Abstract
This longitudinal study aimed to examine the enduring effects of parental HIV/AIDS on children's psychological well-being in Asia. A sample of 1625 children aged from 6 to 18 years old were assessed annually for their depressive symptoms over three years. Latent growth curve modeling (LGCM) was used to examine the trajectories of depressive symptoms among AIDS orphans and vulnerable children in comparison with children from HIV-free families. AIDS orphans demonstrated the highest initial level of depressive symptoms among the three groups. On average, children's depressive symptoms scores can be expected to realize an approximate 25% decrease for AIDS orphans, 19% decrease for vulnerable children and 15% decrease for comparison children over a 3-year period. Individual differences within the groups showed that children with higher initial level of depressive symptoms can be expected to decrease slower over time. Multiple group LGCM showed that the three groups of children demonstrated significantly different trajectories of depressive symptoms. Among the key demographic factors, only age exerted an effect on the trajectory of depressive symptoms of vulnerable children, indicating that the younger children showed higher level of initial depressive symptoms and lower rate of decrease than the older children. The current study enriched our knowledge on the longitudinal effect of parental HIV/AIDS on children's emotional distress. Future psychological support might take the children's developmental stages and cultural appropriateness into consideration and deliver service for the most vulnerable group of children affected by HIV/AIDS.
Keywords: HIV/AIDS, Children, Longitudinal Trajectories, Depressive Symptoms, Latent Growth Curve Model
Introduction
The death of a parent due to AIDS during childhood can be particularly traumatic, with a profound and potentially lasting impact on a child's psychosocial well-being (X. Li et al., 2008). Existing cross-sectional findings regarding the impact of parental HIV/AIDS on children's well-being were mixed. Some studies have suggested that losing a parent to HIV/AIDS is a significant risk factor to child and adolescent psychological adjustment (Chi & Li, 2012; Cluver & Orkin, 2009; Fang et al., 2009; Kaggwa & Hindin, 2010). However, some other studies reported that many of these children were not reporting clinically significant or elevated levels of mental health problems (Mellins et al., 2008; Nyamukapa et al., 2010).
To gain a better understanding of persistence or resilience concerning children's mental health problems in the context of parental HIV/AIDS in a developmental perspective, cross-sectional evidence may be insufficient. Limited longitudinal evidence regarding the effect of parental HIV/AIDS on children's psychological well-being was only available in South Africa and the US, but not in Asia. Cluver and colleagues (2012) found that, in South Africa, AIDS orphans showed a higher level of depressive symptoms, anxiety, and post-traumatic stress at both baseline assessment and four-year follow-up when compared with children orphaned by other causes and children from HIV-free families. Three longitudinal studies in the US indicated a different trajectory of psychological distress among children affected by HIV/AIDS. Rotheram-Borus and colleagues (2005) found that psychological distress among bereaved adolescents showed a peak 1 year prior to parental death and then declined to the level similar to that among non-bereaved adolescents after one year following parental death. Forehand and colleagues (1999) also found that AIDS orphans did not differ from children of HIV-free families in externalizing problems and depressive symptoms by either 6-month or 2-3 years after maternal death. Likewise, Pelton and colleagues (2005) found that more AIDS orphans fell into the clinical range of internalizing problems before maternal death than comparison children from HIV-free families, but no differences existed among the two groups at 6 months after maternal death.
Such discrepant findings in South Africa and US remind researchers to be cautious about the transferability of study findings on AIDS orphanhood and psychological distress among different regions. The political, economic and cultural factors may play important roles regarding the impact of parental HIV/AIDS on children's psychological well-being (Chi & Li, 2012). With the generalized epidemic and relatively low-resources in South Africa, parental HIV/AIDS has been found to be associated with ongoing social and economic hardship (Cluver et al., 2012; Mueller, Alie, Jonas, Brown, & Sherr, 2011). Many studies in sub-Saharan Africa reported that children affected by HIV/AIDS experienced extreme food scarcity (e.g., Cluver, Gardner, & Operario, 2009), inadequate medical support (Ostergaard & Meyrowitsch, 2008), and poor school enrollment (Nyamukapa et al., 2010). These unsatisfied but very basic developmental needs may account for the sustained or amplified distress of children affected by HIV/AIDS in the region. In contrast, risk factors related to extreme poverty were seldom reported in the US studies. Moreover, children of parents with HIV/AIDS in US are typically of ethnic minority background and might have experienced racism, discrimination and stigma even before parental HIV infection (Havens & Mellins, 2009). Thus, it is possible that regardless of parental HIV status, the majority of children living in the same community was exposed to similar levels of stress and thereby experience similar levels of psychological distress.
