Abstract
Hemilaminectomy and mini-hemilaminectomy were performed on opposite sides of the spine at T11–T12, T13-L1, and L2–L3 in 11 canine cadavers in order to report differences in the access provided to the thoracolumbar vertebral canal. Measurements of the vertebral canal height, defect height, and dorsal and ventral remnants of the vertebral arch were obtained after computed tomography. A median of 7% to 20% of the vertebral canal height was not removed dorsally after mini-hemilaminectomy compared to 1% to 2% in hemilaminectomy. Thirteen to 25% of the vertebral canal height was left ventrally in mini-hemilaminectomy and 11% to 27% in hemilaminectomy. Potential for a restricted exposure of thoracolumbar lesions should be considered if lesions are located in the ventral 11% to 27% vertebral canal height when performing either procedure or in the dorsal 7% to 20% of the canal height when performing a mini-hemilaminectomy.
Résumé
Comparaison, à l’aide de tomodensitométrie, de la fenêtre d’accès créée par une hémilaminectomie et une mini-hémilaminectomie dans le canal vertébral thoracolombaire. Une hémilaminectomie et une mini-hémilaminectomie ont été réalisées sur les côtés opposés de la colonne vertébrale à T11–T12, à T13-L1 et à L2–L3 sur 11 cadavres canins afin de signaler les différences de l’accès fourni au canal vertébral thoracolombaire. Les mesures de la hauteur du canal vertébral et des vestiges dorsaux et ventraux de l’arc vertébral ont été obtenues après une tomodensitométrie. Une médiane de 7 % à 20 % de la hauteur du canal vertébral n’a pas été enlevée dorsalement après une mini-hémilaminectomie comparativement à 1 % ou 2 % pour une hémilaminectomie. De 13 % à 25 % de la hauteur du canal vertébral a été laissée ventralement dans la mini-hémilaminectomie et de 11 % à 27 % dans l’hémilaminectomie. Le potentiel d’une exposition restreinte des lésions thoracolombaires devrait être considéré si les lésions sont situées dans le 11 % à 27 % de la portion ventrale de la hauteur du canal vertébral lors de la réalisation des deux interventions ou dans le 7 % à 20 % de la portion dorsale de la hauteur du canal lors de la réalisation d’une mini-hémilaminectomie.
(Traduit par Isabelle Vallières)
Introduction
Access to the vertebral canal is needed in neurosurgical conditions such as intervertebral disc (IVD) extrusions, exploratory surgical procedures and resection of neoplastic lesions, granulomas, cysts, and hematomas. Herniation of the IVD is the most common cause of spinal cord dysfunction in dogs (1–3), with the thoracolumbar spine most commonly affected (3–9). Spinal cord decompression through removal of the extruded compressive disc material after gaining access to the vertebral canal is the treatment of choice for dogs showing neurological deficits and/or persistent or recurrent spinal pain, and with spinal cord compression identified on diagnostic imaging (1,2,10,11).
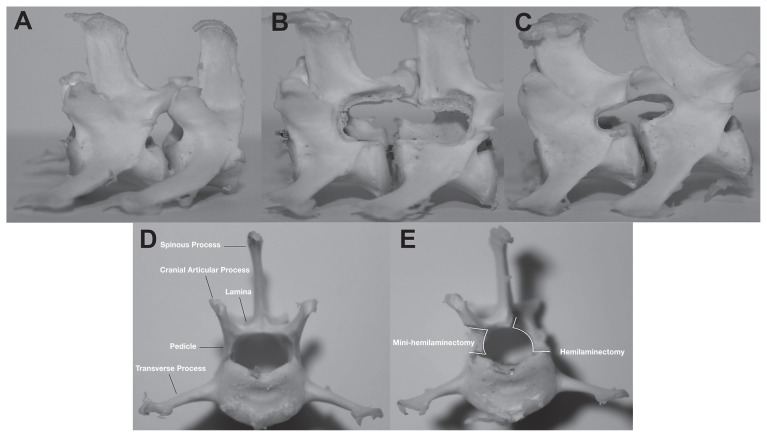
The 2 most common decompressive surgical procedures used for the thoracolumbar spine, hemilaminectomy and mini-hemilaminectomy (Figure 1), differ in their access to the vertebral canal and the amount of bone removed (10,12). Hemilaminectomy requires removal of one-half of the vertebral arch, including the lamina, pedicle, and the articular processes on 1 side of the vertebrae (10,12–14). Mini-hemilaminectomy preserves the articular processes by removing only the pedicles adjacent to the intervertebral foramen (6,10,12,15–22). Proposed benefits for creating a smaller window are decreased soft tissue dissection, surgical time, and a possible reduced impact on the biomechanical stability, leading to less postoperative morbidity (10,12,15,20,23,24). However, the benefit of creating a smaller surgical and bone window may sometimes be outweighed by decreased exposure and ability to remove the compressive lesion. In the case of IVD herniation, one potential cause for absence of improvement or continued deterioration in neurological function is inadequate evacuation of compressive material resulting in residual compression.
Figure 1.
