Abstract
Background
Although CT can be greatly beneficial, its relatively high radiation doses have caused public health concerns.
Objective
To assess patterns in CT usage among patients aged less than 22 years in Northern England during the period 1993–2002.
Materials and methods
Electronic data were obtained from radiology information systems of all nine National Health Service trusts in the region.
Results
A total of 38,681 scans had been performed in 20,483 patients aged less than 22 years. The number of CT examinations rose, with the steepest increase between 1997 and 2000. The number of patients scanned per year increased less dramatically, with 2.24/1,000 population aged less than 22 years having one scan or more in 1993 compared to 3.54/1,000 in 2002. This reflects an increase in the median number of scans per patient, which rose from 1 in 1993 to 2 by 1999. More than 70% of CT examinations were of the head, with the number of head examinations varying with time and patient age.
Conclusion
The frequency of CT scans in this population more than doubled during the study period. This is partly, but not wholly, explained by an increase in the number of scans per patient.
Keywords: Radiation dose, Computed tomography, Trends, Child
Introduction
CT is an indispensable, sometimes life-saving, diagnostic tool with increasing clinical application. In the United Kingdom, the number of CT scans increased by 39% between 1997/1998 and 2001/2002, whereas the number of conventional radiographic examinations increased by only 1% in the same period [1]. By 2008, the number of CT examinations in England alone (population 51 million) was more than 3 million per year [2].
Ionizing radiation from CT has become a public health concern, as there is a possible attributable future cancer risk [3–11]. It is particularly worrisome that children receive higher radiation doses than necessary if adult CT settings are used [12]. Surveys have estimated that children under 15 years of age make up between 3% and 11% of patients undergoing CT in Western Europe and North America [13–15]. The concerns regarding CT in young people, coupled with the fact that few empirical data are available for risk prediction, make studying potential risks associated with radiation exposure from CT in young people an important area of epidemiological research. Younger patients are more susceptible to the effects of radiation, both due to their longer post-irradiation life expectancy and to the increased vulnerability of rapidly dividing cells [4]. To better ascertain likely risks associated with CT radiation exposure in young people, a large cohort study of individuals first scanned before 22 years’ of age in the United Kingdom is under way. The primary objective is to assess the potential risks associated with CT radiation exposure at a young age. In this first descriptive paper from the study, we describe trends and patterns in CT usage in Northern England.
Materials and methods
Northern England as defined for this study includes the counties of Durham, Cumbria (excluding Barrow-in-Furness), Northumberland, Tyne and Wear and the South Tees area of North Yorkshire. The region includes nine National Health Service (NHS) hospital trusts, including two neurosurgical centers, which vary in the size of geographical area covered, number and type of patients treated, number and type of hospitals, the radiology departments’ patient load and services provided, and public health and clinical responsibilities. The estimated total population of the region is around 3 million, with an estimated 800,000 of these under the age of 22 years. Population figures for the region were obtained, as aggregated midyear population estimates, from the North East Public Health Observatory. As different age bands were used for the official figures, pro rata adjustments were made to allow estimation of age-group-specific populations. Electronic data from radiology information systems (RIS) were obtained for patients who had had CT in any of the nine trusts. The retrieved data included national and/or local patient identifiers, date of birth, sex, postcode, and the date and type of CT examination(s). Patient identifiers were used to identify patients having multiple procedures within one trust, while matching on patients’ name, sex and date of birth was done to identify patients examined at more than one trust.
The data included in this study cover the 10-year period from 1993 to 2002 for patients under the age of 22 years. This age range was chosen to include all available data from an ongoing epidemiological study of the potential risks associated with radiation exposure from CT. Complete data were available across the entire study period for five trusts, including the two largest. Four trusts were missing data for 1993–1994, three for 1995–1997, two for 1998–1999 and one for 2000. Where the installation of a RIS took place midway through a year, a pro rata adjustment was used to estimate the total number of scans in that year. Where RIS data were missing for early years of the study period, the number of scans in the earliest year available (with complete or pro rata adjusted data) was taken to apply to all previous years of CT operation in the trust. The highest number of scans in any one year for these trusts by the above replacement of missing data was 215. Replacement of missing data was done only to assess temporal trends (of numbers of scans and patients, by sex) and to estimate rates of scans for the whole region. All other descriptive statistics are based on actual data.
