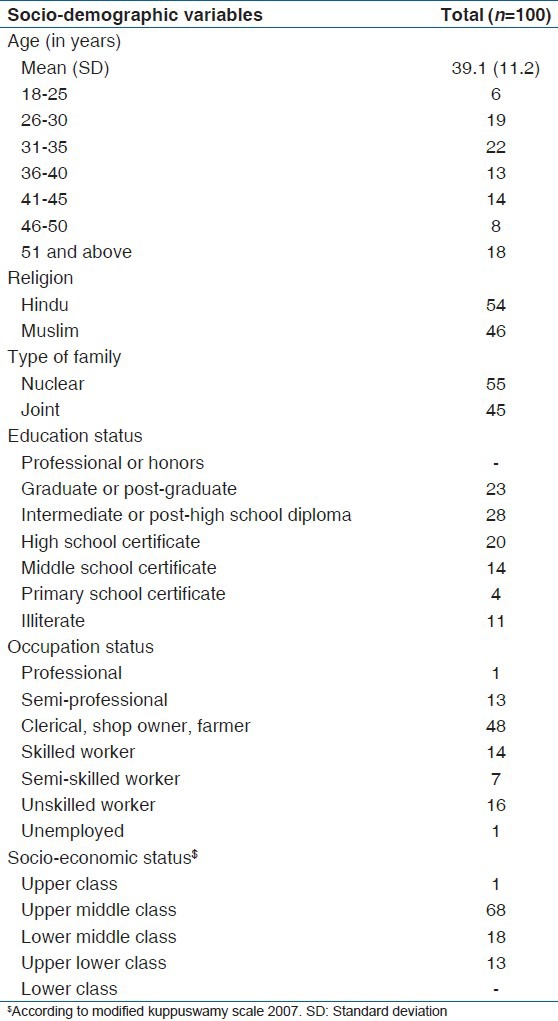
Out of the 100 families surveyed, large proportion of the participants belonged to nuclear families (55%). The mean age of the participants was 39.1 (11.2) years (19-66 years). Out of the total participants, 58% were males. Most of the respondents belonged to upper middle class families (68%) according to modified Kuppuswamy Scale.[10] No gender wise significant difference was noted in the demographic profile of the participants except for religion and type of family [Table 1].
Table 1.
Socio-demographic profile of the participants (n=100)
Knowledge regarding MBDs and their prevention
Majority of the participants had heard about MBDs such as dengue (65%) and malaria (58%) while only 13% had known about chikungunya. There were only 7% of the participants who had no knowledge about the MBDs. “Dengue” was named by 52% of the participants as MBD, which is highly prevalent in Delhi, followed by “malaria.” Enquiry into the knowledge about the mosquito breeding sites revealed that 68% respondents knew that mosquitoes breed in stagnant clean water whereas nearly one-third (29%) believed that breeding occurs in polluted stagnant water. There were only 6% of the participants who named desert coolers as the breeding site for mosquitoes. Nearly, 20% of the participants named incorrect breeding sites such as toilets, air, garbage etc. Majority of the participants (70%) also believed that MBDs are the highest during and after monsoons largely because of collection of water [Table 2].
Table 2.
