Abstract
Background: Effective physician communication at the end-of-life is a cornerstone to providing patient-centered palliative care. Educational programs in physician communication often rely on self-assessments of physician knowledge and attitudes and seldom provide patients' reports. Thus, it is unclear whether physician self-assessments are associated with patient perspectives.
Objective: To determine whether physician trainees' self-assessments of their communication skills in religious/spiritual discussions were associated with assessments obtained from patients under their care.
Design: Prospective, observational, survey-based study of internal medicine trainees' self-assessments matched with their patients' reports. Data were obtained from preintervention surveys prior to the trainees participating in a communication educational intervention.
Setting and subjects: The study took place at two internal medicine training programs, one in the southeastern United States and one in the northwestern United States. Our subjects were 181 physician trainees in internal medicine and 541 patients with advanced medical illnesses under their care.
Measurements: The outcomes were patient reports of the occurrence of religious/spiritual communication and patient ratings of the quality of this communication. The primary predictor of interest was trainees' preintervention self-assessments of their competency in religious/spiritual communication.
Results: Using multiple variable and path analysis we found that trainees' self-assessments of their communication skills in religious/spiritual communication was significantly and positively associated with their patients' reports of the occurrence and ratings of religious/spiritual communication.
Conclusions: Physician trainee self-assessments may be a valid surrogate for patient ratings of quality with respect to religious/spiritual communication. This specific domain of physician–patient communication should receive further investigation as our finding contrasts with reports of more general measures of physician–patient end-of-life communication.
Introduction
Effective physician–patient communication is considered an essential physician skill and vital to building a quality health care system that should include patient-centered care aligned with patients' beliefs and values.1 The Accreditation Council for Graduate Medical Education (ACGME) designated residents' interpersonal and communication skills as one of six core competencies2 and the Institute of Medicine designated a therapeutic healing relationship as a cornerstone for quality health care.1 The imperative for high-quality physician–patient communication is especially important in the context of end-of-life care.
Physician communication is responsible for more complaints and gratitude than any other aspect of care at the end-of-life.3 Thus, educational programs have been developed to improve physician skills in end-of-life communication.4–8 Evaluation measures for these educational programs have included self-assessments, expert observer checklists, and analysis of interactions with standardized patients. To date, studies suggest that physician self-assessments of overall communication skills are not associated with patient assessments,9,10 although no study has reported whether physician self-assessments of specific aspects of communication, such as religion and spirituality, are associated with patient or family evaluations of those particular physician communication skills.
As part of a 5-year, randomized trial to evaluate the effectiveness of a workshop to improve the communication skills of internal medicine trainees about end-of-life care, we collected preintervention surveys in which trainees self-assessed their competence in different aspects of communication about end-of-life care. In a prior publication we reported that physician trainees' self-assessments of their competence in communication about end-of-life care were not associated with the trainees' patient and family assessments of their communication skills.10 This implies that self-assessments of communication competence may be an inadequate outcome for interventions designed to improve communication. In the current report, we build on our prior work in religious and spiritual communication from this same study11 to examine the relationship between physician trainees' self-assessments of religious and spiritual communication and their patients' reports. Our hypothesis was that self-assessments may be more useful when targeted at a specific component of communication, such as communication about religion and spirituality.
Support for patients' and families' religious and spiritual needs is a cornerstone of palliative care12 yet is often inadequate from the perspective of patients.13–15 We previously used structural equation modeling to characterize physician trainees' self-assessed communication skills in discussing religion and spirituality and found that religious and spiritual discussions are an advanced communication skill as compared to other communication skills such as discussing do-not-resuscitate (DNR) status with patients and families.11 The objective of the current article is to describe the relationship between trainee preintervention self-assessed competence in discussing religion and spirituality and patients' assessments of trainees' competence in discussing religion and spirituality. Our ultimate goal is to provide a better understanding of the communication of religious and spiritual issues related to end-of-life care and help inform future intervention studies to improve this communication.16,17
Methods
Study design and setting
Data for this observational study were obtained from preintervention surveys completed by physician trainees over the entire course of the Improving Clinician Communication Skills (ICCS) study, a 5-year randomized trial of a simulation-based workshop designed to improve physicians' end-of-life communication skills. We also obtained surveys from patients under the trainees' care. All study procedures were approved by the Institutional Review Boards of all involved institutions.
Participants
Trainees
Trainees in internal medicine and select medicine specialty fellowships at the University of Washington and the Medical University of South Carolina were invited to participate in ICCS. Eligible trainees included internal medicine trainees in postgraduate years (PGY) 1–5 as well as fellows in geriatrics, nephrology, oncology, palliative medicine, and pulmonary/critical care medicine. A total of three recruitment attempts for nonrespondents were made and our overall acceptance rate for participation was 58% (n=395) of 680 eligible physicians, with 52% (n=352) of eligible physicians completing participation.
For the current analyses, we included 181 physician trainees of the 376 who were randomized (either as active participants or “usual education” controls). Trainees were excluded if they did not complete the preintervention self-assessment of skill in discussing religion/spirituality or if no patient under their care during the preintervention period had returned a rating of the trainee's skill in discussing religious/spiritual issues by August 16, 2012, when data were compiled for the analyses.
