INTRODUCTION
Chronic pilonidal disease is a common surgical condition. The Office of Population Censuses and Surveys (OPCS 4) indicated that in England there are over 4,500 operations performed per year as inpatients, with many more being operated on in emergency departments or general practice.1 The condition is primarily seen in young males who are afflicted twice as often as women. It is rare prior to puberty or over the age of 40.
The literature on the management of pilonidal sepsis is complex to analyse because many series include patients presenting with a primary abscess as well as those undergoing their first elective operation for the condition. There is, furthermore, very little data on what to do when these operations fail, as they do in about 10% of cases.2, 3
This study examines one surgeon's outcomes when surgery is performed for patients who have recurrent or persistent pilonidal sepsis despite having had an elective definitive procedure for the condition. This does not include those patients who have had a single operation for acute pilonidal abscess and are returning for a definitive elective procedure.
PATIENTS AND METHODS
All patients with refractory pilonidal sepsis who were referred to a single surgeon between 2000 and 2010 were studied. Suitable patients were identified from a prospectively collected database, as well as being checked against theatre logs and discharge letters. The clinical notes were examined and relevant information extracted.
The case notes were reviewed to determine the nature and number of previous operations, the duration of disease and the source of referral. Following referral we reviewed the surgical management, the outcomes of definitive surgery for recurrent pilonidal sepsis and any interventions required to achieve this outcome.
Patients were excluded if we could not identify the specific nature of previous interventions or if they had undergone only drainage of an abscess, even if this was regarded as the definitive treatment. Patients were also excluded if follow-up was incomplete.
The primary aim of the study was to assess the healing rate for operations performed for recurrent pilonidal sepsis.
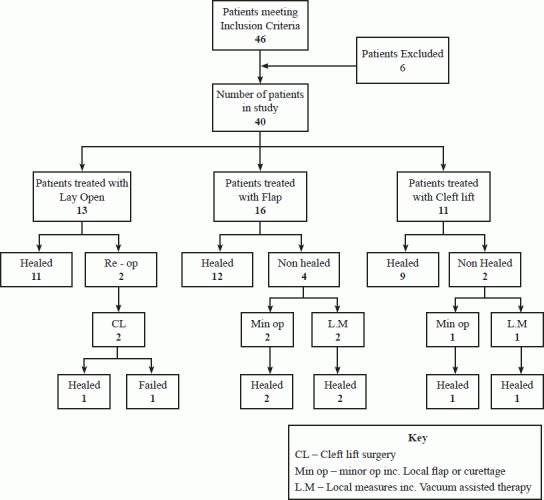
Forty-six patients met the inclusion criteria. Four were excluded because of inadequate follow-up and two because the nature of the original surgical intervention could not be determined, leaving a total of 40 patients in the study.
Twenty-nine of these patients were male. The duration of the unhealed wound or persistent sepsis at the time of referral was recorded in 33 of the 40 patients and ranged from 11 months to 10 years with a median of 3.5 years.
The number of previous surgical procedures ranged from 1 – 10 with a median of 2.1. These included a simple lay open, primary midline closure and flap procedures.
Patients were referred from a variety of sources. Fifty-four per cent came from general practitioners, 10% from Accident & Emergency Departments and 36% from other surgical consultants.
Of the 40 patients, 13 (33%) underwent a simple lay open procedure, 16 (40%) had a local flap procedure and the remaining 11 (27%) underwent a cleft lift procedure.
RESULTS
In the 13 patients who underwent a simple lay open procedure, 11 (83.6%) healed without further surgical intervention. In all cases the sinus laid open was oblique and did not involve the mid-line in the internatal cleft.
Two of these 13 patients (15.4%) had persistently unhealed wounds. One of these underwent a cleft lift procedure one year later with successful healing. The second patient underwent two further flap procedures, both of which failed to secure primary healing, this patient subsequently refused vacuum-assisted closure therapy and is currently waiting for further surgery.
Sixteen patients (42.1%) underwent flap procedures as their definitive operation. These included nine Limberg flaps, six Karydakis procedures and one Z-plasty. Twelve patients (75%) had primary healing without further surgical intervention. Two patients required minimal intervention to secure healing, one having a vacuum-assisted closure and the other curettage of some excess granulation tissue. In both cases healing by secondary intention occurred within a few weeks. Two wounds (6.5%) failed to heal completely and further small local flap procedures were performed with a plastic surgeon. Both of these wounds healed following these procedures. There have been no recurrences in this group.
Fig 1.
Outcomes in the patients referred
In eleven patients a cleft lift procedure was performed. Of these, nine (82%) healed by primary intention. Two (18%) required further surgical input. In both cases this was a small local flap. One of these healed without further complications. In the other patient the wound broke down due to extremely poor anal hygiene. This was managed with vacuum-assisted closure and the wound ultimately healed by secondary intention.
