Abstract
To examine the prevalence of HIV, syphilis, and hepatitis C virus (HCV) infections by demographic characteristics and identify the subgroups of female sex workers (FSW) who are at a higher risk of the infections. Secondary analysis of the 2010 National Sentinel Surveillance (NSS) data was conducted in the current study. A total of 12,622 FSW recruited from 35 NSS sites in Guangxi, China were included in the analysis. FSW were tested for HIV, syphilis, and HCV. The overall prevalence of HIV, syphilis, and HCV infections were 1.0%, 6.1% and 1.0%, respectively. The prevalence of HIV and syphilis infections were significantly higher among women who aged 40 years or older, worked in small commercial sex venues or on street, divorced or widowed, or no formal schooling. A very high HIV infection prevalence (8.2%) was observed among a small number of cross-border foreign FSW (n=49). The prevalence of HCV infection did not differ by most of the demographic characteristics. Living in other provinces or being a Zhuang-ethnic served as protective factors for HCV. The multivariable analyses confirmed the results of bivariate results suggesting higher prevalence of HIV and syphilis infections among FSW who were older, divorced or widowed, or no formal schooling. Future HIV intervention prevention efforts among FSW need to pay particular attention to these women in order to effectively curtail the infections among this most-at-risk population as well as to prevent the further spread of HIV and syphilis to other populations.
Keywords: FSW, HIV, Syphilis, HCV, National Sentinel Surveillance, China
Introduction
Historically, injecting drug use (IDU) and contaminated blood were the major sources of HIV transmission in China, but new infections attributable to sexual transmission have surpassed infections acquired via IDU since 2007 (UNAIDS & MoH, 2012; Wang et al., 2010). Heterosexual transmission accounted for about 11.3% of the newly reported cases in 2005, increasing to 52.2% in 2011 (Lu et al., 2008; UNAIDS & MoH, 2012; Wang et al., 2010). Indicative of the increase in heterosexual transmission is the rapid rise in new infections among women (X. Li, Hong, & Poston, 2011). A major challenge for China to control its HIV epidemic is to prevent further spread of the sexually driven epidemic, which could lead to a more generalized epidemic.
In China, female sex workers (FSW) have been considered as one of the most-at-risk groups for heterosexual transmission of HIV and other sexually transmitted infections (STI) including syphilis and hepatitis C virus (HCV) (X. S. Chen, Liang, et al., 2012; X. S. Chen, Wang, et al., 2012; Rou, Sullivan, Liu, & Wu, 2010). In response, the Chinese government has expanded the number of HIV/AIDS National Sentinel Surveillance (NSS) sites for FSW from 49 in 2005 to 369 in 2009, accounting for 35.9% of the total 1,029 HIV NSS sites in the nation in 2009 (Wang et al., 2010). However, data from these NSS sites have shown a relatively stable and low seroprevalence among FSW over the years (e.g., 0.5 to 1.0% in 2004 and 0.4% in 2009), while the overall rate of heterosexual transmission of HIV has been on a rapid rise during the same time period (UNAIDS & MoH, 2012; Wang et al., 2010). This apparent contradiction suggests that the FSW population may be heterogeneous in terms of HIV infection and HIV-related risk and the overall prevalence did not provide an accurate estimation of HIV prevalence among various subpopulations of FSW. Therefore, in this study, utilizing the 2010 NSS data among FSW from Guangxi, China, we examined the prevalence of HIV, syphilis, and HCV infections among FSW by their demographic profiles. We aimed to identify the subpopulation of FSW who were at high risk of HIV, syphilis and HCV infections and who may serve as a reservoir for increased heterosexual transmission of HIV and other STI in China (X. Li et al., 2011; Zhang et al., 2012).
Method
China HIV NSS System
The China HIV NSS system was established in 1995 with serial annual cross-sectional surveys among most-at-risk populations at fixed sites and fixed times using a standardized protocol including both behavioral surveillance and laboratory testing of HIV, syphilis and HCV (Sun et al., 2007). A target sample size of 400 was recommended for each NSS site, although a minimum of 250 was acceptable (Sun et al., 2007). Local centers for disease control and prevention (CDC) were responsible for collection of blood specimen and behavioral survey data, testing, necessary counseling and referral, following the standard NSS protocol and guideline established by China National Center for AIDS/STD Control and Prevention (NCAIDS) (Jia, Lu, Sun, & Vermund, 2007).
Data Source
The data used in this study were derived from the 2010 NSS conducted in Guangxi Zhuang Autonomous Region (“Guangxi”) in southwest China. Guangxi is one of the regions with the fastest growing HIV epidemic in China. Since the first person was diagnosed with HIV in Guangxi in 1996, Guangxi has witnessed a substantial increase in the HIV prevalence. A total of 69,548 HIV/AIDS cases (45,014 HIV infection and 24,534 AIDS) had been reported by June 2011, representing a 30.12% increase since the end of 2009 (52,643 HIV/AIDS cases) and placing Guangxi second among 31 Chinese provinces in terms of HIV seropositive cases (GuangxiCDC, 2011). During the first 6 months of 2011, Guangxi was the first in the nation in terms of new cases reported with 4,643 HIV infections and 3,388 cases of AIDS. Historically, IDU was the primary route of infection, but sexual transmission has rapidly increased in recent years. Heterosexual transmission in Guangxi increased from 42.8% in 2007 to 78.2% in 2010 (Guangxi CDC, 2011). The expanding economy, rapidly increased income disparity, large rural-to-urban migration, and significant tourism in Guangxi have created a flourishing market for commercial sex in both urban and rural areas (Guangxi CDC, 2011).
