Significance
The ultimate success of the Affordable Care Act (ACA) depends on how well the health insurance exchanges can bring the benefits of private competition to individuals in the form of lower premiums. Doing so requires that individuals, when shopping for health insurance, correctly weigh the benefits and costs of various insurance options. Our work suggests that the overall population, and even more so those most likely affected by the ACA, is not well equipped to do so. We documented low levels of ACA and health insurance knowledge in the month preceding the introduction of the exchanges. We propose that simplified options, decision aids, and health insurance product design to address the limited understanding of health insurance contracts will be crucial for ACA’s success.
Abstract
This paper investigates whether individuals are sufficiently informed to make reasonable choices in the health insurance exchanges established by the Affordable Care Act (ACA). We document knowledge of health reform, health insurance literacy, and expected changes in healthcare using a nationally representative survey of the US population in the 5 wk before the introduction of the exchanges, with special attention to subgroups most likely to be affected by the ACA. Results suggest that a substantial share of the population is unprepared to navigate the new exchanges. One-half of the respondents did not know about the exchanges, and 42% could not correctly describe a deductible. Those earning 100–250% of federal poverty level (FPL) correctly answered, on average, 4 out of 11 questions about health reform and 4.6 out of 7 questions about health insurance. This compares with 6.1 and 5.9 correct answers, respectively, for those in the top income category (400% of FPL or more). Even after controlling for potential confounders, a low-income person is 31% less likely to score above the median on ACA knowledge questions, and 54% less likely to score above the median on health insurance knowledge than a person in the top income category. Uninsured respondents scored lower on health insurance knowledge, but their knowledge of ACA is similar to the overall population. We propose that simplified options, decision aids, and health insurance product design to address the limited understanding of health insurance contracts will be crucial for ACA’s success.
Although a lot of attention has been paid to the startup problems of the Affordable Care Act’s (ACA) health insurance exchanges (“exchanges”), the ultimate success of the program depends on how well these exchanges can bring the benefits of private competition to individuals in the form of better coverage and lower premiums. Doing so requires that individuals, when shopping for health insurance, correctly weigh the benefits and costs of various insurance options. Unfortunately, there is evidence that individuals are usually at risk for making poor choices when it comes to health insurance (1). Although exchanges in Medicare Part D, for example, are considered a success in terms of achieving high enrollment rates (2, 3), recent analysis on plan choice and drug claims shows that the majority of enrollees ignore Medicare’s readily available plan recommendations, and choose plans that fail to minimize their expected costs based on current drug needs, health status, and health risks (4, 5). Moreover, consumers have been shown not to understand traditional health insurance plans (6). More generally, the populations most likely to be affected by the ACA—the young, less educated, and those with lower incomes—are also more likely to be financially illiterate (7).
Individuals who do not fully understand the rules governing ACA and the financial consequences of their insurance choices are likely to make mistakes. They might over- or underinsure (or not insure at all) or choose overly costly insurance policies. Similarly, individuals may choose policies on the basis of premiums only and fail to fully account for potential out-of-pocket costs (such as copayments) or gaps in coverage (such as formulary restrictions for prescription drugs).
This study investigates how well equipped individuals are to make adequate health insurance choices in light of the fast-changing environment of the ACA. During late August and September 2013, we collected data on subjective and objective knowledge about the health reform law, health insurance literacy (defined as the ability to make financial decisions regarding health insurance), and expected changes in healthcare using a nationally representative sample. The analysis focused on subpopulations most likely to be affected by the new law: those likely eligible for Medicaid (incomes below 100% of the federal poverty level [FPL]; 138% of FPL in states that expand Medicaid), those eligible for subsidies in the exchanges (income 100–400% of FPL), and those without health insurance. We compare their knowledge and expectations with that in the general population controlling for differences in education, age, race, sex, marital status, health status, and state-level characteristics (their state’s political orientation; whether their state is likely to expand Medicaid; and whether their state will have a federal exchange). In addition, we determine whether some subpopulations believe they are better prepared to deal with the recent ACA changes than they truly are.
Methods
Data.
We used the American Life Panel (ALP) to collect data on individuals’ subjective and objective knowledge of health insurance and ACA. The ALP is a panel of about 6,000 individuals aged 18 and older who agreed to participate in occasional online surveys. Respondents were recruited using a nationally representative sampling frame, and were provided with Internet access and a computer when necessary. Sample weights are calculated to correct for remaining selectivity. Respondents participate in ∼2 surveys per month and are compensated for their time. Since 2006, the ALP has included more than 350 surveys on a wide range of topics. Notably it was used for the RAND Election Poll in 2012, providing one of the most accurate predictions of the results of the presidential election (8). The American Life Panel data collection for this project was approved by RAND's Institutional Review Board on August 1, 2013.
Our results are based on a survey written specifically for this research. The full text of the survey, as well as the collected data, is available on the ALP website as “Well Being 356.” (9) The SI Appendix includes questions used in this study. The survey was fielded during the 5 wk preceding the introduction of the new health insurance exchanges. On August 23, 2013, we invited 4,758 ALP respondents aged 18–64 to participate in the survey, and 3,490 completed the survey by September 30, 2013, for a response rate of 73.4%. Because of the timing of our survey, we can only document knowledge before the launching of the exchanges; any increase in knowledge due to public information campaigns or media coverage after October 1, 2013, will not be reflected in our results.