Patients
All patients in the study had either inpatient or outpatient clinical encounters with enrolled physician trainees and were identified by screening the medical records of patients cared for by an enrolled trainee. The clinical encounters occurred either in trainees' primary care or selected specialty clinic or during trainees' rotations through certain inpatient services (e.g., general medicine, medical intensive care unit, hematology–oncology). Eligible patients were those for whom it was likely that a discussion about end-of-life care would be indicated. These eligibility criteria included an approximately 1- to 2-year median survival based on published prediction criteria. We also included patients with documentation of end-of-life care or communication, an intensive care unit (ICU) stay of 72 hours or more, or aged 80 years or more with a hospital stay of 72 hours or more. For outpatients, we required three or more visits with the trainee to enhance opportunity to discuss end-of-life care. An additional patient eligibility criterion was that the patient knew the trainee well enough to evaluate the trainee's communication skills. Thus, study materials included a picture of the trainee to ensure that the patient recognized the trainee as someone who had provided clinical care to him or her. Both in-person and mail-based patient recruitment procedures were utilized with a total of three contacts for nonrespondents.
Of 2310 communicative patients who were paired with a physician trainee during the preintervention period, 696 (30%) evaluated at least one trainee. Of the 696, 544 (78%) were paired with a trainee who provided a preintervention self-assessment of skill in discussing religion/spirituality. The full dataset for ICCS included cross-clustering of patients and trainees. Trainees could be evaluated by multiple patients and patients could evaluate up to two trainees. To accommodate hierarchical modeling, we clustered patients under trainees and, for patients who completed evaluations of multiple preintervention trainees, selected one evaluation per patient for use in the analysis. In selecting between surveys, we gave preference to the survey for a trainee who had provided a preintervention self-assessment of skill in discussion religion/spirituality, and who had fewer evaluations from other patients. Where use of these criteria resulted in a tie, we randomly selected one of the patient's surveys for use. This selection of one survey per patient reduced the analysis sample to 541 patients.
Data collection
Patient surveys were mailed or hand-delivered between October 2007 and April 2012 to patients whose last visit with the trainee occurred prior to the trainee's participation in the ICCS communication skills training intervention.
Measures
Outcomes
We had two outcomes of interest for this study: (1) whether the patient rated the trainee's skill in discussing religion/spirituality implying the occurrence of a religious/spiritual discussion with the trainee (as opposed to selecting the “doctor did not do this” response option) and (2) the patient's numerical rating of the trainee's skill in discussing religion/spirituality. The rating item uses a 0–10 rating response scale; surveys where patients selected the “doctor did not do this” response option or one of several other missing data codes were excluded from the analysis of ratings. These items were obtained from the validated Quality of Communication (QOC) survey instrument18 that was completed by the trainee's patients.
Predictors
The primary predictor of interest for this article was a single item taken from the 17-item Perceived Competence Questionnaire5,10,19 in which trainees self-assessed their competence discussing religious or spiritual issues with patients and families. We also included several trainee and patient characteristics, selected a priori, as possible predictors: trainees' years of clinical training, age, sex, and race; and patients' age, sex, race, education attainment, income, comorbid disease burden (Charlson score),20 and self-assessed current health status.21
Data analysis
Data analysis included two phases, each based on regression modeling. In phase 1 we used bivariate and multiple-predictor regression models to evaluate the associations of variables in the predictor pool with the outcomes. We used clustered probit regression models for the dichotomous outcome of whether or not religious/spiritual discussions occurred. Because patient ratings of trainees' skills in discussing religion/spirituality had a strong ceiling effect (one third of the valid ratings having value of 10), we defined this outcome as censored from above and used clustered tobit regression models to evaluate its association with the predictors of interest. Tobit regression provides a method for analyzing outcomes with a strong ceiling effect by substituting for the measured outcome an estimation of a latent variable representing the “true” value of the outcome. Coefficients in both analyses were produced with weighted mean- and variance-adjusted least squares estimation.
Although multiple-predictor regression models are invaluable in providing information about factors that independently predict an outcome, we were also interested in the indirect paths of influence (i.e., the ways in which factors lacking an independent direct effect on the outcome of interest may have affected one another and thereby collaborated in producing the outcome). Therefore, in phase two we constructed two general path models,22 hypothesized in response to the findings from phase 1 and tested our hypothesized models of influence on patients' reports of the occurrence and quality of discussions about religious/spiritual issues. The first path model included six variables (site, patient race, age, education, and income and the trainee's self-assessed competency in discussing religious/spiritual topics) as predictors of the two outcomes of interest (occurrence and patient ratings of religious/spiritual discussions). The second model added the patient's self-assessed health status as a seventh predictor. In both models, we established site as an exogenous predictor, with the remaining predictors as potential mediating variables, and we began both as saturated models (i.e., models in which each variable was linked to all other variables in the model). We established the direction of the links between the predictors in the following order: site, black race, age, education, income, patient health status rating, and trainee self-rating of competency at religious/spiritual communication. We then simplified each of the two general models by removing statistically nonsignificant pathways, and compared the resulting model's deviance to that of the saturated model, thus ensuring that the simplified model was not a significant oversimplification of the causal pathways. Finally, we compared the deviances of the two simplified models to evaluate whether removal of health status significantly degraded the explanatory potential of the model. As with the regression models in phase one, we used a weighted mean- and variance-adjusted least squares estimator; defined the occurrence and rating outcomes as, respectively, categorical and censored from above; and reported probit and tobit regression coefficients, as appropriate.
We based all statistics on two-sided tests and labeled all results with p<0.05 as statistically significant. We used SPSS 17.0 for Windows (SPSS, Chicago, IL; www.spss.com/) for descriptive statistics, and Mplus 6.1 (Informer Technologies; www.statmodel.com/) for regression and path analyses.
Results
The physician trainee characteristics and self-assessments of communication competencies are provided in Table 1. A majority of trainees were PGY1 (61%) and most reported they had conducted at least one end-of-life treatment discussion at study entry. Only 13% had never conducted an end-of-life treatment discussion. In general, physician trainees rated their communication competence in discussing religious/spiritual and existential issues lower than their competency in discussing medical decisions such as DNR status.