Lumbar vertebrae of cadavers. Lateral views of unaltered (A), left-sided hemilaminectomy (B), and left-sided mini-hemilaminectomy (C). Transverse view of the cranial aspect of an unaltered lumbar vertebra (D). Transverse view of the cranial aspect of an altered lumbar vertebra with a left-sided hemilaminectomy and right-sided mini-hemilaminectomy (E).
During pre-surgical planning, the exact location of the compression should guide the selection of a surgical approach and the extension of the bone window. Nevertheless, many surgeons refer to described guidelines to create a “standard” hemilaminectomy or mini-hemilaminectomy defect to approach the vast majority of IVD extrusions and typically use one procedure over the other depending on preference and experience. Information regarding the exact anatomical landmarks and indications for each procedure are limited and variable (12–20). There have been no direct accurate comparisons of the section of the vertebral canal accessed and the height of the lamina removed through these 2 surgical procedures or determination of the superiority of one procedure at specific thoracolumbar sites.
Factors that could influence the ability to achieve the desired bone window, such as the longitudinal location within the thoracolumbar spine, should be considered during pre-surgical planning; however, few variables have been objectively assessed. For instance, if particular aspects of the thoracic vertebrae, such as the articulation with the rib head, visually or physically impede the ability to maintain anatomical landmarks during mini-hemilaminectomy, this could result in greater bone removal and negate the proposed advantages over a hemilaminectomy. While the goal of surgery is adequate removal of the compressive lesion, and this should be tailored to the individual patient (17), specific knowledge of these limits is required before any potential benefit can be conveyed.
Since specific quantitative data about the access window provided by each of these 2 standard procedures is missing, clear indications for either procedure cannot be made. As an inadequate lesion removal can affect the outcome, more accurate knowledge of the physical limits of each technique is necessary to improve our ability to decide which surgical technique would be more beneficial in each particular scenario.
The objectives of this study were to describe standardized anatomical limits of each technique in the canine thoracolumbar spine and report any observed differences in the access provided to the thoracolumbar vertebral canal that could be considered during pre-surgical planning.
Materials and methods
Eleven canine cadavers from a colony of research beagles euthanized for reasons unrelated to the study were utilized. The study was approved by the University of Guelph animal use and care committee. Ten cadavers, weighing 8 to 11 kg, had both hemilaminectomy and mini-hemilaminectomy procedures performed on opposite sides of the vertebral column at T11–T12, T13-L1, and L2–L3 intervertebral sites. Procedure side was alternated between cadavers to ensure an even number for left and right sides. An eleventh cadaver had only mini-hemilaminectomies performed (right side). All hemilaminectomies were performed by 1 surgeon (LG) and all mini-hemilaminectomies were performed by another surgeon (BB). Both techniques adhered to previous descriptions in the veterinary literature and to clinical practice at our institution (10,12–14,16,17).
Hemilaminectomy was performed through a dorsal approach to the spine with the cadaver in sternal recumbency (10,12–14). The dorsal midline incision was extended from T10 to L4, through the skin and subcutaneous tissues. A small incision through the thoracolumbar fascia and supraspinatous ligament was made just lateral to the spinous process of L4, on the side of the hemilaminectomy and extended to T10 with scissors. Osteotomes were used for sharp dissection of the epaxial musculature (mulfidifus and longissimus) at its insertion on the dorsal spinous processes, articular processes, accessory, and mamillary processes, and surgical sites T11–T12, T13-L1, and L2–L3 were identified. The articular processes were removed at the appropriate surgical sites with rongeurs. Hemilaminectomy was performed with a Hall’s pneumatic drill, with the margins being the base of the spinous process dorsally, ventral aspect of the intervertebral foramen ventrally, and the base of the adjacent articular facet both cranial and caudal. Only the outer margins were burred, and once at the level of the inner periosteum the remaining vertebral arch was pulled away from the vertebral canal.
Mini-hemilaminectomy was performed through a dorsolateral approach with the cadaver positioned obliquely, midway between sternal and lateral recumbency with the surgical side up (10,12,15,20). A skin incision was made approximately 2 cm lateral to dorsal midline, and extended from T10 to L4 through the subcutaneous fat and lumbo-dorsal fascia. The intermuscular plane ventral to the longissimus musculature was identified and bluntly dissected to allow identification of the correct surgical sites. Once the desired space was identified, an incision was made through the longissimus muscles midway between the articular processes and the rib or transverse process and the bony lamina identified. The pedicles were cleared of soft tissues using a periosteal elevator and sharp dissection, exposing the desired intervertebral foramen. Surgical exposure spanned a space dorsal to the level of the ribs or transverse processes, and ventral to the base of the articular facet. Cranially and caudally, the dissection extended to, but did not expose the adjacent intervertebral foramina. Mini-hemilaminectomy was performed using a Hall’s pneumatic drill. The accessory process was first removed and this was used as the dorsal extent of the mini-hemilaminectomy. Ventral to this, the pedicle was burred cranial and caudal to the intervertebral foramen over approximately 2/3 of the length of each vertebra. The ventral extent of the mini-hemilaminectomy was the ventral aspect of the intervertebral foramen. Once exposed, the inner periosteum was removed using a 22-gauge needle with the tip bent at 90° and a #11 scalpel blade to expose the vertebral canal over the entire length of the window.