Although some cross-sectional studies in China found that parental HIV/AIDS was associated with poor psychological adjustment of children (e.g., He & Ji, 2007; L. Li, Jiang, Lord, & Rotheram-Borus, 2007; X. Li, Barnett, et al., 2009), limited evidence indicated whether this effect is relatively short-term or persisting. The current longitudinal study aims to address this knowledge gap. Specifically, the three objectives of this study are (a) to estimate the depressive symptoms trajectories of three groups of children: AIDS orphans (children who have lost one or both of their parents to HIV-related illness), vulnerable children (children whose one or both parents are living with HIV/AIDS), and comparison children (children from HIV-free families); (b) to examine whether the three groups of children demonstrate different depressive symptoms trajectories; (c) to explore the effects of children's age and gender, and family SES on their depressive symptoms trajectories.
Method
Study Site and Participants
The current study was conducted in 2006-2010 in two rural counties in central China where many residents had been infected with HIV through unhygienic blood collection. Both counties have more than 94% rural residents and have the highest prevalence of HIV-infection in the area. The participants in the current study were mainly recruited from five administrative villages (administrating111 natural villages). Children 6 to 18 years of age were eligible to participate in the study. The participants in the first annual assessment included 755 orphans, 466 vulnerable children, and 404 comparison children. The same participants were assessed annually for three times.
Sampling Procedure
The sampling and consenting procedure for the study was described in detail elsewhere (X. Li, Barnett, et al., 2009). Briefly, 206 orphans living in orphanages were recruited from four government-funded orphanages and eight community-based group homes. To recruit 549 orphans and 466 vulnerable children from family or kinship care, we obtained the lists of families caring for orphans or with confirmed diagnosis of parental HIV/AIDS. We approached the families on the lists and recruited one child per family to participate in the study. This process was repeated until the target sample size for the AIDS orphans and vulnerable children (i.e., about 1,200 in total) was achieved. The comparison group was recruited from the same villages where the orphans and vulnerable children were recruited. The research protocol, including sampling and consenting procedure, was approved by the Institutional Review Boards at both Wayne State University in the United States and Beijing Normal University in China.
Survey Procedure
Each child participating in the study completed a confidential assessment inventory including demographic information, depressive symptoms scale and other scales of psychosocial adjustment. The interviewers were trained education and psychology graduate students and faculty members from the local universities. After the households were randomly selected, interviewers will visit the households. To protect participants' privacy, we worked with children to come up with an individualized plan for assessment in terms of the preferable time and place for them to feel comfortable to meet with the researchers. During the survey, necessary clarification or instruction was provided promptly when needed. The entire assessment inventory took about 75 to 90 minutes including breaks. Each child received a gift at completion of the assessment as a token of appreciation.
Measures
Depression
Children's depressive symptoms were measured using the Center for Epidemiological Studies Depression Scale for Children (CES-DC; Fendrich, Wessiman, & Warner, 1990). The CES-DC was translated into Chinese in the early 1990s and was validated with various Chinese populations (Wang, 1993; Zhang, Yang, Huang, Liu, & Sun, 2010). The scale is a 20-item self-report measure with a four-point response option (0 = not at all, 1 = a little, 2 = sometimes, 3 = a lot). A mean score was employed with higher scores indicating increasing levels of depressive symptoms. Cronbach alpha of the scale was .81 across three years for the current sample.
Demographic characteristics
Children were asked to report on individual and family characteristics during the survey. These characteristics included age, sex, ethnicity, parental education (i.e., no schooling, elementary school, middle school, ≥ high school), and the main occupational activities that their parents were currently engaged in or were engaged in before their death (i.e., farmer, migrant worker, local small merchant, or other). A composite score was created to estimate children's family SES by indexing those children whose parents had greater than elementary school education and engaged in non-farming occupational activities. The SES score was ranged from 0 to 4 with higher scores indicating a higher family SES.
