Abstract
An enlarged peroneal tubercle can cause a peroneal tendon tear and/or tenosynovitis due to chronic friction. We present the case of a 45-year-old man with tenosynovitis in the peroneus longus and brevis tendons associated with a hypertrophic peroneal tubercle. On admission to our facility, the patient presented with pain while walking and had a fixed mass on the lateral aspect of his right foot. In addition, an osseous prominence corresponding to a hypertrophic peroneal tubercle was seen on the lateral side of the right calcaneus on radiography. MRI confirmed the hypertrophic peroneal tubercle and revealed high-signal intensity within the peroneus longus and brevis tendons along with fluid in their sheaths.
Background
There are two protuberances on the lateral wall of the calcaneus: the peroneal tubercle and the retrotrochlear eminence.1 The peroneal tubercle separates the peroneus longus and brevis tendons, both of which are covered by the inferior peroneal retinaculum. The inferior peroneal retinaculum is located inferoposteriorly to the peroneal tubercle on the retrotrochlear eminence.2 3 If the peroneal tubercle is enlarged, it can cause tenosynovitis and/or tear of the peroneal tendons due to chronic friction and increased tension on the peroneus longus tendon.4
Case presentation
A 45-year-old male patient with right ankle pain and a fixed mass on the lateral aspect of his right foot was referred to the orthopaedics department at our institution. The patient's pain increased while walking and tenderness in the area was observed on evaluation. He had a recent history of excessive sports activities. Anterior talofibular ligament (ATFL) injury and synovitis were considered clinically at the initial presentation.
Investigations
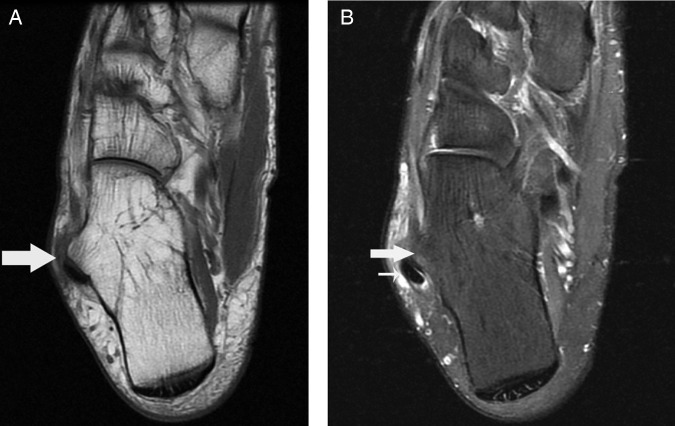
Ankle radiography in anteroposterior view showed an osseous prominence corresponding to the hypertrophic peroneal tubercle on the lateral wall of the calcaneus (figure 1). Axial T1-weighted (figure 2A) and fat-saturated protondensity (figure 2B) images verified the presence of the hypertrophic peroneal tubercle, which measured 10 mm in width. In addition, coronal fat-saturated proton density imaging also showed high-signal intensity within the peroneus longus tendon, fluid within the sheath of the peroneal tendons and oedema in the surrounding soft tissue (figure 3). Furthermore, there was evidence of bone marrow oedema involving the peroneal tubercle (figure 3). However, no adventitial bursitis or thickening of the inferior peroneal retinaculum was detected via MRI.
Figure 1.

Radiograph showing an osseous prominence on the lateral wall of the calcaneus (arrow).
Figure 2.
Axial T1-weighted MRI (A) revealing the hypertrophic peroneal tubercle (thick arrow). Axial fat-saturated proton density MRI (B) indicating high-signal intensity within the peroneus longus tendon (thin arrow) along with soft tissue oedema.
Figure 3.

Coronal fat-saturated proton density MRI showing the hypertrophic peroneal tubercle with bone marrow oedema (arrowhead) and intratendinous high-signal intensity of the peroneus longus (long arrow) and peroneus brevis (short arrow) tendons.
Differential diagnosis
In a differential diagnosis of lateral ankle pain lateral ankle ligament injury, the peroneal tendon subluxation/dislocation and talar osteochondral lesions should be considered.
Discussion
Detailed anatomical descriptions of the peroneal tubercle were performed by Laidlaw5 and Edwards6 early in the 20th century. In the literature, the prevalence of peroneal tubercles, first reported by Burman,7 ranges from 24% to 98.58%.5–8 This wide variance can be attributed to the use of different criteria in the description of the peroneal tubercle. Additionally, there are also different reports regarding the size of peroneal tubercles in the literature. Hyer et al8 reported that the mean length, height and width of the peroneal tubercle in adults was 13.04, 9.44 and 3.13 mm, respectively. They also noted that the prominent peroneal tubercle, a local, nodular tuberosity on the lateral wall, was observed in 30% of the cases in their report. In actuality, there is no precise size criteria for hypertrophic peroneal tubercles, but a cut-off point of 5 mm in width can be used for diagnosis.9
The aetiology of hypertrophic peroneal tubercles is varied. Most enlargements are believed to be congenital in nature, but some are acquired via previous trauma, altered weight bearing and/or inflammatory diseases related to peroneus longus tendon spasms.2 10 Symptoms first occur when the hypertrophic peroneal tubercle causes chronic irritation of the tendons and tendon sheath, with the peroneus longus tendon being more vulnerable to damage than the peroneus brevis tendon because of its length, acute change of direction and posterior location to the peroneal tubercle.11 Furthermore, irritation of the tendons due to an enlarged peroneal tubercle may lead to tenosynovitis and/or tear. It is also possible that an adventitial bursa can develop over the peroneal tubercle. A recent study by Saupe et al12 identified the presence of a peroneal tubercle in 55% of their study population. Despite the relative frequency of enlarged peroneal tubercles, it is still not obvious why symptoms associated with this condition occur in some patients.13 One possibility is that they could be related to the size of the peroneal tubercle or recent intensified activity, as with our case.