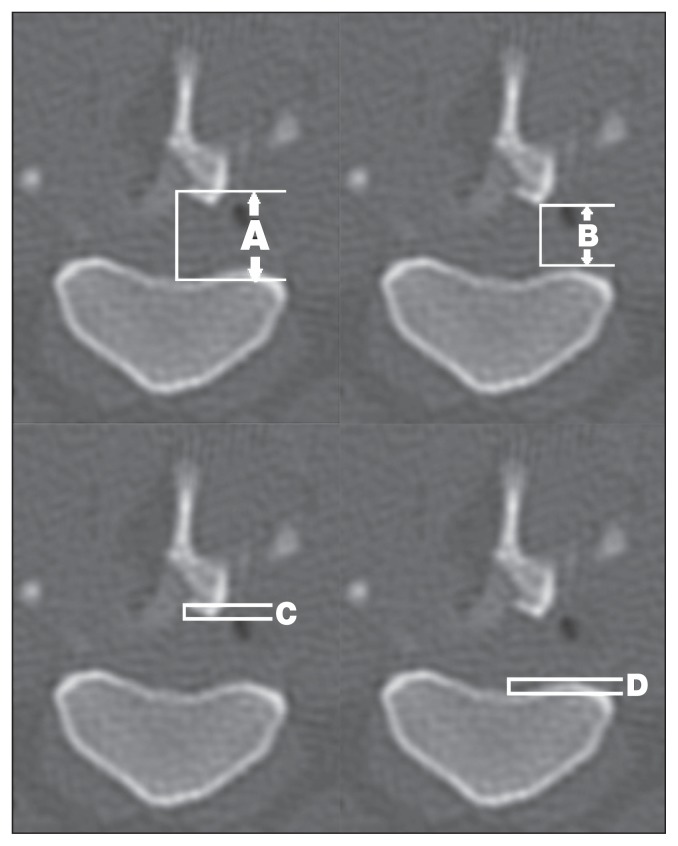
The thoracolumbar spine was imaged in each cadaver with a helical computed tomography (CT) unit (LightSpeed Quadslice Helical Scanner; General Electric, Milwaukee, Wisconsin, USA), 1.25 mm slice thickness, 0.75 mm slice interval, small scan field of view, sharp reconstruction kernel, kV 120, mA 300. Scans were viewed and analyzed with DICOM viewing software (Advantage Workstation, version 4.2; General Electric). Measurements were taken from the transverse slice in the point of the greatest defect height (Figure 2). The maximum height of the vertebral canal was measured (Figure 2C) and a perpendicular line tool overlain. Defect height was defined as the length from the most dorsal and ventral limits of the remaining vertebral arch (Figure 2D). To assess the relative dorsoventral position of the laminectomy window, the height of any remaining vertebral arch was measured, providing dorsal (Figure 2A) and ventral markers (Figure 2B). Dorsal and ventral remnants were defined as the height of the dorsal (lamina) and ventral (pedicle) aspects of the vertebral arch not removed during the laminectomy and measured at their maximum distance from the perpendicular line tool. Complete unilateral access would be a 100% removal of 1 side of the vertebral arch, with no dorsal or ventral remnants.
Figure 2.
Transverse computed tomography (CT) image at the point of greatest dorsoventral defect height for a right-sided mini-hemilaminectomy at T11-T12. Measurements demonstrated are vertebral canal height (A), defect height (B), dorsal remnant (C), and ventral remnant (D). A concurrent left-sided hemilaminectomy has also been performed.
Four variables (vertebral canal, defect, dorsal remnant, and ventral remnant heights) were measured at each surgery site. A total number of 252 measurements were taken. Each measurement was replicated and recorded 3 times, resulting in a total of 756 measurements. Three-dimensional reconstructions were created and assessed subjectively for uniformity. All measurements were performed individually by a single reviewer (JH). All measurements were linear, reported in mm, and maintained parallel to the sagittal axis using angles reported by the software program. To control for variation in size, the measurements defect height, dorsal remnant, and ventral remnant were later expressed as percentages of the vertebral canal height. When articular processes were invaded at a mini-hemilaminectomy, the dorsoventral height of the articular processes was measured at its smallest point within the cranial and caudal boundaries of the mini-hemilaminectomy. Given the lack of contralateral articular processes (concurrent hemilaminectomy), ipsilateral articular processes of the immediately caudal intervertebral disc space served as a control and height missing expressed as a percentage of the control’s height.
Statistical analyses
The data were collected in the form of a split-plot design, with each animal receiving a particular technique (whole-plot factor) and being split into a 2-factor factorial with the 2 factors side and site (split-plot factors); also, there was sub-sampling, which allows repeatability to be assessed. Each animal constituted a random blocking variable, while technique, side, and site are fixed effects variables. In addition, there was the covariate of canal height. The response measures may be related to this covariate. The covariate was entered into the model as a linear fixed effect as well as a quadratic effect. All 2-term interactions were included (along with the covariate and quadratic covariate) in the model to start, and then non-significant terms removed.