We dropped observations for respondents with missing information for any of the variables used in the analysis; our final sample contains 3,414 observations. We excluded adults age 65 and older because they are eligible for Medicare and therefore face a different set of insurance choices.
All of the statistics are weighted using the ALP sample weights. We compared key variables in our ALP sample with similarly constructed variables from the March 2012 Current Population Survey, a nationally representative survey conducted by the US Census Bureau (10). We matched a subsample of ALP 356 survey respondents to ALP 243 survey to investigate patterns of financial literacy across the groups of interest.
ACA Objective Knowledge.
We asked 11 questions about health reform, as shown in the SI Appendix. These included true/false questions on the health insurance mandate, penalties for the uninsured, health insurance exchanges, available subsidies in the exchanges, preexisting conditions, and Medicaid expansion. Some of these questions were drawn from the March 2013 Kaiser Health Tracking Poll (11). We constructed an ACA knowledge binary variable that is equal to 1 if the respondent answered more questions correctly than the median (median correct = 5).
Health Insurance Literacy.
Questions about health insurance include three true/false questions on the relation between deductibles and premiums, and differences in prices for generic or brand-name prescriptions or in-network or out-of-network providers. Four multiple-choice questions (SI Appendix) were included on provider networks, deductibles, coinsurance, and copays. We constructed a health insurance knowledge binary variable that is equal to 1 if the respondent answered more questions correctly than the median (median correct = 5).
Subjective Knowledge.
We also included questions on respondent’s self-assessed knowledge of ACA and health insurance. We constructed an ACA subjective knowledge binary variable equal to 1 if the respondent claimed to know a great deal or a fair amount about the health reform law. The ACA subjective knowledge question was adapted from the Retirement Perspectives Survey (12). For health insurance, a binary variable is equal to 1 if the respondent strongly agreed (on a five-point Likert scale) with the statement: “I am confident about dealing with day-to-day financial matters,” which included a list of common financial products, including insurance. This question was drawn from the Financial Industry Regulatory Authority’s 2009 National Financial Capability Study (13).
Expected Changes in Healthcare.
We asked how respondents expect five dimensions of healthcare to be affected by the new law: access, waiting time, quality of care, out-of-pocket spending, and emergency care spending. Respondents were asked whether they expected each of these dimensions to improve (coded as 1), worsen (−1), or not change (0). We aggregated these responses into an index of expected change due to health reform by summing the answers to all five dimensions (i.e., index varies between −5 and 5). In addition, we asked an “overall” expectation question of whether the respondent expected him and his family to be better off (+1), worse off (−1), or the same (0) under the new health law. We analyze the dimensions index and the overall expectation variable separately below. Although these question formats have the merit of simplicity, an important limitation is that they do not allow respondents to express uncertainty about each of these outcomes, as would have been the case had we used a probabilistic format (14, 15).
Multivariate Analysis.
We used logistic models and reported odds ratios for the binary outcomes. The odds ratios are the exponents of the corresponding coefficients of the logit model and their SEs were calculated using the delta method. Ordinary least squares (OLS) and ordered logit models were used for the expectations outcomes. We estimated models of the likelihood that an individual is more knowledgeable than the median or expects changes as a function of income, health insurance status, age, education, race, ethnicity, sex, marital status, and health status. Because information campaigns about health reform likely vary from state to state, especially with differing state political leanings and level of state involvement in implementing the reform, we also included state-level variables in the analysis (red/blue state; whether the state is likely to expand Medicaid; whether the state uses the federal, a state-based, or a state–federal partnership exchange). We assigned states to red or blue based on whether the state voted for Mitt Romney or Barack Obama in the 2012 presidential election. We used information from the Kaiser Family Foundation to determine whether each state is currently moving forward with Medicaid expansion and which type of exchange is in place (16).
Results
Table 1 presents weighted descriptive statistics of the ALP sample; column 2 presents similar statistics using the 18–64 sample from the 2012 March CPS. Twenty-two percent of the sample had incomes below 100% of the FPL and are likely eligible for Medicaid, 55% had incomes 100–400% of FPL and may be eligible for subsidies in the exchanges, and 19% were uninsured. Overall, the figures in our ALP sample correspond well to those in the CPS. Two exceptions are income and marital status, for which discrepancies might be explained by differences in survey questions. In the case of income, for example, the ALP question is asked in intervals, and the CPS asks about total dollar amount.
Table 1.