Statistical Analysis
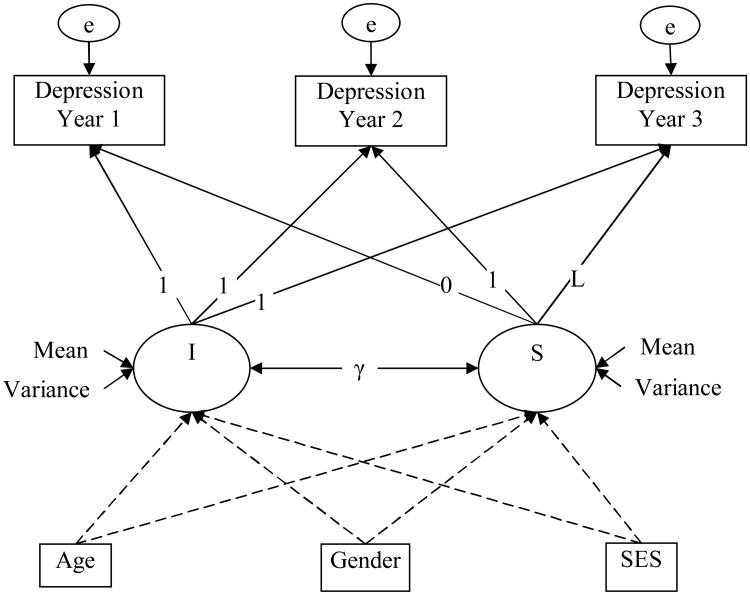
First, an unspecified growth curve model (Figure 1) was proposed. The basic model without covariates was analyzed to depict the depressive symptoms trajectory of each group of children (orphans, vulnerable children, and comparison children). Second, multiple group analysis was conducted to test whether there is difference of the depressive symptoms trajectories among the three groups. Six nested models were tested and compared in a hierarchical order. Finally, conditional models with three covariates (child's age and gender and family SES) were estimated to investigate the effects of these covariates on the depressive symptom trajectories. We estimated four conditional growth curve models for each group of children, with one for each covariate and one examining all three covariates simultaneously.
Figure 1.
The unspecified growth curve model for the trajectory of depressive symptoms of children across three annual assessments. The intercept, denoted as I, represents information concerning overall mean and variance of individual intercepts that characterize each individual's initial level of depressive symptoms. The slope (denoted as S) represents the trend of an individual's trajectory determined by the repeated assessments of depressive symptoms. The factor loadings of the intercept are fixed at 1. With the two factor loadings of slope fixed at 0 and 1, the third factor loading is allowed to be freely estimated (denoted as L in Figure 1). For the purpose of model identification, error variances associated with depressive symptoms across three years were constrained to be equal.
The analyses were performed using Mplus 5.1 (Muthén & Muthén, 2007). Acceptable model fit is determined by an RMSEA (Root Mean Square or Errors of Approximation) less than .08 (Hatcher, 2005) and values of CFI (Comparative Fit Index) and TLI (Tucker Lewis Index) greater than .95 (Hu & Bentler, 1999). To deal with missing values, we used full information maximum likelihood (FIML) estimation, which produces less biased and more reliable results compared with conventional methods of missing data treatment (Enders & Bandalos, 2001).
Results
Preliminary Data Analysis
The sample in the first annual assessment consisted of 826 boys and 799 girls. The mean age did not differ between boys and girls. Orphans were older than either vulnerable children or the comparison children (F(2,1613) = 19.24, p<.0001). The family SES composite score differed among three children groups with comparison children scoring the highest and vulnerable children scoring the lowest (F(2,1623) =11.00, p < .0001). Ninety-nine percent of the children were of Han ethnicity.
Data were available for 1625 children at year 1, for 1288 at year 2, and for 1019 at year 3. Nineteen percent of children did not provide data in both year 1 and year 2. Those lost to follow ups were more likely to have higher average level of depressive symptoms at year 1 assessment (Ms = 1.03 vs. .91, p < .001, d = .21), to be orphans (χ2(2) = 14.57, p < .001), and to be older (Ms = 14.49 vs.12.48, p < .001, d = .75). About 74.2% orphans or vulnerable children were aware parental HIV infection. Children's awareness of parental HIV was not correlated to children's depressive symptoms at baseline or follow-ups. As shown in Table 2, the correlations of depressive symptoms across three years were medium.
Table 2. Descriptive statistics and intercorrelations of depressive symptoms score across three years.