Types of CT examinations were grouped into six categories (head/neck, abdomen/pelvis, chest, spine, extremities and miscellaneous) as suggested by Mettler et al. [16]. As the number of scans including more than one part of the body was small, they were included in the “miscellaneous” category. The term “multiple scans” used for reporting the results of this study incorporates scans that involved more than one scan region as well as scans performed in the same patients on separate occasions.
These data are described in relation to population estimates, temporal trends, patient age and sex, and type of examination. Associations between categorical variables were assessed using chi-square tests and correlations were assessed using Spearman rank tests. All statistical analyses were performed using the statistical software package Stata, version 10 (Stata Corp., College Station, TX).
This study, as part of a larger retrospective epidemiological cohort study, was given a favourable ethical opinion by the Newcastle and North Tyneside Local Research Ethics Committee (akin to approval) and was approved by the National Information Governance Board so as not to require individual patient-level consent. The study was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Results
A total of 38,681 scan records were abstracted from RIS records for 20,483 patients under the age of 22 years for the period 1993–2002, inclusive. This included 15,481 scans (40%) among 8,472 female patients (41%), 23,186 scans (60%) among 12,000 male patients (59%), and 14 among 11 patients of unknown sex. When substituting for missing data in the early years of the study period, the estimated numbers of patients and scans were 25,688 and 42,126, respectively. This represented 3 scanned patients/1,000 population aged less than 22 years, and 0.5 scans per individual aged less than 22 years over the 10-year study period.
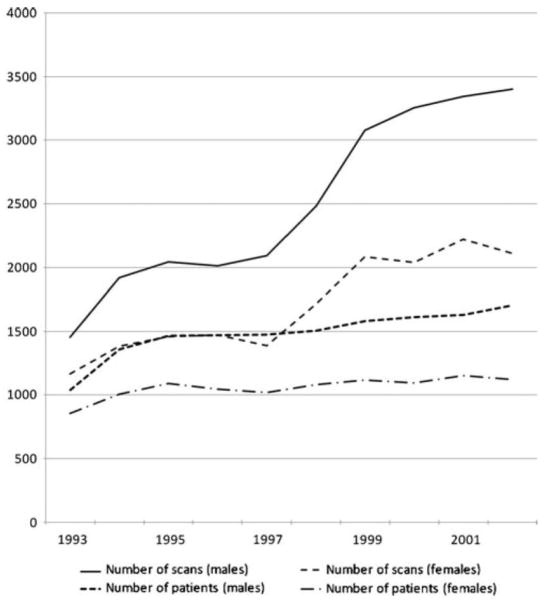
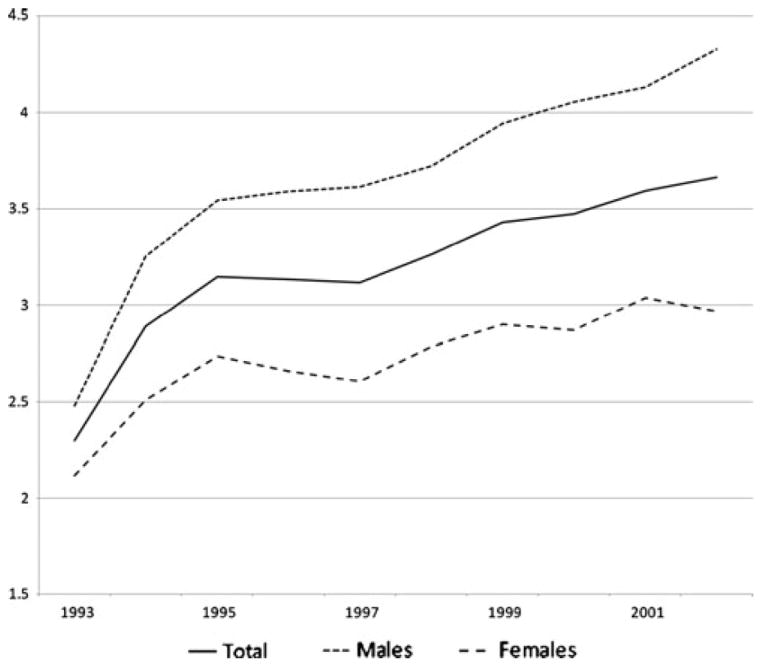
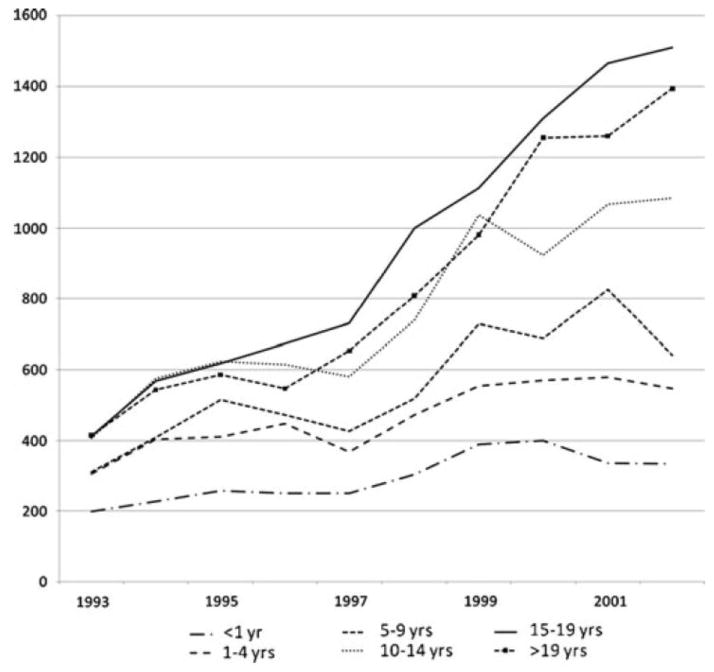
In the 10-year period, the number of scans/year more than doubled from an estimated 2,624 to 5,513. The most striking increase was seen in the years 1997–2000. The increase in the number of patients scanned per year was less marked, rising from an estimated 1,896 patients in 1993 to 2,826 in 2002. These trends were observed for males and females, but the rise was steeper for males as seen in Fig. 1. Similar trends were seen when treating missing data as zeros (results not