Table 1.
Physician Trainee Characteristics and Self-Assessments of Select End-of-Life Communication Competencies
| Trainee characteristics and self-assessments (n=181) | |
|---|---|
| Study site, n (%) | |
| Northwest | 115 (64) |
| Southeast | 66 (36) |
| Female, n (%) | 96 (53) |
| Race/ethnicity, n (%) | |
| African American | 6 (3) |
| Other racial/ethnic minority | 32 (18) |
| White non-Hispanic | 143 (79) |
| Age, mean (SD) | 29.8 (4.9) |
| Postgraduate year, n (%) | |
| 1 | 111 (61) |
| 2 | 27 (15) |
| 3 | 21 (12) |
| >3 | 22 (12) |
| Number of end-of-life treatment discussions | |
| None, n (%) | 23 (13) |
| 1–3, n (%) | 75 (42) |
| 4+, n (%) | 81 (45) |
| Satisfaction with skills/knowledge,a mean (SD) | 5.5 (1.8) |
| Self-assessed competence,b median (IQR) | |
| Discussing religious/spiritual issues | 3 (1) |
| Eliciting patients' fears for end of life | 3 (2) |
| Response to desire for inappropriate treatment | 3 (1) |
| Discussing DNR status with patients | 4 (1) |
| Discussing DNR status with families | 4 (1) |
Response scale for trainee's satisfaction with knowledge of end-of-life issues and skills in palliative care 0 (not at all satisfied) to 10 (completely satisfied)
Response scale for competence ratings: 1 (not very competent)…3 (somewhat competent)…5 (very competent)
SD, standard deviation; IQR, interquartile range; DNR, do not resuscitate.
Patient characteristics and patient ratings of the physician trainees' religious/spiritual communication are provided in Table 2. Our patient population came from diverse backgrounds with 33% being non-white race and 83% having an educational attainment of at least a high school diploma. The self-reported health status among our patients was generally low with a median rating “fair” and a majority of patients reported they had participated in a religious/spiritual discussion with the trainee.
Table 2.
Patient Characteristics and Ratings of Trainees' Communication Competencies in Religious/Spiritual Discussion
| Patient characteristics and ratings of trainees | |
|---|---|
| Study site, n (%) | |
| Northwest | 328 (61) |
| Southeast | 213 (39) |
| Female, n (%) | 243 (45) |
| Race/ethnicity, n (%) | |
| African American | 124 (23) |
| Other racial/ethnic minority | 56 (10) |
| White non-Hispanic | 361 (67) |
| Age, mean (SD) | 65.6 (13.9) |
| Education, n (%) | |
| Eighth grade or less | 37 (7) |
| Some high school | 52 (10) |
| High school diploma or equivalent | 111 (21) |
| Trade school or some college | 163 (31) |
| Four-year college degree | 79 (15) |
| Graduate or professional school | 78 (15) |
| Income, n (%) | |
| $500 or less | 26 (6) |
| $1000 or less | 92 (20) |
| $1500 or less | 67 (15) |
| $2000 or less | 52 (11) |
| $3000 or less | 61 (13) |
| $4000 or less | 44 (10) |
| More than $4000 | 119 (26) |
| Charlson comorbidity score, mean (SD) | 5.4 (2.1) |
| Self-assessed current health status,a median (IQR) | 1 (2) |
| Had religious/spiritual discussion with trainee, n (%) | 294 (54) |
| Rating of trainee's skill in religious/spiritual discussion,b mean (SD) | 7.6 (2.7) |
Single-item health rating from the SF-12 Health Survey, recoded so that higher scores indicated better self-assessed health status: 0 (poor), 1 (fair), 2 (good), 3 (very good), 4 (excellent).
The rating scale ran from 0 (poor) to 10 (absolutely perfect).
SD, standard deviation; IQR, interquartile range.
Results of our regression analyses are shown in Tables 3 and 4. Table 3 provides the findings of our single-predictor and multiple-predictor regression models for the occurrence of religious/spiritual discussions as reported by trainee's patients. Patient characteristics associated with the occurrence of religious/spiritual discussion in our single-predictor models included a positive association with African American race and an inverse association with educational attainment and income. African American race and income remained statistically significant in our multiple-predictor model. The only trainee characteristic associated with the occurrence of religious/spiritual discussion was southeastern site (single-predictor analysis) although this was not statistically significant in the multiple-predictor analyses.
Table 3.
