Abstract
Vertebral hemangiomas are benign vascular tumors of the spine that remain asymptomatic in most cases and incidentally encountered on imaging. Rarely, altered hemodynamic and hormonal changes during pregnancy may expand these benign lesions resulting in severe cord compression. The management of symptomatic vertebral hemangioma during pregnancy is controversial as modalities like radiotherapy and embolization are not suitable and surgery during pregnancy has a risk of preterm labor. Few cases of pregnancy related symptomatic vertebral hemangioma with marked epidural component have been reported in the literature. We report a case of 23-year-old primigravida who developed rapidly progressive paraparesis at 28 weeks of gestation and spine magnetic resonance imaging (MRI) revealed upper thoracic vertebral hemangioma with extensive extra-osseous extension and spinal cord compression. Laminectomy and surgical decompression of the cord was performed at 32 weeks of the pregnancy. There was significant improvement in muscle power after a week of surgery. Six weeks postoperatively she delivered a full term normal baby with subsequent improvement of neurologic deficit. Repeat MRI of dorsal spine performed at 3 months postoperatively showed reduced posterior and anterior epidural components of vertebral hemangioma.
Keywords: Epidural extension, laminectomy, pregnancy, spinal cord compression, vertebral hemangioma
Introduction
Vertebral hemangiomas are the most common benign tumors of the spine and occur in approximately 10-12% of the general population.[1] In most cases the lesion remains asymptomatic and incidentally encountered on imaging. The tumors are usually solitary and located in the lower thoracic and lumbar vertebra and less often in the cervical spine.[2] In rare circumstances like during pregnancy, these lesions may increase in size and produce symptoms in the form of local bony pain, radicular pain or compressive myelopathy.[2] There are few published case reports in literature regarding pregnancy related symptomatic vertebral hemangiomas with marked epidural component and only nine cases have been reported which were surgically managed during pregnancy.[2,3] Here we describe a pregnant female with symptomatic thoracic vertebral hemangioma with extradural extension that was successfully treated antepartum by laminectomy and tumor decompression.
Case Report
A 23-year-old primigravida presented at 28 weeks of gestation with progressive asymmetric weakness of both lower limbs for last 15 days. She also complained of diminished sensation over the lower limbs, along with plaster cast like sensation over the lower limbs and band like feeling at lower chest. She had no back or radicular pain, visual complain, urinary or bowel symptoms. There was no history of trauma, fever, weight loss or anorexia. Past and personal history was non-contributory. General physical examination including the spine was normal. Neurological examination revealed mild spasticity in lower limbs; motor power in left lower limb was Medical Research Council grade 4/5 and in right lower limb was 4/5 except at the ankle dorsiflexors where it was 2/5. Deep tendon reflexes in both lower extremities were brisk, abdominal reflex was absent and had bilateral extensor planter reflex. Sensory examination showed impaired sensation for touch and pain with a sensory level at D10 (spinal segment) and zone of hyperesthesia at D8 spinal segmental level. Posterior column sensations were impaired in both lower limbs and Romberg's sign was positive. Other systemic examination was unremarkable. A working diagnosis of compressive myelopathy (compression at D4-5 vertebral level) was considered.
Complete hemogram, erythrocyte sedimentation rate, coagulation tests, blood glucose, renal and liver function tests were normal. Ultrasound of abdomen revealed 28 weeks single live intrauterine fetus. Magnetic resonance imaging (MRI) of dorsal spine showed marrow signal alteration in D3-D5 vertebral bodies and associated para-vertebral and posterior epidural extension compressing the spinal cord. Any osseous destruction or collapse of the involved vertebrae was not evident. The MRI findings were consistent with vertebral hemangioma with paravertebral-epidural component [Figure 1a, b and d].
Figure 1.