presented). Overall rates of patients having one or more CT scan(s) rose from 2.24/1,000 in 1993 to 3.54/1,000 in 2002 (Fig. 2). For 2002, age-specific rates were highest in infants and in patients aged 20 or 21 years (Table 1). In 2002, there were 11 scans/1,000 infants in the region, with similar rates in males and females. The variance between scan rates for males and females increased with age, with increasingly higher rates in males. Similar results were seen for rates of patients, with 5.6 infants/1,000 and 10.4/1,000 aged 20 or 21 years having one or more CT(s) in 2002 (Table 1). While increases in numbers of recorded scans were seen across all age groups, the greatest increases over the study period were in the older patients, most notably those aged 15 years and above (Fig. 3). This was reflected by a positive association between the year a scan took place and the age of the patient at the time of the scan (Spearman rho = 0.08, P < 0.0001).
Fig. 1.
Number of CT scans/year, and number of patients scanned with CT/year in a cohort of patients under 22 years of age in Northern England 1993–2002 inclusive, by sex
Fig. 2.
Rates of CT scans per year per 1,000 population aged less than 22 years in a cohort of patients in Northern England 1993–2002 inclusive, by sex
Table 1.
CT scans/1,000 agematched population in a cohort of patients in Northern England in 2002
| Age group | Scans
|
Patients
|
||||
|---|---|---|---|---|---|---|
| Total | Males | Females | Total | Male | Females | |
| <1 year | 11.62 | 11.60 | 11.65 | 5.62 | 6.04 | 5.18 |
| 1–4 years | 4.45 | 5.09 | 3.79 | 2.10 | 2.38 | 1.80 |
| 5–9 years | 3.71 | 4.51 | 2.87 | 2.01 | 2.39 | 1.62 |
| 10–14 years | 5.73 | 7.28 | 4.11 | 3.02 | 3.64 | 2.36 |
| 15–19 years | 8.00 | 10.11 | 5.81 | 4.42 | 5.40 | 3.40 |
| 20–21 years | 20.04 | 23.78 | 16.26 | 10.35 | 12.26 | 8.42 |
Fig. 3.
Number of CT scans/year by age group in a cohort of patients under 22 years of age in Northern England 1993–2002 inclusive (age intervals differ in length)
A total of 73% of scans were of the head (including 514 scans of the neck in 354 patients), with similar proportions in males and females (Table 2). The second and third most common examination types were of the abdomen or chest, both accounting for 9% of all scans. The miscellaneous group included 52 scans that were recorded as combinations of scans in other groups. The majority (37) of these were of the chest and abdomen together, while the remaining 15 involved the pelvis with either abdomen or chest.