| Mean | SD | Depression year 2 | Depression year 3 | |
|---|---|---|---|---|
| Total | ||||
| Depression year 1 | .93 | .42 | .38*** | .26*** |
| Depression year 2 | .76 | .37 | .43*** | |
| Depression year 3 | .72 | .36 | ||
| AIDS orphans | ||||
| Depression year 1 | 1.02 | .43 | .37*** | .31*** |
| Depression year 2 | .81 | .39 | .55*** | |
| Depression year 3 | .75 | .38 | ||
| Vulnerable children | ||||
| Depression year 1 | .89 | .39 | .29*** | .20*** |
| Depression year 2 | .74 | .35 | .38*** | |
| Depression year 3 | .71 | .38 | ||
| Comparison children | ||||
| Depression year 1 | .81 | .41 | .43*** | .20*** |
| Depression year 2 | .69 | .34 | .25*** | |
| Depression year 3 | .69 | .30 |
Note:
p < .001
Trajectory of Depressive Symptoms
To answer our first research question regarding the depressive symptoms trajectories of orphans, vulnerable children and comparison children, we estimated the basic model among three groups. The proposed model fit the data well among all three groups (see Table 3). As shown in Table 4, all the parameters in the basic model were significant, including the means of the intercept, the slope and the factor loading at year 2. Figure 2A illustrates the average, predicted trajectories of depressive symptoms of the three groups. Overall, depressive symptoms tended to decrease from the first assessment. Orphans demonstrated the highest rate of change and comparison children demonstrated the lowest (-.22, vs. -.13 vs. -.08). The average depressive symptoms score was expected to realize an approximate 25% decrease for orphans, 19% decrease for vulnerable children and 15% decrease for comparison children over a 3-year period. The covariance of latent intercept and slope were significantly negative in all three groups, suggesting that the higher initial level of depressive symptoms accompanied with the higher rate of decrease expected over time. Individual differences significantly existed in the initial level of depressive symptoms and rate of change within each group.
Table 3. Model fit of Basic Multiple Group Growth Curve Models.
| χ2 | df | RMSEA | 90%CI | CFI | TLI | Δχ2/Δdf | |||
|---|---|---|---|---|---|---|---|---|---|
| Single group analysis | |||||||||
| AIDS orphans | 5.24 | 2 | .05 | .00-.10 | .99 | .98 | — | ||
| Vulnerable children | 2.13 | 2 | .01 | .00-.09 | 1.00 | 1.00 | — | ||
| Comparison children | 6.12 | 2 | .07 | .01-.14 | .95 | .93 | — | ||
|
| |||||||||
| Multiple group analysis | |||||||||
| M1 Unconstrained | 13.49 | 6 | .05 | .01-.08 | .98 | .97 | — | ||
| M2 Constrained (L) | 16.11 | 8 | .04 | .01-.07 | .98 | .98 | 2.62/2 | ||
| M3 Constrained (L, Means of I S) | 97.73 | 12 | .12 | .09-.14 | .79 | .84 | 81.62/4*** | ||
| M4 Constrained (L, Means of I S, Variances of I S) | 116.12 | 16 | .11 | .09-.13 | .75 | .86 | 18.39/4** | ||
| M5 Constrained (L, Means of I S, Variances of I S, γ) | 134.36 | 18 | .11 | .09-.13 | .71 | .86 | 18.24/2*** | ||
| M6 Constrained (L, Means of I S, Variances of I S, γ, errors) | 142.43 | 20 | .11 | .09-.12 | .70 | .86 | 8.07/2* | ||
Table 4. Unstandardized estimates of parameters of Growth Curve Models.
| Estimates | Basic Model | Conditional Model | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Age covariate | SES covariate | Gender covariate | All covariates | ||||||||||||
| Mean | Var | L | Mean | Var | L | Mean | Var | L | Mean | Var | L | Mean | Var | L | |
| AO | |||||||||||||||
| I | 1.03a | .12a | 1.19a | .89a | .12a | 1.18a | 1.04a | .12a | 1.19a | 1.03a | .12a | 1.19a | .91a | .12a | 1.19a |
| S | -.22a | .06a | -.36a | .06a | -.23a | .06a | -.24a | .06a | -.40a | .06a | |||||
| γ | -.05a | -.05a | -.05a | -.05a | -.05a | ||||||||||
| VC | |||||||||||||||
| I | .88a | .07a | 1.27a | 1.10a | .07a | 1.21a | .90a | .07a | 1.26a | .87a | .07a | 1.28a | 1.11a | .07a | 1.22a |
| S | -.13a | .05b | -.66a | .04b | -.12a | .05b | -.15a | .05b | -.68a | .04b | |||||
| γ | -.04b | -.03a | -.04b | -.04a | -.03b | ||||||||||
| CC | |||||||||||||||
| I | .80a | .10a | 1.54a | .68a | .10a | 1.46a | .82a | .10a | 1.59a | .81a | .10a | 1.58a | .70a | .10a | 1.55a |
| S | -.08a | .02c | -.21 | .03c | -.10b | .02c | -.07c | .02c | -.21 | .02c | |||||
| γ | -.04a | -.04a | -.04a | -.04a | -.04a | ||||||||||
Note: I = Intercept, S = Slope, γ = covariance between Intercept and Slope, Var = Variance, L = factor loading of depression of wave 3 on slope; Coding for gender (0 = male, 1 = female).
p < .001;
p < .01,
p < .05
Figure 2.
