Abstract
Background
Medical trainees infrequently use health literacy (HL) skills and overestimate their use of plain language and teach back skills. The aim of this study is to assess if level of training impacts the perception of medical trainees around HL knowledge and skills.
Methods
A structured questionnaire consisting of 5 questions assessing the respondents’ perception of their confidence in their HL knowledge, ability to identify and communicate with low HL patients, and use of relevant resources was completed by medical students and residents of 2 community-based internal medicine programs in Pennsylvania and Maryland between July 2012 and January 2013.
Results
The response rate was 100% (40) for the PA program and 42% (17) for the MD residency program. All rotating medical students (17) completed the questionnaire. Out of 74 participants, less than 10% were confident of their HL knowledge and ability to identify and communicate with low HL patients. Only 1.4% (1) were confident of their ability to identify appropriate resources. There was no significant difference in communication skills (P=0.305) and ability to identify appropriate resources (P=0.143) across all participants irrespective of their training level. A significant improvement in HL knowledge was observed during the progression from first-year to third-year medical school (P=0.0126) and from internship to second year of residency (P=0.0496).
Conclusion
Medical trainees perceive that they do not receive adequate training on HL knowledge and skills required to feel confident in identifying and communicating with low HL patients and identifying appropriate resources. There is a need for addressing these deficiencies via medical school and residency curricula.
Keywords: health literacy, patient–provider communication, medical education
Institute of Medicine defines health literacy (HL) as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions (1). Approximately 36% of Americans have low HL (2). These individuals are less likely to use preventive services, such as mammograms, pap smears, and flu shots, and more likely to visit emergency rooms and hospitals (3–6). These patients demonstrate poor knowledge and control of their chronic conditions such as asthma and diabetes (7–9).
An important factor mediating these patients’ inability to access care and poor health outcomes is patient–provider communication (10). These patients have difficulty reading health instructions and pamphlets, and hence, they depend heavily on their physicians for obtaining health information (11). They hide their limitation from their providers and their family members (10, 12). They ask fewer questions during medical encounters and do not engage actively in their care (13). Therefore, HL experts recommend the use of specific techniques that would allow identification of these patients and assessment of their understanding. In addition, they also provide guidelines on the type of resources that may be helpful for these patients to take care of their medical problems.
Studies have demonstrated that physicians including those in training have been found to overestimate the literacy level of their patients (14, 15). They are not adequately prepared to communicate with low HL patients when they are informed about the literacy levels of their patients (15). The communication techniques recommended for low HL patients are often overlooked during the patient–physician encounters (16, 17). An important contributor to this communication gap may be the training received by health care providers.
The accreditation bodies for medical schools in the United States, Liaison Committee on Medical Education (LCME) and US residency programs, and Accreditation Council for Graduate Medical Education (ACGME) require communication skills as a core requirement for medical training. The aim of this study is to assess if trainees’ perception of their HL knowledge or communication skills changes over the course of their medical training.
Methods
A structured questionnaire was distributed to all interns (categorical and transitional), second- and third-year residents of 2 community-based internal medicine (IM) residency program in Maryland (MD) and Pennsylvania (PA) during the period of July 2012 to Jan 2013. It was also distributed to first- and third-year medical students rotating through the MD program. In the PA program, 25% (2 out of 8) of the categorical interns and 100% of the transitional interns are US medical graduates. In the MD program, 18% of the categorical interns and 87.5% of the transitional interns are US medical graduates. Seventy-five percentage of residents in the PA program and 100% residents in the MD program are International Medical Graduates (IMG).
The survey provided a brief explanation of the purpose of the study. It consisted of 5 items that assessed participants’ perception of their knowledge pertaining to HL, teach back technique, methods to identify patients with low HL, strategies to communicate with low HL patients, and identifying appropriate resources for patients with low HL. The scores ranged from 1 to 4 with 1 for the perception of not being familiar, 2 for the perception of being familiar, 3 for perception of having receiving formal training, and 4 for perception of being confident around an area pertinent to HL knowledge and skills. The perception of formal training was the perception of the trainee. There was no objective documentation or verification of whether any formal training was provided or received by the trainee. Similarly, there was no objective assessment of the trainee's knowledge or skills pertaining to HL.