Descriptive statistics
| Variable | ALP (%) | CPS (%) |
| Health insurance | ||
| Yes | 81 | 79 |
| No | 19 | 21 |
| Income | ||
| <100% of FPL | 22 | 19 |
| 100–250% of FPL | 31 | 31 |
| 251–400% of FPL | 24 | 22 |
| >400% of FPL | 23 | 28 |
| Education | ||
| No degree | 11 | 12 |
| High school or equivalent degree | 28 | 29 |
| Some college | 20 | 20 |
| Associate degree | 10 | 10 |
| Bachelor's degree | 20 | 19 |
| More than bachelor’s degree | 10 | 10 |
| Sex | ||
| Male | 49 | 49 |
| Female | 51 | 51 |
| Age | ||
| Younger than 26 | 15 | 18 |
| 26–44 | 41 | 40 |
| 45 and older | 44 | 42 |
| Marital status | ||
| Not married | 37 | 47 |
| Married | 63 | 53 |
| Race | ||
| White | 75 | 78 |
| Nonwhite | 25 | 22 |
| Ethnicity | ||
| Non-Hispanic | 79 | 84 |
| Hispanic | 21 | 16 |
| Health | ||
| Excellent/very good/good | 86 | 88 |
| Fair/poor | 14 | 12 |
| State of residence | ||
| Red state in 2012 election | 38 | 38 |
| Blue state in 2012 election | 62 | 62 |
| Federal exchange | 51 | 54 |
| State exchange | 37 | 36 |
| Partnership exchange | 12 | 11 |
| State likely to expand Medicaid | ||
| Yes | 58 | 54 |
| No | 42 | 46 |
| Number of observations | 3,414 | 122,296 |
Weighted averages using ALP survey 356 and 2012 March CPS, individuals younger than 65.
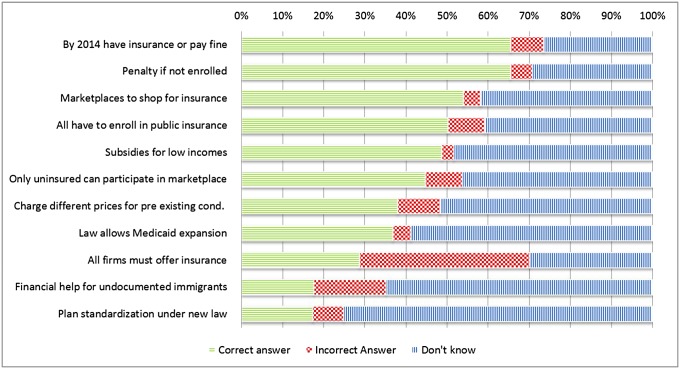
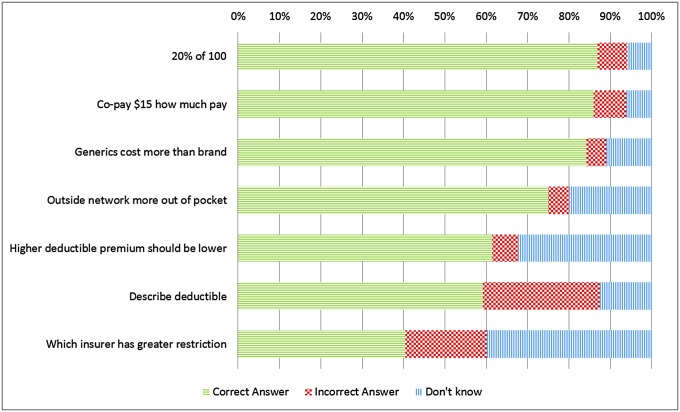
Figs. 1 and 2 display the prevalence of correct, incorrect and “don’t know” answers for each objective knowledge question asked. The fraction of correct answers is low overall, but it is generally higher among the health insurance than the health reform knowledge questions. Seventy-five percent of respondents answered “don’t know” to the plan standardization question and 65% to the question of whether undocumented immigrants are eligible for financial help to buy insurance. Moreover, 40% of the sample incorrectly answered the true/false question on whether, under the new law, all firms must provide insurance to employees—probably because they failed to take into account that only firms that meet certain criteria must provide insurance. For simplicity, in the analysis below we group “don’t know” and incorrect answers together. Using a multinomial logit model we found that there are no consistent differences in the characteristics of those who answer “don’t know” versus an incorrect answer (SI Appendix, Tables A8–A14) and concluded that this grouping does not lead to significant loss of information.
Fig. 1.
Fractions of correct, incorrect, and “don’t know” answers to ACA objective knowledge questions.
Fig. 2.
Fractions of correct, incorrect, and “don’t know” answers to health insurance objective knowledge questions.
Table 2 corroborates the finding that knowledge about health reform and health insurance shortly before exchange implementation is low. Less than one-quarter of the population claims to know at least a fair amount about ACA, and less than one-half considers themselves confident in financial matters. Only about one-half knows about the exchanges and the subsidies, 42% cannot correctly describe a deductible, and 62% do not know that a health maintenance organization (HMO) plan has greater provider restrictions than a preferred provider organization (PPO).
Table 2.
