Description
A 40-year-old woman presented with altered bowel movements, 10-pound weight loss and abdominal discomfort for 1 month. Prior to this, she had been on a week-long trip to Mexico. The patient’s complete metabolic profile, complete blood count, serum amylase and lipase, urine analysis and culture and stool studies for white cell count, ova, parasite and culture were all either in the reference range or negative. An ultrasonography of the abdomen was normal. An axial CT scan of the abdomen with oral and intravenous radiocontrast material showed multiple tubular filling defects about 15 cm in length predominantly located in the jejunal lumen (figures 1–3), highly suggestive of intestinal parasites. She was treated with a dose of oral albendazole 400 mg. After 1 week, her symptoms improved and she reported passage of 15–20 cm long cream coloured cylindrical worms in her stool.
Figure 1.
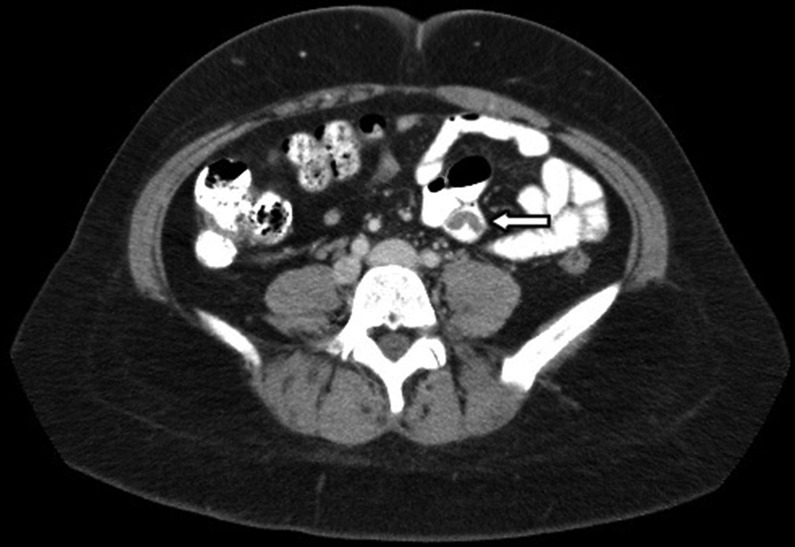
Axial section of contrast CT of the abdomen showing tubular filling defects in the jejunal lumen.
Figure 2.

Coronal section of contrast CT of the abdomen showing tubular filling defects about 15 cm or more in length in the jejunal lumen.
Figure 3.
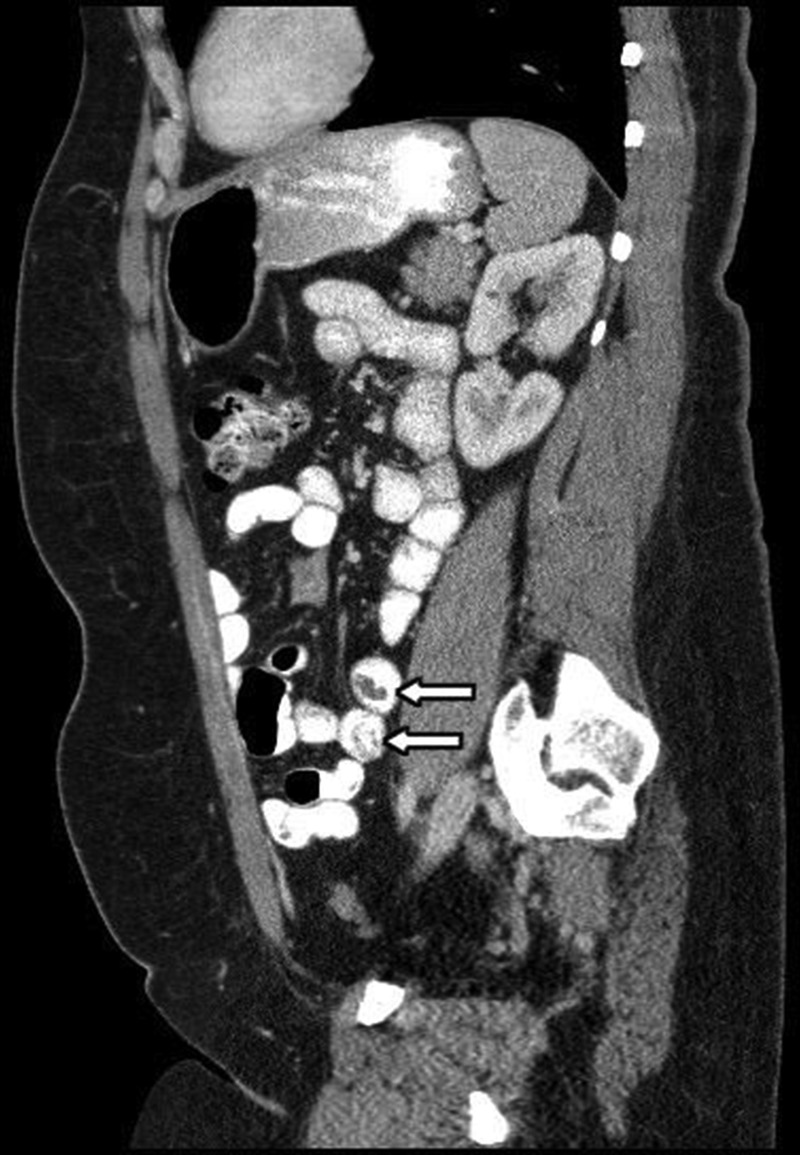
Sagittal section of contrast CT of the abdomen showing tubular filling defects in jejunum.
Ascariasis is caused by the parasitic roundworm, Ascaris lumbricoides and is uncommon in developed countries. Most patients are asymptomatic, hence it can be undetected for years until they develop some symptoms.1 2 Diagnosis is usually made through a combination of blood counts showing marked leucocytosis with eosinophilia, stool studies and radiographic imaging. Complications can range from nutritional deficiency to obstruction of the bowel lumen, the bile or pancreatic duct, perforation, volvulus, intussusception, appendicitis, cholecystitis, biliary colic, cholangitis, hepatic abscess and pancreatitis depending on the site and severity of infestation.1 3 Antihelminthic therapy is usually sufficient except in few cases where surgical interventions might be needed.4
Learning points.
Intestinal ascariasis can present with non-specific symptoms and signs.
Diagnosis requires high index of suspicion and can be usually made through a combination of blood counts showing marked leucocytosis with eosinophilia, stool studies and radiographic imaging.
Antihelminthic therapy is usually sufficient except in few cases where surgical interventions might be needed.
Footnotes
Contributors: SR wrote the initial manuscript and got the patient consent. PK and MRA edited the final manuscript and the images.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kanneganti K, Makker JS, Remy P. Ascaris lumbricoides: to expect the unexpected during a routine colonoscopy. Case Reports Med 2013;2013:579464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suzuki A, Yabushita Y, Takahashi H, et al. Gastrointestinal: ascariasis. J Gastroenterol Hepatol 2008;23:1770. [DOI] [PubMed] [Google Scholar]
- 3.Zheng P-P, Wang B-Y, Wang F, et al. Esophageal space-occupying lesion caused by Ascaris lumbricoides. World J Gastroenterol 2012;18:1552–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tay K-V, Teo J-Y. Education and imaging. Gastrointestinal: incidental findings of Ascaris lumbricoides in patient presenting with ureteric colic. J Gastroenterol Hepatol 2012;27:1127. [DOI] [PubMed] [Google Scholar]


