Abstract
Lumbar hernia is one of the rare cases that most surgeons are not exposed to. Hence the diagnosis can be easily missed. This leads to delay in the treatment causing increased morbidity. We report a case of lumbar hernia in a middle-aged woman. It was misdiagnosed as lipoma by another surgeon. It was a case of primary acquired lumbar hernia in the superior lumbar triangle. Clinical and MRI findings were correlated to reach the diagnosis. We also highlight the types, the process of diagnosis and the surgical repair of lumbar hernias. We wish to alert our fellow surgeons to keep the differential diagnosis of the lumbar hernia in mind before diagnosing any lumbar swelling as lipoma.
Background
Lumbar hernia is one of the rare cases reported in the literature. It is not commonly seen by surgeons hence when a patient presents with a lumbar hernia, it is commonly misdiagnosed as lipoma, fibroma, muscle strain, etc.
We report a case of primary acquired lumbar hernia in a female patient (stated in the literature to be more common in men than in women). It was on the right side in the superior lumbar triangle of Grynfeltt-lesshaft (stated in the literature to be more common on the left side and in the inferior lumbar triangle of petit).
It was misdiagnosed as lipoma by another surgeon. It is an extremely rare case with only 300 cases reported in history.1
Case presentation
A 45-year-old woman presented with a vague lumbar pain and a mass in the right lumbar region (figures 1–3). She had been diagnosed as having lipoma and was recommended excision by a local medical practitioner. There was no history of trauma. The mass was 4×5 cm in size and was located just below the right 12th rib tip. It was globular in shape, soft in consistency with smooth surface and well-defined borders. It was expansile on coughing and straining. No pulsations were felt over the swelling.
Figure 1.
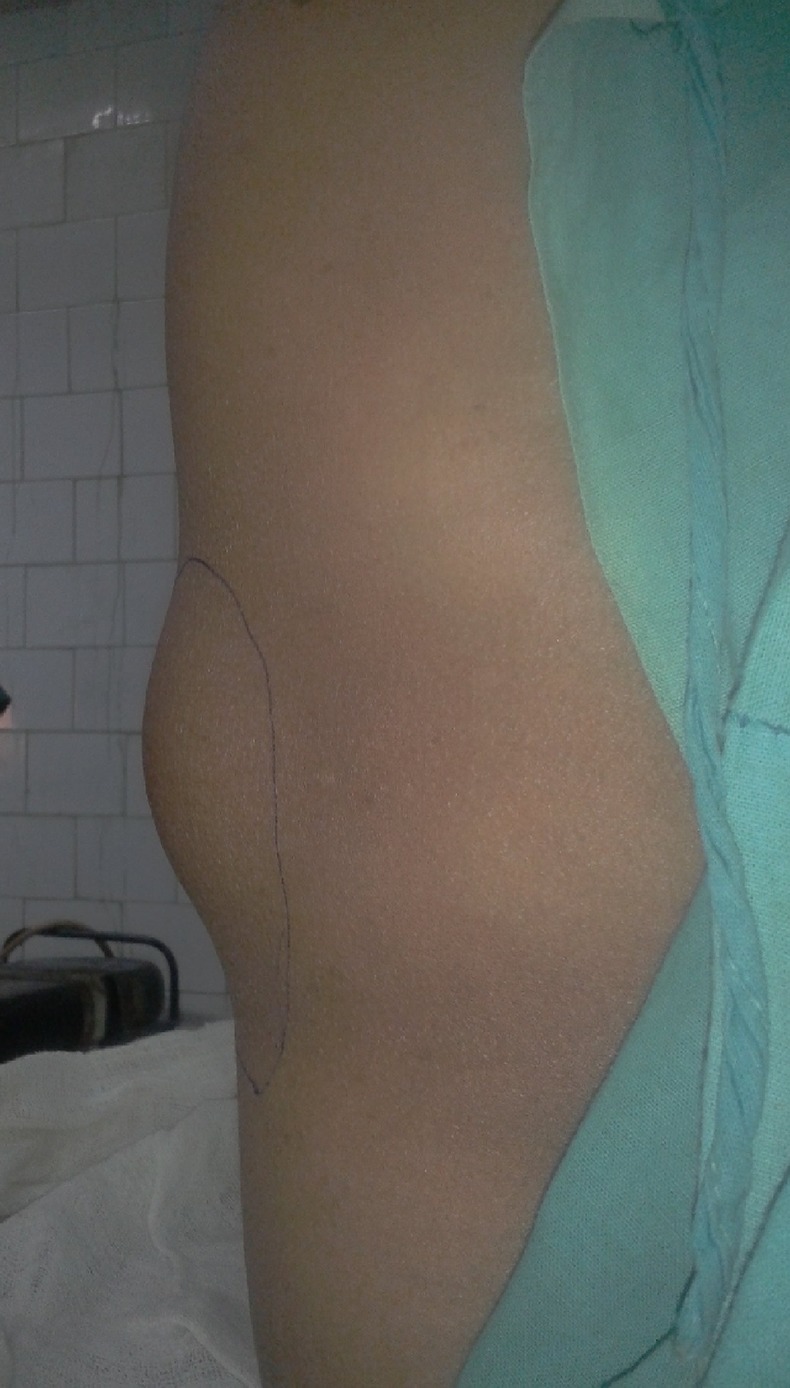
Lumbar hernia lateral view.