Knowledge about Affordable Care Act, health insurance, and financial literacy
| Income in % of FPL | ||||||
| All (%) | Uninsured (%) | <100 (%) | 100–250 (%) | 251–400 (%) | >400 (%) | |
| Knowledge about ACA | ||||||
| Knows a great deal/fair amount | 24 | 17 | 16 | 20 | 27 | 35 |
| Average number correct ACA knowledge questions | 4.46 | 3.26 | 2.74 | 4.04 | 5.02 | 6.10 |
| More than median correct ACA knowledge questions | 50 | 34 | 26 | 45 | 58 | 70 |
| Has heard of healthcare reform | 78 | 64 | 53 | 77 | 87 | 95 |
| Knows about new exchanges | 51 | 36 | 35 | 43 | 56 | 71 |
| Knows about penalty | 63 | 52 | 44 | 63 | 69 | 77 |
| Knows about subsidy | 46 | 31 | 29 | 41 | 53 | 62 |
| Health Insurance Literacy | ||||||
| Strongly agrees to be confident in financial matters | 46 | 34 | 26 | 43 | 50 | 64 |
| Strongly agrees to be good at mathematics | 28 | 25 | 21 | 27 | 29 | 36 |
| Average number correct HI knowledge questions | 4.84 | 3.70 | 3.25 | 4.62 | 5.55 | 5.90 |
| More than median correct HI knowledge questions | 49 | 27 | 18 | 40 | 63 | 74 |
| Can describe a deductible | 58 | 42 | 30 | 55 | 70 | 78 |
| Knows about deductible/premium tradeoff | 61 | 42 | 32 | 56 | 74 | 82 |
| Knows that HMO greater provider restriction than PPO | 38 | 19 | 20 | 28 | 48 | 57 |
| Average expected changes in health care | ||||||
| Family will be better off (1), no change (0), worse off (−1) | −0.23 | −0.09 | −0.09 | −0.21 | −0.30 | −0.31 |
| Average index for different dimensions | −1.44 | −0.83 | −0.79 | −1.32 | −1.75 | −1.88 |
| Expects access to care to increase (1), stay unchanged (0), decrease (−1) | −0.23 | −0.05 | −0.03 | −0.18 | −0.36 | −0.35 |
| Expects waiting times decrease (1), no change (0), increase (−1) | −0.36 | −0.28 | −0.24 | −0.32 | −0.43 | −0.44 |
| Expects quality of care increase (1), no change (0), decrease (−1) | −0.25 | −0.13 | −0.08 | −0.24 | −0.33 | −0.32 |
| Expects out-of-pocket decrease (1), no change (0), increase (−1) | −0.33 | −0.18 | −0.23 | −0.31 | −0.33 | −0.45 |
| Expects ER costs decrease (1), no change (0), increase (−1) | −0.28 | −0.19 | −0.21 | −0.28 | −0.30 | −0.33 |
| Number of observations | 3,414 | 698 | 963 | 1081 | 724 | 646 |
| Financial literacy (FL) | ||||||
| Numeracy | 85 | 71 | 69 | 82 | 90 | 96 |
| Inflation | 73 | 55 | 46 | 66 | 82 | 90 |
| Risk diversification | 62 | 42 | 36 | 52 | 71 | 83 |
| Average FL Index | 2.20 | 1.68 | 1.50 | 1.99 | 2.42 | 2.68 |
| Number of observations | 2,246 | 401 | 507 | 715 | 541 | 483 |
ALP survey 356, individuals younger than 65, raking weights used. Financial literacy is only available for a subset of respondents that have also answered ALP survey 243. FL index is the sum of correct answers to the three financial literacy questions.
Both subjective and objective knowledge increase with income. The population most likely affected by ACA—those with incomes between 100% and 400% of FPL and the uninsured—know significantly less than those in the top income category. Approximately 58% of those earning 100–250% of FPL have not heard about the exchanges or subsidies, and 44% do not know or have an incorrect understanding of the relationship between deductibles and premiums. Those earning 100–250% of FPL correctly answered, on average, 4 out of 11 questions about health reform and 4.6 out of 7 questions about health insurance. This compares with 6.1 and 5.9 correct answers, respectively, for those in the top income category (P = 0.00). Those earning 100–250% of FPL also lag behind on traditional financial literacy measures such as numeracy and understanding of inflation and risk diversification—in fact the patterns we observe in our data are similar to the ones reported in the financial literacy literature (7).
Most of the sample expects the health reform to result in worse healthcare, both in terms of overall changes and changes in different dimensions—on average all of the expectation variables are negative. However, those most likely to be affected by the reform are relatively more optimistic: the indexes are decreasing in income and tend to be closer to zero for the uninsured. Overall, Table 2 suggests that the population most likely to be affected by ACA is the least informed and least prepared to deal with the changes but, at the same time, is the most optimistic about improvements that the reform might bring.