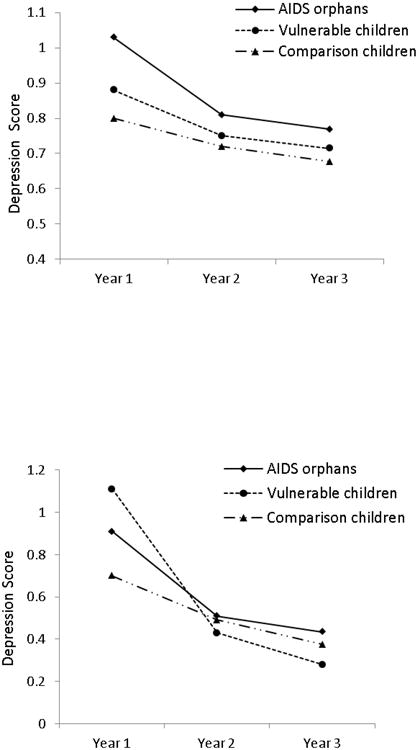
A. Average predicted trajectory of depressive symptoms for AIDS orphans, vulnerable children and comparison children.
B. Average predicted trajectory of depressive symptoms for AIDS orphans, vulnerable children and comparison children, controlling for age, gender and family socio-economic status.
Group Differences of Trajectory of Depressive Symptoms
Using a set of multiple group comparisons, we tested whether a model in which parameters were freely estimated yielded a better fit than models with cross group equality constraints on the parameters. The unconstrained model (M1) that allowed all the parameters to be freely estimated fit the data well. In M2, we set the factor loadings (L) to be invariant across three groups. The model fit did not change significantly (Δχ2/Δdf = 2.62/2, p >.05), suggesting that the rate of change at third annual assessment across groups were not significantly different. In M3, we further constrained the means of intercept and slope to be equal and these restrictions worsen the model fit significantly (Δχ2/Δdf = 81.62/4, p < .001). This result indicated that the averaged initial level and rate of change were different across three groups. In M4, M5 and M6, we further restricted the variances of intercept and slope, covariance between intercept and slope, and error variances to be equal across groups, which result in significantly worse model fit (Δχ2/Δdf = 18.39/4, 18.24/2, 8.07/2, ps < .01, .001 and .05). Thus, the findings suggest that orphans, vulnerable children and comparison children showed different depressive symptoms trajectories.
Effects of Demographic Covariates on Trajectory of Depressive Symptoms
Gender and family SES did not predict changes of depressive symptoms in either group of children. Age significantly and negatively influenced the initial level and rate of change of depressive symptoms for vulnerable children, even after controlling the effects of gender and family SES. Older vulnerable children have lower initial depressive symptoms score and a higher rate of decrease. In other words, parental illness is more influential to younger children than older children. Figure 2B illustrates the average, predicted trajectory of depressive symptoms scores among the three groups of children controlling for age, gender and family SES.
Discussion
This study examined the trajectories of depressive symptoms over three years among AIDS orphans and vulnerable children in comparison with children from HIV-free families, and investigated the effects of children's age and gender and family SES on the trajectories of depressive symptoms. Our data indicated a significant decrease in depressive symptoms across three groups of children over three years. Our findings are relatively consistent with the three US-based longitudinal studies but inconsistent with the one in South Africa. The inconsistent results in different regions may be attributable to three reasons.
First, the decrease of depressive symptoms in our sample might be due partially to the AIDS relief efforts in China since 2004. At the end of 2004, the central government of China initiates a “four free, one care” policy including the provision of free antiretroviral drugs to AIDS patients, free voluntary counseling and testing, free drugs to prevent mother-to-child transmission, free schooling for AIDS orphans, and care and economic assistance to the households of people living with HIV/AIDS (Wu, Sullivan, Wang, Rotheram-Borus, & Detels, 2007). This policy might benefit children in two aspects: improved school attendance and reduced financial hardship. In an earlier study, it was reported that a quarter to a half of AIDS orphans quitted school because of financial hardship (Yang et al., 2006). In contrast, according to the data from our field work in 43 villages in one of our study counties, only 7% (42/577) school-age AIDS orphans did not go to school and most of these children migrated to cities with their surviving parent or relatives (X. Li, Fang, et al., 2009). In addition, the financial assistance to the HIV-affected households may also protect children against the stress of family economic hardship, and in turn relieve children from the risk of psychological distress.