Data analysis was carried out via SOSS version 20.0. Descriptive statistics were used to estimate knowledge perceptions. Specifically, sample means are used to describe perceived knowledge parameters as ordinal quantitative variables, while frequencies and percents are used to describe the distributions categorically. Distributions were compared statistically using Fisher's exact tests, with significance taken at the 0.10 level due to the small sample sizes and limited power.
Results
All 40 interns and residents of the PA IM residency program participated. The response rate from interns and residents of the MD program was 41.5% (17). All rotating first- (8) and third-year medical students (7) participated.
First- and third-year medical students
Neither the first- nor the third-year medical students were confident about their HL knowledge or skills. About 12% of first-year medical students and 14% of third-year medical students reported receiving training on HL and teach back technique, respectively. No training in any other HL-related area was reported. Between 25% and 85% of first-year students reported unfamiliarity with HL knowledge or skills compared to 14–28% of third-year students.
Categorical and transitional interns
Around 14% of categorical interns expressed confidence in the areas of HL knowledge, identification, and communication with patients with low HL. Less than 10% reported receiving any training in teach back technique and communicating with low HL patients. Between 57% and 78% were unfamiliar with HL knowledge or skills.
The only area in which 6% of transitional interns felt confident was the teach back technique. Between 5% and 23% reported receiving training in HL knowledge and skills. The only area where no training was received was identification of patients with low HL. Between 23% and 71% reported unfamiliarity with HL knowledge or skills. The 2 areas where the transitional interns’ score were significantly better than the categorical interns were teach back technique (P=0.075) and identification of resources for low HL patients (P=0.020).
Second- and third-year residents
Less than 25% of second years and less than 10% of third years reported being confident in HL knowledge or skills. Less than 40% of second years and less than 30% of third years reported receiving training around HL knowledge and skills. Between 30% and 60% of second- and third-year residents reported unfamiliarity with HL knowledge and skills.
All medical trainees
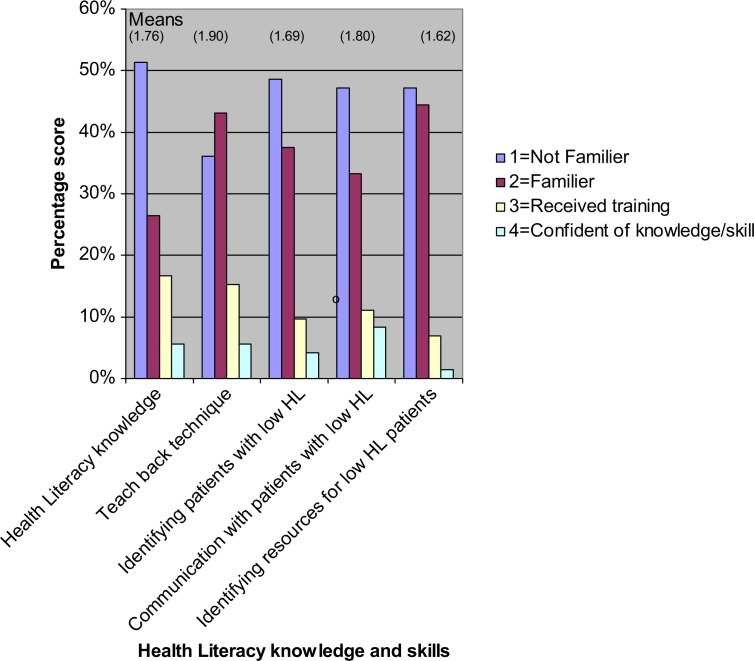
The overall scores indicated that less than 10% of participants felt confident about their HL knowledge or use of skills for identifying and communicating with low HL patients. Less than 20% of participants reported receiving any formal training in HL knowledge or HL specific communication skills. Between 36% and 51% of participants were unfamiliar with either HL knowledge or skills. The highest mean scores were in the areas of teach back technique (1.9) and HL knowledge (1.76), and the lowest mean score was in the area of identification of resources for low HL patients (Fig. 1).