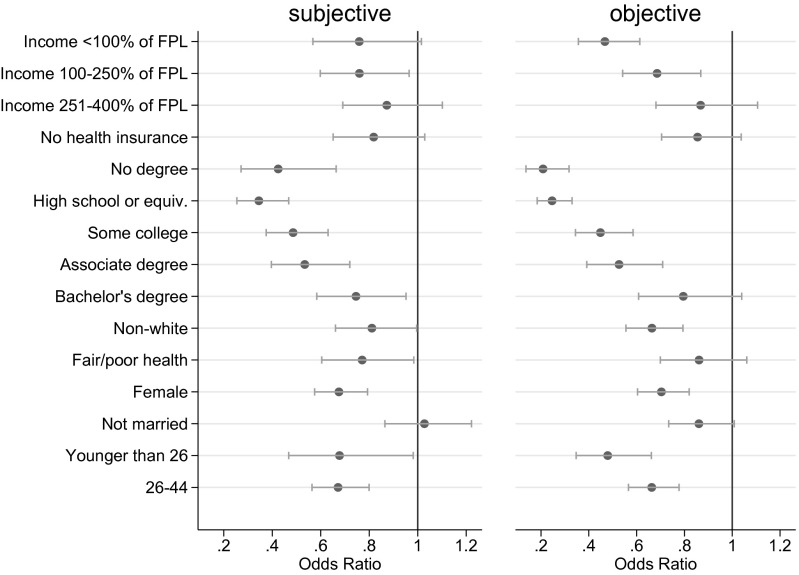
In part, the differences by income could be because lower-income individuals tend to be younger, less educated, and live in states with different political leanings and levels of ACA information than their wealthier counterparts. Therefore, we used multivariate regression to investigate differences in knowledge, taking into account differences in individual and state-level characteristics. Fig. 3 presents odds ratios for the subjective and objective health reform knowledge measures (the full logistic model is presented in SI Appendix, Table A1). Even controlling for a range of characteristics, the higher the income, the greater the knowledge. A person in the lowest income category is 53% less likely to score above the median on ACA knowledge than a person in the top income category [odds ratio (OR) = 0.47, P = 0.00]; this figure is 31% (OR = 0.69, P = 0.00) for a person with income 100–250% of FPL. The income gradient is stronger for the objective measure than the subjective measure, suggesting that those in the lowest income category think they know more than their actual knowledge would imply. There is also a steep education gradient: Although those with less than a high school education are 79% less likely than those with more than bachelor’s degree to score above the median (OR = 0.21, P = 0.00), those with a bachelor’s degree are just 20% less likely (OR = 0.80, P = 0.05). The uninsured seem to be about as knowledgeable about health reform as the rest of the population. Models with an interaction of income and health insurance coverage resulted in statistically insignificant estimates for the interaction coefficients and are not included in our main specifications.
Fig. 3.
ACA subjective and objective knowledge. Point estimates of odds ratios and 95% confidence intervals after logit estimation, full models are displayed in columns 1 and 2 of SI Appendix, Table A1. An odds ratio smaller than 1 indicates that people who have the stated condition are less likely to score above the median on ACA knowledge questions than people who do not have the stated condition when everything else is equal.
Less-educated, female, and young respondents have lower subjective and objective knowledge of ACA. Nonwhite respondents’ objective knowledge is relatively lower than their subjective knowledge, suggesting that they are not as informed as they think they are. The state-level variables do not predict knowledge in any of the cases (see coefficients in SI Appendix, Table A1).
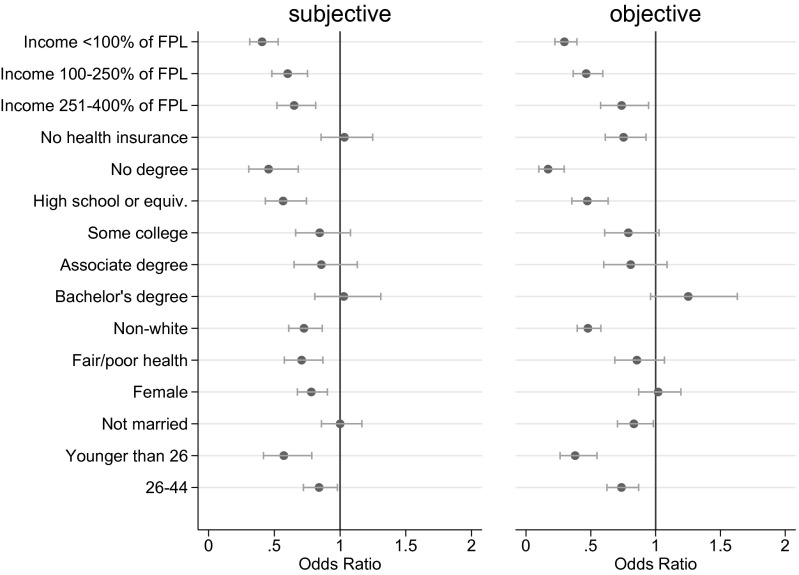
Fig. 4 shows similar results for health insurance knowledge. Income, education, race, and age are important predictors of knowledge, but again the state-level variables are not (columns 3 and 4 of SI Appendix, Table A1). The odds of scoring above the median on health insurance knowledge questions are 70% lower for an individual in the bottom income category (OR = 0.30, P = 0.00), 54% lower for an individual at 100–250% of FPL (OR = 0.46, P = 0.00), and 26% lower for an individual at 251–400% of FPL (OR = 0.74, P = 0.05), relative to an individual in the top income category. There is also an education gradient: Those with no degree or just a high school degree are less likely to score above the median than more educated respondents. The uninsured have lower objective health insurance knowledge, even though they do not rate themselves lower in the subjective knowledge measure.
Fig. 4.
Health insurance subjective and objective knowledge. Point estimates of odds ratios and 95% confidence intervals after logit estimation, full models are displayed in columns 3 and 4 of SI Appendix, Table A1. An odds ratio smaller than 1 indicates that people who have the stated condition are less likely to score above the median on health insurance knowledge questions than people who do not have the stated condition when everything else is equal.