Table 2.
Number of CT scans by sex and type of examination in a cohort of patients under 22 years of age in Northern England 1993—2002
| Scan region | All N (%) |
Males N (%) |
Females N (%) |
|---|---|---|---|
| Head and/or neck | 28,326 (73) | 16,811 (73) | 11,503 (74) |
| Abdomen and/or pelvis | 3,467 (9.0) | 2,109 (9.1) | 1,358 (8.8) |
| Chest | 3,443 (8.9) | 2,058 (8.9) | 1,384 (9.0) |
| Spine | 1,420 (3.7) | 942 (4.1) | 478 (3.1) |
| Extremities | 1,352 (3.5) | 899 (3.9) | 453 (2.9) |
| Miscellaneous | 610 (1.6) | 321 (1.4) | 288 (1.9) |
| Unknown | 63 (0.2) | 46 (0.2) | 17 (0.1) |
| Total | 38,681 (100) | 23,186 (100) | 15,481 (100) |
The patient’s sex was unknown for 14 scans (12 head, 1 chest and 1 miscellaneous)
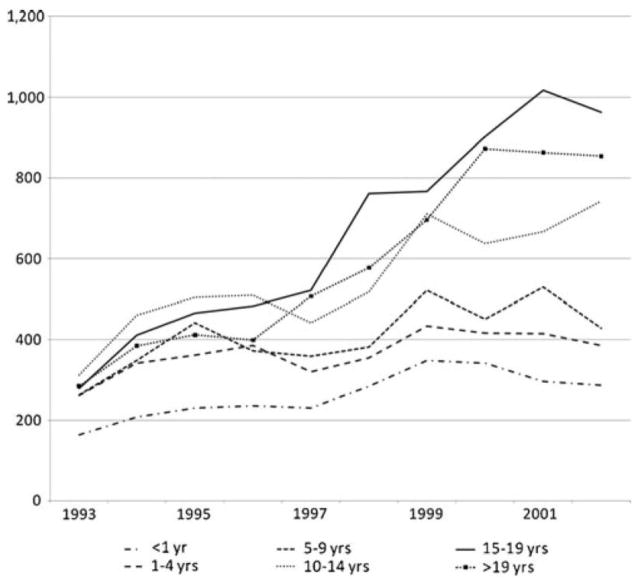
The number of scans per year rose similarly for all scan types, particularly among those aged over 15 years (Fig. 4). The number of chest scans in 1999 was twice the number in 1997. The number had doubled again in 2001. Similar increases were seen for scans of the abdomen and pelvis, with smaller increases for scans of other sites.
Fig. 4.
Head and/or neck CT scans/year in patients under 22 years of age in Northern England 1993–2002 inclusive (age intervals differ in length)
There was a significant association between age at the time of the scan and the type of examination (chi-square test, P < 0.001); 89% of CT scans in infants were of the head, with the percentage of head scans falling with increasing age (Table 3).
Table 3.
Numbers of CT scans by age and type of examination in a cohort of patients under 22 years of age in Northern England 1993—2002a
| Categories | Age at time of the scan (years)
|
|||||
|---|---|---|---|---|---|---|
| <1 N (%) |
1–4 N (%) |
5–9 N (%) |
10–14 N (%) |
15–19 N (%) |
20–21 N (%) |
|
| Head and/or neck | 2,622 (89) | 3,668 (79) | 4,086 (74) | 5,497 (72) | 6,565 (70) | 5,845 (69) |
| Abdomen and/or pelvis | 123 (4.2) | 219 (4.7) | 315 (5.7) | 598 (7.8) | 1,066 (11) | 1,134 (13) |
| Chest | 165 (5.6) | 507 (11) | 759 (14) | 675 (8.8) | 730 (7.8) | 604 (7.2) |
| Extremity | 8 (0.3) | 58 (1.3) | 151 (2.7) | 457 (6.0) | 375 (4.0) | 303 (3.6) |
| Spine | 11 (0.4) | 70 (1.5) | 142 (2.6) | 302 (4.0) | 487 (5.2) | 407 (4.8) |
| Miscellaneous | 17 (0.6) | 122 (2.6) | 74 (1.3) | 103 (1.4) | 163 (1.7) | 131 (1.6) |
| Unknown | 1 (0.03) | 12 (0.3) | 7 (0.1) | 15 (0.2) | 12 (0.1) | 16 (0.2) |
| Total | 2,947 (100) | 4,656 (100) | 5,534 (100) | 7,647 (100) | 9,398 (100) | 8,440 (100) |
The patient’s age was unknown for 59 scans (43 head, 3 abdomen and/or pelvis, 12 chest and 1 spine)
Four percent of patients had more than five scans, while 10% of patients had more than three scans (Table 4). The median number of scans per patient per year rose from one in 1993 to two in 1999. In the years 1992–1997, 75% of scanned patients had one CT scan per year, with 91% having one or two scans and 95% having three or fewer. In 1998, the proportion of patients having only one scan fell to 65%, with 96% of patients having 1–4 scans. In 1999, the proportion of patients having only one scan fell to 49% and remained around 50% for the rest of the study period.
