Abstract
Background: Pediatricians cite a lack of physical activity referral (PAR) opportunities as a major barrier to treating obesity. However, no literature exists on PARs for youth in the clinical setting. This study explores the feasibility of implementing PARs in a pediatric obesity clinic.
Methods: Patients ages 6–18 years in an obesity clinic from July 2010 to October 2011 were referred to PARs in their community. Researchers confirmed enrollment and participation in activities by follow-up phone calls.
Results: Of 130 eligible youth, 102 (78%) agreed to be referred to a physical activity program; 45 (35%) enrolled and 35 (27%) reported actually participating in an activity, for an average of 1.4 hours per week. Youth participated in 9 of 69 available activity programs included in the PAR network. Patient characteristics at baseline did not predict participation in an activity. Youth referred to organizations that contacted interested families were 5 times as likely to enroll in activities as youth referred to organizations that did not contact families (p<0.001).
Conclusion: Although only 27% of eligible youth participated in an activity through the PAR network, exposing 1 in 4 obese youth to 1.4 hours of physical activity weekly could have a significant public health impact. These results suggest that PAR networks for overweight and obese youth should focus on organizations that have the infrastructure to contact youth and their families, and that a small number of physical activity programs could form the basis for launching PAR networks.
Introduction
Increasing physical activity is critical in treating obese youth: Not only can physical activity reduce obesity,1 but it can also reduce cardiovascular risk (CVR) independent of changes in weight.2 Despite the importance of promoting activity among obese youth, healthcare providers frequently cite a lack of physical activity referral (PAR) options as a major barrier to treating obesity.3–5
Although there is limited research on PARs in the United States, PARs have been widely studied among adults in the UK and Scandinavia.6,7 Those studies, in which medical providers linked patients to community exercise programs, demonstrated increases in physical activity among adults and weight loss in the short term.6,7 However, no studies have documented the use of PARs among youth. Youth may not participate in PARs as readily as adults, because youth lack autonomy and would depend on adults for logistical support.
To address this research gap, this study sought to determine the feasibility of implementing a PAR network in a pediatric obesity clinic by examining the proportion of eligible youth who were willing to be referred and who ultimately participated in a physical activity program. Additionally, predictors of participation were examined and the dose of physical activity achieved among participants was estimated.
Methods
Design
This was a retrospective chart review approved by the University of California San Francisco's (San Francisco, CA) Committee on Human Research.
The setting was a multidisciplinary pediatric obesity clinic, which has been described previously.8 In early 2010, clinic staff created a PAR database of 69 community organizations (e.g., YMCA and Boys & Girls Clubs) offering physical activities in San Francisco. Organizations were identified through Internet searches and word of mouth, and clinic staff recorded the schedule of activities offered, age requirements, location, and cost for each organization. Costs ranged from free to $630, with 23% of activities being free. Clinic staff contacted all organizations to identify an on-site coordinator whom patients could contact. Eight of the 69 organizations offered to directly contact patients interested in some or all of their activities and requested that the clinic provide contact information for interested patients.