Although our binary measure of knowledge allows us to summarize a wealth of information from all of the 18 questions we collected data on, it might lead us to miss some important patterns, because questions vary in difficulty and the dimension of knowledge measured. Therefore, we conducted two robustness exercises. First, we analyzed the number of correct answers as an alternative measurement of knowledge (SI Appendix, Table A7). These results are similar to those using our binary measure as a dependent variable. Second, in SI Appendix, Tables A2–A6 we analyzed each of the 18 questions in isolation. The analyses by item are largely consistent with the results using the aggregated binary measure—namely those with higher income and education, and those who are older, male, and white tend to be more knowledgeable. Two exceptions are the results using the questions on plan standardization and benefits for undocumented immigrants, where income and education (the latter only in the case of the standardization question) do not predict knowledge. This might be explained by the fact that overall lack of knowledge seems to be particularly high for these two questions (Fig. 1).
Another surprising finding from the disaggregated analyses is the variation in sex difference in knowledge across questions. Although for every ACA question women do worse than men, the picture is less clear for health insurance literacy. In questions on provider restriction differences between HMOs and PPOs and deductible definition, women do significantly better than men; in questions about provider networks, generic drug pricing, and copayment they do just as well. The ACA knowledge results align with the findings from the financial literacy literature where women do consistently worse than men (7, 17); and the ones on health insurance literacy align with the literature on health literacy that suggests that women are more literate (18). The questions where we find women do better are related to use of the healthcare system, something women might experience earlier in life due to childbearing and childrearing, and therefore know more about.
Table 3 shows the results for expected changes in healthcare—the first two columns present results for the index of expected changes in five specific healthcare dimensions, and the last two for the overall change variable. Those with lower income, and who are uninsured, unmarried, Hispanic, and nonwhite are the most optimistic according to the specific dimensions index. Those living in blue states are more likely to expect improvements, and those in states with a federal or partnership exchange are less likely. Similarly, if we use the overall expectation variable, we find that uninsured, unmarried, nonwhite, and Hispanic respondents are the most optimistic. In addition, we find respondents in blue states, states with their own exchanges, and states that are likely to expand Medicaid to be more likely to expect improvements. Results for both outcomes are similar if an ordered logit model is used (columns 2 and 4).
Table 3.
Expected changes due to health reform
| Specific dimension | Overall | |||
| OLS | Ordered Logit | OLS | Ordered Logit | |
| (1) | (2) | (3) | (4) | |
| No health insurance | 0.341*** (0.103) | 0.274*** (0.083) | 0.114*** (0.032) | 0.313*** (0.089) |
| Income <100 of FPL | 0.470*** (0.140) | 0.355*** (0.114) | 0.102** (0.042) | 0.289** (0.123) |
| Income 100–250 of FPL | 0.313*** (0.119) | 0.227** (0.098) | 0.081** (0.036) | 0.231** (0.107) |
| Income 251–400 of FPL | 0.234** (0.119) | 0.184* (0.099) | 0.053 (0.036) | 0.170(0.107) |
| Younger than 26 | 0.264* (0.156) | 0.262** (0.130) | −0.110** (0.046) | −0.268* (0.138) |
| 26–44 | 0.054 (0.081) | 0.036 (0.067) | −0.025 (0.025) | −0.056(0.072) |
| Female | −0.018 (0.077) | −0.019 (0.063) | 0.004 (0.024) | 0.022 (0.069) |
| Not married | 0.332*** (0.080) | 0.271*** (0.066) | 0.093*** (0.025) | 0.268*** (0.072) |
| Nonwhite | 0.575*** (0.089) | 0.448*** (0.075) | 0.318*** (0.028) | 0.890*** (0.081) |
| Hispanic | 0.445*** (0.097) | 0.341*** (0.080) | 0.188*** (0.030) | 0.557*** (0.086) |
| No degree | −0.230 (0.175) | −0.239 (0.159) | −0.216*** (0.059) | −0.617*** (0.173) |
| High school or equivalent | −0.417*** (0.142) | −0.360*** (0.119) | −0.250*** (0.044) | −0.704*** (0.128) |
| Some college | −0.581*** (0.132) | −0.519*** (0.109) | −0.216*** (0.040) | −0.606*** (0.117) |
| Associate degree | −0.774*** (0.155) | −0.666*** (0.125) | −0.221*** (0.046) | −0.610*** (0.133) |
| Bachelor's degree | −0.488*** (0.131) | −0.432*** (0.107) | −0.129*** (0.041) | −0.373*** (0.115) |
| Fair/poor health | 0.033 (0.107) | 0.028 (0.087) | 0.011 (0.033) | 0.037 (0.094) |
| State likely to expand Medicaid | 0.150 (0.130) | 0.106 (0.109) | 0.108** (0.042) | 0.311*** (0.120) |
| Federal exchange | −0.243* (0.126) | −0.163 (0.107) | −0.032 (0.042) | −0.091 (0.118) |
| Partnership exchange | −0.424*** (0.132) | −0.313*** (0.108) | −0.187*** (0.040) | −0.511*** (0.119) |
| Blue state in 2012 election | 0.344*** (0.097) | 0.297*** (0.080) | 0.121*** (0.030) | 0.361*** (0.087) |
| Constant | −1.828*** (0.184) | −0.341*** (0.060) | ||
| Number of observations | 3414 | 3414 | 3414 | 3414 |
Coefficients and SEs after OLS and ordered logit estimation respectively. Estimates of cutpoints for ordered logit models not reported. Columns 1 and 2 use an index that averages information on expected changes in five different dimensions (access to care, quality of care, waiting times, out-of-pocket costs, and costs for emergency care) as dependent variables. The index counts 1 for improvement, 0 for no change, and −1 for deterioration. Columns 3 and 4 use expected overall changes for the family as dependent variables. 1 indicates that family will be better off, 0 not much change, and −1 that family will be worse off.