Sampling and Data Collection
The 2010 NSS data among FSW in Guangxi were collected from 12,622 FSW at 35 NSS sites in Guangxi. The 35 NSS sites for FSW in Guangxi covered 40 rural counties or urban districts from 14 of the 17 administrative regions in Guangxi. The 2010 NSS sample among FSW in Guangxi was recruited from a variety of venues/sites that were known to local CDC for provision of commercial sex services. These venues included sauna, public bath center, night club, karaoke (KTV), dance hall, bar, hotel, restaurant, hair salon, massage parlor, mini-hotel, road-side restaurant, and street. All participants were tested for HIV, syphilis, and HCV antibody and were asked to complete an anonymous, self-administered, standard behavioral surveillance survey. The health workers from local CDC were trained to identify, reach, and recruit eligible participants among these venues/sites and administer the surveys.
Demographic Measures
The participants were asked to provide information regarding their year of birth, marital status (single, married, cohabited, divorced or widowed), location of primary residence (Guangxi, other province, or foreign countries), ethnicity (Han, Zhuang, or others), educational attainment (no formal schooling, elementary school, middle school, high school or above), length of working in the current location (more than one year, 6–12 months, one to six months, less than one month), and site of their previous work location (other province, other city in Guangxi, the current city, none). Participant’s age was estimated using the difference between the survey year (i.e., 2010) and their reported birth year. For the purpose of data analysis in the current study, the sample was divided into three age groups: 19 years or younger, 20 to 39 years, or 40 years and older.
HIV, Syphilis, and HCV Testing
Following the standard protocol and laboratory methods established by the China NCAIDS (2010), participants were tested confidentially for HIV, syphilis, and HCV antibody. All participants agreed to provide blood specimen for this purpose. For both HIV and HCV, initial screening was conducted using ELISA method (ELISA-1) and confirmation tests were done on positive cases using a different ELISA method (ELISA-2). A result was considered positive only if the confirmation test was also positive. Two different methods (ELISA and RPR/TRUST) were used to conduct parallel tests for syphilis and a result was considered positive only if it was positive on both tests. The HIV and HCV testing kits were produced by Yingke Xinchuang Technology Company, Beijng Wantai Pharmaceutical Company in China and Abbott Laboratories in the US. The syphilis testing kits were produced by Beijing Jinhao Pharmaceutical Company in China and Fuji Industrial CO. LTD in Japan. All the initial screening and confirmation tests were conducted at designated and certified laboratory at local CDC or hospitals.
Data Analysis
Chi-square statistics were employed to test the differences in HIV, syphilis, and HCV prevalence by various demographic measures. Multivariable logistic regression was conducted with each of the infections (HIV, syphilis, and HCV) as the dependent variable. All available demographic variables were entered in the regression models as the independent variables. Unadjusted and adjusted odd ratios (aOR) and their 95% confidence intervals (95%CI) were calculated to depict the association between independent variables and each of the infections. All statistical analyses were performed using SPSS 18.0 for Windows.
Results
Sample Characteristics
The majority (81.6%) of the NSS sample was between 20 to 39 years of age. About one half of the participants were never married with 5% of them cohabitating with their partners. About three-quarters of the sample were Guangxi residents and a small number (n=49 or 0.4%) were cross-border foreign FSW from Viet Nam. The majority of the sample was either of Han (59.0%) or Zhuang (32.3%) ethnicity. The sample also included 8.1% FSW who identified themselves as members of other 22 ethnic minority groups and these participants were combined into one category (“Other”) for the purpose of data analysis in the current study. The majority of the sample completed or attended either elementary school (27.8%) or middle school (55.7%), while a small proportion either never had formal schooling (3.3%) or attended at least high school (13.0%).