To analyze the data, a General Linear Mixed Model was employed using Proc Mixed in SAS (SAS, version 9.2; SAS Institute, Cary, North Carolina, USA). To assess the analysis of variance (ANOVA) assumptions, the residuals were formally tested for normality using the four tests offered by SAS (Proc UNIVARIATE): Shapiro-Wilk, Kolmogorov-Smirnov, Cramérvon Mises, and Anderson-Darling tests. All cases adequately met ANOVA assumptions. Data for the ventral remnant measure fit normality, so a log transformation with an added constant of 0.01 was applied. The residuals were also plotted against the predicted values as well as all explanatory variables (animal, side, site, technique, and canal height). A P-value < 0.05 was considered statistically significant.
Results
The observed differences in results varied with the covariate vertebral canal height. To trend this difference, estimated means were calculated for the lowest recorded vertebral canal height (6.8 mm), the median canal height (7.9 mm), and the tallest canal height (9.5 mm), with all reported results representing the estimated least squares means and confidence interval (CI) (Table 1). For mini-hemilaminectomies, estimated mean defect height was 75% (range: 71% to 79%) of the canal height at the lowest canal (6.8 mm height), 67% (range: 64% to 69%) at the median canal (7.9 mm), and 58% (range: 55% to 61%) at the tallest canal (9.5 mm). For hemilaminectomies, estimated mean defect height was 87% (range: 83% to 91%) of the canal at the lowest canal height, 81% (range: 79% to 84%) at the median canal height, and 76% (range: 2% to 79%) at the tallest canal. Therefore, 58% to 75% (estimated mean range) of the canal height was removed by mini-hemilaminectomies and 76% to 87% by hemilaminectomies.
Table 1.
Estimated differences of measured variables between mini-hemilaminectomies and hemilaminectomies (mm and % of vertebral canal height)
| Vertebral canal height | Defect height | Dorsal remnant | Ventral remnant | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mini-hemi | Hemi | Mini-hemi | Hemi | Mini-hemi | Hemi | |
| Lowest | 5.12 mm (75%) | 5.91 mm (87%) | 0.50 mm (7%) | 0.07 mm (1%) | 0.89 mm (13%) | 0.73 mm (11%) |
| Median | 5.28 mm (67%) | 6.42 mm (81%) | 1.05 mm (13%) | 0.13 mm (2%) | 1.37 mm (17%) | 1.12 mm (14%) |
| Tallest | 5.51 mm (58%) | 7.18 mm (76%) | 1.86 mm (20%) | 0.23 mm (2%) | 2.34 mm (25%) | 1.92 mm (20%) |
A statistically significant difference was observed in the laminectomy defect height between hemilaminectomy and mini-hemilaminectomy, and this was consistent at all vertebral canal heights. At the lowest canal height there was an estimated mean difference of 12% in defect height between surgical techniques (CI: 4% to 20%; P < 0.0001), at the median canal height a 14% mean height difference (CI: 10% to 20%; P < 0.0001), and at the tallest canal height an 18% height difference (CI: 11% to 24%; P < 0.0001). There was no effect of surgical site or side on defect height. However, the proportion of vertebral arch removed with both surgical techniques (defect height as a percentage of the vertebral canal height) significantly decreased with larger vertebral canals (P < 0.0001). This inverse relationship was greater for the mini-hemilaminectomy compared to the hemilaminectomy (P < 0.0001).
Dorsal remnant height (as estimated mean and CI) in the mini-hemilaminectomy group was 7% (range: 5% to −10%) of the vertebra; canal height for the lowest canal height, 13% (range: 12% to 15%) in the median canal, and 20% (range: 17% to 22%) in the tallest canal. In the hemilaminectomy group, dorsal remnant height was 1% (range: 0% to 4%) of the canal height for the lowest canal, 2% (range: 0% to 3%) in the median canal, and 2% (0% to 5%) in the tallest canal. Roughly, 7% to 20% of the vertebral canal height was not removed dorsally by mini-hemilaminectomy, while 1% to 2% was not removed by hemilaminectomy. The difference observed in the height of the dorsal remnant between mini-hemilaminectomy and hemilaminectomy was also statistically significant at all vertebral canal heights (P < 0.0009 to 0.0001). No effect of surgical site or side was observed.
Regarding mini-hemilaminectomies, estimated ventral remnant height for the lowest, median, and tallest vertebral canal heights were 13% (range: 10% to 17%), 17% (range: 14% to 22%), and 25% (range: 19% to 32%) of the corresponding canal height, respectively. In the hemilaminectomies, ventral remnant heights were 11% (range: 8% to 14%), 14% (range: 11% to 18%), and 20% (range: 15% to 27%) of the canal height for the lowest, median, and the tallest canal heights, respectively. Approximately 13% to 25% (estimated mean range) of the vertebral canal height was not removed ventrally by mini-hemilaminectomy, while 11% to 27% was not removed by hemilaminectomy. The ventral remnant height difference was not significant between surgical techniques, or surgery site, but was significant between the left and right sides of the vertebral column for the smaller vertebral canal height (P = 0.0097) but not the median or tallest canal height. For the lowest canal height the ventral remnant was larger on the left side compared to the right (1.09 mm or 16% of the vertebral canal height; CI: 0.75 to 1.43 mm, 11% to 21%).