Knowledge regarding MBDs and its prevention among the participants (n=100)
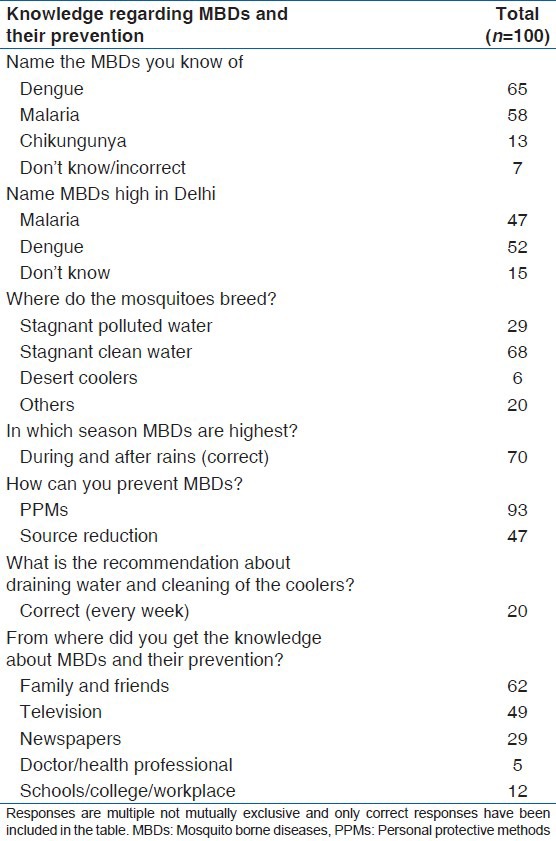
The knowledge regarding PPMs (93%) was very high followed by source reduction (47%). Knowledge regarding other preventive measures such as cleaning of coolers and cleaning the surroundings was poor. The recommendation about draining water and cleaning of coolers at least once in week,[17] was answered correctly by only 20% of the respondents. Only 26% of the participants knew about any knowledge activity against MBDs in the city with nearly 77% (20/26) of them citing advertisements as source of such activities. There was negligible knowledge regarding the anti-malarial month (2%). Though 84% of the respondents said that anti-mosquito activities were being undertaken by Municipal Corporation of Delhi, only 14% (12/84) found them adequate [Table 2]. Majority of the participants cited corruption, late reactive approach and lack of accountability and ownership in the system for such inadequacy in their work.
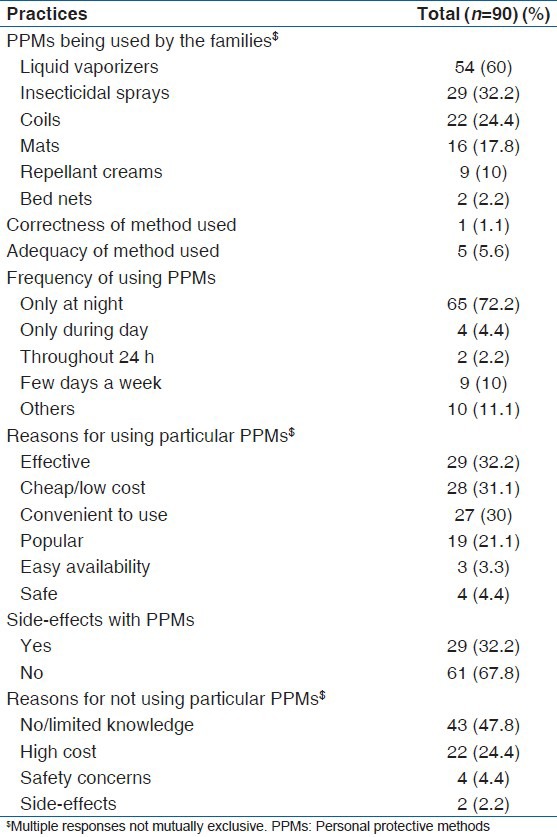
Practices and pattern of usage of PPMs
Most of the participants (90%) were using PPMs. The most common PPM being used by the study population was Liquid vaporizers (54/90; 60%) followed by insecticidal spray (29/90; 32.2%). However, they were just handful of the participants who were using the methods correctly (1/90; 1.1%) and adequately (5/90; 5.6%). Majority of the households were using PPMs only at night (65/90; 72.2%). Nearly one-third of the participants stated convenience, effectiveness and cost as the main reasons for choosing a particular PPM. Only 32.2% (29/90) of the users said that they experienced side-effects on using the PPMs [Table 3]. The most common side-effect reported by the participants was irritation to smell of PPMs (15/29; 51.7%) followed by headache (13/29; 44.8%).
Table 3.