(a and b) preoperative magnetic resonance imaging T1 and T2W saggital images revealing altered marrow signals in D3 to D5 vertebrae appearing hypointense on T1W along with patchy hyperintensities and hyperintense signal on T2W sequence with marked epidural component and cord compression (d) T2 axial image, D4 vertebra showing paravertebral and posterior epidural component displacing cord anteriorly, (c) and (e) postoperative T1W post-gadolinium sagittal and axial images showing intense enhancement of lesion with significantly reduced epidural component and spinal cord compression
Patient was advised for surgery; however, she declined for it. When her weakness further worsened over next 3 weeks leading to paraplegia and bladder disturbance, she agreed for the surgery. Although the lesion was confined to three vertebrae, the epidural component was relatively more extensive, hence extended laminectomy at D1-5 vertebrae and tumor decompression was done. Histopathology of tumor tissue was also suggestive of hemangioma [Figure 2]. Post-operative ultrasonography showed 32 weeks live intrauterine fetus. There was significant improvement in motor deficit after a week of surgery and she was able to stand with support. Four weeks post-operatively she was able to walk with minimal assistance and also regained normal urinary bladder function. Six weeks postoperatively she delivered a full term normal baby by elective lower segment caesarean section. After delivery there was further clinical improvement and at 3 months follow-up she had minimal residual deficit with brisk deep tendon reflexes in lower limbs and normal sensory examination. Repeat MRI of dorsal spine at 3 months postoperatively showed reduced epidural component of vertebral hemangioma [Figure 1c and e].
Figure 2.
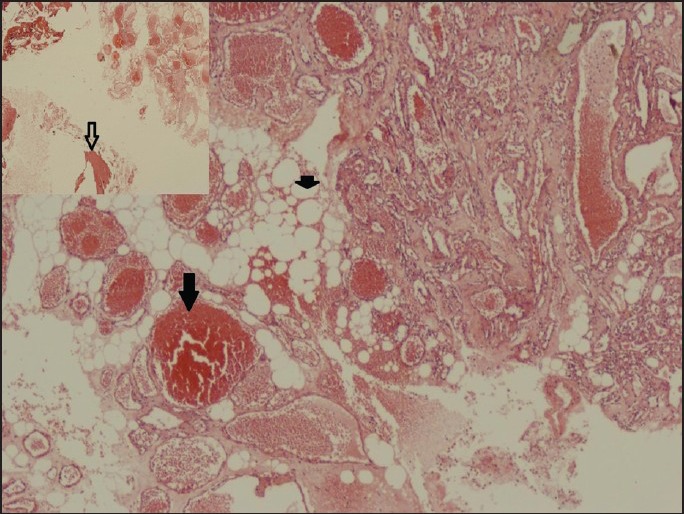
Histology from biopsy of the tumor tissue showing varying size thin-walled blood vessels mainly blood filled capillaries (filled arrow) along with fatty tissue (small filled arrow). A bony spicule is also evident (empty arrow, inset image). Findings consistent with osseous hemangioma (H and E, ×10) (inset ×2)
Discussion
Vertebral hemangiomas are the commonest benign vascular tumors of the spine and probably are due to an embryonic dysraphic disturbance.[2] Symptomatic vertebral hemangiomas are extremely rare and constitute <1% of all spinal hemangiomas. Vertebral hemangiomas were first described by Virchow in 1867 and Balado first time described pregnancy related symptomatic hemangioma.[3] Subsequently few cases of pregnancy related vertebral hemangiomas have been published in the literature.[3,4] Similar to our case, most of the pregnancy related vertebral hemangiomas became symptomatic during third trimester in previous reports and occurred more frequently in the upper thoracic regions. Postpartum improvement of neurologic deficit has been reported in symptomatic cases. The neurological manifestations may be caused by various mechanisms including: (1) Vascular expansion of involved vertebrae or posterior elements resulting in the spinal canal narrowing (2) subperiostial growth of the haemangioma with epidural extension and spinal cord compression (3) compression fracture of the involved vertebral body (4) hemorrhage into the epidural sac (5) spinal cord ischemia.[3,5]
The vascular, hemodynamic and endocrinal changes in pregnancy have role in increasing the size of pre-existing hemangioma. The compression of the inferior vena cava (IVC) caused by gravid uterus hampers the blood flow from the paravertebral veins into the IVC and increased blood flow through the vertebral venous plexus results in the expansion of preexisting vertebral hemangiomas. High progesterone level and increased plasma volume during pregnancy may further increase venous channel distension and endothelial proliferative effects of estrogen are other contributors in pathogenesis of hemangioma enlargement.[4]