Figure 2.

Lumbar hernia becoming more prominent after sitting.
Figure 3.

Lumbar hernia posterior view.
Investigations
Routine investigations were normal. MRI showed defect in the lumbar fascia with the protrusion of the abdominal content through the defect (figure 4). Provisional diagnosis of superior lumbar hernia was given.
Figure 4.
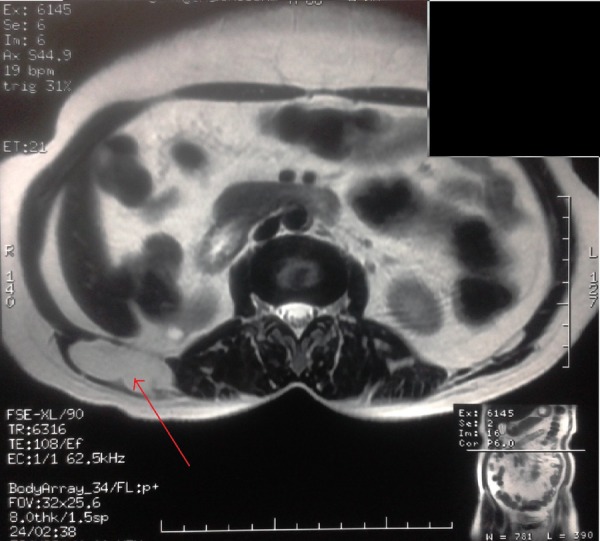
MRI showing the hernia content.
Differential diagnosis
The various differential diagnoses that were excluded were lipomas, haematomas, fibromas, abscesses and kidney tumours. Expansile cough impulse confirmed our diagnosis of lumbar hernia.
Treatment
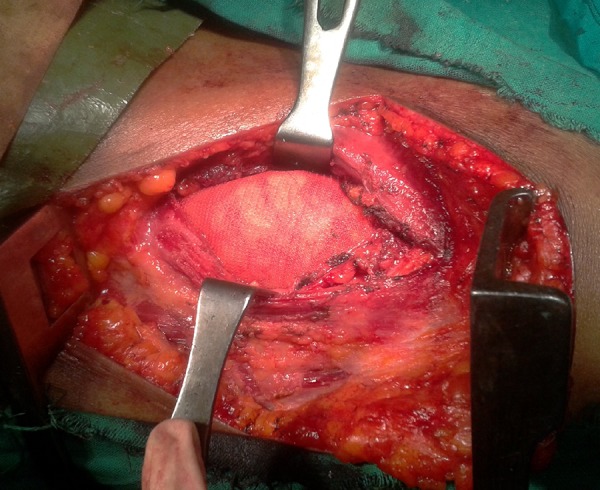
The patient was explored in the modified left lateral position. A wide incision was given and the sac delineated (figure 5). The defect was bounded anteriorly by latissimus dorsi muscle, posteriorly by quadrates lumborum and erector spinae and superiorly by the lower end of 12th rib. A space was created between the peritoneum and the muscle layer all around and a 15×15 cm nylon mesh was placed (figure 6). It was fixed to the muscle layer with interrupted sutures. Postoperative recovery was uneventful.
Figure 5.

The hernial defect with the hernia sac exposed intraoperatively.
Figure 6.
The exposed hernia defect with the mesh placed.
Outcome and follow-up
The patient attended the outdoor department for follow-up at 2 weeks, 1 month, 3 months and 6 months after the operation. The patient has been asymptomatic. There has been no recurrence in the past 6 months since the operation. The patient is expected to attend the outdoor department yearly from now on for follow-up.