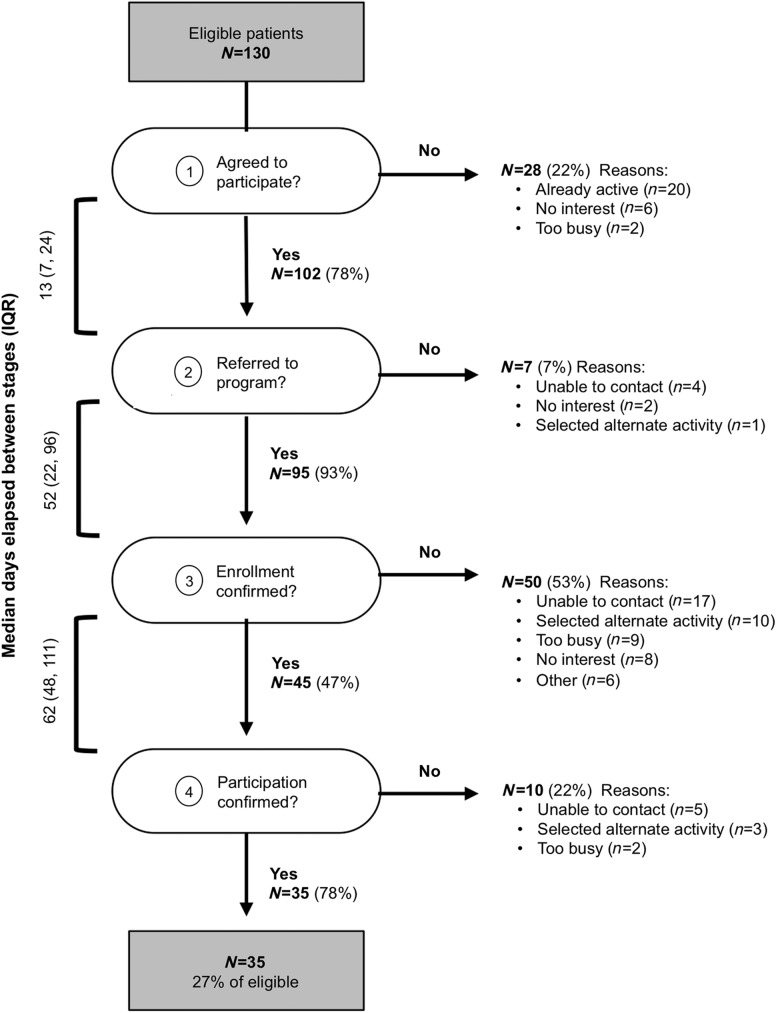
Youth were considered eligible for the PAR program if they were ages 6–18 years, resided in San Francisco, and were able to participate in physical activity. There were four steps in the referral process (Fig. 1). Step 1, recruitment: A half-time clinic coordinator screened patients and recruited eligible patients during a clinic visit; willing patients provided their activity interests. Step 2, referral: The coordinator provided patients with the contact information for activities tailored to their interests by e-mail (most commonly), US mail, or phone (least commonly). If patients expressed interest in a program that offered to contact patients, the clinic coordinator provided patient contact information to the organization (no protected health information was conveyed). Step 3, enrollment: Within 2 weeks, the coordinator contacted the patient's parent to inquire whether the patient had enrolled in a program. Step 4, participation: Within 1.5 months, the coordinator verified participation in the activity. At each step, the coordinator made at least three follow-up phone calls. The database was configured to prompt the clinic coordinator with “next steps.” For example, once the coordinator checked a box indicating the child had enrolled in a program, a “next phone call” field was populated with a date 1.5 months hence to verify the patient's participation in the program.
Figure 1.
Disposition of patients eligible for PAR program (n=130).
During the initial screening (Step 1), families reported maternal education and the number of days in a typical week that the youth exercised for at least 60 minutes. The youth's height and weight at the screening visit and race/ethnicity were extracted from the medical record. During the final phone check-in (Step 4), youth who confirmed program participation reported the frequency and duration of their physical activity sessions.
Chart reviews were conducted for all patients ages 6–18 years who were observed in the first 16 months after the clinic had implemented the PAR network. The proportion of youth who advanced through each step of the referral pathway (Fig. 1) was calculated. t-tests and chi-squared tests were used to examine differences at baseline between youth who advanced and those who did not.
Results
Of 262 youth screened, 130 were eligible (129 ineligible patients lived outside of the city and 3 had medical conditions precluding physical activity). Baseline characteristics of participants are shown in Table 1. Figure 1 illustrates the disposition of all 130 eligible youth: 102 (78%) agreed to participate in the referral process; 95 (73%) received a referral; 45 (35%) confirmed enrollment; and 35 (27%) confirmed participation in an activity. Most patients who initially declined to participate (Step 1) stated that they were already physically active (Fig. 1). The clinic coordinator called youth who agreed to participate 3.5 times, on average (maximum, 10 times), between steps and made an average of eight calls in total to youth who ended up participating (maximum, 24). Many youth could not be contacted for follow-up (Fig. 1).
Table 1.