Associations of Patient and Trainee Characteristics with Occurrence of Religious/Spiritual Discussions (clustered probit regression models)a
| Single-predictor modelsb | Multiple-predictor modelc | |||||
|---|---|---|---|---|---|---|
| b | p | CI | b | p | CI | |
| Patient characteristics | ||||||
| Age | −0.005 | 0.151 | −0.013, 0.002 | −0.004 | 0.365 | −0.014, 0.003 |
| Female | −0.076 | 0.426 | −0.264, 0.112 | −0.220 | 0.072 | −0.459, 0.019 |
| Race/ethnicity | <0.001 | 0.003 | ||||
| African American | 0.560 | 0.296, 0.824 | 0.505 | 0.157, 0.853 | ||
| Other minority | 0.165 | −0.187, 0.518 | 0.222 | −0.173, 0.617 | ||
| Educationd | −0.140 | 0.001 | −0.221, −0.059 | −0.082 | 0.111 | −0.182, 0.019 |
| Incomee | −0.130 | <0.001 | −0.188, −0.072 | −0.086 | 0.021 | −0.159, −0.013 |
| Charlson comorbidity score | 0.036 | 0.114 | −0.009, 0.081 | 0.046 | 0.113 | −0.011, 0.102 |
| Self-assessed current health statusf | 0.010 | 0.847 | −0.096, 0.117 | −0.016 | 0.802 | −0.138, 0.107 |
| Trainee characteristics | ||||||
| Southeastern site | 0.280 | 0.006 | 0.079, 0.481 | 0.007 | 0.963 | −0.271, 0.284 |
| Years of clinical training | 0.010 | 0.783 | −0.060, 0.079 | −0.062 | 0.132 | −0.142, 0.019 |
| Age | 0.013 | 0.332 | −0.013, 0.040 | 0.020 | 0.252 | −0.015, 0.055 |
| Female | −0.022 | 0.830 | −0.218, 0.175 | 0.070 | 0.549 | −0.158, 0.298 |
| Race/ethnicity | 0.087 | 0.359 | ||||
| African American | 0.074 | −0.414, 0.561 | 0.024 | −0.509, 0.557 | ||
| Other minority | −0.245 | −0.478, −0.011 | −0.164 | −0.428, 0.101 | ||
| Self-assessed competence | ||||||
| Discussing religious/spiritual issues | 0.077 | 0.129 | −0.022, 0.176 | 0.046 | 0.464 | −0.076, 0.167 |
Associations evaluated with clustered probit regression models (dichotomous outcome), with estimates based on weighted mean- and variance-adjusted least squares.
Single-predictor models based on 541 surveys evaluating 181 trainees, except where otherwise indicated.
Multiple-predictor model based on 431 surveys evaluating 176 trainees.
Single-predictor model based on 520 surveys evaluating 180 trainees.
Single-predictor model based on 461 surveys evaluating 177 trainees.
Single-predictor model based on 516 surveys evaluating 181 trainees.
CI, confidence interval.
Table 4.
Association of Patient and Trainee Characteristics with Patient Ratings of Religious/Spiritual Discussions (clustered tobit regression models)a
| Single-predictor modelsb | Multiple-predictor modelsc | |||||
|---|---|---|---|---|---|---|
| b | p | CI | b | p | CI | |
| Patient characteristics | ||||||
| Age | −0.012 | 0.605 | −0.056, 0.033 | −0.005 | 0.857 | −0.060, 0.050 |
| Female | 0.533 | 0.365 | −0.620, 1.687 | 1.329 | 0.077 | −0.145, 2.803 |
| Race/ethnicity | 0.622 | 0.652 | ||||
| African American | 0.407 | −0.931, 1.745 | −0.227 | −2.044, 1.590 | ||
| Other minority | 0.139 | −1.687, 1.964 | 0.459 | −1.485, 2.403 | ||
| Educationd | −0.135 | 0.587 | −0.623, 0.352 | −0.095 | 0.754 | −0.690, 0.500 |
| Incomee | 0.126 | 0.476 | −0.219, 0.471 | 0.200 | 0.270 | −0.156, 0.557 |
| Charlson comorbidity score | −0.090 | 0.550 | −0.385, 0.205 | −0.242 | 0.117 | −0.544, 0.060 |
| Self-assessed current health statusf | 0.658 | 0.013 | 0.141, 1.175 | 0.762 | 0.014 | 0.157, 1.367 |
| Trainee characteristics | ||||||
| Southeastern site | 1.593 | 0.010 | 0.385, 2.801 | 1.524 | 0.079 | −0.178, 3.226 |
| Years of clinical training | −0.240 | 0.247 | −0.646, 0.166 | −0.458 | 0.126 | −1.046, 0.130 |
| Age | −0.027 | 0.721 | −0.173, 0.120 | 0.089 | 0.320 | −0.086, 0.263 |
| Female | 0.615 | 0.322 | −0.602, 1.832 | 0.709 | 0.296 | −0.621, 2.040 |
| Race/ethnicity | 0.113 | 0.671 | ||||
| African American | 1.920 | −0.370, 4.211 | 0.682 | −2.413, 3.776 | ||
| Other minority | −0.790 | −2.255, 0.675 | −0.137 | −1.742, 1.468 | ||
| Self-assessed competence | ||||||
| Discussing religious/spiritual issues | 0.756 | 0.008 | 0.201, 1.312 | 0.723 | 0.037 | 0.044, 1.402 |
Associations evaluated with clustered tobit regression models (outcome ratings censored from above), with estimates based on weighted mean- and variance-adjusted least squares.
Single-predictor models based on 168 surveys evaluating 119 trainees, except where otherwise indicated.
Multiple-predictor model based on 144 surveys evaluating 107 trainees.
Single-predictor model based on 162 surveys evaluating 115 trainees.
Single-predictor model based on 149 surveys evaluating 110 trainees.
Single-predictor model based on 167 surveys evaluating 119 trainees.
CI, confidence interval.
Table 4 provides results from single-predictor and multiple-predictor regression analyses on patient ratings of trainee skill in discussing religion/spirituality. The only patient characteristic associated with the patient's rating of trainee skill was a positive association with higher self-assessed current health status. This was true in our single-predictor and the multiple-predictor models. The only trainee characteristic associated with greater patient ratings of the trainee's skill in discussing religion/spirituality in the multiple-predictor model was greater trainee self-assessed competence in religious/spiritual communication. Southeastern site was associated with higher patient ratings in our single-predictor model but lost statistical significance in the multiple-predictor model.