Classic radiological features of vertebral hemangiomas on plain X-ray spine or computed tomography (CT) scan consist of coarse vertical striations and thick traberculae producing a honeycomb appearance.[3] Although, bony structures are well visualized on CT scan, epidural extension and cord compression can be best delineated on MRI and is also the preferred imaging modality during pregnancy. Asymptomatic vertebral hemangiomas because of their high fat content usually have high signal intensity on spin-echo T1 weighted and T2 weighted images. MRI of the symptomatic or aggressive vertebral hemangiomas typically shows intermediate or low soft tissue signal on T1 weighted and increased signal on T2 weighted images. An extradural component usually appears isointense but fatty component of the tumor may produce hyperintense signal intensities on T1 weighted images.[3]
In general, the management options for symptomatic vertebral hemangioma include surgical decompression, endovascular embolization, sclerosants like absolute alcohol or methyl methacrylate injection into the vertebral body and radiotherapy.[4] However, the treatment of symptomatic vertebral hemangioma during pregnancy is debatable. Radiotherapy and embolization carries high risk to the fetus and are not suitable during pregnancy. Although, no class I recommendation is available regarding management, based on the review of previously reported cases, an algorithm has been suggested by Chi et al.[4] Observation is recommended for patients at 36 weeks of gestation or later and if neurological deficit worsens, induction of labor followed by management of the lesion may be considered. Between 32 and 36 weeks of gestation, expectant observation is recommended and surgical decompression is reserved for patients with severe neurologic deficit. For patients in whom gestation is less than 32 weeks, antepartum surgical intervention may be considered for those who are severely symptomatic. Thus, surgery is usually not recommended at any gestational week if symptoms are mild or moderate and progressive or severe neurologic deficit is main indication for surgical decompression. However, there is increased risk of preterm labor and profuse bleeding if surgery is performed antepartum. Nine patients have been reported in the English literature, which were surgically managed antepartum. Seven patients underwent laminectomy and two had a vertebrectomy and fusion. Out of seven, five patients which were treated with laminectomy had a favorable outcome. Another two patients who underwent vertebrectomy also had good outcome.[3] Laminectomy and tumor decompression was done in our patient as her neurological deficit progressed rapidly. Vertebral stabilization was not performed as the there was no evident pathological fracture of the vertebral body. Postpartum reversals of hemodynamic and endocrinal changes of pregnancy were the other important factors which also contributed to significant improvement.
Conclusion
Although vertebral hemangiomas remain quiescent in most cases, pregnancy related expansion of the lesion and extra-osseous extension may lead to severe neurological deficit and this differential diagnosis should be considered while evaluating a case of compressive myelopathy especially during pregnancy. Pregnancy related symptomatic vertebral hemangiomas with rapidly progressive or severe neurologic deficit due to cord compression are candidates for immediate surgical decompression.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Fox MW, Onofrio BM. The natural history and management of symptomatic and asymptomatic vertebral hemangiomas. J Neurosurg. 1993;78:36–45. doi: 10.3171/jns.1993.78.1.0036. [DOI] [PubMed] [Google Scholar]
- 2.Lavi E, Jamieson DG, Granat M. Epidural haemangiomas during pregnancy. J Neurol Neurosurg Psychiatry. 1986;49:709–12. doi: 10.1136/jnnp.49.6.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vijay K, Shetty AP, Rajasekaran S. Symptomatic vertebral hemangioma in pregnancy treated antepartum. A case report with review of literature. Eur Spine J. 2008;17(Suppl 2):S299–303. doi: 10.1007/s00586-008-0592-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chi JH, Manley GT, Chou D. Pregnancy-related vertebral hemangioma. Case report, review of the literature, and management algorithm. Neurosurg Focus. 2005;19:E7. doi: 10.3171/foc.2005.19.3.8. [DOI] [PubMed] [Google Scholar]
- 5.Robbins LR, Fountain EM. Hemangioma of cervical vertebras with spinal-cord compression. N Engl J Med. 1958;258:685–7. doi: 10.1056/NEJM195804032581403. [DOI] [PubMed] [Google Scholar]