Table 4.
Numbers of multiple scans/patient, by sexa
| Number of scans | Total N (%) |
Males N (%) |
Females N (%) |
|---|---|---|---|
| 1 | 12,401 (61) | 7,207 (60) | 5,186 (61) |
| 2 | 5,407 (26) | 3,137 (26) | 2,267 (27) |
| 3 | 679 (3.3) | 428 (3.6) | 251 (3.0) |
| 4 | 1,035 (5.1) | 640 (5.3) | 395 (4.7) |
| 5 | 177 (0.9) | 104 (0.9) | 73 (0.9) |
| 6 | 290 (1.4) | 165 (1.4) | 125 (1.5) |
| 7 | 69 (0.3) | 49 (0.4) | 20 (0.2) |
| 8 | 135 (0.7) | 76 (0.6) | 59 (0.7) |
| 9 | 25 (0.1) | 15 (0.1) | 10 (0.1) |
| 10 | 75 (0.4) | 53 (0.4) | 22 (0.3) |
| 11–20 | 153 (0.8) | 101 (0.8) | 52 (0.6) |
| >20 | 37 (0.2) | 25 (0.2) | 12 (0.1) |
| Total | 20,483 (100) | 12,000 (100) | 8,472 (100) |
The sex was unknown for 11 patients (eight had one scan, three had two scans)
Percentages were broadly similar for males and females across the range of numbers of scans per patient (Table 4), with no significant association between sex and number of scans (chi-square test, P = 0.19). In the 190 patients who had more than 10 CT scans, 2,059 scans (67%) were of the head and/or neck, 501 (16%) of the abdomen or pelvis and 372 (12%) of the chest. Again, percentages for males and females were similar (results not presented).
Of the 20,483 patients in this study, 484 (2.3%) had CT scans at two different trusts in the region and four at three different trusts. Whilst most of the patients seen at more than one trust included at least one of the two regional referral centers as one of the trusts in which they had been scanned, 39 individuals underwent CT scans at two different non-regional referral centers within the Northern Region. Of patients scanned at more than one trust, the median number of scans/patient was four, with 20% having two scans and 27%, 11% and 11% having three, four or five scans, respectively.
Fourteen CT scanners in 13 hospitals were in use in the NHS trusts in Northern England in 1993 (with one hospital having a second specialist radiology department). By the end of 1997, this had risen to 18, and by the end of 2002, a total of 20 scanners were in use in 18 hospitals.
Discussion
While a number of previous publications have described trends in the use of CT, these have described primarily adult populations [1, 17, 18]. Very little has been published regarding trends and patterns in the use of CT in young patients. This study of electronic data from radiology departments shows that the use of CT in young people in Northern England increased over the 10 years 1993–2002. The greatest increase in the annual number of scans was in the period 1997–2000. Although an increase was also seen in numbers of patients having one or more CT(s), this was less pronounced. This difference is explained by the increase in multiple scans per patient per year over the same time period. The most common type of CT examination, particularly in infants, was of the head. The number of scans increased similarly over time for all examination types. The temporal trends in our study broadly mirror those seen in adult populations in the United Kingdom [1] and elsewhere [17]. The general increase seen in CT usage partly reflects the increasing availability and the nature of the technology. The increasing speed with which CT can be performed makes it especially applicable in those children who would otherwise require sedation or anaesthesia to keep them motionless for long enough to obtain diagnostic images. We obtained RIS data from all nine NHS hospital trusts in Northern England. These included a large regional center with four radiology departments, including one in the largest teaching hospital within the region, a further large teaching hospital and seven smaller hospitals. Although data were not complete over the entire study period, they were complete for the two largest trusts in the region. The method chosen to estimate missing data was likely to be one of the most conservative in terms of assessing increases in numbers of scans. By replacing missing numbers of scans with the number in the earliest year available, we believe that this overestimated the number of scans for the trusts with missing data for the early years of the study period and hence reduced the magnitude of the trends. However, as the trusts with missing data were those that performed relatively few CT scans, any overestimation is likely to have had little overall effect on our results.