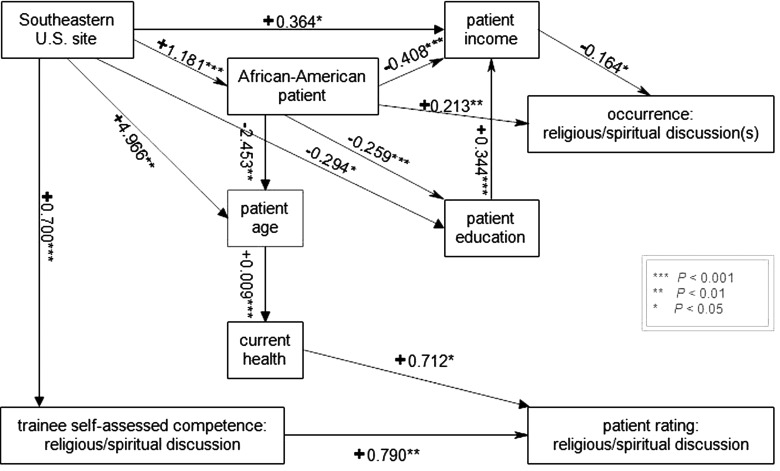
Our single-predictor and multiple-predictor regression analyses suggested complex relationships between certain patient measures and the occurrence and ratings of religious/spiritual communication with trainees, such that some predictors were likely acting as mediators between other predictors and the outcome. Therefore, we developed and refined two path models, with the model shown in Figure 1 providing the best estimate of the direct and indirect effects of our predictors of interest on the two religious/spiritual communication outcomes. A summary of these effects is provided in Table 5. Southeastern recruitment site and African American race had an overall positive association with the occurrence of religious/spiritual communication whereas patient education attainment and income had overall negative effects, with some of these variables demonstrating a direct influence and others operating indirectly through mediating variables. For example, patient education did not directly influence the occurrence of religious/spiritual discussion but instead exerted its effect through a mediating variable: patient income. Patient self-assessed current health and trainee self-assessed competence in communication about religion/spirituality were significantly, directly, and positively associated with patient ratings of trainee's skill in discussing religious/spiritual issues. Southeastern training site and patient age were significantly and positively associated with patient ratings of trainee's skills in discussing religious/spiritual issues, but appeared to exert their effect indirectly, through their association with mediating variables. For example, patient age exerted its effect by affecting patient-reported current health status, which in turn affected ratings of religious/spiritual discussion.
FIG. 1.
Hypothesized path model for occurrence and ratings of religious/spiritual discussion. See Table 5 for estimates of direct, indirect, and total effects.
Table 5.
Estimates of Direct, Indirect, and Total Effects in the Path Model
| Direct effect | Indirect effect | Total effect | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Predictor | b | pa | b | pa | b | pa |
| Occurrence of discussions | Recruitment siteb | 0.000 | 0.999 | 0.305 | <0.001 | 0.305 | <0.001 |
| African American patient | 0.213 | 0.005 | 0.082 | 0.015 | 0.295 | <0.001 | |
| Patient ageb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient educationb | 0.000 | 0.999 | −0.057 | 0.033 | −0.057 | 0.033 | |
| Patient incomec | −0.164 | 0.017 | 0.000 | 0.999 | −0.164 | 0.017 | |
| Self-assessed current healthb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Self-assessed competenceb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient rating of discussions | Recruitment siteb | 0.000 | 0.999 | 0.567 | 0.009 | 0.567 | 0.009 |
| African American patientb | 0.000 | 0.999 | −0.017 | 0.057 | −0.017 | 0.057 | |
| Patient ageb | 0.000 | 0.999 | 0.007 | 0.025 | 0.007 | 0.025 | |
| Patient educationb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient incomeb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Self-assessed current healthc | 0.712 | 0.012 | 0.000 | 0.999 | 0.712 | 0.012 | |
| Self-assessed competencec | 0.790 | 0.002 | 0.000 | 0.999 | 0.790 | 0.002 | |
| African American patient | Recruitment sitec | 1.181 | <0.001 | 0.000 | 0.999 | 1.181 | <0.001 |
| Patient age | Recruitment site | 4.966 | 0.003 | −2.897 | 0.005 | 2.070 | 0.120 |
| African American patientc | −2.453 | 0.003 | 0.000 | 0.999 | −2.453 | 0.003 | |
| Patient education | Recruitment site | −0.294 | 0.018 | −0.306 | <0.001 | −0.600 | <0.001 |
| African American patientc | −0.259 | <0.001 | 0.000 | 0.999 | −0.259 | <0.001 | |
| Patient ageb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient income | Recruitment site | 0.364 | 0.015 | −0.688 | 0.001 | −0.324 | 0.016 |
| African American patient | −0.408 | <0.001 | −0.089 | <0.001 | −0.497 | <0.001 | |
| Patient ageb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient educationc | 0.344 | <0.001 | 0.000 | 0.999 | 0.344 | <0.001 | |
| Self-assessed current health | Recruitment siteb | 0.000 | 0.999 | 0.020 | 0.180 | 0.020 | 0.180 |
| African American patientb | 0.000 | 0.999 | −0.023 | 0.036 | −0.023 | 0.036 | |
| Patient agec | 0.009 | 0.001 | 0.000 | 0.999 | 0.009 | 0.001 | |
| Patient educationb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient incomeb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Self-assessed competence | Recruitment sitec | 0.700 | <0.001 | 0.000 | 0.999 | 0.700 | <0.001 |
| African American patientb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient ageb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient educationb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Patient incomeb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
| Self-assessed current healthb,c | 0.000 | 0.999 | 0.000 | 0.999 | 0.000 | 0.999 | |
The p values for relationships that were constrained to 0.000 in the model are shown as 0.999. The combined constraints did not significantly degrade model fit (p=0.2381, when compared with a saturated model).