P < 0.10, **P < 0.05, ***P < 0.01.
Discussion
Overall knowledge about health reform and health insurance was low, suggesting that individuals were not well prepared for the changes under the ACA. Among the overall population, only one-quarter of respondents reported knowing a fair amount or a great deal about the ACA. One-half did not know about the new health insurance exchanges or their subsidies, and 42% could not correctly describe a deductible.
This lack of knowledge is even more acute among those at the bottom of the income distribution and among those currently uninsured. In addition, those with low incomes and who were uninsured had significantly lower levels of financial literacy (19), which has been linked to low levels of retirement planning, stock market participation, and wealth accumulation (20–22). Even after taking into account differences in potential confounders such as education, age, sex, and race, those in the lower income categories had significantly less knowledge about the ACA and health insurance than those in the top income category. Not having health insurance implied less objective health insurance knowledge. Knowledge about health insurance and the ACA did not vary systematically with state political leaning or the state’s stance on implementation of exchanges or expansion of Medicaid. However, respondents residing in blue states or states that implemented their own exchange were more optimistic in terms of the changes brought by the ACA. Moreover, uninsured, unmarried, nonwhite, and Hispanic respondents were more likely to expect health reform to improve healthcare.
The comparison of subjective and objective knowledge measures suggests that some groups were not as knowledgeable as they believed they were. With regard to knowledge about health insurance, this was true for unmarried, Hispanic, and uninsured respondents.
Conclusion
Clearly some of those most likely to be affected by ACA were ill prepared to navigate the new health insurance environment. Particularly worrisome is the lack of understanding among lower income families. This group is ineligible for Medicaid and could benefit from the exchanges. They appear at high risk of making poor decisions when shopping for health insurance. Given that this group was not well informed about the exchanges, they may miss out on the opportunity to obtain coverage (and possibly subsidies) and, as a result of the mandate, be penalized for the lack of health insurance. Moreover, even those who sign up for health insurance in the exchanges may not be equipped to make financially sound choices among different insurance products.
There are a few possible policy responses to the lack of health reform and health insurance knowledge, including simplified options, decision aids, and defaults. In the Medicare literature, there is evidence that plan standardization as well as providing simple and personalized plan information can lead to better plan choice (23, 24). Adding options to support better decision-making, such as the Centers for Medicare and Medicaid Services’ “Plan Finder” for Medicare Part D, is clearly valuable, but information on how to access and incentives to use such tools might be needed (5).
Defaults have not been discussed often in the context of health insurance choice—the literature focuses mostly on retirement savings decisions (25, 26). However, it is reasonable to expect that the findings of large default effects would translate to the context of health insurance choice, especially given the complex choice environment in the exchanges. For example, one common finding in the complexity literature is that if choices get complicated, people tend to avoid making them. They either do not choose at all, or they pick a simple alternative they can understand even if it is not optimal (25, 27–29). This suggests that the complexity of the health insurance choices themselves will reduce the number of people signing up in the exchanges and that providing simple alternatives may help.
One potential way to overcome the difficulties posed by the complex choice environment and the low knowledge, and still maintain competition among insurers in the exchanges, is to nudge consumers toward efficient, welfare-maximizing choices. The exchanges could, for example, present in a first screen the least costly silver, gold, and platinum coverage plans, leaving the presentation of other plans in these categories to subsequent screens. This would focus the attention of the insurers on premium competition for given coverage requirements, and would likely be procompetitive. Moreover, in the context of the exchanges where too much choice, particularly complex and ambiguous choice, combined with lack of basic knowledge can lead to confusion and use of inappropriate heuristics, such defaults that limit choice unless the consumer chooses to override the default, are probably welfare-increasing.
Supplementary Material
Acknowledgments
This research was supported in part by Grants P30AG24962 and P30AG024968, and a pilot grant from the Leonard D. Schaeffer Center for Health Policy & Economics at the University of Southern California. No sponsors had any input into the research.
Footnotes
Conflict of interest statement: The RAND Corporation is a not-for-profit research organization and has no commercial interest in the data used in this article. The data are freely available at https://mmicdata.rand.org/alp.
*This Direct Submission article had a prearranged editor.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1320488111/-/DCSupplemental.