Discussion
Lumbar hernia is a form of flank hernia. Flank hernia is defined as any hernia from the anterior axillary line to spine and from costal margin to ischial tuberosity. It is of two types: superior lumbar hernia and inferior lumbar hernia according to the anatomical location of the defect, that is, either through the superior or the inferior lumbar triangle.
The superior lumbar triangle of Grynfeltt-lesshaft is bounded anteriorly by the latissimus dorsi muscle, posteriorly by the quadrates lumborum and erector spinae muscles and superiorly by the 12th rib and serratus posterior inferior muscle.
The inferior lumbar triangle of petit is bounded anteriorly by the external oblique muscle, posteriorly by the latissimus dorsi muscle and inferiorly by the iliac crest.2
Depending on the aetiology, it is classified into two types: congenital (20%) and acquired (80%). Congenital lumbar hernias are found in infants and are caused due to musculoskeletal defect. Acquired lumbar hernias can be of two types: primary (55%) with no known cause and secondary (25%) which are found after trauma, iliac crest graft, infection, etc.3
A lumbar hernia is difficult to diagnose as the patient is either asymptomatic or presents with non-specific symptoms. Clinical feature of a lumbar hernia is usually dull aching pain over an increasing size of lumbar mass. The lumbar mass becomes more prominent on straining and coughing and reduces in size in prone position. Expansile cough impulse is positive in a minority of patients (as found in our case).1 3 Diagnosis of these hernias may be missed as these are very rare cases.
Lumbar hernias have to be differentiated from lipomas, haematomas, fibromas, abscesses and kidney tumours. Lipomas are usually soft mobile masses which are not attached to the muscle layer. Fibromas are firm masses attached to fascia or muscle. Haematomas present with a history of trauma and local ecchymosis. Abscesses present with pain, oedema, cellulitis, fever and leucocytosis. Kidney tumours are non-painful, firm to hard in consistency, dull on percussion and may be associated with haematuria. None of these differential diagnoses increase in size on straining or decrease in size in prone position. Expansile cough impulse is absent in all of them unlike a lumbar hernia.
A lumbar hernia though rarely may also become incarcerated and strangulated. The most important differential diagnosis of strangulated lumbar hernia is haematoma found in the flanks after trauma. In a case of strangulated lumbar hernia there is bowel obstruction which is not found in haematomas.1
CT scan or MRI may be performed to confirm the diagnosis.4 Both can show the defect in the musculofascial layer, the content of the hernia and help us to plan the repair. They can also rule out the other differential diagnoses of lumbar hernia.
These hernias should not be managed conservatively without surgery for two reasons. First, around 25%of these hernias are prone to incarceration and 10% to strangulation which may present with features of acute abdomen and need emergency surgery.5 Second, these hernias tend to increase in size with time. Surgical repair of a large lumbar hernia is difficult. Hence surgical repair without delay is the treatment of choice.1 6
Surgical treatment is either open or laparoscopic with equivalent success.7 8 In the open anterior approach the patient is positioned in the lateral decubitus position, the hernia is explored and the defect identified. The sac is isolated. The sac may then be excised or simply inverted. If the defect is small, simple darning may be done to strengthen the wall. If the defect is large then a large non-absorbable mesh may be put in the extraperitoneal space between the peritoneum and the muscle layer. It is fixed to the muscle layer with interrupted non-absorbable suture.2 9 This sub-lay mesh technique can be either routine or extended (significantly larger mesh size) with extended sub-lay technique recommended to decrease the chance of recurrence.10
Recently laparoscopic repair of these hernias has also been successfully attempted. There are two laparoscopic approaches: transabdominal and extraperitoneal. In the transabdominal approach, pneumoperitoneum is created and the peritoneal reflection along the white line of Toldt is opened to mobilise the colon. The borders of the lumbar hernia defect are defined and an extraperitoneal mesh is placed. Mesh fixation is performed by a combination of transabdominal stitches and metallic tacks.11
In total extraperitoneal repair, a small incision is made over the hernia defect. The retroperitoneal fat is detached with blunt dissection by an index finger. The space is expanded by a balloon dissector. The incision is plugged and pneumoperitoneum created. With the help of one 30° 5 mm scope and two 5 mm working ports retroperitoneal fat and structures are detached from the hernia defect. A polypropylene mesh is introduced and secured in place with tackers.12
The laparoscopic repair and classical open repair have their own advantages and disadvantages. The main advantage of the laparoscopic approach is that it helps the surgeon to precisely locate and evaluate the characteristics of the defect.13 It also has a lower morbidity rate, shorter length of hospital stay, lower postoperative pain and an earlier return to daily routine activities.11 The disadvantages of laparoscopic repair of lumbar hernia are threefold. First, the laparoscopic approach does not allow for parietal reconstruction or repair to be done under controlled tension. For an adequate aesthetic and functional result, repair should be done under a certain degree of tension.1 Second, laparoscopic repair of lumbar hernia is a technically challenging job and requires a senior surgeon specialised in laparoscopic hernia repair.11 13 Third, laparoscopic repair may be difficult for incisional lumbar hernias as in these hernias the defects are very large and occupy most of the lumbar region.11 14
Recurrences are known with laparoscopic and open surgical repair. Patients with high risk of recurrence are those with diffuse lumbar hernias, hernias greater than 16 cm in size and hernias associated with muscular atrophy.11 Hence the choice of the technique of surgical repair depends on the patient factors and the expertise of the surgeon.