The direct effect of this predictor was constrained to 0.000 in the hypothesized model because the path was not statistically significant in an alternative model in which it was freely estimated.
The indirect effect of this predictor was constrained to 0.000 in the hypothesized model because the path or paths that constituted it were not statistically significant in an alternative model in which they were freely estimated.
Discussion
Our findings offer important insights into physician–patient communication and are novel in that we were able to directly link physician trainees' self-assessments of competency with evaluations from patients under the trainees' care. In educational programs designed to teach end-of-life skills, self-assessments are common measures of knowledge and attitudes5–7 although the validity of self-assessment as an outcome measure is controversial.9,23,24 In previous work we demonstrated that trainees' global self-assessed end-of-life communication skills were not associated with their patients' ratings.10 However, religious/spiritual communication between physicians and patients may be unique and sufficiently specific to detect the associations we report. Religious/spiritual communication is also uniquely challenging because of discrepant perspectives between patients and physicians.13
Patients and families characterize religious and spiritual beliefs as important when they are confronting serious illness and end-of-life care. This has been documented in a variety of clinical settings, including outpatient, inpatient, intensive care, and palliative care.14,25–30 Religion and spirituality have an impact on multiple health outcomes including quality of life,31,32 mental health,30,33–35 coping with serious illness,26,34,36,37 medical decision-making,14,27,38,39 and use of intensive life-prolonging treatments prior to death.40 Surveys from 1,732,652 patients in the National Inpatient Database found that spiritual needs were ranked second in the National Inpatient Priority Index.13 While 58% of patients thought it appropriate for their physicians to inquire about spiritual needs, only 6% reported that any staff had inquired about them and only 0.9% of the inquiries came from physicians.13
In contrast to patients' and families' perspectives, physicians do not perceive religion and spirituality to be as relevant with the result that these topics are often neglected during patient–physician encounters.13 Investigation among physicians consistently finds that religion and spirituality are omitted during discussions with patients and families.13–15,38,41 Notably, 54% of patients in our study reported having a religious or spiritual discussion with the trainee which is significantly higher than in these reports. Nonetheless, a substantial proportion of our patient surveys could not be used to evaluate hypotheses related to the quality of communication about religious and spiritual issues.
The physician trainees in our study who had higher self-assessments of their competency in religious/spiritual communication may be distinct from their peers with greater self-efficacy in this particular dimension of communication, translating into the higher patient ratings we identified. Since we did not collect information on trainee's religious/spiritual beliefs we cannot answer how their personal beliefs might influence our findings. Future investigation should obtain this information as a potentially important covariate influencing patient and family experience in addressing religious/spiritual needs.
Religion/spirituality consistently emerges as a particularly important aspect in end-of-life care and communication among African American patients and their surrogates.39,42–49 Indeed, in our path analysis African American patient race was significantly and positively associated with the occurrence of religious/spiritual communication. These findings highlight the call to develop and evaluate culturally sensitive communication techniques that elicit and support potential religious/spiritual needs and may represent an important strategy for reducing health disparities.
The relationship we identified between patient education attainment and income is congruent with the common observation that higher educational achievement confers greater socioeconomic status including income. More complex is the inverse relationship we identified between patient education attainment and income with the occurrence of religious/spiritual communication. This may in part be related to the observation that lower socioeconomic status is associated with greater degrees of religiosity50 and perhaps patients from lower socioeconomic status were thus more likely to raise a religious/spiritual issue with the trainee.
Patients with higher self-assessed health status also gave higher ratings of trainee skill in discussing religious/spiritual issues. This may be because higher health status ratings are often associated with more positive perceptions in a variety of domains including illness perceptions,37 mental health,51 and health behaviors.52 Neurobiological mechanisms for this “optimism bias' have even been characterized53 and perhaps the patients with higher self-reported health status reflect this phenomenon.
The influence of southeastern U.S. site was significant in our path analysis for both the occurrence and rating of religious/spiritual communication. This may reflect the greater prevalence of religion/religiosity in the southeastern United States compared to the northwestern United States54 and thus southeastern trainees may have personal beliefs that give them more self-assessed competence in this specific communication skill. In addition, the southeastern trainees may encounter religious/spiritual values among their patients and families more frequently and thus may acquire greater competence in religious/spiritual communication. Inquiry into the regional influences in other geographic areas of the United States is an important future direction.
While our study offers important insights we acknowledge some limitations. The proportion of eligible trainees participating in the parent ICCS trial is 52%, which may limit generalizability. Additionally, 61% of our trainees were PGY1 and we may have found different results among more experienced physicians. Future investigation should include physicians further along their professional trajectory. Finally, path analysis is an exploratory procedure and thus our findings should be taken as hypothesis generating rather than definitive.
In summary, using both traditional regression analysis and path analysis, we found that trainees' self-assessments of their skill in religious/spiritual communication were significantly and positively associated with patients' ratings of the trainee's skill in religious/spiritual communication. However, we did not find an association between self-assessments and the patient's assessments of the occurrence of religious/spiritual communication. We also found that African American race was associated with greater occurrence of religious/spiritual discussions but not with ratings of the quality of religious/spiritual communication. Physician trainee self-assessments may be a valid surrogate for patient ratings of quality with respect to religious/spiritual communication. This specific domain of physician-patient communication should receive further investigation as our finding contrasts with reports of more general measures of physician–patient end-of-life communication.10 As our health care system strives to identify strategies to evaluate for and attempt to meet the religious/spiritual needs of patients and families in order to provide patient-centered care, physician training should be a priority and self-assessment of physician skill may be a useful tool.