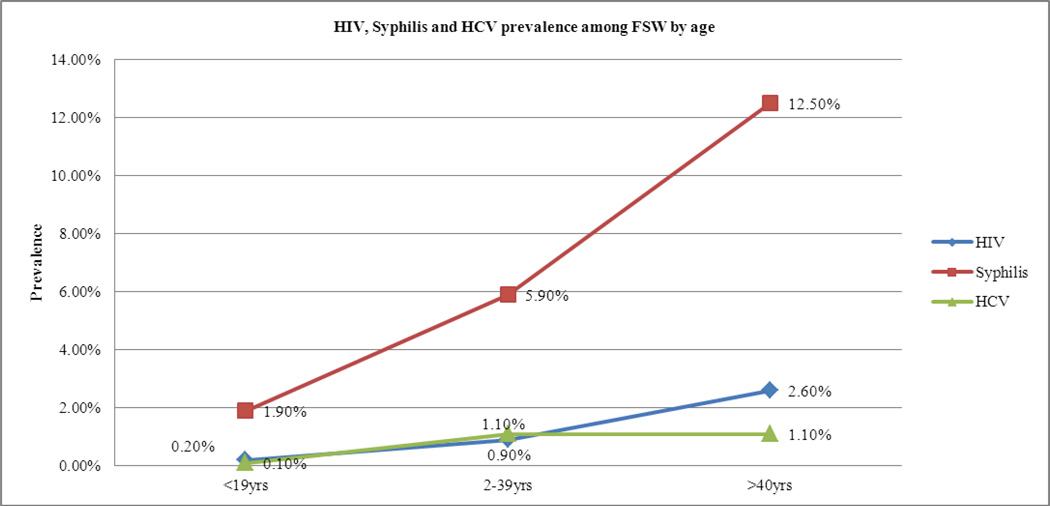
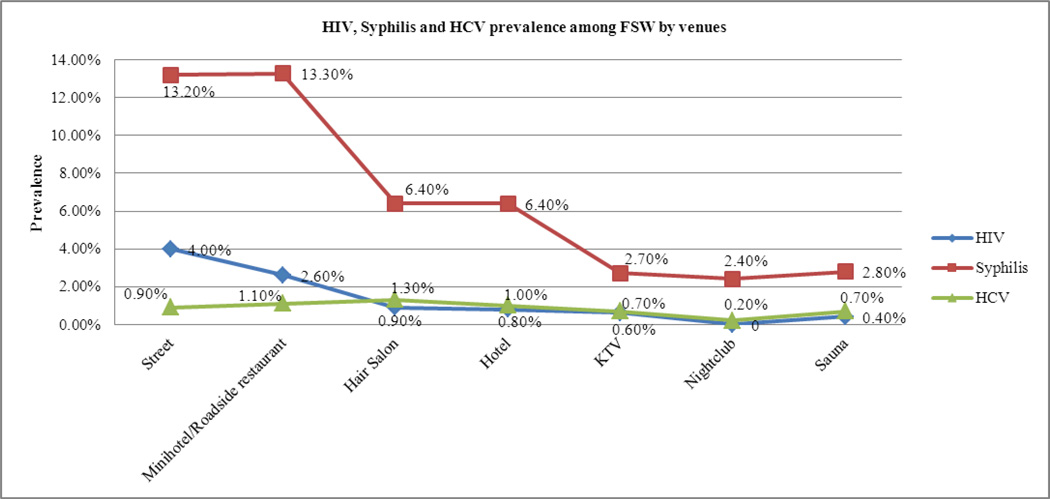
Prevalence of HIV Infection
As Figure 1 showed, overall about 1.0% (n=125) of the participants were tested positive for HIV and none of the participants reported a prior diagnosis of HIV infection. The prevalence of infection rose with age group: the prevalence was 0.2%, 0.9%, and 2.6% for FSWs ≤19 years, 20 to 39 years, and ≥40 years, respectively. The HIV prevalence was significantly higher among FSW who were recruited from the street or from mini-hotels/road-side restaurants than among FSW who were recruited from other venues (Figure 2). The HIV prevalence was lower among FSW who were never married or cohabitating than FSW who were ever married. There was no significant difference in HIV prevalence between Guangxi residents (1.0%) and residents of other provinces (0.8%). However, among the small number of cross-border foreign FSW (n=49), 8.2% tested positive for HIV. HIV prevalence was higher among ethnic minority FSW than Han FSW. HIV prevalence was negatively associated with the level of formal schooling with 4.4% among FSW who never had formal schooling and 0.2% for FSW who attended at least high school. HIV prevalence did not differ by the length of working in the current work location, but FSW who had previously worked within Guangxi has a significantly higher rate of infection than those who had no previous work or had worked previously in other provinces.
Figure 1.
HIV, Syphilis and HCV prevalence among FSW by ages
Figure 2.
HIV, Syphilis and HCV prevalence among FSW by venues
Prevalence of Syphilis
Overall, 6.1% (n=772) of the sample tested positive for syphilis. The demographic pattern of syphilis prevalence was similar to that of HIV prevalence. As shown in Figure 1, the prevalence of syphilis was positively associated with increasing age. Syphilis infection was significantly higher among women who were recruited from mini-hotels/road-side restaurants (13.3%) or the street (13.2%) than among women who recruited from other venues (Figure 2). More FSWs who ever married had syphilis than those who never married. There was no difference in syphilis infection by place of primary residence. FSW of ethnic minority has a higher prevalence than FSW of Han ethnicity. Educational attainment was negatively associated with the syphilis prevalence with the highest (12.8%) among FSW with no formal schooling and the lowest (2.6%) among FSW who attended at least high school. Although the syphilis prevalence significantly differed by the length working in the current work location, there was not a clear trend by time. In general, women who had worked in Guangxi before (either in other cities or in the current city) had higher syphilis prevalence (7.3% and 6.3%) than those who either worked in other province (5.1%) or did not have a previous work location (4.9%). Nearly Thirty percent (n=33) of women infected with HIV in the current study were co-infected with syphilis.