Fig. 1.
This figure is a graphical representation of the scores obtained by all participants (medical students, interns, and residents irrespective of their level of training in the areas of health literacy (HL) knowledge, skills in identifying patients with low HL, and communicating and providing them with appropriate resources.
Knowledge of HL and the skill to identify patients with low HL consistently improved from first year of medical school to the second year of residency. There was no change in the knowledge or skills on progression from second to third year of residency (Table 1).
Table 1.
Comparison of scores of medical trainees at different levels of medical training for health literacy (HL) knowledge, skills pertaining to identifying low HL patients, and communicating and providing them with appropriate resources
| Knowledge and skills | First-year vs. third-year medical students | Third-year medical student vs. interns (transitionals and categoricals) | Interns (transitionals and categoricals) vs. second-year residents | Second-year vs. third-year residents |
|---|---|---|---|---|
| HL knowledge | 8.75 (P=0.01)* | 6.49 (P=0.09)* | 7.83 (P=0.04)* | 0.25 (P=0.97) |
| Teach back technique | 1.36 (P=0.50) | 2.84 (P=0.41) | 10.58 (P=0.01)* | 1.61 (P=0.66) |
| Identifying patients with low HL | 6.56 (P=0.01)* | 11.80 (P=0.002)* | 13.72 (P=0.003)* | 4.28 (P=0.23) |
| Communication with patients with low HL | 3.23 (P=0.07)* | 4.17 (P=0.24) | 3.19 (P=0.36) | 2.62 (P=0.45) |
| Identifying resources for low HL patients | 0.28 (P=0.60) | 4.42 (P=0.11) | 5.25 (P=0.15) | 2.69 (P=0.44) |
indicates a significant P value of ≤=0.05.
Discussion
To our knowledge this is the first study that focused on the impact of medical training on the perception of trainees regarding acquisition of HL knowledge and skills. The study clearly indicates that a large number of medical trainees are unfamiliar with HL and communication skills required for effective interaction with low HL patients at all levels of training from med school through residency. These numbers are not very different from that of a recent study that was conducted in a university setting where over 65% of the residents reported receiving no training or very little training in physician–patient communication, including HL skills such as using simple language (18). These findings underscore the need for more effective teaching of HL and communication skills at all levels. The inability of medical trainees to have the knowledge and skills to communicate with 90 million US adults with low HL impacts the quality, safety, and cost of healthcare.
It was interesting to note there is wide variation in terms of the HL areas that trainees are familiar with or have reported receiving training within and across the different training levels. These differences can be explained by the heterogeneity that exists among residency programs and medical schools with regards to HL content being taught. A survey of US medical schools by Coleman and Appy found that around 70% of US allopathic schools report teaching HL to medical students (19). However, there was considerable variation among medical schools in terms of the time allocated and the teaching and evaluation techniques being used (19). A survey of community-based IM residency programs by Ali found that less than 50% of these programs provided any kind of teaching around HL to their residents (20). They reported that their programs lacked resources needed for incorporating HL in their core curriculum such as access to an HL curriculum, faculty development around teaching and evaluating HL, and availability of materials to teach HL.
The ACGME identifies 6 core competencies that are required to be taught and evaluated by training programs, including interpersonal and communication skills. The new accreditation system (NAS) has outlined 3 specific milestones within each competency that need to be obtained by trainees as they progress from one level to another. No milestones addressing the acquisition of communication skills required for low HL patients have been included. This is an important step required for drawing the attention of program directors toward a potential area of need.
An important finding was the significant difference between the scores of transitional and categorical interns in areas of teach back and identification of resources for low HL patients. There can be a couple of reasons for this difference. The first could be that the majority of the categorical residents are IMGs who may not have received training around HL. Identification of resources requires an understanding of the health system, and the IMGs are not familiar with the US health system and its resources. This study highlights the knowledge gaps among IMGs that need to be addressed early on to improve patient care and communication.