Practices and pattern of usage of PPMs against mosquitoes
Observations by the investigator
On house visit, adult mosquitoes were seen in 67% of the houses of the respondents. As visit was made during the day, it was observed that only 3% were using PPM at that time. Screening of windows with mesh was seen in only 63% of the houses. Majority of the houses (56%) had potential mosquito breeding sites in and around the house while actual mosquito larvae were seen in 36% houses.
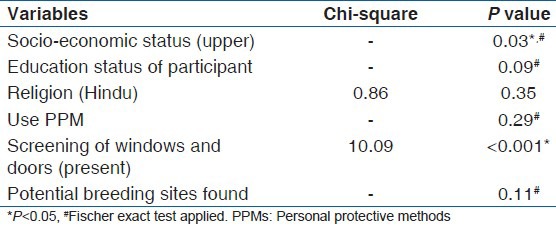
On bivariate analysis, upper socio-economic status of the family (P = 0.03) and presence of appropriate screening of windows and doors (P < 0.001) were found to be significantly protective against presence of adult mosquito in the house [Table 4].
Table 4.
Bivariate analysis of the association between presence of adult mosquito in the house and socio-demographic and other independent factors
Discussion
The present community based observational study assessed the knowledge and practices regarding MBDs and their prevention in an urban resettlement colony in Delhi. The study revealed that knowledge regarding MBDs like dengue (65%) and malaria (58%) was fair in the study participants. However, chikungunya was named by only 13%. The findings are similar to that found in a study by Boratne et al.[7] in 2010 in peri-urban areas of Puducherry where nearly 57% of the study population was aware about malaria while the knowledge about dengue was just 19%. A study in Rajkot in 2011 also revealed similar knowledge about MBDs with only 62% being aware of malaria.[9] These findings show low perception about risk of mosquitoes as a cause of morbidity and mortality, by the study participants. Thus, the study emphasizes the need for intensification of health education regarding MBDs as the prevention of MBDs through better knowledge and knowledge is the appropriate way to keep the disease away.[18]
Majority of the participants (68%) knew about the breeding site of anopheles and dengue mosquito and nearly 70% also believed that the mosquito breeding peaks during and after rainy seasons due to collection of water. These findings are similar to those reported in studies done on similar peri-urban populations in Gujarat,[9] in 2011 (69.6%) and Puducherry,[7] in 2010 (61%). A study performed by Rasania et al.[19] in 2002 in patients attending malaria clinic in Delhi also showed prevalence of knowledge regarding breeding places of mosquito to be 62.9%. The “use of PPMs” followed by environmental measures were cited as the most common methods for controlling the mosquitoes. The findings are consistent with above finding that mosquito breeding takes place in collection of water and hence source reduction is emphasized in control of MBDs.
The knowledge regarding the correct recommendation of cleaning of coolers was quite low. Participants were also unaware about any knowledge generation activity regarding MBDs being undertaken by municipality. This finding points towards strengthening and promoting of effective Information Education Communication (IEC) campaigns. The most common source of information about MBDs and their prevention were family and friends followed by television. This finding is in contrast to the results found in other study where television was reported as the most common source.[7] Finding of the study highlights the role of social integration in health promotion efforts. Health-care professionals as source of information were reported by few only which points towards the low participation by doctors and paramedical staff in spreading Knowledge regarding MBDs. Though majority (84%) of respondents felt that anti-malarial activities were being undertaken by municipality, but at the same time found them grossly inadequate. Thus, there is a need for strengthening of efforts for control of MBDs at community level.
