Abstract
Vomiting and hiccups can be due to peripheral or central causes. Neurological diseases causing vomiting and hiccups are due to lesions of medulla involving area postrema and nucleus tractus solitarius. Neuromyelitis optica (NMO) is one such disease which involves these structures. However refractory vomiting and hiccups as the presenting symptom of NMO is unusual. Here we report a patient with NMO in whom refractory vomiting and hiccups were the sole manifestation of the first attack. Diagnosis can be missed at this stage leading to delay in treatment and further complications. This case demonstrates the importance of considering NMO in any patient presenting with refractory vomiting and hiccups and with local and metabolic causes ruled out and linear medullary lesion on magnetic resonance imaging may indicate the diagnosis even when the classical clinical criteria are not met. Anti NMO antibody testing should be done and if positive appropriate treatment should be initiated to prevent further neurological damage.
Keywords: Aquaporin antibody, hiccups, intractable vomiting, neuromyelitis optica
Introduction
The definition of typical neuromyelitis optica (NMO) according to Wingerchuk's revised diagnostic criteria includes patients with optic neuritis, acute myelitis, and at least two of the following three supportive criteria: Longitudinally extensive spinal cord lesions contiguous over three or more vertebral segments; lack of brain lesions in the magnetic resonance imaging (MRI) fulfilling multiple sclerosis (MS) criteria at the disease onset and serum positivity for aquaporin (AQP-4) antibody.[1] With increasing knowledge about the role and specificity of AQP-4 antibody in this disorder spectrum of NMO has been recognized and usually it is thought to be relapsing disease rather than monophasic. However, many atypical presentations have been recognized like hypersomnia, intractable hiccups, nausea, and vomiting (symptoms lasting for more than 48 hours); transient asymptomatic elevation of creatine kinase levels; and painful tonic spasm during transverse myelitis recovery period.[2] Awareness of these atypical presentations may help in early diagnosis and proper management in the presence of other supportive criteria to prevent disability. We report a patient of NMO who initially had a presenting episode of intractable vomiting and hiccups and later on developed other attacks involving spinal cord and optic nerves.
Case Report
A 24-year-old lady developed recurrent projectile vomiting, 8-10 times/day for initial few days and 2-3 episodes/day later, associated with hiccups which used to come intermittently. Symptoms continued for 1.5 months. There were no other systemic or neurological complaints. Initially patient was seen by a general practitioner and was treated symptomatically. She did not experience weight loss, dehydration, or electrolyte disturbances as she was being treated with intravenous (IV) fluids. Later, she was evaluated by an ear, nose, and throat (ENT) specialist and a neurologist. A computed tomography (CT) scan was done which was normal again she was continued on symptomatic treatment. Later she was evaluated by another neurologist and MRI of brain was done, which showed T2/fluid attenuated inversion recovery (FLAIR) hyperintensity in periaqueductal grey matter of midbrain, midbrain tectum, medulla, and right temporal periventricular region [Figure 1a and b]. The diagnosis considered were Wernicke's encephalopathy/acute disseminated encephalomyelitis (ADEM). There were no symptoms/signs of encephalopathy. Electroencephalogram and lumbar puncture were not performed. Vomiting and hiccups stopped after a 5-day course of IV methylprednisolone (IVMP). She was continued on oral steroids 1 mg/kg (weight 62 kg) initially and later on tapered for 5-6 months and she was asymptomatic subsequently. Five months later (11 months after initial symptom) she developed numbness of the right upper limb followed by right lower limb without facial involvement over 2 weeks. There was no weakness of limbs and bowel bladder disturbances. She was again given 5-day course of IVMP, but there was no significant improvement. Oral steroids were not given. Patient was independent for her daily activities.
Figure 1.