Acknowledgments
Funded by NIH-NINR R01NR009987. Registered at ClinicalTrials.gov: NCT00687349
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press, 2001 [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education: ACGME Program Requirements for Graduate Medical Education in Internal Medicine, 2009 [Google Scholar]
- 3.Field M, Cassel CK. (eds): Approaching Death: Improving Care at the End of Life. Washington, D.C.: National Academy Press, 1997 [PubMed] [Google Scholar]
- 4.Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE, Gooley TA, Tulsky JA: Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–460 [DOI] [PubMed] [Google Scholar]
- 5.Baile WF, Kudelka AP, Beale EA, Glober GA, Myers EG, Greisinger AJ, Bast RC, Jr, Goldstein MG, Novack D, Lenzi R: Communication skills training in oncology. Description and preliminary outcomes of workshops on breaking bad news and managing patient reactions to illness. Cancer 1999;86:887–897 [PubMed] [Google Scholar]
- 6.Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R: Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet 2002;359:650–656 [DOI] [PubMed] [Google Scholar]
- 7.Torke AM, Quest TE, Kinlaw K, Eley JW, Branch WT, Jr: A Workshop to teach medical students communication skills and clinical knowledge about end-of-life care. J Gen Intern Med 2004;19:540–544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Downar J, Knickle K, Granton JT, Hawryluck L: Using standardized family members to teach communication skills and ethical principles to critical care trainees. Crit Care Med 2012;40:1814–1819 [DOI] [PubMed] [Google Scholar]
- 9.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L: Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA 2006;296:1094–1102 [DOI] [PubMed] [Google Scholar]
- 10.Dickson RP, Engelberg RA, Back AL, Forrd DW, Curtis JR: Internal medicine trainee self-assessments of end-of-life communication skills do not predict assessments of patients, families, or clinician-evaluators. J Palliat Med 2012;15:418–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ford DW, Downey L, Engelberg R, Back AL, Curtis JR: Discussing religion and spirituality is an advanced communication skill: An exploratory structural equation model of physician trainee self-ratings. J Palliat Med 2012;15:63–70 [DOI] [PubMed] [Google Scholar]
- 12.National Consensus Project For Quality Palliative Care: Clinical Practice Guidelines for Quality Palliative Care. Pittsburgh, PA: National Consensus Project For Quality Palliative Care, 2004 [DOI] [PubMed] [Google Scholar]
- 13.Clark PA, Drain M, Malone MP: Patient centeredness: Addressing patients' emotional and spiritual needs. Jt Comm J Qual Saf 2003;29:659–670 [DOI] [PubMed] [Google Scholar]
- 14.Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen-Flaschen J: Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803–1806 [DOI] [PubMed] [Google Scholar]
- 15.Monroe MH, Bynum D, Susi B, Phifer N, Schultz L, Franco M, MacLean CD, Cykert S, Garrett J: Primary care physician preferences regarding spiritual behavior in medical practice. Arch Intern Med 2003;163:2751–2756 [DOI] [PubMed] [Google Scholar]
- 16.Borneman T, Ferrell B, Puchalski CM: Evaluation of the FICA Tool for Spiritual Assessment. J Pain Symptom Manag 2010;40:163–173 [DOI] [PubMed] [Google Scholar]
- 17.Puchalski C, Ferrell B, Virani R, Otis-Green S, Baird P, Bull J, Chochinov H, Handzo G, Nelson-Becker H, Prince-Paul M, Pugliese K, Sulmasy D: Improving the quality of spiritual care as a dimension of palliative care: The report of the consensus conference. J Palliat Med 2009;12:885–904 [DOI] [PubMed] [Google Scholar]
- 18.Engelberg R, Downey L, Curtis J: Psychometric characteristics of a quality of communication questionnaire assessing communication about end-of-life care. J Palliat Med 2006;9:1086–1098 [DOI] [PubMed] [Google Scholar]
- 19.Maguire P: Can communication skills be taught? Br J Hosp Med 1990;43:215–216 [PubMed] [Google Scholar]
- 20.Charlson M, Pompei P, Ales K, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudional studies: Development and validation. J Chronic Dis 1987;40:373–383 [DOI] [PubMed] [Google Scholar]
- 21.Hays RD, Sherbourne CD, Mazel RM: User's Manual for the Medical Outcomes Study (MOS) Core Measures of Health-Related Quality of Life. Santa Monica, CA: RAND, 1995 [Google Scholar]
- 22.Kline RB. Principles and Practice of Structural Equation Modeling. New York: Guilford Press; 2011. pp. 103–112. [Google Scholar]
- 23.Barnsley L, Lyon PM, Ralston SJ, Hibbert EJ, Cunningham I, Gordon FC, Field MJ: Clinical skills in junior medical officers: A comparison of self-reported confidence and observed competence. Med Educ 2004;38:358–367 [DOI] [PubMed] [Google Scholar]
- 24.Fitzgerald JT, White CB, Gruppen LD: A longitudinal study of self-assessment accuracy. Med Educ 2003;37:645–649 [DOI] [PubMed] [Google Scholar]
- 25.King DE, Bruce B: Beliefs and attitudes of hospital inpatients about faith healing and prayer. J Fam Pract 1994;39:349–352 [PubMed] [Google Scholar]
- 26.Koenig HG: Religious attitudes and practices of hospitalized medically ill older adults. Int J Geriatr Psychiatry 1998;13:213–224 [DOI] [PubMed] [Google Scholar]
- 27.McCord G, Gilchrist VJ, Grossman SD, King BD, McCormick KE, Oprandi AM, Schrop SL, Selius BA, Smucker DO, Weldy DL, Amorn M, Carter MA, Deak AJ, Hefzy H, Srivastava M: Discussing spirituality with patients: A rational and ethical approach. Ann Fam Med 2004;2:356–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abbott KH, Sago JG, Breen CM, Abernethy AP, Tulsky JA: Families looking back: One year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med 2001;29:197–201 [DOI] [PubMed] [Google Scholar]