Prevalence of HCV infection
Overall, about 1.0% of FSW tested positive for HCV. The prevalence of HCV was significantly associated with age group (Figure 1), with the prevalence (1.1%) among older women (20 years or older) being more than 10-fold that of younger women (e.g., 0.1% among those 19 years or younger). FSW of Han ethnicity had a significant higher rate of HCV (1.3%) than FSW of ethnic minority (0.6% for Zhuang and 0.7% for others). There were some differences in HCV prevalence among types of venue, marital status, place of primary residence, educational attainment, length working in the current location, and location of previous job, but none of these differences reached statistical difference. Seven of the 125 cases of HIV infections (5.6%) were also con-infected with HCV.
Multivariable Analysis
Both unadjusted OR and aOR from the multivariable logistic regression analyses were presented in Table 2. The multivariable analyses confirmed the results of bivariate results regarding the higher risk of HIV and syphilis infection among women who were old, working at small commercial sex venues or at the street, divorced/widowed, or having low educational attainment. The significant predictors for HIV infection in the multivariable analysis included being older than 40 years of age (aOR=5.40), working at mini-hotel/road side restaurant or hair salon/massage parlor (aOR=5.31 and 4.10, respectively), being divorced or widowed (aOR=2.68), no formal schooling or finishing only elementary school (aOR=7.62 and 5.08, respectively), and previously working other cities within Guangxi (aOR=3.90). The significant predictors for syphilis infection included older age (aOR=3.81 and 2.48 for age groups of “>40 years” and “20–39 years”, respectively), working at mini-hotel/road side restaurant, hair salon/massage polar, hotel/restaurant, or KTV/dancehall/bar (aOR=2.79, 3.52, 2.00, and 2.07, respectively), being divorced/widowed (aOR=1.60), being Zhuang or other ethnic minority (aOR=1.33 and 1.50, respectively), and low educational attainment (aOR=2.52, 2.31, and 1.75 for no schooling, elementary school and middle school, respectively). Working at hair salon/massage parlor (aOR=2.31), non-Guangxi residence (aOR=0.46), and working in the current location between one to six months (aOR=0.53) were associated with HCV infection.
Table 2.
Results of Multivariable Logistic Regression (n=12,622)
| HIV | Syphilis | HCV | ||||
|---|---|---|---|---|---|---|
| Unadjusted aOR(95%CI) |
Adjusted aOR(95%CI) |
Unadjusted aOR (95%CI) |
Adjusted aOR(95%CI) |
Unadjusted aOR (95%CI) |
Adjusted aOR(95%CI) |
|
| AGE GROUP | ||||||
| ≥ 40 years | 15.97(3.81,66.99)**** | 5.40(1.19,24.62)* | 7.52(4.76,11.87)**** | 3.81(2.32,6.26)**** | 12.57(1.63,96.86)* | n/a |
| 20–39 years | 5.39(1.33,21.91)* | 3.25(0.78,13.66) | 3.32(2.16,5.10)**** | 2.48(1.59,3.87)**** | 13.38(1.87,95.86)* | n/a |
| ≤ 19 years | Reference | Reference | Reference | Reference | Reference | Reference |
| TYPES OF VENUE | ||||||
| Street | 10.90(4.28,27.74)**** | 5.31(1.87,15.04)*** | 5.35(3.39,8.40)**** | 2.79(1.72,4.53)**** | 1.31(0.30,5.75) | 1.59(0.35,7.29) |
| Mini-hotel/Road-side restaurant | 6.96(3.34,14.50)**** | 4.10(1.83,9.15)*** | 5.37(4.02,7.18)**** | 3.52(2.60,4.76)**** | 1.60(0.79,3.25) | 1.92(0.90,4.09) |
| Hair salon/Massage | 2.51(1.22,5.14)* | 2.08(0.96,4.49) | 2.39(1.83,3.14)**** | 2.00(1.52,2.64)**** | 2.01(1.16,3.48)* | 2.31(1.30,4.11)*** |
| Hotel/Restaurant | 2.25(1.02,4.98)* | 2.14(0.92,4.95) | 2.40(1.79,3.24)**** | 2.07(1.53,2.80)**** | 1.46(0.77,2.79) | 1.72(0.88,3.36) |
| KTV/Dancehall/Bar | 1.62(0.60,4.36) | 1.28(0.43,3.79) | 0.97(0.63,1.50) | 0.89(0.57,1.38) | 1.04(0.44,2.43) | 1.16(0.48,2.77) |
| Nightclub | n/a | n/a | 0.87(0.44,1.70) | 0.93(0.46,1.90) | 0.36(0.05,2.70) | 0.35(0.05,2.67) |
| Sauna/Bath | Reference | Reference | Reference | Reference | Reference | Reference |
| MARITAL STATUS | ||||||
| Divorced/Widowed | 5.75(2.94,11.22)**** | 2.68(1.27,5.68)* | 2.88(2.04,4.08)**** | 1.60(1.11,2.32)* | 1.66(0.71,3.87) | 1.30(0.54,3.13) |