In 18 of the 33 mini-hemilaminectomy sites (55%), the most ventral aspect of the articular processes was at least partially invaded. When the articular processes height at the mini-hemilaminectomy site was expressed as a percent of the articular processes height caudal to the procedure, a mean of 22% was removed (range: 4% to 41%).
Discussion
While retrospective studies of both procedures show similarly high clinical success rates (19,25–30), no direct comparison of the access window created by each procedure has been made. As expected, this study showed that the larger defect in hemilaminectomy was due to greater removal of bone dorsal to the intervertebral foramen (10,12), but no difference in the ventral limit.
The difference in the amount of dorsal remnant between surgical techniques ranged from 6% to 18% of the canal height (0.43 to 1.62 mm), meaning that 7% to 20% of the canal height was not removed dorsally by mini-hemilaminectomy, while 1% to 2% remained following hemilaminectomy. The clinical relevance of this is limited for ventral, ventrolateral, or lateral lesions, and likely of little significance for dorsolateral compressions considering exploratory instruments have curved tips with a length > 1 to 2 mm to access this area. In contrast, access to the central dorsal and opposite dorsolateral vertebral canal would be impeded without substantial manipulation of the spinal cord. This is not the case with most IVD herniations, as they are usually ventral, ventrolateral, or lateral (10). Laminectomy alone without evacuation of the offending lesion does not provide sufficient decompression (31,32); therefore, there is no potential benefit to providing a larger window if the lesion is not removed. However, these results should still be considered during pre-surgical planning. Visualization and access to lesions in the most dorsal 7% to 20% height of the vertebral canal could be more challenging with mini-hemilaminectomy compared to hemilaminectomy based on our data suggesting retention of 7% to 20% of the dorsal vertebral arch with mini-hemilaminectomy. That could be the case when dealing with intramedullary, intradural or even extradural lesions (neoplasia, synovial cyst) not associated with the intervertebral disc, where exposure of the entire lesion is necessary to address its removal and avoid unnecessary iatrogenic spinal trauma. Similarly, greater exposure could be desirable in more solid or chronic IVD extrusions with dural adhesions.
Although the authors expected that the ventral remnant height would be minimal or absent, it ranged from 13% to 25% of the canal height in mini-hemilaminectomies and 11% to 27% in hemilaminectomies. An explanation for these findings is that the measurement of vertebral canal height extends ventrally on the midline to the dorsal surface of the vertebral body, and thus enters the vertebral gutter, including vertebral body in the measurement when taken at the most lateral aspect of the vertebra. This would be especially true in lumbar vertebrae where the dorsal surface of the body is concave. Extending the laminectomy to the bottom of the canal would require invading the rib head, transverse process and vertebral body. This finding needs to be kept in mind as material in the most ventral 11% to 27% of the canal could be not exposed with either procedure. Other procedures providing a better access to the ventral canal floor, such as corpectomy, could be more desirable in chronic IVD protrusions, frequently located in the ventral midline and associated with adhesions (33).
No effect of intervertebral site was observed, suggesting that one procedure cannot be specifically recommended at a specific disc space along the thoracolumbar spine. However, an effect of surgery side was identified, but only for the ventral remnant of the lowest canal height. Anecdotally, right-handed surgeons seem to be more comfortable with a left-sided surgery, although both surgeons in this study were right-handed and the left side actually had the larger ventral remnant. Perhaps, the angle obtained from the left side may provide as good visualization through a smaller approach.
The “smaller” mini-hemilaminectomy procedure could reduce post-operative morbidity (10,12,20), as decreased bone removal is associated with lower morbidity in humans (23,24). Mini-hemilaminectomy and microdiscectomy are preferred in humans to limit bone removal (34).
Formation of a laminectomy membrane, a constrictive, fibrotic tissue covering the bone defect, is a reported cause of surgical failure in humans (35). The incidence of laminectomy membrane formation in the thoracolumbar spine in dogs is unknown, with only 3 confirmed cases following dorsal laminectomy (36). Formation of a laminectomy membrane is thought to be associated with techniques that remove large sections of the lamina, and in this case mini-hemilaminectomy could theoretically be superior to hemilaminectomy, although this has not been investigated and it does not appear to be a clinical problem (10).
Another concern with large laminectomies is the potential for low grade spinal instability that could increase morbidity (10). Spinal instability is not a concern in hemilaminectomies extended up to 3 consecutive spaces but it could be in active large breed dogs (1,37). Although removal of articular processes has minimal effects on lateral bending, it affects rotation (38–41). These factors are potentially more relevant in large-breeds and could be associated with the higher morbidity and lower surgical success compared with small dogs (42,43); consequently, mini-hemilaminectomies could be preferred in large dogs.