References
- 1.Sinaiko AD, Hirth RA. Consumers, health insurance and dominated choices. J Health Econ. 2011;30(2):450–457. doi: 10.1016/j.jhealeco.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Heiss F, McFadden D, Winter J. Who failed to enroll in Medicare Part D, and why? Early results. Health Aff (Millwood) 2006;25(5):w344–w354. doi: 10.1377/hlthaff.25.w344. [DOI] [PubMed] [Google Scholar]
- 3.Goldman DP, Joyce GF. Medicare Part D: A successful start with room for improvement. JAMA, J Am Med Assoc. 2008;299(16):1954–1955. doi: 10.1001/jama.299.16.1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abaluck J, Gruber J. Choice inconsistencies among the elderly: Evidence from plan choice in the Medicare Part D program. Am Econ Rev. 2011;101(4):1180–1210. doi: 10.1257/aer.101.4.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heiss F, Leive A, McFadden D, Winter J. Plan selection in Medicare Part D: Evidence from administrative data. J Health Econ. 2013;32(6):1325–1344. doi: 10.1016/j.jhealeco.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loewenstein G, et al. Consumers’ misunderstanding of health insurance. J Health Econ. 2013;32(5):850–862. doi: 10.1016/j.jhealeco.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Lusardi A, Mitchell OS. Financial literacy around the world: An overview. J Pension Econ Finance. 2011;10(4):497–508. doi: 10.1017/S1474747211000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gutsche T, Kapteyn A, Meijer E, Weerman B. The RAND continuous 2012 presidential election poll. Public Opin Q. 2014 in press. [Google Scholar]
- 9.American Life Panel 2010. Well Being 365 [Internet]. Santa Monica, CA: RAND Corporation. Available from: http://mmicdata.rand.org/alp/index.php?page=data&p=showsurvey&syid=356.
- 10.King M, et al. 2010. Integrated Public Use Microdata Series, Current Population Survey: Version 3.0 (University of Minnesota, Minneapolis) [Machine-readable database]
- 11. Henry J Kaiser Family Foundation (March 2013) Kaiser Health Tracking Poll [Internet]. Available from: http://kaiserfamilyfoundation.files.wordpress.com/2013/03/8425-t1.pdf.
- 12.Winter J, et al. Medicare prescription drug coverage: Consumer information and preferences. Proc Natl Acad Sci USA. 2006;103(20):7929–7934. doi: 10.1073/pnas.0601837103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Investor FINRA Education Foundation (2009) Financial Capability in the United States [Internet]. Available from: http://www.finrafoundation.org/web/groups/foundation/@foundation/documents/foundation/p120536.pdf.
- 14.Manski CF. Measuring expectations. Econometrica. 2004;72:1329–1376. [Google Scholar]
- 15.Delavande A, Manski CF. Probabilistic polling and voting in the 2008 presidential election: Evidence from the American Life Panel. Public Opin Q. 2010;74:433–459. doi: 10.1093/poq/nfq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Henry J Kaiser Family Foundation (2013) Status of State Action on the Medicaid Expansion Decision [Internet]. Available from: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/
- 17.Lusardi A, Mitchell OS. Baby Boomer retirement security: The roles of planning, financial literacy, and housing wealth. J Monet Econ. 2007;54:205–224. [Google Scholar]
- 18.Gazmararian JA, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281(6):545–551. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 19. Bauhoff S, Carman K, Wupperman A (2013) Financial literacy and consumer choice of health insurance: Evidence from low-income populations in the United States. Santa Monica, CA: RAND. Available from: http://www.rand.org/pubs/working_papers/WR1013.
- 20.Lusardi A, Mitchell OS. Financial literacy and planning: Implications for retirement wellbeing. In: Lusardi A, Mitchell OS, editors. Financial Literacy: Implications for Retirement Security and the Financial Marketplace. Oxford, UK: Oxford Univ Press; 2012. pp. 17–39. [Google Scholar]
- 21.van Rooij M, Lusardi A, Alessie R. Financial literacy and stock market participation. J Financ Econ. 2011;101(2):449–472. [Google Scholar]
- 22.van Rooij M, Lusardi A, Alessie R. Financial literacy, retirement planning and household wealth. Econ J. 2012;122(560):449–478. [Google Scholar]
- 23.Rice T, Graham ML, Fox PD. The impact of policy standardization on the Medigap market. Inquiry. 1997;34(2):106–116. [PubMed] [Google Scholar]
- 24.Kling JR, Mullainathan S, Shafir E, Vermeulen LC, Wrobel MV. Comparison friction: Experimental evidence from Medicare drug plans. Q J Econ. 2012;127(1):199–235. doi: 10.1093/qje/qjr055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Madrian B, Shea DF. The power of suggestion: Inertia in 401(k) participation and savings behavior. Q J Econ. 2001;116(4):1149–1187. [Google Scholar]
- 26.Choi JJ, Laibson D, Madrian B, Metrick A. For better or worse: Default effects and 401(K) savings behavior. Perspectives on the Economics of Aging. In: Wise DA, editor. Chicago: Univ of Chicago Press; 2004. pp. 81–121. [Google Scholar]
- 27.Tversky A, Shafir E. Choice under conflict: The dynamics of deferred decision. Psychol Sci. 1992;3(6):358–361. [Google Scholar]
- 28.Dhar R. Context and task effects on choice deferral. Mark Lett. 1997;8(1):119–130. [Google Scholar]
- 29.Iyengar SS, Huberman G, Jiang W. How much choice is too much? Contributions to 401(k) retirement plans. In: Mitchell O, Utkus S, editors. Pension Design and Structure: New Lessons from Behavioral Finance. Oxford: Oxford Univ Press; 2004. pp. 83–95. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.