Limitations
Our study has several limitations. First is the small sample size, which makes it difficult to draw absolute conclusions. The study however provides an opportunity to trend the perception of medical trainees at all levels in community-based residency programs regarding adequacy of their training around HL and their confidence in dealing with low HL patients. The second limitation is that the study did not objectively assess the knowledge and skills of the medical trainees to verify their use of HL knowledge and skills in the clinical setting. Third, the cross-sectional nature of the study lends itself to recall bias and trainees may not recall the training that they may have received at some point in time. This may particularly be true if the teaching was provided in an informal or indirect manner rather than a didactic format.
Conclusion
Our study suggests the need for training the medical students and residents in the acquisition and application of HL knowledge and skills. This will require an effort on the part of the accreditation organizations to provide better guidance and support around HL curriculum and faculty development as well as outlining measurable milestones for achieving competence in HL skills. It will also require medical schools and residency programs to identify the needs of their trainees around patient–provider communication and take appropriate steps to address them.
References
- 1.Institute of Medicine. Health literacy: A prescription to end confusion. April 8th 2004. Available from: http://www.nap.edu/openbook.php?isbn=0309091179 [cited 16 May 2013]
- 2.Institute of Education Sciences, National Center for Education Statistics. National Assessment of Adult Literacy (NAAL) 2003. Available from: http://nces.ed.gov/naal/ [cited 16 May 2013]
- 3.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40(5):395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Baker DW, Parker RM, Williams MV, Clark WS. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87(6):1027–30. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13(12):791–8. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92(8):1278–83. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114(4):1008–15. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 8.Williams MV, Baker DW, Parker RM, Nurse JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 9.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. J Am Med Assoc. 2002;288(4):475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 10.Baker DW, Parker RM, Williams MV, Pitkin K, Parikh NS, Coates W, et al. The health care experience of patients with low literacy. Arch Fam Med. 1996;5(6):329–34. doi: 10.1001/archfami.5.6.329. [DOI] [PubMed] [Google Scholar]
- 11.White SP. Chicago, IL: American Medical Association Foundation; 2008. Assessing the nation's health literacy; key concepts and findings of the National Assessment of Adult Literacy (NAAL) [Google Scholar]
- 12.Parikh NS, Parker RM, Nurse JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient Educ Couns. 1996;27(1):33–9. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- 13.Katz MG, Jacobson TA, Veledar E, Kripalani S. Patient literacy and question-asking behavior during the medical encounter: A mixed-methods analysis. J Gen Intern Med. 2007;22(6):782–6. doi: 10.1007/s11606-007-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bass PF, Wilson JF, Griffith CH, Barnett DR. Residents’ ability to identify patients with poor literacy skills. Acad Med. 2002;77(10):1039–41. doi: 10.1097/00001888-200210000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Seligman HK, Wang FF, Palacios JL, Wilson CC, Daher C, Piette JD, et al. Physician notification of their diabetes patients’ limited health literacy. A randomized, controlled trial. J Gen Intern Med. 2005;20(11):1001–7. doi: 10.1111/j.1525-1497.2005.00189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: Physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 17.Schwartzberg JG, Cowett A, VanGeest J, Wolf MS. Communication techniques for patients with low health literacy: A survey of physicians, nurses, and pharmacists. Am J Health Behav. 2007;31(Suppl 1):S96–104. doi: 10.5555/ajhb.2007.31.supp.S96. [DOI] [PubMed] [Google Scholar]
- 18.Howard T, Jacobson KL, Kripalani S. Doctor talk: Physicians’ use of clear verbal communication. J Health Commun. 2013;18(8):991–1001. doi: 10.1080/10810730.2012.757398. [DOI] [PubMed] [Google Scholar]
- 19.Coleman CA, Appy S. Health literacy teaching in US medical schools, 2010. Fam Med. 2012;44(7):504–7. [PubMed] [Google Scholar]
- 20.Ali NK. Are we training residents to communicate with low health patients? J Community Hosp Intern Med Perspect. 2012;2:19238. doi: 10.3402/jchimp.v2i4.19238. [DOI] [PMC free article] [PubMed] [Google Scholar]