Practice of using PPMs against mosquitoes was quite high among study subjects. Similar observations were noted in study performed in 300 households of Vadodra District in Gujarat where 97% of the participants were using at least some kind of the PPMs.[6] A study performed in rural, semi-rural and bordering areas of East Delhi showed the use of PPMs to be nearly 100%.[20] Thus, there is evidently varying practices against mosquito bites from place-to-place. Liquid vaporizers followed by insecticidal sprays, mosquito coils and mats were the most common PPMs used in the current study. Studies done in South India,[7,21] found a similar pattern of use of PPMs. However, almost all the study participants were reported to be using PPMs inadequately and incorrectly. Further, PPMs were being used by them only at night time. These findings were consistent with another study in a resettlement colony in South Delhi in 2005.[22] As the A. aegypti mosquito bites during daytime,[23] it is imperative to use these methods during the daytime also. Convenience, effectiveness and cost of a particular PPM were cited as the common reasons for usage of a particular PPM. These factors could be taken into consideration while development and marketing of PPMs under the national program to ensure its wider acceptability by the people.
On observation, 56% houses had potential breeding sites while actual mosquito larvae were seen in and around 36% houses. This finding is much higher than stagnant water collections that were observed around 44% houses in areas in South Delhi.[22] It could be attributed to close proximity of the houses and poor drainage system in the community under current study. Presence of adult mosquito was found to be significantly associated with lower socio-economic status in the present study and has been reported by others also.[20,22]
Strengths and limitations of the study
One of the strength of this study is that it is first study of its kind, which had objective parameters for assessment of correctness and adequacy of PPMs taken by the study population. However, the study being a cross-sectional in design could not reflect the varying pattern of usage of various personal protective methods. Hence, a follow-up study is required to find out the variations of usage of PPMs with different seasons and mosquito density.
To conclude, there are crucial gaps in knowledge about MBDs and practices of participants with regard to prevention and control of MBDs. As the efforts of government health authorities are not always adequate, it therefore, becomes responsibility of the individuals themselves to use protection against MBDs. Role of mass media particularly television and radio needs to be further emphasized in reaching out to the general public. Role of social environment in spread of Knowledge regarding MBDs can be explored. Further, health education and IEC campaigns need to be intensified in the community by local civil authorities and municipalities.
Acknowledgment
We would like to thank Indian Council of Medical Research (ICMR) for providing the financial assistance for the study.
Footnotes
Source of Support: Indian Council of Medical Research provided financial assistance
Conflict of Interest: None declared.
References
- 1.SEARO, WHO. Vector-Borne Diseases in India: Report of Brainstorming Session, 2006. 2012. [Accessed on 2012 Sep 6]. Available from: http://www.searo.who.int/LinkFiles/CDS_vector-borne_diseases_in_India.pdf .
- 2.National Programme for Prevention and Control of Vector Borne Diseases: Malaria-Magnitude of Problem. 2012. [Accessed on 2012 Dec 25]. Available from: http://nvbdcp.gov.in/malaria3.htm .
- 3.World Health Organization. 2007. [Accessed on 2012 Dec 25]. Available from: http://www.whoindia.org/LinkFiles/Malaria Country Profile-Malaria.pdf .
- 4.Das A, Anvikar AR, Cator LJ, Dhiman RC, Eapen A, Mishra N, et al. Malaria in India: The center for the study of complex malaria in India. Acta Trop. 2012;121:267–73. doi: 10.1016/j.actatropica.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Programme for Prevention and Control of Vector Borne Diseases. 2012. [Accessed on 2012 Sep 7]. Available from: http://mohfw.nic.in/NRHM/PIP_09_10/Delhi/NVBDCP_text.pdf .
- 6.Pandit N, Patel Y, Bhavsar B. Knowledge and practice about preventive method against mosquito bite in Gujarat. Health Line. 2010;1:16–20. [Google Scholar]
- 7.Boratne AV, Datta SS, Singh Z, Purty A, Jayanthi V, Senthilvel V. Attitude and practices regarding mosquito borne diseases and socio-demographic determinants for use of personal protection methods among adults in coastal Pondicherry. IJMS. 2010;1:91–6. [Google Scholar]
- 8.Sharma AK, Bhasin S, Chaturvedi S. Predictors of knowledge about malaria in India. J Vector Borne Dis. 2007;44:189–97. [PubMed] [Google Scholar]
- 9.Patel AB, Rathod H, Shah P, Patel V, Garsondiya J, Sharma R. Perception regarding mosquito borne diseases in an urban area of Rajkot city. Natl J Med Res. 2011;1:45–7. [Google Scholar]
- 10.Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy's socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007;74:1131–2. [PubMed] [Google Scholar]
- 11.Armed Forces Pest Management Board. Personal Protective Measures Against Insects and Other Arthropods of Military Significance. 2012. [Updated on 2009 Oct; Accessed on 2012 Oct 24]. Available from: http://www.afpmb.org/sites/default/files/pubs/techguides/tg36.pdf .