Second, the different sample characteristics might account for the inconsistency of findings. As reported, children and adolescents, in the study by Cluver and colleagues, were recruited from 9 schools, 18 community organizations, and door-to-door sampling to approach highly vulnerable children (Cluver et al., 2012). In our sample, nonetheless, due to the government policy discussed before, the majority of our sample attended primary or junior high schools. As suggested by developmental theory, school plays a crucial role in children's socialization process. Attending school regularly might help children to acquire life skills to cope with problems in their life and to create social support networks (Nyamukapa et al., 2010).
Third, the inconsistency in the findings might reveal the underlying developmental trajectories in different developmental stages. As noted, the average age in the sample of South Africa is around 17, but the average age of our sample is around 12. One of the longitudinal studies in US is around 15. The other two US-based studies recruited children from 6 to 11 years old. Studies with sample of children in face of various adversities (Garber, Keiley, & Martin, 2002; Ge, Natsuaki, & Conger, 2006; Kim & Cicchetti, 2006) have corroborated that, the development of depressive symptoms was best characterized by a U-shaped trajectory, with declining depressive symptoms from early adolescence and an increase starting around age 14 (Dekker et al., 2007). Thus, the increased distress associated with AIDS orphanhood in the South Africa study might reflect the particularly stressful transition from adolescence into young adulthood.
Importantly, our data showed that AIDS orphans, vulnerable children and comparison children showed different trajectories of depressive symptoms over three years. AIDS orphans and vulnerable children demonstrated higher initial levels of depressive symptoms and also higher decrease rate of change at group level. These findings are consistent with theory and empirical evidence regarding bereaved children in general. That is, most parentally bereaved children experienced one to two year periods of intense distress, followed by recovery to the level of mental health that were similar to that of prior to parental loss (Akerman & Statham, 2011; Dowdney, 2000). From our data, younger vulnerable children were expected to experience higher levels of depressive symptoms and lower decrease rate over time than older children. Younger children are more dependent on their parents for instrumental and emotional support in their development, thus the anticipated death or actual death of a parent may result in more extensive disturbance and provoke severer bereavement among younger children (Dowdney, 2000).
The current study had some potential limitations requiring attention. First, after three years, our study had a retention rate of 63%. The results must be interpreted in light of the fact that some of the most vulnerable children (such as children dropped from schools or more depressed) were among those who were unable to be located. Second, statistically, the possibility of regression toward the mean cannot be ruled out from the current research design. More time points of assessments are needed to be designed in future studies, which may provide more information about sequential patterns such as diminutions, escalations, or other changes of children's depressive symptoms. Third, due to concerns of missing data and inaccurate reporting from children, the data on the onset of parental illness and death during the study were not included in the current analysis.
Despite the limitations, this study is one of the first known efforts that examined the longitudinal effect of parental HIV/AIDS on children's psychological well-being in Asia. It included children from HIV-free families in the same community as comparison group with reasonable follow-up rates over three years. The results of the present study enriched our knowledge on the developmental trajectories of depressive symptoms among children in the context of HIV-related parental illness and death by providing data in Asia.
Table 1. Sample Characteristics at Year One and retention rate.
| Overall | AIDS Orphans | Vulnerable Children | Comparison Children | |
|---|---|---|---|---|
| N(%) | 1625(100%) | 755(47%) | 466(29%) | 404(25%) |
| Boys | 826(51%) | 403(53%) | 219(47%) | 204(51%) |
| Girls | 799(49%) | 352(47%) | 247(53%) | 200(50%) |
| Mean Age in Years (SD) | 12.85(2.21) | 13.16(2.20) | 12.36(2.24) | 12.83(2.11)* |
| Family SES Score (SD) | 1.94(1.17) | 1.92(1.17) | 1.79(1.17) | 2.15(1.15)* |
| Awareness of Parental HIV | 862(74.2%) | 534(73.5%) | 328(75.6%) | N/A |
| Year Two Follow-up | 1288(79%) | 569(75%) | 384(82%) | 335(83%)* |
| Year Three Follow-up | 1019 (63%) | 417(55%) | 326(70%) | 276(68%)** |
p < .001,
p < .0001
Table 5. Regression coefficients of three covariates on growth curve parameters.