Baseline Characteristics among Eligible Patients (n=130), by Participation Status
| Initial decision to participate in PAR (n=130) | Participation in an activity among those who initially agreed (n=102) | ||||||
|---|---|---|---|---|---|---|---|
| Characteristics | All (n=130) | Declined (n=28) | Agreed (n=102) | 95% CI for difference | Did not participate (n=67) | Participation confirmed (n=35) | 95% CI for difference |
| Age, months | 12.6±3.0 [6.4, 18.9] | 12.9±3.0 [7.7, 18.3] | 12.6±3.0 [6.4, 18.9] | [−1.0, 1.6] | 12.9±3.1 [6.5, 18.9] | 12.0±2.7 [6.4, 17.8] | [−2.1, 0.3] |
| Female, % | 45 | 39 | 46 | [−10, 19] | 40 | 57 | [−34, 3] |
| Race/ethnicity, % | |||||||
| White | 24 | 32 | 22 | [−28, 8] | 22 | 20 | [−19, 26] |
| Latino | 36 | 21 | 40 | [0, 27]* | 39 | 43 | [−23, 15] |
| Black | 18 | 14 | 20 | [−11, 23] | 19 | 20 | [−24, 23] |
| Asian | 6 | 14 | 4 | [−66, 5] | 4 | 3 | [−34, 54] |
| Other | 15 | 18 | 15 | [−25, 17] | 15 | 14 | [−25, 27] |
| Days/week ≥60 minutes of exercise | 3.6±1.9 [0, 6] | 2.9±1.7 [0, 5] | 3.8±1.9 [0, 6] | [−2.1, 0.1] | 3.7±2.1 [0, 6] | 4.1±1.5 [1, 6] | [−0.9, 1.5] |
| Mother's education, % | |||||||
| <High school | 38 | 33 | 39 | [−16, 17] | 41 | 35 | [−16, 26] |
| High school/GED | 14 | 10 | 15 | [−17, 28] | 16 | 13 | [−26, 35] |
| Some college | 23 | 19 | 24 | [−18, 21] | 23 | 26 | [−30, 22] |
| Finished college | 26 | 38 | 22 | [−37, 5] | 20 | 26 | [−34, 20] |
| BMI, kg/m2 | 33.1±6.8 [22, 55] | 32.2±7.0 [23, 48] | 33.4±6.8 [22, 55] | [−4.1, 1.7] | 33.6±6.6 [22, 55] | 32.8±7.1 [23, 55] | [−3.8, 2.2] |
| BMI z-score | 2.4±0.3 [1.4, 3.2] | 2.3±0.4 [1.6, 3.1] | 2.4±0.3 [1.4, 3.2] | [−0.3, 0.0] | 2.4±0.4 [1.4, 3.2] | 2.4±0.3[1.9, 2.9] | [−0.2, 0.1] |
Range is shown in brackets.
p<0.05.
PAR, physical activity referral; GED, General Educational Development; CI, confidence interval.
To account for potential conflicts with programs' schedules or locations, youth were referred to an average of six possible activities in which they had expressed interest (Step 2). Organizations to which youth were most frequently referred were YMCAs (17% of referrals), city recreation centers (17%), Boys & Girls Clubs (12%), city pools (7%), and fitness centers (5%). Of 45 youth who confirmed enrollment (Step 3), 22 enrolled in a swimming program; all of the swimming programs were organizations that had elected to contact youth directly, and programs were free or low cost ($8/session). Thirteen youth enrolled in a fitness center (12 at the free university-affiliated fitness center that contacted youth directly); no more than 2 youth enrolled in any other single activity. Activities in which youth ultimately participated (which took place within nine community organizations) are shown in Table 2. The 35 youth who participated in a physical activity reported attending 1.5 sessions per week, on average (range, 0.5–3.0), with sessions lasting an average of 56 minutes (range, 30–120).
Table 2.
Activities to Which Participants Were Most Frequently Referred and in Which Patients Participated
| Activity | Top referrals (%) (of 545 total referrals) | Participation (%) (n=35 patients participating)a |
|---|---|---|
| Swimming | 132 (24) | 16 (46) |
| Basketball | 70 (13) | 3 (9) |
| Dance | 56 (10) | 1 (3) |
| Soccer | 46 (8) | |
| Fitness center | 33 (6) | 10 (29) |
| Baseball | 26 (5) | 1 (3) |
| Capoeira | 22 (4) | 2 (6) |
| Martial arts | 20 (4) | |
| Volleyball | 18 (3) | |
| Biking | 12 (2) | 1 (3) |
One student enrolled in an alternate activity that was not among the top 10 activities to which youth were referred.
During initial conversations, 45 families reported barriers that could interfere with engaging in the program: 19 cited cost, 16 a lack of time in parents' and youths' schedules, 7 a need to prioritize school, and 6 a lack of transportation. (Only 52% of families in this urban setting reported having access to a car on weekdays.) The primary reason youth did not progress from one step to the next was that they could not be contacted (most phone numbers were working and the coordinator left messages, but families did not respond). Among those families contacted, the most frequently cited reasons for declining participation across Steps 2, 3, and 4 were loss of patient interest, patient identification of an alternate activity, or being too busy (Fig. 1).
