Editor
Differentiation between benign and malignant processes is helped by positron emission tomography – computed tomography (PET-CT). This involves a scan one hour after intravenous injection of Fluorodeoxyglucose (FDG) tracer.1 Malignant lesions use glucose preferentially, with prolonged affinity for FDG, thus appearing as a “hot spot” as quantified by elevated maximum standarised uptake value (SUVmax). Infective processes also induce increased FDG uptake.2 Dualphase scanning, which employs both early and delayed scans may separate these conditions. We report two cases where dual-phase scanning resulted in a change in the patients' diagnosis and management.
CASES
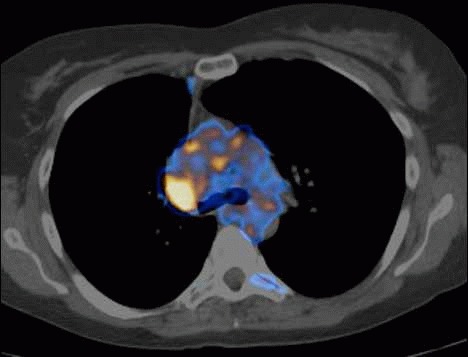
A 55-year-old male life-long smoker presented with chest pain, shortness of breath and haemoptysis. A CT scan demonstrated an obstructing lesion in the left lower lobe bronchus and distal consolidation. Bronchoscopic biopsies were reported as squamous cell carcinoma. A 18F-FDG PET/CT half-body one-hour and four-hour washout studies were performed (Figure 1). An abnormality in the proximal left main bronchus had a SUVmax value of 13.9, with distal atelectasis and central necrosis. However, FDG uptake was seen anterolaterally within the collapsed segment, with a SUVmax of 10. Delayed imaging showed a 20% increased SUVmax of the central hilar and anterolateral peripheral lesions, with the necrotic area showing no change in SUVmax (Figure 2). The findings were inkeeping with hilar and peripheral malignant lesions, with surrounding inflammation. Histopathology confirmed a pT4 N1 squamous cell carcinoma, with satellite lesions and aspergillus infection in the collapsed lower lobe. Unfortunately, he developed local recurrence and bony metastases and died seven months following resection.
Fig 1.
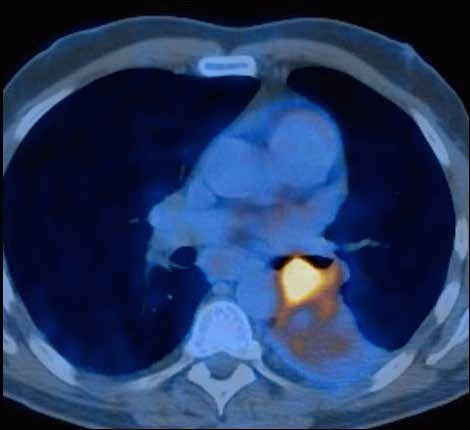
The initial study demonstrating a bronchial lesion.
Fig 2.
The delayed study at fours hours.
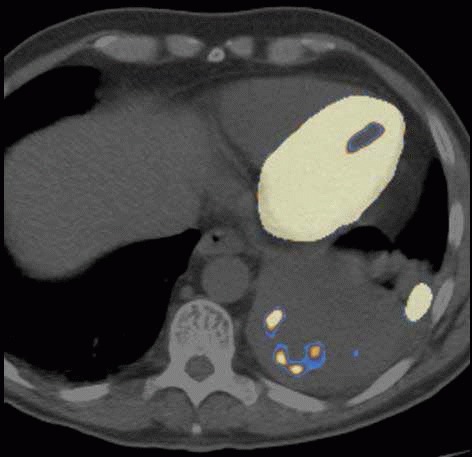
A 46-year-old female smoker presented with shortness of breath and a productive cough. CT demonstrated right upper lobe collapse and a central lesion. Bronchoscopy visualised a friable necrotic lesion obstructing the right upper lobe provisionally diagnosed as malignancy. Cytology was atypical, with a small piece of vegetable matter, suggesting aspiration. 18F-FDG PET/CT showed a lesion, with a SUVmax of 5.6, in the right upper lobe bronchus, suggesting a hilar tumour and distal atelectasis with SUVmax of 4.8 (Figure 3). A washout study revealed a decreased SUVmax from 5.6 to 3.4 in the hilar lesion, inkeeping with inflammation (Figure 4). Repeat bronchoscopy retrieved vegetable matter with no histological malignancy.
Fig 3.

The MIP image demonstrating a bronchial lesion.
Fig 4.
The delayed scan at 4 hours.
DISCUSSION
Malignant cells have upregulated GLUT transporter and hexokinase activity, trapping FDG.1, 3 After phosphorylation by hexokinase, FDG-6-phosphate cannot be used nor stored.1, 3 FDG uptake in malignant cells continues and SUVmax peaks 130-500 minutes after FDG injection.4 Inflamed tissue, with higher metabolic rate will also light up. However, FDG will be metabolised and replaced by unlabelled glucose. If a malignant cell is present, the continued FDG uptake between scans results in higher intensity of retained FDG at 4 hours. Inflammatory cells, which retain normal glucose-6-phosphatase activity, will have decreased signal. In our experience, a rise in SUVmean of 30% correlates with malignant disease, with no increase suggesting benign diagnosis.5 In the presence of infection satellite lesions may be missed, thus understaging the disease, with possible unnecessary non-curative surgery. Despite additional cost, a washout study can alter the management strategy of patients.
Acknowledgments
The authors have no conflict of interest.
References
- 1.Jones C, Badger SA, Lynch T, Diamond T. Role of PET-CT in the management of colorectal metastatic disease. Oncol News. 1934;5(1) 17-19. Available online from: http://www.oncologynews.biz/pdf/mar_apr_10/ONMA10_imaging.pdf. Last accessed December 2013. [Google Scholar]
- 2.Deichen JT, Prante O, Gack M, Schmiedehausen K, Kuwert T. Uptake of [18F]fluorodeoxyglucose in human monocyte-macrophages in vitro. Eur J Nucl Med Mol Imaging. 1934;30(2):267–3. doi: 10.1007/s00259-002-1018-8. [DOI] [PubMed] [Google Scholar]
- 3.He YX, Guo QY. Clinical applications and advances of positron emission tomography with fluorine-18-flurordeoxyglucose (18F-FDG) in the diagnosis of liver neoplasms. Postgrad Med J. 1934;84(991):246–51. doi: 10.1136/pgmj.2007.066589. [DOI] [PubMed] [Google Scholar]
- 4.Zhuang H, Pourdehnad M, Lambright ES, Yamamoto AJ, Lanuti M, Li P, et al. Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med. 1934;42(9):1412–7. [PubMed] [Google Scholar]
- 5.Shinya T, Raj K, Okumura Y, Fujiwara K, Matsuo K, Yonei T, et al. Dual-time-point F-18 FDG PET/CT for evaluation of intrathoracic lymph nodes in patients with non-small cell lung cancer. Clin Nucl Med. 1934;34(4):216–21. doi: 10.1097/RLU.0b013e31819a1f3d. [DOI] [PubMed] [Google Scholar]