Although a smaller dorsal remnant was present in hemilaminectomies, 55% of the mini-hemilaminectomies in this study invaded the articular processes, although none extended beyond the level of the hemilaminectomies. While most mini-hemilaminectomy descriptions state that articular processes should be preserved (15,16,18–20), some reported the dorsal limit of the mini-hemilaminectomy window being just dorsal to the accessory process (21), which suggests that a portion of the articular processes would be inevitably encroached upon in small dogs. Other authors suggest removal of vertebral arch dorsal to the intervertebral foramen should vary with each individual case according to the location of the lesions (17). The effect of such an invasion on stability is not known.
One limitation of this study was the involvement of only 2 surgeons, each performing different techniques as per their clinical practice. Limiting each surgeon to 1 technique was chosen to prevent inadequate vertebral canal exposure from surgeons attempting a technique with which they were not familiar. However, we cannot argue that these results are not a direct comparison of the 2 surgeons. In addition, only a single reviewer performed the CT measurements. While it is unlikely to have biased the results, given the simplicity of obtaining the measurements, additional reviewers would be required to eliminate this potential.
The Hawthorne effect is suggested to occur when a study participant’s behavior and results are altered by their awareness of being monitored or included in a study, and may even have more influence on outcome measures than the placebo effect (44,45). As neither of the surgeons in our study was blinded to the inclusion of cadavers, the influence this may have had on the laminectomy created needs to be considered.
The procedures were performed on cadavers in a controlled environment, and did not take into account variation provided by clinical cases in a clinical scenario such as the location and extent of herniated disc material, hemorrhage, and the presence of a normal spinal cord. However, the purpose of the study was to document the access to the vertebral canal for both surgical techniques, and report any observed differences that may contribute to pre-surgical planning. A prospective study utilizing clinical cases would be necessary to assess post-operative morbidity and influence of intra-operative hemorrhage on visualization. Cadavers were chosen to provide greater control over anatomical variability, allowing multiple surgical sites to be assessed bilaterally along the longitudinal axis of the vertebral column in a single dog. Another limitation of this study may have been using the transverse image with the greatest defect height for measurements, as this could have resulted in underestimation of dorsal and ventral remnants, and subsequent overestimation of defect height. However, 3-D reconstructions were evaluated and determined the laminectomy windows to be relatively consistent in height across their length.
In conclusion, this study described anatomical limits provided by hemilaminectomy and mini-hemilaminectomy in the thoracolumbar spine. A potential limited exposure of lesions located in the dorsal 7% to 20% canal height after mini-hemilaminectomy and dorsal 1% to 2% after hemilaminectomy, and a restricted exposure of the ventral 11% to 27% vertebral canal height after either procedure should be considered. Although this difference is probably of limited significance in many acute intervertebral disc extrusions, it can influence the ability to evacuate some lesions leading to residual compression after surgery and a complicated or limited neurological functional recovery.
Acknowledgments
The authors acknowledge Jennifer Collins, Carolyn Bennett, and Sue Kinsella for their technical assistance, and Roberto Poma for his clinical insight. CVJ
Footnotes
Presented as a poster at the Annual American College of Veterinary Internal Medicine Forum, Denver, Colorado, June 2011. This manuscript represents a portion of a D.V.Sc thesis submitted by Dr. Huska to the University of Guelph.
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
Supported by a grant from the Ontario Veterinary College Pet Trust Fund.
References
- 1.Sturges BK, Dickinson PJ. BSAVA Manual of Canine and Feline Neurology. Gloucester, United Kingdom: British Small Animal Veterinary Association; 2004. Principles of Neurosurgery; pp. 355–367. [Google Scholar]
- 2.Dewey CW. A Practical Guide to Canine and Feline Neurology. Ames, Iowa: Wiley; 2008. Myelopathies; pp. 323–388. [Google Scholar]