Of the 95 patients who received referrals to activities, 58 (61%) were referred to at least one organization that offered to contact the patient and these youth were 5 times as likely to confirm enrollment in an activity (69% vs. 14%; p<0.001) and ultimately participate (53% vs. 11%; p<0.001) as those referred to other organizations. Latino and African American youth were more likely to initially agree to participate than white or Asian youth (Table 1). However, baseline age, sex, physical activity, weight status, and maternal education did not predict program participation in this small sample.
Discussion
This article represents an important first step in investigating the use of PARs in the clinical setting to reduce pediatric obesity. Twenty-seven percent of eligible patients observed in a pediatric obesity clinic ultimately participated in a physical activity to which they were referred. Though 27% participation is modest from a clinical perspective, increasing physical activity for 1 in 4 obese youths would be an important public health achievement. The 1.4 hours per week of exercise that youth reported doing in programs to which they were referred represents almost 25% of recommended weekly physical activity for youth, which could have an important impact on CVR.9
The 27% participation rate observed (35 of 130 eligible patients) is considerably lower than participation rates reported for PARs among adults (pooled rates of 66–81% participation).7 The lower rates of participation noted in the present study may reflect a variety of factors. First, youth may be less likely to participate in PARs than adults because they are dependent on their parents for transportation to programs and payment of program fees. This is consistent with parents reporting cost and transportation as barriers in this study and with previous research showing that logistical support from parents predicts physical activity among youth.10,11 Second, even among adults, younger age has been associated with lower rates of participation in PAR programs,7 which could reflect a greater investment in maintaining good health with increasing age. Third, obesity may have less salience as a chronic disease than other disease states. Adults referred to physical activity programs as a result of overweight or obesity were less likely to participate than those referred for other chronic conditions, such as cardiovascular disease or diabetes.12 Taken together, these findings suggest that obese youth may have lower participation rates in PARs than adults have demonstrated in previously published studies. However, it is worth noting that among patients who agreed to be referred (n=102), the participation rate was 34%.
In the present study, managing the PAR network required a half-time clinic coordinator. Achieving participation rates of 27% involved an average of eight follow-up phone calls with patients, and participating organizations changed their programming frequently, necessitating ongoing database maintenance. Further thought should be given to structuring PAR networks to ensure that they are sustainable and affordable (e.g., Could organizations be incentivized to update a central database themselves? Could the database be managed by the local health department, to allow schools and other community agencies ready access as well?).
Although PAR networks require ongoing investment, they may not need to cast a wide net to be effective. The clinic in the present study attempted to create a comprehensive database of all local physical activity opportunities, but participation was concentrated in a few activities within only nine organizations. Maintaining a smaller database and close ties to a few key programs may lead to similar success in increasing physical activity for youth, and this approach is likely more feasible for clinical practices than tracking a large number of organizations. Additionally, a key finding was that youth referred to organizations that contacted families were 5 times more likely to enroll and participate than youth referred to other organizations. Partnering with organizations willing to do outreach can decrease the follow-up efforts required of clinical practices conducting PAR programs.
Demographic characteristics may predict participation in PAR programs, though little research exists in this area. Although, in the present study, Latino families were more likely to participate than white families, one study examining ethnicity among adults did not find it predictive of participation.13 Larger studies might be able to identify predictors of participation among children. Notably, though demographically diverse, the youth in the present study were uniformly severely obese, which may have hampered physical activity. Further studies should explore participation rates among sedentary youth without severe obesity.
Whereas the present study suggests that PARs could increase physical activity for some youth, the effects of PARs on BMI have proven minimal among adults.14–17 Further work examining PARs in youth should objectively assess impact on BMI, physical activity levels, and cardiorespiratory fitness, which the present feasibility study was not constructed to do. The cost-effectiveness of PAR networks will depend on their success in reducing CVR and improving quality of life and/or productivity.
Additional limitations merit comment. It is not possible to attribute causality without a control group. All results were self-reported; patient participation was not verified with organizations and may be overestimated. Conversely, many patients could not be contacted and it was assumed they had not participated, which could underestimate participation. There was no verification that agencies contacted patients (when they had agreed to do so) nor was duration of the physical activity programs ascertained. Importantly, activity costs and distance from the patient were not carefully tracked, but could be associated with program participation.