- 12.WHO. Insecticide Treated Bed Nets: A WHO position Statement. 2012. [Accessed on 2012 Oct 24]. Available from: http://www.who.int/malaria/publications/atoz/itnspospaperfinal.pdf .
- 13.Smoke from mosquito coils may be as harmful as fumes from a vehicle exhaust. 2012. [Accessed on 2012 Oct 25]. Available from: http://www.caiindia.org/PDFs/mosquito%20coil_eng.pdf .
- 14.Cupp EW. Protection against mosquitoes. In: Dupont HL, Steffen R, editors. Textbook of Travel Medicine and Health. 2nd ed. Hamilton, Ontario: BC Decker; 2001. pp. 189–92. [Google Scholar]
- 15.Bonds JA. Ultra-low-volume space sprays in mosquito control: A critical review. Med Vet Entomol. 2012;26:121–30. doi: 10.1111/j.1365-2915.2011.00992.x. [DOI] [PubMed] [Google Scholar]
- 16.Salifou S, Gouissi FM, Edorh AP, Gbetoh MH, Gouissi SG, Okereke E, et al. Impact of propoxur use in indoor residual spraying (IRS) on malaria transmission in the commune of aguegues in Benin. Int J Biomol Biomed. 2012;2:13–20. [Google Scholar]
- 17.Vector Management and Control. 2012. [Accessed on 2012 Oct 14]. Available from: http://www.searo.who.int/LinkFiles/Dengue_DHF_pcg_ch9.pdf .
- 18.Klein RE, Weller SC, Zeissig R, Richards FO, Ruebush TK., 2nd Knowledge, beliefs, and practices in relation to malaria transmission and vector control in Guatemala. Am J Trop Med Hyg. 1995;52:383–8. doi: 10.4269/ajtmh.1995.52.383. [DOI] [PubMed] [Google Scholar]
- 19.Rasania SK, Bhanot A, Sachdev TR. Awareness and practices regarding malaria of catchment population of a primary health centre in Delhi. J Commun Dis. 2002;34:78–84. [PubMed] [Google Scholar]
- 20.Tyagi P, Roy A, Malhotra MS. Knowledge, awareness and practices towards malaria in communities of rural, semi-rural and bordering areas of east Delhi (India) J Vector Borne Dis. 2005;42:30–5. [PubMed] [Google Scholar]
- 21.Snehalatha KS, Ramaiah KD, Vijay Kumar KN, Das PK. The mosquito problem and type and costs of personal protection measures used in rural and urban communities in Pondicherry region, South India. Acta Trop. 2003;88:3–9. doi: 10.1016/s0001-706x(03)00155-4. [DOI] [PubMed] [Google Scholar]
- 22.Acharya A, Goswami K, Srinath S, Goswami A. Awareness about dengue syndrome and related preventive practices amongst residents of an urban resettlement colony of south Delhi. J Vector Borne Dis. 2005;42:122–7. [PubMed] [Google Scholar]
- 23.NVBDCP, MoHFW. Guidelines for Integrated Vector Management for Control of Dengue/Dengue Hemorrhagic Fever. [Internet] 2006. [Accessed on 2012 Dec 6]. Available from: http://nvbdcp.gov.in/Doc/dengue_1_.%20Director_Desk%20DGHS%20meeting%20OCT%2006.pdf .