- 3.Priester W. Canine intervertebral disc disease — Occurrence by age, breed, and sex among 8117 cases. Therio. 1976;6:293–303. [Google Scholar]
- 4.Ball MU, McGuire JA, Swaim SF, Hoerlein BF. Patterns of occurrence of disk disease among registered dachshunds. J Am Vet Med Assoc. 1982;180:519–522. [PubMed] [Google Scholar]
- 5.Bray JP, Burbidge HM. The canine intervertebral disk. Part two: Degenerative changes — nonchondrodystrophoid versus chondrodystrophoid disks. J Am Anim Hosp Assoc. 1998;34:135–144. doi: 10.5326/15473317-34-2-135. [DOI] [PubMed] [Google Scholar]
- 6.Brisson BA, Holmberg DL, Parent J, Sears WC, Wick SE. Comparison of the effect of single-site and multiple-site disk fenestration on the rate of recurrence of thoracolumbar intervertebral disk herniation in dogs. J Am Vet Med Assoc. 2011;238:1593–1600. doi: 10.2460/javma.238.12.1593. [DOI] [PubMed] [Google Scholar]
- 7.Goggin JE, Li AS, Frante CE. Canine intervertebral disk disease: Characterization by age, sex, breed, and anatomic site of involvement. Am J Vet Res. 1970;31:1687–92. [PubMed] [Google Scholar]
- 8.Hansen H. A pathologic-anatomical study on disc degeneration in the dog. Acta Orthop Scand (Suppl) 1952;11:1–117. doi: 10.3109/ort.1952.23.suppl-11.01. [DOI] [PubMed] [Google Scholar]
- 9.Hoerlein BF. Comparative disc disease: Man and dog. J Am Anim Hosp Assoc. 1979;15:535–545. [Google Scholar]
- 10.Sharp N, Wheeler S. Small Animal Spinal Disorders: Diagnosis and Surgery. Philadelphia, Pennsylvania: Elsevier Mosby; 2005. Thoracolumbar disc disease; pp. 121–159. [Google Scholar]
- 11.Prata RG. Neurosurgical treatment of thoracolumbar disks: The rationale and value of laminectomy with concomitant disk removal. J Am Anim Hosp Assoc. 1981;17:17–26. [Google Scholar]
- 12.Coates JR, Hoffman AG, Dewey CW. Textbook of Small Animal Surgery. Philadelphia, Pennsylvania: Saunders; 2003. Surgical approaches to the central nervous system: Spine; pp. 1148–1163. [Google Scholar]
- 13.Gage ED, Hoerlein BF. Hemilaminectomy and dorsal laminectomy for relieving compressions of the spinal cord in the dog. J Am Vet Med Assoc. 1968;152:351–359. [PubMed] [Google Scholar]
- 14.Hoerlein BF. The treatment of intervertebral disc protrusions in the dog. Proceedings of the 89th Annual Meeting of the American Veterinary Medical Association; Atlantic City, New Jersey. June 23–26, 1952; p. 206. [Google Scholar]
- 15.Bitetto WV, Thacher C. A modified lateral decompressive technique for treatment of canine intervertebral disk disease. J Am Anim Hosp Assoc. 1987;23:409–413. [Google Scholar]
- 16.Black AP. Lateral spinal decompression in the dog: A review of 39 cases. J Small Anim Pract. 1988;29:581–588. [Google Scholar]
- 17.Braund KG, Taylor TKF, Ghosh P, Sherwood AA. Lateral spinal decompression in the dog. J Small Anim Pract. 1976;17:583–592. doi: 10.1111/j.1748-5827.1976.tb07005.x. [DOI] [PubMed] [Google Scholar]
- 18.Jeffery ND. Treatment of acute and chronic thoracolumbar disc disease by mini hemilaminectomy. J Small Anim Pract. 1988;29:611–616. [Google Scholar]
- 19.Yovich JC, Read R, Eger C. Modified lateral spinal decompression in 61 dogs with thoracolumbar disc protrusion. J Small Anim Pract. 1994;35:351–356. [Google Scholar]
- 20.Lubbe AM, Kirberger RM, Verstraete JM. Pediculectomy for thoracolumbar spinal decompression in the dachshund. J Am Anim Hosp Assoc. 1994;30:233–238. [Google Scholar]
- 21.McCartney W. Partial pediculectomy for the treatment of thoracolumbar disc disease. Vet Comp Orthop Traumatol. 1997;10:117–121. [Google Scholar]
- 22.Seim HB. Small Animal Surgery. St Louis, Missouri: Mosby Elsevier; 2007. Surgery of the Thoracolumbar Spine; pp. 1460–1492. [Google Scholar]
- 23.Eule JM, Breeze R, Kindt GW. Bilateral partial laminectomy: A treatment for lumbar spinal stenosis and midline disc herniation. Surg Neurol. 1999;52:329–338. doi: 10.1016/s0090-3019(99)00102-0. [DOI] [PubMed] [Google Scholar]
- 24.Thome C, Zevgaridis D, Leheta O, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: A randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3:129–141. doi: 10.3171/spi.2005.3.2.0129. [DOI] [PubMed] [Google Scholar]
- 25.Davis GJ, Brown DC. Prognostic indicators for time to ambulation after surgical decompression in non-ambulatory dogs with acute thoracolumbar disk extrusions: 112 cases. Vet Surg. 2002;31:513–518. doi: 10.1053/jvet.2002.36015. [DOI] [PubMed] [Google Scholar]
- 26.Ferreira AJA, Correia JHD, Jaggy A. Thoracolumbar disc disease in 71 paraplegic dogs: Influence of rate of onset and duration of clinical signs on treatment results. J Small Anim Pract. 2002;43:158–163. doi: 10.1111/j.1748-5827.2002.tb00049.x. [DOI] [PubMed] [Google Scholar]