| Currently Married | 1.27(0.50,3.27) | 1.45(0.56,3.80) | 1.19(0.82,1.72) | 1.15(0.79,1.68) | 1.20(0.57,2.53) | 1.28(0.60,2.72) |
| Cohabitate | 2.22(1.47,3.36)**** | 1.28(0.80,2.06) | 1.89(1.61,2.22)**** | 1.18(0.99,1.42) | 0.99(0.68,1.43) | 0.77(0.52,1.15) |
| Never Married | Reference | Reference | Reference | Reference | Reference | Reference |
| PRIMARY RESIDENCE | ||||||
| Foreigner /Viet Nam | 8.65(3.05,24.53)**** | 3.83(0.96,15.34) | 1.35(0.48,3.76) | 0.73(0.25,2.12) | n/a | 0.60(0.27,1.30) |
| Other Provinces | 0.76(0.48,1.19) | 0.81(0.47,1.40) | 0.96(0.81,1.13) | 1.03(0.83,1.28) | 1.39(0.95,2.02) | 0.46(0.28,0.75)*** |
| Guangxi | Reference | Reference | Reference | Reference | Reference | Reference |
| ETHNICITY | ||||||
| Other ethnicity | 1.84(1.04,3.24)* | 0.99(0.50,1.93) | 1.77(1.39,2.26)**** | 1.50(1.16,1.94)*** | 0.53(0.25,1.14) | 0.60(0.27,1.29) |
| Zhuang | 1.50(1.03,2.19)* | 0.93(0.60,1.45) | 1.58(1.36,1.85)**** | 1.33(1.11,1.59)*** | 0.47(0.30,0.74)*** | 0.46(0.28,0.75)*** |
| Han | Reference | Reference | Reference | Reference | Reference | Reference |
| EDUCATION | ||||||
| No Formal Schooling | 24.88(7.29,84.88)**** | 7.62(2.12,27.32)*** | 5.47(3.60,8.31)**** | 2.52(1.62,3.92)**** | 1.14(0.37,3.47) | 1.04(0.32,3.33) |
| Elementary | 9.34(2.92,29.83)**** | 5.08(1.57,16.51)** | 3.68(2.66,5.09)**** | 2.31(1.65,3.24)**** | 1.00(0.53,1.89) | 0.82(0.41,1.62) |
| Middle | 3.52(1.09,11.35)* | 2.70(0.83,8.77) | 2.00(1.45,2.76)**** | 1.75(1.26,2.43)*** | 1.32(0.75,2.34) | 1.27(0.70,2.31) |
| >High School | Reference | Reference | Reference | Reference | Reference | Reference |
| TIME IN CURRENT LOCATION | ||||||
| < 1 month | 1.29(0.76,2.21) | 1.70(0.97,2.98) | 0.88(0.69,1.11) | 1.03(0.80,1.31) | 0.99(0.58,1.71) | 1.20(0.69,2.10) |
| 1~6 month | 0.91(0.59,1.40) | 1.33(0.84,2.10) | 0.68(0.56,0.81)**** | 0.81(0.67,0.98)* | 0.60(0.38,0.95)* | 0.64(0.39,1.04) |
| 6~12 month | 0.77(0.46,1.29) | 1.05(0.62,1.78) | 0.78(0.64,0.95)* | 0.89(0.73,1.10) | 0.85(0.54,1.35) | 0.94(0.59,1.51) |
| > 12 month | Reference | Reference | Reference | Reference | Reference | Reference |
| LOCATION OF PREVIOUS JOB | ||||||
| Other Province | 2.27(0.65,7.90) | 1.54(0.42,5.57) | 1.04(0.75,1.44) | 0.82(0.58,1.16) | 1.58(0.71,3.50) | 1.11(0.49,2.53) |
| Other cities in GX | 5.14(1.56,16.94)** | 3.90 (1.16,13.09)* | 1.52(1.11,2.09)** | 1.21(0.87,1.67) | 1.43(0.63,3.25) | 1.25(0.54,2.87) |
| Current City | 4.21(1.32,13.35)* | 2.87(0.89,9.29) | 1.29(0.97,1.72) | 0.93(0.69,1.25) | 1.45(0.69,3.01) | 1.35(0.63,2.86) |
| No Previous Work | Reference | Reference | Reference | Reference | Reference | Reference |
p<.05,
p<.01,
p<.001,
p<.0001
Discussion
The current study, utilizing a large sample of FSW from NSS data from Guangxi, China, strongly suggested higher rates of HIV and syphilis among FSW who were older, worked at small commercial sex venues or at street, were divorced/widowed or of minority ethnicity, and had lower educational attainment. Because of their age disadvantage, older women were more likely to work in low-paying venues, which increased their risks of HIV/STI (X. S. Chen, Wang, et al., 2012; Huang, Henderson, Pan, & Cohen, 2004; Zhang et al., 2012). In the context of commercial sex, women who were divorced or widowed usually had more financial pressure to support families, and they were prone to conduct unprotected sex for more money. Being ethnic minority women in China, they usually grew up in resources-poor settings and usually lacked opportunities of education and skill trainings. Without job-related skills, these disempowered women may lack of opportunities to find alternative jobs. The data in the current study not only identify a high risk group of FSW, but also support the association between disadvantaged socioeconomic status (e.g., low educational attainment, working at the lower stratum of the sex industry, divorced/widowed, ethnic minority members) and high HIV risk that has been hypothesized or speculated in the global literature (Baral et al., 2012; Buzdugan, Halli, & Cowan, 2009; X. S. Chen, Liang, et al., 2012; X. S. Chen, Peeling, Yin, & Mabey, 2011; Tucker, Yin, Wang, Chen, & Cohen, 2011; Zhang et al., 2012).