Learning points.
Lumbar hernia can create diagnostic dilemma with lipoma being the most common differential diagnosis.
Treatment should not be delayed as the lumbar hernia becomes more difficult to repair as it increases in size.
As much as one of four cases of lumbar hernia is prone to incarcerate and present as acute abdomen. Hence emergency surgeons should keep strangulated lumbar hernia in differential diagnosis of any acute abdomen and a lumbar mass.
Diagnosis of a simple lumbar hernia is mostly clinical which can be confirmed with either a CT scan or MRI which shows a defect in the fascia.
Treatment is surgical with the use of a large mesh in the preperitoneal space either through the open or laparoscopic approach.
Footnotes
Contributors: All the authors had substantial contributions to the conception and drafting of the paper and were actively involved in critically revising it; and the final version of the paper was approved.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Moreno-Egea A, Baena EG, Calle MC, et al. Controversies in the current management of lumbar hernias. Arch Surg 2007;142:82–8 [DOI] [PubMed] [Google Scholar]
- 2.Javid PJ, Brooks DC. Hernias. In: Zinner MJ, Ashley SW. eds. Maingot's abdominal operations. 11th edn The McGraw-Hill Companies; 1997:163–4 [Google Scholar]
- 3.Lillie GR, Deppert E. Inferior lumbar triangle hernia as a rarely reported cause of low back pain: a report of 4 cases. J Chiropr Med 2010;9:73–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanker B, Chernyavsky VC, Johnson K, et al. Repair of a traumatic lumbar hernia with biosynthetic mesh: a novel approach and review of the literature. J Curr Surg 2012;2:105–9 [Google Scholar]
- 5.Killeen KL, Girard S, DeMeo JH, et al. Using CT to diagnose traumatic lumbar hernia. AJR Am J Roentgenol 2000;174:1413–15 [DOI] [PubMed] [Google Scholar]
- 6.Esposito C, Settimi A, de Marco M, et al. Congenital lumbar hernia: two case reports and a review of the literature. J Paediatr Surg Spec 2009; 3:40–2 [Google Scholar]
- 7.Parihar S, Bali G, Sharma S, et al. Congenital lumbar hernia. JK Sci 2008;10:144–5 [Google Scholar]
- 8.Mingolla GP, Amelio G. Lumbar hernia misdiagnosed as a subcutaneous lipoma: a case report. J Med Case Rep 2009;103:9322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mismar A, Al-Ardah M, Albsoul N, et al. Underlay mesh repair for spontaneous lumbar hernia. Int J Surg Case Rep 2013;4:534–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fei Y, Li L. [Comparison of two repairing procedures for abdominal wall reconstruction in patients with flank hernia]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2010;24:1506–9 [PubMed] [Google Scholar]
- 11.Moreno-Egea A, Alcaraz AC, Cuervo MC. Surgical options in lumbar hernia: laparoscopic versus open repair. A long-term prospective study. Surg Innov 2013; 20:331–44 [DOI] [PubMed] [Google Scholar]
- 12.Lim MS, Lee HW, Yu CH, et al. Laparoscopic total extraperitoneal repair of lumbar hernia. J Korean Surg Soc 2011;81:287–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yavuz N, Ersoy YE, Demirkesen O, et al. Laparoscopic incisional lumbar hernia repair. Hernia 2009;13:281–6 [DOI] [PubMed] [Google Scholar]
- 14.Suarez S, Hernandez JD. Laparoscopic repair of a lumbar hernia: report of a case and extensive review of the literature. Surg Endosc 2013;27:3421–9 [DOI] [PubMed] [Google Scholar]