Conclusion
The Institute of Medicine calls for a systems-based approach to addressing obesity, highlighting the interdependent factors that underlie the obesity epidemic and the need to build healthy bridges between environments.18 In multiple studies, healthcare providers cite a lack of referral opportunities as one of the top three barriers to addressing obesity.3–5 PARs could bridge the gap between healthcare and community. Whereas further experimental studies should examine the health impacts of PARs, the present findings suggest that, as an initial step, healthcare providers can identify organizations that are willing to do outreach to families to begin the process of linking sedentary youth to community activities.
Acknowledgment
This work was supported by the National Institutes of Health/National Institute of Child Health and Human Development (K23HD054470).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Goodpaster BH, Delany JP, Otto AD, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: A randomized trial. JAMA 2010;304:1795–1802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kraus WE, Houmard JA, Duscha BD, et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med 2002;347:1483–1492 [DOI] [PubMed] [Google Scholar]
- 3.Boyle M, Lawrence S, Schwarte L, et al. Health care providers' perceived role in changing environments to promote healthy eating and physical activity: Baseline findings from health care providers participating in the Healthy Eating, Active Communities program. Pediatrics 2009;123:S293–S300 [DOI] [PubMed] [Google Scholar]
- 4.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: Attitudes, barriers, skills, and training needs among health care professionals. Pediatrics 2002;110:210–214 [PubMed] [Google Scholar]
- 5.He M, Piché L, Clarson CL, et al. Childhood overweight and obesity management: A national perspective of primary health care providers' views, practices, perceived barriers and needs. Paediatr Child Health 2010;15:419–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pavey TG, Anokye N, Taylor AH, et al. The clinical effectiveness and cost-effectiveness of exercise referral schemes: A systematic review and economic evaluation. Health Technol Assess 2011;15:i–xii, 1–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pavey T, Taylor A, Hillsdon M, et al. Levels and predictors of exercise referral scheme uptake and adherence: A systematic review. J Epidemiol Community Health 2012;66:737–744 [DOI] [PubMed] [Google Scholar]
- 8.Madsen KA, Garber AK, Mietus-Snyder ML, et al. A clinic-based lifestyle intervention for pediatric obesity: Efficacy and behavioral and biochemical predictors of response. J Pediatr Endocrinol Metab 2009;22:805–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Physical Activity Guidelines Advisory Committee. 2008 Physical Activity Guidelines for Americans. US Department of Health and Human Services: Washington, DC, 2008 [Google Scholar]
- 10.Jago R, Davison KK, Brockman R, et al. Parenting styles, parenting practices, and physical activity in 10- to 11-year olds. Prev Med 2011;52:44–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raudsepp L. The relationship between socio-economic status, parental support and adolescent physical activity. Acta Paediatr 2006;95:93–98 [DOI] [PubMed] [Google Scholar]
- 12.James DVB, Johnston LH, Crone D, et al. Factors associated with physical activity referral uptake and participation. J Sports Sci 2008;26:217–224 [DOI] [PubMed] [Google Scholar]
- 13.Damush TM, Stump TE, Saporito A, et al. Predictors of older primary care patients' participation in a submaximal exercise test and a supervised, low-impact exercise class. Prev Med 2001;33:485–494 [DOI] [PubMed] [Google Scholar]
- 14.Isaacs AJ, Critchley JA, Tai SS, et al. Exercise Evaluation Randomised Trial (EXERT): A randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only. Health Technol Assess 2007;11:1–165, iii–iv. [DOI] [PubMed] [Google Scholar]
- 15.Sørensen JB, Kragstrup J, Kjær K, et al. Exercise on prescription: Trial protocol and evaluation of outcomes. BMC Health Serv Res 2007;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor AH, Doust J, Webborn N. Randomised controlled trial to examine the effects of a GP exercise referral programme in Hailsham, East Sussex, on modifiable coronary heart disease risk factors. J Epidemiol Community Health 1998;52:595–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gusi N, Reyes MC, Gonzalez-Guerrero JL, et al. Cost-utility of a walking programme for moderately depressed, obese, or overweight elderly women in primary care: A randomised controlled trial. BMC Public Health 2008;8:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Committee on Accelerating Progress in Obesity Prevention; Food and Nutrition Board, Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. The National Academies Press: Washington, DC, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]