| Age covariate | SES covariate | Gender covariate | All covariates | |
|---|---|---|---|---|
| AIDS orphans | ||||
| Predicting Intercept | ||||
| Age | .03 | .03 | ||
| SES | -.03 | -.03 | ||
| Gendera | .00 | .00 | ||
| Predicting Slope | ||||
| Age | .05 | .05 | ||
| SES | .04 | .05 | ||
| Gendera | .20 | .19 | ||
| Vulnerable children | ||||
| Predicting Intercept | ||||
| Age | -.06* | -.07* | ||
| SES | -.03 | -.05 | ||
| Gendera | .09 | .09 | ||
| Predicting Slope | ||||
| Age | .20*** | .20*** | ||
| SES | -.06 | .01 | ||
| Gendera | .11 | .12 | ||
| Comparison children | ||||
| Predicting Intercept | ||||
| Age | .03 | .03 | ||
| SES | -.03 | -.03 | ||
| Gendera | -.03 | -.03 | ||
| Predicting Slope | ||||
| Age | .07 | .06 | ||
| SES | .08 | .08 | ||
| Gendera | -.13 | -.12 |
Note:
0 = male, 1 = female
Acknowledgments
The content of the article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental health and the National Institute of Nursing Research.
Funding: This study reported in this article was supported by NIH Research Grant from the National Institute of Mental health (R01MH76488) and the National Institute of Nursing Research (R01NR13466).
References
- Akerman R, Statham J. Childhood Bereavement: A rapid literature review. London: Child Wellbeing Research Centre; 2011. [Google Scholar]
- Chi P, Li X. Impact of Parental HIV/AIDS on Children's Psychological Well-Being: A Systematic Review of Global Literature. AIDS and Behavior. 2012 doi: 10.1007/s10461-012-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver L, Gardner F, Operario D. Poverty and psychological health among AIDS-orphaned children in Cape Town, South Africa. AIDS care. 2009;21(6):732–741. doi: 10.1080/09540120802511885. [DOI] [PubMed] [Google Scholar]
- Cluver L, Orkin M. Cumulative risk and AIDS-orphanhood: Interactions of stigma, bullying and poverty on child mental health in South Africa. Social Science & Medicine. 2009;69(8):1186–1193. doi: 10.1016/j.socscimed.2009.07.033. [DOI] [PubMed] [Google Scholar]
- Cluver L, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. Journal of Child Psychology and Psychiatry. 2012;53(4):363–370. doi: 10.1111/j.1469-7610.2011.02459.x. [DOI] [PubMed] [Google Scholar]
- Dekker MC, Ferdinand RF, Van Lang NDJ, Bongers IL, Van Der Ende J, Verhulst FC. Developmental trajectories of depressive symptoms from early childhood to late adolescence: gender differences and adult outcome. Journal of Child Psychology and Psychiatry. 2007;48(7):657–666. doi: 10.1111/j.1469-7610.2007.01742.x. [DOI] [PubMed] [Google Scholar]
- Dowdney L. Annotation: Childhood bereavement following parental death. Journal of Child Psychology and Psychiatry. 2000;41(7):819–830. doi: 10.1111/1469-7610.00670. [DOI] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8(3):430–457. doi: 10.1177/0013164401615001. [DOI] [Google Scholar]
- Fang X, Li X, Stanton B, Hong Y, Zhang L, Zhao G, et al. Lin D. Parental HIV/AIDS and psychosocial adjustment among rural Chinese children. Journal of Pediatric Psychology. 2009;34(10):1053–1062. doi: 10.1093/jpepsy/jsp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fendrich M, Wessiman MM, Warner V. Screening for depressive disorder in children and adolescents: Validating the Center for Epidemiologic Studies Depression Scale for Children. American Journal of Epidemiology. 1990;131(3):538–551. doi: 10.1093/oxfordjournals.aje.a115529. [DOI] [PubMed] [Google Scholar]
- Forehand R, Pelton J, Chance M, Armistead L, Morse E, Morse PS, Stock M. Orphans of the AIDS epidemic in the United States: transition-related characteristics and psychosocial adjustment at 6 months after mother's death. AIDS Care. 1999;11(6):715–722. doi: 10.1080/09540129947622. [DOI] [PubMed] [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents' depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70(1):79–95. doi: 10.1037/0022-006X.70.1.79. [DOI] [PubMed] [Google Scholar]
- Ge X, Natsuaki MN, Conger RD. Trajectories of depressive symptoms and stressful life events among male and female adolescents in divorced and nondivorced families. Development and psychopathology. 2006;18(1):253–273. doi: 10.1017/S0954579406060147. 10.10170S0954579406060147. [DOI] [PubMed] [Google Scholar]
- Hatcher L. A step-by-step approach to using SAS for factor analysis and structural equation modeling. Cary, NC: SAS Institute Inc; 2005. [Google Scholar]
- Havens JF, Mellins CA. Psychiatric aspects of HIV/AIDS in childhood and adolescence. In: Rutter M, Taylor M, editors. Rutter's Child and Adolescent Psychiatry. Oxford, UK: Blackwell; 2009. pp. 945–955. [Google Scholar]
