Editor,
Antiphospholipid antibody syndrome (APS) is traditionally characterized by the presence of circulating antiphospholipid antibodies (aPL) that lead to an increased risk of thrombosis and pregnancy morbidity.1, 2 Considered rare, diffuse alveolar hemorrhage (DAH) is thought to be a non-thrombotic manifestation of APS, likely secondary to aPL induced pulmonary capillaritis.3 The diagnosis needs to be considered even in the absence of known thrombosis, as multiple recent case reports have identified DAH as the presenting symptom.4
CASE
A 35-year-old mother of four from El Salvador presented with a two day history of pronounced dyspnea and hemoptysis. Two years prior she had been diagnosed with adult-onset epilepsy and had undergone mitral valve replacement (MVR) for severe presumed rheumatic mitral stenosis. Pathologic evaluation of the resected valve revealed leaflet fibrosis with Libman-Sacks endocarditis. There was no previous history of thrombosis or pregnancy loss. She was afebrile and was able to speak in full sentences with a SpO2 of 92% on room air. Inspiratory crackles were auscultated bilaterally. No systemic findings of a connective tissue disease were present. CXR demonstrated extensive bilateral air space disease. Computed tomography of the chest identified bilateral groundglass opacities (Figure 1). Fiberoptic bronchoscopy demonstrated no endobronchial source of bleeding. Sequential bronchoalveolar lavage aliquots became progressively more hemorrhagic with microscopic evidence of hemosiderin-laden macrophages, suggesting diffuse alveolar hemorrhage (Figure 2). Laboratory investigations revealed the presence of a non-specific inhibitor, positive anti-cardiolipin IgG antibody, positive anti-dsDNA antibody, and serum thrombocytopenia and lymphopenia. Workup was negative for ANCA or anti-GBM related disease. A probable diagnosis of APS with suspected underlying systemic lupus erythematosus (SLE) was made. The patient underwent induction therapy with pulse-dose corticosteroids and IV cyclophosphamide with rapid clinical and radiographic improvement.
Figure 1.
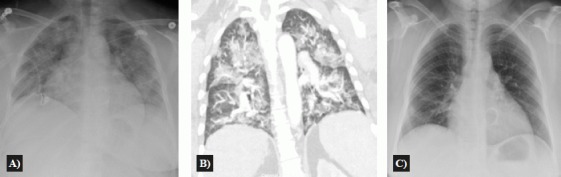
CXR completed at time of presentation reveals bilateral airspace disease (a). Coronal CT chest images completed at the same time reveal bilateral, predominantly central, heterogeneous groundglass opacities, involving both upper and lower zones with subpleural sparing (b). These opacities quickly resolved upon treatment with high-dose corticosteroids and IV cyclophosphamide (c).
Figure 2.

First (left) and second (right) sequential aliquots obtained from bronchoalveolar lavage. Serial returns are progressively hemorrhagic.
DISCUSSION
APS mediated capillaritis represents a rare cause of DAH.4 Although APS is traditionally defined by strict diagnostic criteria, recent literature supports the pathogenic role of APS in many non-thrombotic disease states.5 Non-criteria manifestations of APL include livedo reticularis, cardiac valve disease, thrombocytopenia, non-thrombotic neurologic manifestations, and nephropathy. Given our patient's thrombocytopenia, recently diagnosed seizure disorder, and positive aPL on two occasions, a diagnosis of probable APS was made. Her valvular disease was not considered diagnostic, as while APS is a known cause of Libman-Sacks endocarditis, it typically causes regurgitant mitral valve lesions rather than stenosis, consistent with the previous diagnosis of rheumatic heart disease.
APS may occur as an independent disease entity – primary APS – or in the setting of an underlying disease, usually SLE. In our patient, comorbid SLE is suspected given the presence of anti-dsDNA antibodies, lymphopenia, and recurrent idiopathic seizure.
Given the morbidity of DAH, the high-risk of recurrence, and the suspected underlying SLE, the patient has been managed with cyclophosphamide and hydroxychloroquine. Her inflammatory markers have normalized and she has had no subsequent disease flare.
Conclusion: DAH can be the presenting manifestation of APS in the absence of traditional manifestations such as venous/arterial thrombosis or pregnancy morbidity.
Acknowledgments
Authors have no conflict of interest.
References
- 1.Wilson WA, Gharavi AE, Koike T, Lockshin MD, Branch DW, Piette JC, et al. International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an international workshop. Arthritis Rheum. 1999;42(7):1309–11. doi: 10.1002/1529-0131(199907)42:7<1309::AID-ANR1>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 2.Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS) J Thromb Haemost. 2006;4(2):295–306. doi: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 3.Deane KD, West SG. Antiphospholipid antibodies as a cause of pulmonary capillaritis and diffuse alveolar hemorrhage: a case series and literature review. Semin Arthritis Rheum. 2005;35(3):154–65. doi: 10.1016/j.semarthrit.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Koolaee RM, Moran AM, Shahane A. Diffuse alveolar hemorrhage and Libman-Sacks endocarditis as a manifestation of possible primary antiphospholipid syndrome. J Clin Rheumatol. 2013;19(2):79–83. doi: 10.1097/RHU.0b013e318278c577. [DOI] [PubMed] [Google Scholar]
- 5.Cartin-Ceba R, Peikert T, Ashrani A, Keogh K, Wylam ME, Ytterberg S, et al. Primary antiphospholipid syndromeassociated diffuse alveolar hemorrhage. Arthritis Care Res. doi: 10.1002/acr.22109. 2013 Aug 27. doi: 10.1002/acr.22109. [DOI] [PubMed] [Google Scholar]
- 6.Erkan D, Lockshin MD. Non-criteria manifestations of antiphopholipid syndrome. Lupus. 2010;19(4):424–7. doi: 10.1177/0961203309360545. [DOI] [PubMed] [Google Scholar]