The increase in the number of scans was not associated directly with changes in the number of scanners. At the time when the number of scans increased most steeply, there was an increase of only one scanner across the entire region, and this was at one of the smaller hospitals towards the end of the period.
An alternative analytical approach may have been to use a formal time series analysis. However, as we do not have complete data on examination type, age group or sex and chose to only replace the missing data for years as with the small numbers in certain categories, this might have introduced unacceptable imprecision. As these are the only data available to this study, there were no other variables that could be included to identify further patterns.
Increases in CT usage in young people have been seen in other studies, although data are very sparse and in some cases limited to certain examination types. In the years 1996–1999, the number of abdominal and pelvic CT examinations among children nearly doubled in a major United States hospital [4]. Markel et al. [19] demonstrated an increased use of CT for paediatric blunt chest trauma in one trauma center in the United States in the years 2001–2005. We found a similar increase, and we are able to demonstrate that the increase started even earlier.
A primary driver of the increased number of scans in the period 1997–2000 was the simultaneous increase in the number of multiple scans per patients. Multiple scans, for example, may be more likely to occur in trauma patients in whom scanning different injured areas could provide useful clinical information. The practice of CT scanning in the trauma setting varies widely, for example, some centers place more reliance on US than on CT for initial abdominal examinations. With shorter scan times, more scans can be done overall, more regions in the same patient, and more complex scans (e.g., different contrast-techniques) can be performed.
Furthermore, with trauma patients (suspected polytrauma) there has been a well-recognized trend to scan more body parts per patient, both because CT is potentially useful and because it is easy to perform once the patient is in the scanner. Indications for scans or evidence of repeated scans were not available from electronic records and were, therefore, unavailable to this study.
It is likely that changes in clinical practice caused most of these increases. National (United Kingdom) guidelines and recommendations on the use of CT in young patients, particularly for head injuries, include three published during the period of the largest increase seen in our study [20–22]. It is likely that such guidelines would have been driven by existing changes in clinical practice and, as such, would reflect a preexisting increase in CT usage. It might then be expected that an additional increase would follow their publication. Given the presumed higher incidence of head injury among the older patients in our study, changes in guidelines and clinical practices resulting in increased use of CT in head trauma may also explain the greatest increase in numbers of CT scans being in the older patients.
Most CT scans in our study were of the head, in line with a study in young patients in Israel [9]. This contrasts studies of populations including all age groups, which report abdomen and pelvis as the most common scan regions [13, 23]. This suggests differing uses of CT in younger and older populations. Although outside the years covered by this study, a survey of paediatric CT practices in Germany during 2005 and 2006 found that just over 50% of paediatric CT examinations were of the brain [24], which is lower than in our study. The age distribution in the German study was uniform, although only three age categories were used, with no delineation between infancy and other ages of early childhood.
Concerns have been raised that the use of CT is not always justified in young people [5, 6, 25–28]. In particular, the use of CT in trauma (multiple scan regions), seizures, chronic headaches and suspected appendicitis in children has been questioned [28–35].
The numbers of multiple scans may have increased if patients moving (both in terms of care and residence) between trusts were scanned at both. However, given that only 488 patients moved between trusts in this study, this cannot explain the increase in either total number of scans per year or in numbers of multiple scans per year.
With such little knowledge about the use of CT in young populations around the world, it is important to report such trends and patterns, as in this report of data collected up to 2002 in our ongoing epidemiological study.
Conclusion
The use of CT in young people in Northern England more than doubled in the period 1993–2002. There was a particularly large increase in the number of scans observed in the period 1997–2000. This is partly, but not wholly, explained by higher numbers of multiple scans per patient. The majority of scans performed in this age group were of the head, but the percentage of head scans decreased with increasing age. The results presented here are part of an ongoing epidemiological study into the long-term health effects of using CT in young people, in which patients are being matched to national-level cancer registry data.