The data in the current study showed a similar demographic pattern of HIV and syphilis infections among FSW in China. This finding is consistent with the global literature on the potential co-infection between HIV and syphilis. The large percentage of co-infection of HIV with syphilis (i.e., 33 of the 125 cases of HIV infection were also infected with syphilis) in the current study suggests the importance of examining the syphilis epidemic among FSW in China. In the past decade, China has witnessed a rapid increase in the prevalence of syphilis among high-risk groups including FSW, with syphilis cases increasing from 0.2 per 100,000 persons in the year 1993 to 5.7 per 100,000 persons in 2005 (Z. Q. Chen et al., 2007; J. Li, Chen, Merli, Weir, & Henderson, 2012). As syphilis infection can facilitate HIV transmission by increasing susceptibility to HIV infection (Galvin & Cohen, 2004), the increasing but relatively hidden syphilis epidemic deserves more attentions in future HIV/STI intervention preventions.
A relatively low prevalence of HCV is identified in the current analysis. The existing literature has showed a large variation of HCV infection among FSW across different countries from less than 1% among FSW in Venezuela to more than 80% among FSW who were also injecting drugs in UK (Camejo, Mata, & Díaz, 2003; Kucirka et al., 2011; Taylor et al., 2008). Therefore, it is unclear whether the low prevalence found in the current study reflects the actual HCV epidemic among this population in China. Future research on HCV infection among FSW, especially among the subgroup of FSW who are using or injecting drugs, is needed to improve our understanding of HCV infection among FSW in China and other low and middle-income countries.
The alarmingly high rate of HIV and syphilis infections among cross-border foreign FSW indicates the need for HIV control programs to consider this largely hidden population in Guangxi and other border areas. Cross-border FSW may have higher risk compared to their counterparts in either original or hosting country as they are highly mobile and lack of access to local HIV/STI prevention intervention programs (J. T. F. Lau & Wong, 2000; Van Duifhuizen & Hendriks, 1992). These women may also facilitate the spread of HIV/STI from high-prevalence regions to low-prevalence areas (J. T. Lau & Tsui, 2003). There is a need to establish an international collaboration to implement HIV prevention interventions across national borders. In addition, the routine surveillance should be strengthened and expanded in order to monitor this most-at-risk but often hard-to-reach population.
The findings in the current study need to be interpreted with some cautions in light of two potential methodological limitations. First, the data were derived from a cross-sectional survey, which prevents us from making a conclusive inference regarding the risk status of different groups of FSW who are at risk of contracting HIV or syphilis. Longitudinal studies are needed in the future to confirm temporality of the exposure (e.g., the most apparent exposure due to their lower socioeconomic status) and HIV/syphilis infection. Second, the data in the current study were collected in a multiethnic region in China, which may limit our ability to generalize the findings to other regions of China.
Despite of these potential limitations, the findings of the current analysis have some important implications for HIV and syphilis prevention intervention among FSW in China. First, China may need to increase the NSS among FSW with socioeconomic disadvantages (e.g., older, low-educated, widowed/divorced, and working at low-tier venues or at the street) and the large proportion of women with high mobility (e.g., short time working in the current location, coming from other cities, and no local residency), as it is difficult to engage these sub-populations of FSW in the HIV/syphilis prevention efforts, and therefore, they are at a much higher risk of HIV and syphilis infection and transmission. Second, China needs to increase community-based HIV and other STI prevention intervention initiatives engaging FSW with socioeconomic disadvantages. These prevention and intervention efforts should include frequent testing and timely treatment. Because of their social and economic disadvantages, empowerment should also be an integrated part of these efforts. Third, attention is needed for cross-border foreign FSW. Because of the complexity in identifying and reaching this largely hidden and mobile population and other challenges in terms of jurisdiction, custom, and language, joint and coordinated efforts cross the national boards may be needed to effectively target this population. The last but not the least, more research is needed to explore the issues of HCV infection among FSW, especially among FSW who are using or injecting illicit drugs in China.
Table 1.