- 29.Wall RJ, Engelberg RA, Gries CJ, Glavan B, Curtis JR; Spiritual care of families in the intensive care unit. Crit Care Med 2007;35:1084–1090 [DOI] [PubMed] [Google Scholar]
- 30.Nelson CJ, Rosenfeld B, Breitbart W, Galietta M; Spirituality, religion, and depression in the terminally ill. Psychosomatics 2002;43:213–220 [DOI] [PubMed] [Google Scholar]
- 31.Ferriss AL: Religion and the quality of life. J Happiness Stud 2002;3:199–215 [Google Scholar]
- 32.Balboni TA, Paulk ME, Balboni MJ, Phelps AC, Loggers ET, Wright AA, Block SD, Lewis EF, Peteet JR, Prigerson HG: Provision of spiritual care to patients with advanced cancer: Associations with medical care and quality of life near death. J Clin Oncol 2010;28:445–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koenig HG, Larson DB: Religion and mental health: Evidence for an association. Int Rev Psychiatry 2001;13:67–78 [Google Scholar]
- 34.McClain C, Rosenfeld B, Breitbart W: Effect of spiritual well-being on end-of-life despair in terminally ill patients. Lancet 2003;361:1603–1607 [DOI] [PubMed] [Google Scholar]
- 35.Woods TE, Antoni MH, Ironson GH, Kling DW: Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosom Res 1999;46:165–176 [DOI] [PubMed] [Google Scholar]
- 36.Tarakeshwar N, Vanderwerker LC, Paulk E, Pearce MJ, Kasl SV, Prigerson HG: Religious coping is associated with the quality of life of patients with advanced cancer. J Palliat Med 2006;9:646–657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ford D, Zapka J, Gebregziabher M, Yang C, Sterba K: Factors associated with illness perception among critically ill patients and surrogates. Chest 2010;138:59–67 [DOI] [PubMed] [Google Scholar]
- 38.Silvestri GA, Knittig S, Zoller JS, Nietert PJ: Importance of faith on medical decisions regarding cancer care. J Clin Oncol 2003;21:1379–1382 [DOI] [PubMed] [Google Scholar]
- 39.Balboni TA, Vanderwerker LC, Block SD, Paulk ME, Lathan CS, Peteet JR, Prigerson HG: Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol 2007;25:555–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phelps AC, Maciejewski PK, Nilsson M, Balboni TA, Wright AA, Paulk ME, Trice E, Schrag D, Peteet JR, Block SD, Prigerson HG: Religious coping and use of intensive life-prolonging care near death in patients with advanced cancer. JAMA 2009;301:1140–1147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kristeller JL, Zumbrun CS, Schilling RF: ‘I would if I could’: How oncologists and oncology nurses address spiritual distress in cancer patients. Psychooncology 1999;8:451–458 [DOI] [PubMed] [Google Scholar]
- 42.Branch WT, Torke A, Brown-Haithco RC: The importance of spirituality in African-Americans' end-of-life experience. J Gen Intern Med 2006;21:1203–1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Braun UK, Beyth RJ, Ford ME, McCullough LB: Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med 2008;23:267–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shrank WH, Kutner JS, Richardson T, Mularski RA, Fischer S, Kagawa-Singer M: Focus group findings about the influence of culture on communication preferences in end-of-life care. J Intern Med 2005;20:703–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kagawa-Singer M, Blackhall LJ: Negotiating cross-cultural issues at the end of life: “You got to go where he lives.” JAMA 2001;286:2993–3001 [DOI] [PubMed] [Google Scholar]
- 46.Koenig B: Cultural diversity in decision-making about care at the end of life. In: Field M, Cassel C. (eds): Approaching Death: Improving Care at the End of Life. Washington, D.C.: National Academy Press, 1997, pp. 363–382 [PubMed] [Google Scholar]
- 47.Loggers ET, Maciejewski PK, Paulk E, DeSanto-Madeya S, Nilsson M, Viswanath K, Wright AA, Balboni TA, Temel J, Stieglitz H, Block S, Prigerson HG: Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol 2009;27:5559–5564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S; Initiative to Improve Palliative and End-of-Life Care in the African American Community: Palliative and end-of-life care in the African American community. JAMA 2000;284:2518–2521 [DOI] [PubMed] [Google Scholar]
- 49.Johnson KS, Elbert-Avila KI, Tulsky JA: The influence of spiritual beliefs and practices on the treatment preferences of African Americans: A review of the literature. J Am Geriatr Soc 2005;53:711–719 [DOI] [PubMed] [Google Scholar]
- 50.Brandt MJ, Henry PJ. Psychological defensiveness as a mechanism explaining the relationship between low socioeconomic status and religiosity. Int J Psychol Relig 2012;22:321–332 [Google Scholar]
- 51.Fava GA, Tomba E: Increasing psychological well-being and resilience by psychotherapeutic methods. J Pers 2009;77:1903–1934 [DOI] [PubMed] [Google Scholar]
- 52.Steptoe A, Dockray S, Wardle J: Positive affect and psychobiological processes relevant to health. J Pers 2009;77:1747–1776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sharot T, Riccardi AM, Raio CM, Phelps EA: Neural mechanisms mediating optimism bias. Nature 2007;450:102–105 [DOI] [PubMed] [Google Scholar]
- 54.The Pew Forum on Religion and Public Life 2009: How religious is your state? http://pewforum.org/How-Religious-Is-Your-State-.aspx (Last accessed March23, 2011)