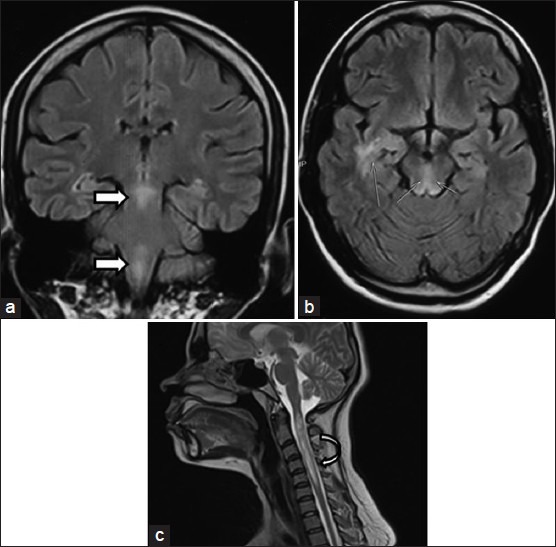
Fluid attenuated inversion recovery coronal sequence of brain (a) showing linear hyperintensity in periaqueductal grey of midbrain and central medulla (block arrow). Axial FLAIR magnetic resonance imaging of brain (b) showing hyperintensity in midbrain tectum and right temporal periventricular region (line arrows). Sagittal T2 weighted MRI of spine (c) done 2.5 years later showing longitudinally extensive transverse myelitis involving cervical cord (C1–C5 vertebral segment)
Three months later she developed bilateral visual loss which improved completely over 1 month following another course of IVMP. Oral steroids 1 mg/kg were given initially and gradually tapered over 1 year along with single dose of IV methylprednisolone injection every month. Later (2 years 2 months after onset of first symptom and 1.5 years of steroid therapy) she developed painful restriction of movements of left hip and imaging with MRI was done and was diagnosed to have avascular necrosis of femur both sides for which she underwent core decompression. Two and half years after the first symptom again she developed weakness of all four limbs requiring two person's support to walk, numbness below the neck, and urinary retention. This time she presented to our institute. MRI of spine showed longitudinally extensive transverse myelitis (LETM) involving first to fifth cervical vertebra [Figure 1c]. We considered the diagnosis of NMO. Her NMO antibody test was positive. Other autoantibodies were negative. Cerebrospinal fluid examination showed six lymphocytes and protein of 41 mg/dL. Human immunodeficiency virus (HIV) and venereal disease research laboratory (VDRL) tests were nonreactive. Vitamin B12 level was normal. She was treated with five cycles of large volume plasmapheresis and she made significant improvement (expanded disability status scale was 6.5 at the time of admission and it was 3.5 during last follow-up 2 months later). For immunomodulation, azathioprine has been started, after explaining the need, short and long term side effects.
Discussion
Vomiting and hiccups can be the manifestations of many systemic and neurological illnesses. Intractable nausea, vomiting, and hiccups (IHN) is defined as symptoms lasting more than 48 h.[3] Neurological illnesses reported to present with intractable vomiting and hiccups are lateral medullary stroke, bilateral carotid artery dissection, giant posterior inferior cerebellar artery aneurysm, basilar artery aneurysm, posterior fossa arteriovenous malformation, cerebellar hemangioblastoma, syringobulbia, compressive lesions of medulla oblongata including cavernoma, ependymoma, choroid plexus papilloma, and tuberculoma.[4,5]
Our patient had intractable vomiting and hiccups lasting for about 1.5 months as sole presenting symptoms with MRI showing characteristic area involvement as described above and these symptoms improved with IVMP. Other symptoms attributable to involvement of spinal cord and optic nerves developed only after 6 months. Thus, we conclude intractable vomiting and hiccups were the sole manifestations of the first attack of NMO in our patient. General practitioner had treated the patient presumptively as gastritis. First neurologist had apparently concluded non-neurological etiology based on normal CT scan. Second neurologist had considered the possibility of Wernicke's encephalopathy/ADEM after MRI. We had the advantage of evaluating the patient in later part of the natural course when the diagnosis was apparent because of involvement of spinal cord and optic nerves.
In a study from Mayo Clinic, 12% of the seropositive AQP-4 patients had intractable vomiting as the initial presenting symptom. The initial evaluation in 75% of them was gastroenterologic. Vomiting lasted for a median of 4 weeks (range: 2 days-80 weeks). Optic neuritis or transverse myelitis developed after vomiting onset in 11 of 12 patients after a median interval of 11 weeks. Among the 12 patients, seven satisfied the criteria for NMO at median of 48 months after the onset of vomiting.[6]
In another study, 15 of the 35 patients with NMO (43%) had episodes of IHN. The episode frequently preceded (54%) or accompanied (29%) myelitis or optic neuritis. In one of the patients, the titers of anti-AQP-4 antibody were remarkably increased when the intractable hiccup appeared. It was suggested that IHN could be a clinical marker for the early phase of an exacerbation and early initiation of therapy may prevent further neurological damage.[7]
Hiccup, nausea, and vomiting are thought to be caused by the lesions involving the dorsomedial medulla including the area postrema, nucleus tractus solitaries (NTS), the ventrolateral respiratory center, and the nucleus ambiguous.[4] MRI of our patient during the episode of IHN showed linear signal changes involving periaqueductal grey of midbrain and central medulla [Figure 1a]. Misu et al., have proposed that long and centrally located myelitis, a linear medullary lesion causing IHN may distinguish NMO from MS.[3] In their study involving NMO and MS patients, IHN was found in eight of 47 cases of relapsing NMO (17%) but in none in 130 cases of MS. In six cases, MRI detected linear medullary lesions involving the periventricular region including the area postrema and NTS.