Acknowledgments
This study was supported by contract NO2-CP-75501 from the United States National Cancer Institute and through funding from the Radiation Research Programme of the United Kingdom Department of Health. We thank the staff in radiology departments across the Northern Region of England who contributed data to this study and Mrs. Katharine Kirton and Mr. Richard Hardy for their assistance with the study. We also thank Dr. John Kotre for his comments on the paper.
References
- 1.Hart D, Wall BF. UK population dose from medical X-ray examinations. Eur J Radiol. 2004;50:285–291. doi: 10.1016/S0720-048X(03)00178-5. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health. [Accessed May 2011];Hospital Activity Statistics. 2008 Available from: http://www.performance.doh.gov.uk/hospitalactivity/data_requests/imaging_and_radiodiagnostics.htm.
- 3.Rehani MM, Berry M. Radiation doses in computed tomography. The increasing doses of radiation need to be controlled. Br Med J. 2000;320:593–594. doi: 10.1136/bmj.320.7235.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brenner DJ, Elliston CD, Hall EJ, et al. Estimated risks of radiation-induced fatal cancer from paediatric CT. AJR. 2001;176:289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 5.Parker L. Computed tomography scanning in children: radiation risks. Pediatr Hematol Oncol. 2001;18:307–308. doi: 10.1080/088800101300312564. [DOI] [PubMed] [Google Scholar]
- 6.Paterson A, Frush DP, Donnelly LF. Helical CT of the body: are settings adjusted for paediatric patients? AJR. 2001;176:297–301. doi: 10.2214/ajr.176.2.1760297. [DOI] [PubMed] [Google Scholar]
- 7.Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body screening. Radiology. 2004;232:735–738. doi: 10.1148/radiol.2323031095. [DOI] [PubMed] [Google Scholar]
- 8.Brenner DJ, Hall EJ. Computed tomography an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 9.Chodick G, Ronckers CM, Shalev V, et al. Excess lifetime cancer mortality risk attributable to radiation exposure from computed tomography examinations in children. IMAJ. 2007;9:584–587. [PubMed] [Google Scholar]
- 10.Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Int Med. 2009;169:2071–2077. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sodickson A, Baeyens PF, Andriole KP, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology. 2009;251:175–184. doi: 10.1148/radiol.2511081296. [DOI] [PubMed] [Google Scholar]
- 12.Voss SD, Reaman GH, Kaste SC, et al. The ALARA concept in pediatric oncology. Pediatr Radiol. 2009;39:1142–1146. doi: 10.1007/s00247-009-1404-5. [DOI] [PubMed] [Google Scholar]
- 13.Mettler FA, Wiest PW, Locken JA, et al. CT scanning: patterns of use and dose. J Radiol Prot. 2000;20:353–359. doi: 10.1088/0952-4746/20/4/301. [DOI] [PubMed] [Google Scholar]
- 14.Shrimpton PC, Jones DG, Hillier MC, et al. Chilton: NRPBR249. HMSO; London: 1991. Survey of CT practice in the UK: Part 2. Dosimetric Aspects. [Google Scholar]
- 15.Chodick G, Ronckers CM, Ron E, et al. The utilization of paediatric computed tomography in a large Israeli HMO. Pediatr Radiol. 2006;36:485–490. doi: 10.1007/s00247-005-0091-0. [DOI] [PubMed] [Google Scholar]
- 16.Mettler FA, Thomadsen BR, Bhargavan M, et al. Medical radiation exposure in the U.S. in 2006: Preliminary results. Health Phys. 2008;95:502–507. doi: 10.1097/01.HP.0000326333.42287.a2. [DOI] [PubMed] [Google Scholar]
- 17.Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol. 2008;81:362–378. doi: 10.1259/bjr/01948454. [DOI] [PubMed] [Google Scholar]
- 18.Boone JM, Brunberg JA. Computed tomography in a tertiary care university hospital. J Am Coll Radiol. 2008:132–138. doi: 10.1016/j.jacr.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Markel TA, Kumar R, Koontz NA, et al. The utility of computed tomography as a screening tool for the evaluation of pediatric blunt chest trauma. J Trauma. 2009;67:23–28. doi: 10.1097/TA.0b013e318184ba9a. [DOI] [PubMed] [Google Scholar]