Differences of HIV, Syphilis, and HCV Infections by Demographic Profile among 12,622 Female Sex Workers in Guangxi, China
| HIV (n=125) | Syphilis (n=772) | HCV (n=128) | ||
|---|---|---|---|---|
| N (%) | % | % | % | |
| Overall | 12622 (100%) | 1.0% | 6.1% | 1.0% |
| AGE GROUP | ||||
| ≥ 40 | 1142 (9.1%) | 2.6% | 12.5% | 1.1% |
| 20–39 | 10296 (81.6%) | 0.9% | 5.9% | 1.1% |
| ≤ 19 | 1184 (9.4%) | 0.2% | 1.9% | 0.1% |
| p-value | 0.000 | 0.000 | 0.004 | |
| TYPES OF VENUE | ||||
| Street | 227 (1.8%) | 4.0% | 13.2% | 0.9% |
| Mini-hotel/Road-side restaurant | 1401 (11.1%) | 2.6% | 13.3% | 1.1% |
| Hair salon/Massage | 4785 (37.9%) | 0.9% | 6.4% | 1.3% |
| Hotel/Restaurant | 2251 (17.8%) | 0.8% | 6.4% | 1.0% |
| KTV/Dancehall/Bar | 1150 (9.1%) | 0.6% | 2.7% | 0.7% |
| Nightclub | 415 (3.3%) | 0 | 2.4% | 0.2% |
| Sauna/Bath | 2387 (18.9%) | 0.4% | 2.8% | 0.7% |
| p-value | 0.000 | 0.000 | 0.074 | |
| MARITAL STATUS | ||||
| Divorced/Widowed | 370 (2.9%) | 3.2% | 11.4% | 1.6% |
| Currently Married | 5863 (46.5%) | 1.3% | 7.8% | 1.0% |
| Cohabitate | 679 (5.4%) | 0.7% | 5.0% | 1.2% |
| Never Married | 5696 (45.1%) | 0.6% | 4.3% | 1.0% |
| p-value | 0.000 | 0.000 | 0.638 | |
| PRIMARY RESIDENCE | ||||
| Foreigner /Viet Nam | 49 (0.4%) | 8.2% | 8.2% | 0 |
| Other Provinces | 3104 (24.6%) | 0.8% | 5.9% | 1.3% |
| Guangxi | 9452 (74.9%) | 1.0% | 6.2% | 0.9% |
| p-value | 0.000 | 0.732 | 0.177 | |
| ETHNICITY | ||||
| Other ethnicity | 1021 (8.1%) | 1.5% | 8.5% | 0.7% |
| Zhuang | 4071 (32.3%) | 1.2% | 7.7% | 0.6% |
| Han | 7442 (59.0%) | 0.8% | 5.0% | 1.3% |
| p-value | 0.032 | 0.000 | 0.001 | |
| EDUCATION | ||||
| No Formal Schooling | 413 (3.3%) | 4.4% | 12.8% | 1.0% |
| Elementary | 3511 (27.8%) | 1.7% | 9.0% | 0.9% |
| Middle | 7025 (55.7%) | 0.6% | 5.1% | 1.1% |
| >High School | 1643 (13.0%) | 0.2% | 2.6% | 0.9% |
| p-value | 0.000 | 0.000 | 0.535 | |
| TIME IN CURRENT LOCATION | ||||
| < 1 month | 1434 (11.4%) | 1.3% | 6.4% | 1.2% |
| 1~6 month | 3754 (29.7%) | 0.9% | 5.0% | 0.7% |
| 6~12 month | 2642 (20.9%) | 0.8% | 5.7% | 1.0% |
| > 12 month | 4770 (37.8%) | 1.0% | 7.2% | 1.2% |
| p-value | 0.410 | 0.000 | 0.157 | |
| LOCATION OF PREVIOUS JOB | ||||
| Other Province | 2352 (18.6%) | 0.6% | 5.1% | 1.1% |
| Other Cities in GX | 2091 (16.6%) | 1.3% | 7.3% | 1.0% |
| Current City | 7011 (55.6%) | 1.1% | 6.3% | 1.0% |
| No Previous Work | 1139 (9.0%) | 0.3% | 4.9% | 0.7% |
| p-value | 0.004 | 0.006 | 0.730 | |
Note: Categories of some variables do not add up to 100% due to missing values.
Acknowledgments
Funding Information
The study described in this report was in part supported by NIH Research Grant R01AA018090 by the National Institute for Alcohol Abuse and Alcoholism. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute for Alcohol Abuse and Alcoholism.