In a neuropathologic study of brains of 15 patients with NMO, five patients with MS, eight neurologically normal subjects, six patients with NMO (40%), but no patients with MS or normal controls exhibited unilateral or bilateral lesions involving the area postrema and the medullary floor of the fourth ventricle.[8] Like other periventricular areas, the medullary floor of the fourth ventricle and area postrema express AQP-4 abundantly and are thus preferential targets for NMO lesions. The fenestrations in the blood brain barrier may facilitate the entrance of AQP-4-antibodies into this area and cause symptoms.[8] These neuropathologic findings suggest that area postrema may be a selective target of the disease process in NMO.
Conclusion
This case demonstrates the importance of recognizing intractable vomiting and hiccups as a presenting symptom in NMO. Vomiting can continue for protracted time without any other neurological deficits. Our patient developed other neurological symptoms 6 months later. Hence, NMO should be considered in any patient with intractable vomiting and hiccups with pericanal linear medullary signal changes. Further testing with NMO antibody may help in diagnosis of NMO to prevent subsequent neurological episodes.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006;66:1485–9. doi: 10.1212/01.wnl.0000216139.44259.74. [DOI] [PubMed] [Google Scholar]
- 2.Sato D, Fujihara K. Atypical presentations of neuromyelitis optica. Arq Neuropsiquiatr. 2011;69:824–8. doi: 10.1590/s0004-282x2011000600019. [DOI] [PubMed] [Google Scholar]
- 3.Misu T, Fujihara K, Nakashima I, Sato S, Itoyama Y. Intractable hiccup and nausea with periaqueductal lesions in neuromyelitis optica. Neurology. 2005;65:1479–82. doi: 10.1212/01.wnl.0000183151.19351.82. [DOI] [PubMed] [Google Scholar]
- 4.Amirjamshidi A, Abbassioun K, Parsa K. Hiccup and neurosurgeons: A report of 4 rare dorsal medullary compressive pathologies and review of the literature. Surg Neurol. 2007;67:395–402. doi: 10.1016/j.surneu.2006.10.070. [DOI] [PubMed] [Google Scholar]
- 5.Gambhir S, Singh A, Maindiratta B, Jaeger M, Darwish B, Sheridan M. Giant PICA aneurysm presenting as intractable hiccups. J Clin Neurosci. 2010;17:945–6. doi: 10.1016/j.jocn.2009.09.046. [DOI] [PubMed] [Google Scholar]
- 6.Apiwattanakul M, Popescu BF, Matiello M, Weinshenker BG, Lucchinetti CF, Lennon VA, et al. Intractable vomiting as the initial presentation of neuromyelitis optica. Ann Neurol. 2010;68:757–61. doi: 10.1002/ana.22121. [DOI] [PubMed] [Google Scholar]
- 7.Takahashi T, Miyazawa I, Misu T, Takano R, Nakashima I, Fujihara K, et al. Intractable hiccup and nausea in neuromyelitis optica with anti-aquaporin-4 antibody: A herald of acute exacerbations. J Neurol Neurosurg Psychiatry. 2008;79:1075–8. doi: 10.1136/jnnp.2008.145391. [DOI] [PubMed] [Google Scholar]
- 8.Popescu BF, Lennon VA, Parisi JE, Howe CL, Weigand SD, Cabrera-Gómez JA, et al. Neuromyelitis optica unique area postrema lesions: Nausea, vomiting, and pathogenic implications. Neurology. 2011;76:1229–37. doi: 10.1212/WNL.0b013e318214332c. [DOI] [PMC free article] [PubMed] [Google Scholar]