DISCUSSION
Chronic pilonidal disease is often regarded by surgeons as relatively trivial, but it causes prolonged and troublesome sepsis for a group of patients who are young and physically active. A Cochrane review analysed recurrence rates from 16 studies. The recurrence rate, regardless of surgical technique, for a total of 1,666 operations, was 7%. The recurrence rate for primary closure with an incision off the midline was 1.7% as compared with closure on the midline of 10.5%. Recurrence for simple lay open was 5.3%.4
Pilonidal disease can cause significant disability and prolonged loss of time from education, sport and social activity for young people. We agree with the consensus view in the literature that laying open a pilonidal sinus in the internatal cleft is a poor option, despite traditional teaching that this is the standard approach.
Those techniques associated with better results aim to achieve a scar off the midline and or flattening of the internatal cleft. These include the Karydakis procedure, Limberg flap, and Z-plasty. A large series of 141 patients undergoing a Karydakis procedure for primary pilonidal sepsis, with long term follow up, demonstrated a recurrence rate of 4%.5
A randomised trial comparing primary midline closure and Limberg flap showed no recurrences in the Limberg flap group after a median review of 28 months, whereas midline closure recurrence rates were 11%. Wound complication rates of 3% for the Limberg flap group compared to 9% in a midline closure group.6
All of these previous studies have addressed the problem of managing pilonidal disease in the elective setting but have not looked specifically at those patients who have already had one or more failed procedures.
Cleft lift not only takes the scar off the midline but also alters the anatomical shape of the internatal cleft in a manner not dissimilar from Karydakis procedures. This technique has been primarily used where there has been failure of previous surgery leaving an open midline wound with unhealthy granulations.
In this study the patient population is entirely made up of those who have had a previous attempt at definitive surgical treatment of pilonidal disease and whose wound has failed to heal. In most instances there was a long and deep midline wound with unhealthy granulations. Patients in this series had undergone a median of two and a maximum of ten previous procedures.
Our philosophy is based on a simple algorithm. Some patients had relatively simple recurrent disease, often because all tracts had not been adequately identified and laid open. If the sepsis was in the upper, flatter part of the internatal cleft (and the cleft was not deep) a further lay open procedure was performed. We would not perform this procedure in patients where the wound lay in a deep internatal cleft. It is interesting that we were able to achieve healing by secondary intention relatively easily in 84% of patients who underwent this simple procedure, even though they had recurrent disease. However, as experience of Karydakis and Cleft lift procedures has grown, lay open is now rarely used.
For those patients with a wound in the depths of an internatal cleft, a lay open procedure was unlikely to succeed. A variety of flap procedures were therefore used and these were designed according to the appearance at operation and after careful discussion with the patient.
The Karydakis procedure is useful when the sepsis is well localised, as it is simple to perform and gives good cosmesis. Cleft lift is appropriate where there is a long unhealed wound in the depths of the inter-natal cleft, and gives reasonable cosmesis. We feel that Z-plasty and Limberg flaps are appropriate when neither of the above procedures is feasible.
Sixteen patients underwent mobilisation of a flap in the form of a Limberg or Karydakis flap, with one Z-plasty. Primary healing was achieved in three quarters of these with a further two patients having healing after a period of wound dressings. Ultimately, only two of the 16 patients had unhealed wounds requiring further procedures and a small local flap was sufficient to achieve healing with no recurrence.
Eleven patients were selected for cleft closure procedure because there was a very deep internatal cleft with an unhealthy wound in the depths of it. Healing was achieved in all of these patients though in two further local flap procedures were necessary, one of which broke down and required prolonged vacuum-assisted closure dressings.
When pilonidal surgery fails to achieve healing, referral to a surgeon with an interest is recommended. Careful selection of the operative strategy is required, rather than repeating previously failed procedures with the resultant additional scarring and tissue loss that makes definitive surgery more complex.
Acknowledgments
The author has no conflict of interest.
References
- 1.Faiz OD, Brown TJ, Colucci G, Grover M, Clark SK. Trends in colorectal day case surgery in NHS Trusts between 1998 and 2005. Colorectal Dis. 2008;10(9):935–42. doi: 10.1111/j.1463-1318.2008.01481.x. [DOI] [PubMed] [Google Scholar]
- 2.Bascom J, Bascom T. Failed pilonidal surgery: new paradigm and new operation leading to cures. Arch Surg. 2002;137(10):1146–50. doi: 10.1001/archsurg.137.10.1146. [DOI] [PubMed] [Google Scholar]
- 3.Senapati A, Cripps NP, Flashman K, Thompson MR. Cleft closure for the treatment of pilonidal sinus disease. Colorectal Dis. 2011;13(3):333–6. doi: 10.1111/j.1463-1318.2009.02148.x. [DOI] [PubMed] [Google Scholar]
- 4.Al-Khamis A, McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2010;20(1) doi: 10.1002/14651858.CD006213.pub3. CD006213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1996;83(10):1452–5. doi: 10.1002/bjs.1800831040. [DOI] [PubMed] [Google Scholar]
- 6.Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg. 2005;92(9):1081–4. doi: 10.1002/bjs.5074. [DOI] [PubMed] [Google Scholar]