- 20.Bartlett J, Kett-White R, Mendelow AD, et al. Recommendations from the Society of British Neurological Surgeons. Br J Neurosurg. 1998;12:349–352. doi: 10.1080/02688699844871. [DOI] [PubMed] [Google Scholar]
- 21.Royal College of Radiologists. Making the best use of a department of clinical radiology: guidelines for doctors. 4. The College; London: 1998. [Google Scholar]
- 22.Royal College of Surgeons England. Report of the working party on the management of patients with head injuries. London: 1999. [Accessed May 2011]. http://www.rcseng.ac.uk/publications/docs/report_head_injuries.html. [Google Scholar]
- 23.Mettler FA, Bhargavan M, Faulkner K, et al. Radiologic and nuclear medicine studies in the United States and Worldwide: Frequency, radiation dose, and comparison with other radiation sources, 1950–2007. Radiology. 2009;253:520–531. doi: 10.1148/radiol.2532082010. [DOI] [PubMed] [Google Scholar]
- 24.Galanski M, Nagel HD, Stamm G. Results of a nationwide survey in 2005/06. Medizinische Hochschule; Hannover: 2006. Pediatric CT exposure practice in the federal republic of Germany. [Google Scholar]
- 25.Clarke JC, Cranley K, Kelly BE, et al. Provision of MRI can significantly reduce CT collective dose. Br J Radiol. 2001;74:926–931. doi: 10.1259/bjr.74.886.740926. [DOI] [PubMed] [Google Scholar]
- 26.Ghotbi N, Ohtsuru A, Ogawa Y, et al. Pediatric CT scan usage in Japan: results of a hospital survey. Radiat Med. 2006;24:560–567. doi: 10.1007/s11604-006-0072-8. [DOI] [PubMed] [Google Scholar]
- 27.Mazrani W, McHugh K, Marsden PJ. The radiation burden of radiological investigations. Arch Dis Child. 2007;92:1127–1131. doi: 10.1136/adc.2006.101782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oikarinen H, Meriläinen S, Pääkkö E, et al. Unjustified CT examinations in young patients. Eur Radiol. 2009;19:1161–1165. doi: 10.1007/s00330-008-1256-7. [DOI] [PubMed] [Google Scholar]
- 29.Ruess L, Sivit CJ, Eichelberger MR, et al. Blunt abdominal trauma in children: impact of CT on operative and nonoperative management. AJR. 1997;169:1011–1014. doi: 10.2214/ajr.169.4.9308453. [DOI] [PubMed] [Google Scholar]
- 30.Renton J, Kincaid S, Ehrlich PF. Should helical CT scanning of the thoracic cavity replace the conventional chest Xray as a primary assessment tool in pediatric trauma? An efficacy and cost analysis. J Pediatr Surg. 2003;38:793–797. doi: 10.1016/jpsu.2003.50169. [DOI] [PubMed] [Google Scholar]
- 31.Durham SR, Liu KC, Selden NR. Utility of serial computed tomography in pediatric patients with head trauma. J Neurosurg. 2006;105:365–369. doi: 10.3171/ped.2006.105.5.365. [DOI] [PubMed] [Google Scholar]
- 32.Maytal J, Krauss JM, Novak G, et al. The role of brain computed tomography in evaluating children with new onset of seizures in the emergency department. Epilepsia. 2000;41:950–954. doi: 10.1111/j.1528-1157.2000.tb00277.x. [DOI] [PubMed] [Google Scholar]
- 33.Donmez FY, Guvenc Z, Emiroglu FK, et al. Evaluation of neurological complications in pediatric liver transplant recipients: MRI versus CT. J Child Neurol. 2009;24:656–663. doi: 10.1177/0883073808329531. [DOI] [PubMed] [Google Scholar]
- 34.Lewis DW, Dorbad D. The utility of neuroimaging in the evaluation of children with migraine or chronic daily headache who have normal neurological examinations. Headache. 2000;40:629–632. doi: 10.1046/j.1526-4610.2000.040008629.x. [DOI] [PubMed] [Google Scholar]
- 35.Frush DP, Frush KS, Oldham KT. Imaging of acute appendicitis in children: EU versus U.S. … or US versus CT? A North American perspective. Pediatr Radiol. 2009;39:500–505. doi: 10.1007/s00247-008-1131-3. [DOI] [PubMed] [Google Scholar]