A peroneal tubercle may be identified via a Harris (axial) view of the calcaneus or anteroposterior ankle radiographs while the size of the peroneal tubercle can be evaluated by multidetector CT and three-dimensional volume rendering.13 However, none of these imaging techniques are sufficient to evaluate the pathologies associated with a hypertrophic peroneal tubercle, such as thickening of the inferior peroneal retinaculum, peroneal tenosynovitis, rupture of the peroneal tendons or an adventitial bursa over the tubercle. Tenography can also be helpful to assess patients with stenosing tenosynovitis or peroneal tendon dislocation.14 Furthermore, ultrasound and MRI are useful diagnostic tools for the evaluation of coexisting peroneal tendon pathologies and differential diagnoses.15 16
Initial treatment is usually conservative, but resection of the hypertrophic tubercle may be necessary if no improvement is seen.13
Learning point.
Physicians and radiologists should be aware of the possibility of a hypertrophic peroneal tubercle in the calcaneus. Furthermore, an enlarged peroneal tubercle can result in lateral ankle pain caused by peroneal tenosynovitis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wang XT, Rosenberg ZS, Mechlin MB, et al. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics 2005;25:587–602 [DOI] [PubMed] [Google Scholar]
- 2.Boles MA, Lomasney LM, Demos TC, et al. Enlarged peroneal process with peroneus longus tendon entrapment. Skeletal Radiol 1997;26:313–15 [DOI] [PubMed] [Google Scholar]
- 3.Numkarunarunrote N, Malik A, Aguiar RO, et al. Retinacula of the foot and ankle: MRI with anatomic correlation in cadavers. AJR Am J Roentgenol 2007;188:W348–54 [DOI] [PubMed] [Google Scholar]
- 4.Bruce WD, Christofersen MR, Phillips DL. Stenosing peroneal tenosynovitis associated with hypertrophy of the peroneal tubercle. Hong Kong J Radiol 2012;15:252–5 [Google Scholar]
- 5.Laidlaw PP. The varieties of the os calcis. J Anat Physiol 1904;38:133–43 [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards ME. The relations of the peroneal tendons to the fibula, calcaneus, and cuboideum. Am J Anat 1928;42:213–53 [Google Scholar]
- 7.Burman M. Subcutaneous tear of the tendon of the peroneus longus; its relation to the giant peroneal tubercle. AMA Arch Surg 1956;73:216–19 [DOI] [PubMed] [Google Scholar]
- 8.Hyer CF, Dawson JM, Philbin TM, et al. The peroneal tubercle: description, classification, and relevance to peroneus longus tendon pathology. Foot Ankle Int 2005;26:947–50 [DOI] [PubMed] [Google Scholar]
- 9.Zanetti M. Founder's lecture of the ISS 2006: borderlands of normal and early pathological findings in MRI of the foot and ankle. Skeletal Radiol 2008;37:875–84 [DOI] [PubMed] [Google Scholar]
- 10.Bruce WD, Christofersen MR, Phillips DL. Stenosing tenosynovitis and impingement of the peroneal tendons associated with hypertrophy of peroneal tubercle. Foot Ankle Int 1999;20:464–7 [DOI] [PubMed] [Google Scholar]
- 11.Sugimoto K, Takakura Y, Okahashi K, et al. Enlarged peroneal tubercle with peroneus longus tenosynovitis. J Orthop Sci 2009;14:330–5 [DOI] [PubMed] [Google Scholar]
- 12.Saupe N, et al. Anatomic variants associated with peroneal tendon disorders: MR imaging findings in volunteers with asymptomatic ankles. Radiology 2007;242:509–17 [DOI] [PubMed] [Google Scholar]
- 13.Dutton P, Edmonds EW, Lark RK, et al. Prevalence of painful peroneal tubercles in the pediatric population. J Foot Ankle Surg 2012;51:599–603 [DOI] [PubMed] [Google Scholar]
- 14.Berquist TH. Imaging of the foot and ankle. 3rd edn Philadelphia, PA: Lippincott Williams & Wilkins; 2011:133 [Google Scholar]
- 15.Lee SJ, Jacobson JA, Kim SM, et al. Ultrasound and MRI of the peroneal tendons and associated pathology. Skeletal Radiol 2013;42:1191–200 [DOI] [PubMed] [Google Scholar]
- 16.Schubert R. MRI of peroneal tendinopathies resulting from trauma or overuse. Br J Radiol 2013;86:1021. [DOI] [PMC free article] [PubMed] [Google Scholar]