- He Z, Ji C. Nutritional status, psychological well-being and the quality of life of AIDS orphans in rural Henan Province, China. Tropical Medicine & International Health. 2007;12(10):1180–1190. doi: 10.1111/j.1365-3156.2007.01900.x. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Kaggwa EB, Hindin MJ. The psychological effect of orphanhood in a matured HIV epidemic: An analysis of young people in Mukono, Uganda. Social Science & Medicine. 2010;70(7):1002–1010. doi: 10.1016/j.socscimed.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Kim J, Cicchetti D. Longitudinal trajectories of self-system processes and depressive symptoms among maltreated and nonmaltreated children. Child Development. 2006;77(3):624–639. doi: 10.1111/j.1467-8624.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Jiang L, Lord L, Rotheram-Borus MJ. The perception of family conflict by parents living with HIV/AIDS and their adolescent children. Journal of HIV/AIDS Prevention in Children & Youth. 2007;8(1):99–114. doi: 10.1300/J499v08n01_06. [DOI] [Google Scholar]
- Li X, Barnett D, Fang X, Lin X, Zhao G, Zhao J, et al. Stanton B. Lifetime incidence of traumatic events and mental health among children affected by HIV/AIDS in rural China. Journal of Clinical Child and Adolescent Psychology. 2009;38(5):731–744. doi: 10.1080/15374410903103601. [DOI] [PubMed] [Google Scholar]
- Li X, Fang X, Stanton B, Zhao G, Lin X, Zhao J, et al. Chen X. Psychometric evaluation of the Trauma Symptoms Checklist for Children (TSCC) among children affected by HIV/AIDS in China. AIDS Care. 2009;21(3):261–270. doi: 10.1080/09540120802195119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Naar-King S, Barnett D, Stanton B, Fang X, Thurston C. A developmental psychopathology framework of the psychosocial needs of children orphaned by HIV. Journal of the Association of Nurses in Aids Care. 2008;19(2):147–157. doi: 10.1016/j.jana.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins CA, Brackis-Cott E, Dolezal C, Leu CS, Valentin C, Meyer-Bahlburg HFL. Mental health of early adolescents from high-risk neighborhoods: The role of maternal HIV and other contextual, self-regulation, and family factors. Journal of Pediatric Psychology. 2008;33(10):1065. doi: 10.1093/jpepsy/jsn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller J, Alie C, Jonas B, Brown E, Sherr L. A quasi-experimental evaluation of a community-based art therapy intervention exploring the psychosocial health of children affected by HIV in South Africa. Tropical Medicine & International Health. 2011;16(1):57–66. doi: 10.1111/j.1365-3156.2010.02682.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. Fifth. Los angeles, CA: Author; 2007. [Google Scholar]
- Nyamukapa CA, Gregson S, Wambe M, Mushore P, Lopman B, Mupambireyi Z, et al. Jukes MCH. Causes and consequences of psychological distress among orphans in eastern Zimbabwe. AIDS Care. 2010;22(8):988–996. doi: 10.1080/09540121003615061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostergaard LR, Meyrowitsch DW. Children at risk: A study of the psychosocial impact of HIV on orphans and other vulnerable children in Benin. Africa Development. 2008;33(3):109–125. [Google Scholar]
- Pelton J, Forehand R. Orphans of the AIDS epidemic: An examination of clinical level problems of children. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(6):585–591. doi: 10.1097/01.chi.0000157551.71831.57. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Weiss R, Alber S, Lester P. Adolescent adjustment before and after HIV-related parental death. [Research Support, U.S. Gov't, P.H.S.] Journal of Consulting and Clinical Psychology. 2005;73(2):221–228. doi: 10.1037/0022-006X.73.2.221. [DOI] [PubMed] [Google Scholar]
- Wang X. Rating Scales for Mental Health (Chinese Journal of Mental Health Supplement) Beijing: Chinese Association of Mental Health; 1993. [Google Scholar]
- Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China's response to HIV/AIDS. The Lancet. 2007;369(9562):679–690. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Wu Z, Duan S, Li Z, Li X, Shen M, et al. Stanton B. Living environment and schooling of children with HIV-infected parents in southwest China. AIDS care. 2006;18(7):647–655. doi: 10.1080/09540120500282896. [DOI] [PubMed] [Google Scholar]
- Zhang G, Yang Y, Huang Y, Liu S, Sun X. Epidemiological investigation on depression among 6–16 years old children and adolescents in Chengdu. Chinese Mental Health Journal. 2010;24:211–214. [Google Scholar]