Reference
- Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, Kerrigan D. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet Infectious Diseases. 2012;12(7):538–549. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- Buzdugan R, Halli SS, Cowan FM. The female sex work typology in India in the context of HIV/AIDS. Tropical Medicine & International Health. 2009;14(6):673–687. doi: 10.1111/j.1365-3156.2009.02278.x. [DOI] [PubMed] [Google Scholar]
- Camejo MI, Mata G, Díaz M. Prevalence of hepatitis B, hepatitis C and syphilis in female sex workers in Venezuela. Revista de Saúde Pública. 2003;37(3):339–344. doi: 10.1590/s0034-89102003000300012. [DOI] [PubMed] [Google Scholar]
- Chen XS, Liang GJ, Wang QQ, Yin YP, Jiang N, Zhou YJ, Wang B. HIV Prevalence Varies Between Female Sex Workers From Different Types of Venues in Southern China. Sexually Transmitted Diseases. 2012;39(11):868–870. doi: 10.1097/OLQ.0b013e318264c3ba. [DOI] [PubMed] [Google Scholar]
- Chen XS, Peeling RW, Yin YP, Mabey DC. The epidemic of sexually transmitted infections in China: implications for control and future perspectives. BMC Medicine. 2011;9:111. doi: 10.1186/1741-7015-9-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen XS, Wang QQ, Yin YP, Liang GJ, Jiang N, Yang LG, Wang B. Prevalence of syphilis infection in different tiers of female sex workers in China: implications for surveillance and interventions. BMC Infectious Diseases. 2012;12:84. doi: 10.1186/1471-2334-12-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen ZQ, Zhang GC, Gong XD, Lin C, Gao X, Liang GJ, Cohen MS. Syphilis in China: results of a national surveillance programme. The Lancet. 2007;369(9556):132–138. doi: 10.1016/S0140-6736(07)60074-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nature Reviews Microbiology. 2004;2(1):33–42. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
- GuangxiCDC. Update on HIV/AIDS epidemic in Guangxi. Guangxi: 2011. [Google Scholar]
- Huang Y, Henderson GE, Pan S, Cohen MS. HIV/AIDS risk among brothel-based female sex workers in China: assessing the terms, content, and knowledge of sex work. Sexually Transmitted Diseaes. 2004;31(11):695–700. doi: 10.1097/01.olq.0000143107.06988.ea. [DOI] [PubMed] [Google Scholar]
- Jia Y, Lu F, Sun X, Vermund SH. Sources of data for improved surveillance of HIV/AIDS in China. The Southeast Asian Journal of Tropical Medicine and Public Health. 2007;38(6):1041. [PMC free article] [PubMed] [Google Scholar]
- Kucirka LM, Sarathy H, Govindan P, Wolf JH, Ellison TA, Hart LJ, Segev DL. Risk of Window Period Hepatitis-C Infection in High Infectious Risk Donors: Systematic Review and Meta-Analysis. American Journal of Transplantation. 2011;11(6):1188–1200. doi: 10.1111/j.1600-6143.2011.03460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau JT, Tsui HY. HIV/AIDS behavioral surveillance surveys of the cross-border sex-networker population in Hong Kong from 1997 to 2001. Sexually Transmitted Diseases. 2003;30(11):827–834. doi: 10.1097/01.OLQ.0000086605.65963.12. [Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- Lau JTF, Wong WS. Behavioural surveillance of sexually-related risk behaviours for the cross-border traveller population in Hong Kong: The evaluation of the overall effectiveness of relevant prevention programmes by comparing the results of two surveillance surveys. Internatinal Journal of STD & AIDS. 2000;11(11):719–727. doi: 10.1258/0956462001915138. [DOI] [PubMed] [Google Scholar]
- Li J, Chen XS, Merli MG, Weir SS, Henderson GE. Systematic Differences in Risk Behaviors and Syphilis Prevalence Across Types of Female Sex Workers: A Preliminary Study in Liuzhou, China. Sexually Transmitted Diseases. 2012;39(3):195. doi: 10.1097/OLQ.0b013e31823d2e2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Hong Y, Poston D. Preventing HIV in women: a top priority in China's efforts in fighting AIDS. AIDS Care. 2011;23(sup1):1–4. doi: 10.1080/09540121.2011.575121. [DOI] [PubMed] [Google Scholar]
- Lu L, Jia M, Ma Y, Yang L, Chen Z, Ho DD, Zhang L. The changing face of HIV in China. Nature. 2008;455(7213):609–611. doi: 10.1038/455609a. [DOI] [PubMed] [Google Scholar]
- Rou K, Sullivan SG, Liu P, Wu Z. Scaling up prevention programmes to reduce the sexual transmission of HIV in China. International Journal of Epidemiology. 2010;39(suppl 2):ii38–ii46. doi: 10.1093/ije/dyq211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X, Wang N, Li D, Zheng X, Qu S, Wang L, Poundstone K. The development of HIV/AIDS surveillance in China. AIDS. 2007;21(Suppl 8):S33–S38. doi: 10.1097/01.aids.0000304694.54884.06. [Review]. [DOI] [PubMed] [Google Scholar]
- Taylor A, Hutchinson SJ, Gilchrist G, Cameron S, Carr S, Goldberg DJ. Prevalence and determinants of hepatitis C virus infection among female drug injecting sex workers in Glasgow. Harm Reduction Jounral. 2008;5(11) doi: 10.1186/1477-7517-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JD, Yin YP, Wang B, Chen XS, Cohen MS. An expanding syphilis epidemic in China: epidemiology, behavioural risk and control strategies with a focus on low-tier female sex workers and men who have sex with men. Sexually Transmitted Infections. 2011;87(Suppl 2):ii16–ii18. doi: 10.1136/sti.2010.048314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS, & MoH. 2012 China AIDS Response Progress Report. 2012 Retrieved from http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_CN_Narrative_Report[1].pdf. [Google Scholar]
- Van Duifhuizen R, Hendriks A. AIDS and mobility: the impact of international mobility on the spread of HIV/AIDS, needs and possibilities for international cooperation (Abstract no. 5235) 1992 [Google Scholar]
- Wang N, Wang L, Wu Z, Guo W, Sun X, Poundstone K, Wang Y. Estimating the number of people living with HIV/AIDS in China: 2003–09. Internatinoal Journal of Epidemiology. 2010;39(suppl 2):ii21–ii28. doi: 10.1093/ije/dyq209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Li X, Hong Y, Zhou Y, Liu W, Stanton B. Unprotected sex with their clients among low-paying female sex workers in southwest China. AIDS Care. 2012 doi: 10.1080/09540121.2012.726345. [DOI] [PMC free article] [PubMed] [Google Scholar]