- 27.Kazakos G, Polizopoulou ZS, Patsikas MN, Tsimopoulos G, Roubies N, Dessiris A. Duration and severity of clinical signs as prognostic indicators in 30 dogs with thoracolumbar disk disease after surgical decompression. J Vet Med Assoc. 2005;52:147–152. doi: 10.1111/j.1439-0442.2005.00698.x. [DOI] [PubMed] [Google Scholar]
- 28.Mayhew PD, McLear RC, Ziemer LS, et al. Risk factors for recurrence of clinical signs associated with thoracolumbar intervertebral disk herniation in dogs: 229 cases (1994–2000) J Am Vet Med Assoc. 2004;225:1231–1236. doi: 10.2460/javma.2004.225.1231. [DOI] [PubMed] [Google Scholar]
- 29.Muir P, Johnson K, Manley P, Dueland RT. Comparison of hemilaminectomy and dorsal laminectomy for thoracolumbar intervertebral disc extrusion in dachshunds. J Small Anim Pract. 1995;36:360–367. doi: 10.1111/j.1748-5827.1995.tb02950.x. [DOI] [PubMed] [Google Scholar]
- 30.Olby N, Harris T, Burr J, Muñana K, Sharp N, Keene B. Recovery of pelvic limb function in dogs following acute intervertebral disc herniation. J Neurotrauma. 2004;21:49–59. doi: 10.1089/089771504772695940. [DOI] [PubMed] [Google Scholar]
- 31.Doppman JL, Girton M. Angiographic study of the effect of laminectomy in the presence of acute anterior epidural masses. J Neurosurg. 1976;45:195–202. doi: 10.3171/jns.1976.45.2.0195. [DOI] [PubMed] [Google Scholar]
- 32.McKee WM. Comparison of hemilaminectomy (with concomitant disc fenestration) and dorsal laminectomy for the treatment of thoracolumbar disc protrusion in dogs. Vet Record. 1992;130:296–300. doi: 10.1136/vr.130.14.296. [DOI] [PubMed] [Google Scholar]
- 33.Moissonier P, Meheust P, Carozzo C. Thoracolumbar lateral corpectomy for treatment of chronic disk herniation: Technique description and use in 15 dogs. Vet Surg. 2004;33:620–628. doi: 10.1111/j.1532-950X.2004.04085.x. [DOI] [PubMed] [Google Scholar]
- 34.Hermantin FU, Peters T, Quartararo L, Kambin L. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdisectomy. J Bone Joint Surg Am. 1999;81:958–965. doi: 10.2106/00004623-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 35.da Costa RC, Pippi NL, Graça DL. The effects of free fat graft or cellulose membrane implants on laminectomy membrane formation in dogs. Vet J. 2006;171:491–499. doi: 10.1016/j.tvjl.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 36.Brown NO, Helphrey ML, Prata RG. Thoracolumbar disk disease in the dog: A retrospective analysis of 187 cases. J Am Anim Hosp Assoc. 1977;13:665–672. [Google Scholar]
- 37.Corse MR, Renberg WC, Friis EA. In vitro evaluation of biomechanical effects of multiple hemilaminectomies on the canine lumbar vertebral column. Am J Vet Res. 2003;64:1139–1145. doi: 10.2460/ajvr.2003.64.1139. [DOI] [PubMed] [Google Scholar]
- 38.Schulz KS, Waldron DR, Grant JW, Shell L, Smith G, Shires PK. Biomechanics of the thoracolumbar vertebral column of dogs during lateral bending. Am J Vet Res. 1996;57:1228–1232. [PubMed] [Google Scholar]
- 39.Shires PK, Waldron DR, Hedlund CS, et al. A biomechanical study of rotational instability in unaltered and surgically altered canine thoracolumbar vertebral motion units. Prog Vet Med. 1991;2:6–14. [Google Scholar]
- 40.Viguier E, Petit-Etienne G, Magnier J, Diop A, Lavaste F. Mobility of the T13-L1 after spinal cord decompression procedures in dogs (an in vitro study) Vet Surg. 2002;31:297. [Google Scholar]
- 41.Smith GK, Walter MC. Spinal decompressive procedures and dorsal compartment injuries: Comparative biomechanical study in canine cadavers. Am J Vet Res. 1988;49:266–273. [PubMed] [Google Scholar]
- 42.Cudia SP, Duval JM. Thoracolumbar intervertebral disk disease in large, nonchondrodystrophic dogs: A retrospective study. J Am Anim Hosp Assoc. 1997;33:456–460. doi: 10.5326/15473317-33-5-456. [DOI] [PubMed] [Google Scholar]
- 43.Olby NJ, Levine J, Harris T, Muñana K, Skeen T, Sharp N. Long-term functional outcome of dogs with severe injuries of the thoracolumbar spinal cord: 87 cases (1996–2001) J Am Vet Med Assoc. 2003;222:762–769. doi: 10.2460/javma.2003.222.762. [DOI] [PubMed] [Google Scholar]
- 44.Berthelot JM, Le Goff B, Maugars Y. The Hawthorne effect: Stronger than the placebo effect? Joint Bone Spine. 2011;78:335–336. doi: 10.1016/j.jbspin.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 45.Fernald DH, Coombs L, DeAlleaume L, West D, Parnes B. An assessment of the Hawthorne Effect in practice-based research. J Am Board Fam Med. 2012;25:83–86. doi: 10.3122/jabfm.2012.01.110019. [DOI] [PubMed] [Google Scholar]