Abstract
The inability to successfully treat women with ovarian cancer is due in large part to the advanced stage of disease at diagnosis, the development of platinum resistance, and the lack of sensitive methods to monitor tumor progression and response to treatment. Vascular cell adhesion molecule-1 (VCAM-1) is expressed on the mesothelium of ovarian cancer patients. We investigated VCAM-1 expression as a marker of peritoneal metastasis and tumor response to platinum-based chemotherapy.
Methods
Peritoneal or omental biopsies obtained from women diagnosed with Stage I, Stage II or Stage III/IV ovarian cancer were evaluated by immunohistochemistry. The effects of carboplatin on mesothelial VCAM-1 expression were determined in cultured cells by Western blot. Radiolabeled VCAM-1-specific peptide imaging probes and single photon emission computed tomography (SPECT) were employed in a mouse model of ovarian cancer peritoneal metastasis to identify VCAM-1 as a viable imaging target.
Results
VCAM-1 expression correlated with tumor stage. All specimens from Stage I patients were negative, while 29% of Stage II patients and the 73% of Stage III/IV patients were positive. While the majority of women with advanced stage disease expressed VCAM-1, the incidence of expression was reduced among women who received neoadjuvant chemotherapy, suggesting a role for chemotherapy in regulating VCAM-1 expression. Treatment of mesothelial cells in culture with carboplatin resulted in a transient decrease in VCAM-1 expression 4 hours after treatment that returned to baseline within 16 to 24 hours. In vivo imaging of VCAM-1 also demonstrated an acute decrease in expression 4 hours after carboplatin administration that recovered within 48 hours in mice harboring platinum-resistant tumors. Chronic VCAM-1 expression reflected the effect of platinum-based treatment on tumor burden. Specifically, carboplatin treatment of mice with platinum-sensitive tumors showed reduced VCAM-1 expression, which correlated with reduced tumor burden; mice with platinum-resistant tumors retained elevated VCAM-1 expression and tumor burden following treatment.
Conclusions
Clinically relevant VCAM-1-specific imaging probes identify VCAM-1 expression as an indicator of ovarian cancer peritoneal metastasis and therapeutic response to platinum-based agents. These observations support testing the utility of VCAM-1 imaging probes to monitor treatment response in ovarian cancer patients, thus providing the potential to improve management of women with this disease.
Keywords: VCAM-1, ovarian cancer, metastasis, SPECT/CT imaging
INTRODUCTION
Ovarian cancer is the most lethal gynecologic malignancy with an overall 5-year survival of 30–40% (1). This statistic is somewhat misleading because women with early stage ovarian cancer account for about 30% of diagnoses and enjoy a 5-year survival of >70%; however, 70% of ovarian cancer patients are diagnosed with advanced stage metastatic disease and suffer a 5-year survival of <30%. Stage III ovarian cancer, characterized by extensive spread throughout the peritoneal cavity, is diagnosed in 55% of patients and Stage IV, which includes the extensive peritoneal spread that identifies Stage III disease as well as hematogenous metastasis to distant organs including lung and liver, occurs in 15% of patients.
The unfavorable prognosis for women with advanced stage ovarian cancer is due in large part to the existence or development of platinum-resistant disease. The current standard of care in the US for women with advanced ovarian cancer is upfront surgical cytoreduction followed by systemic platinum/taxane based chemotherapy (2). While extensive retrospective data support aggressive surgery as important in improving overall survival (3), some will present with disease that is not resectable (for example, intra-parenchymal liver metastases) or will be too medically ill to undergo surgery safely, without significant morbidity. In these cases neoadjuvant chemotherapy has been shown to allow optimal cytoreduction without significant morbidity (4). Unfortunately, as many as 20% of women in either scenario (i.e., upfront surgery or neoadjuvant chemotherapy) will not achieve first remission, and some will suffer disease progression during primary therapy. Up to 90% of women who entered remission will recur through a process that is poorly understood and succumb to platinum-resistant disease within 2–3 years. Currently, it is not possible to identify patients pre-operatively who will respond to primary therapy. Moreover, patients with platinum resistant disease are identified only after failure to respond to therapy; the definition of platinum sensitivity is based largely on retrospective data.
Presently, CA125, the only marker for ovarian cancer, is approved for use to assess treatment response. However, levels of CA125 are not predictive of successful cytoreduction. Moreover, some patients will experience recurrence without a rise in CA125, and recent data suggest that rising CA125 in the setting of recurrent disease is not useful in identifying the appropriate time to start treatment (5). Finally, it has been noted that the traditional disease response to treatment as measured by CT scan and CA125 may not apply to the newer biologic therapies (6). There is therefore a need to identify new markers and to develop technologies to guide treatment decisions at different phases of this disease (7).
We identified vascular cell adhesion molecule-1 (VCAM-1) as a regulator of ovarian cancer peritoneal metastasis. Importantly, VCAM-1 is expressed preferentially on the mesothelium of ovarian cancer patients compared to women with benign disease (8). Furthermore, inhibition of VCAM-1 function decreases mesothelial invasion, diminishes tumor burden and increases survival in a mouse model of metastatic ovarian cancer (8). Therefore, we tested the hypothesis that VCAM-1 is a marker of peritoneal metastasis and tumor response to platinum-based chemotherapy. Moreover, we used a VCAM-1 targeted Single Photon Computed Tomography (SPECT) based contrast agent to provide proof of principle data to support the clinical use of VCAM-1 imaging probes to monitor women treated for ovarian cancer.
MATERIALS AND METHODS
Patients
A retrospective review of patient data was performed with Institutional Review Board approval and meets the criteria for waiver of consent under 45CFR46.116 and 45CFR164.512(i)(2). Medical records of 58 epithelial ovarian cancer patients undergoing treatment at the University of Virginia (UVA) between 1998 and 2010 were retrospectively reviewed and clinicopathologic data including stage at diagnosis, grade, histology, treatment regimen, and degree of surgical cytoreduction obtained (Table 1). Among the 58 patients identified, 2 were excluded due to incomplete medical records, and 9 excluded due to inadequate tissue or staining.
Table 1.
Patient Demographic Data
| Patient Characteristics | Stage I/II | Stage III/IV | p-value |
|---|---|---|---|
| Number | 26 | 30 | -------- |
| Age (median) | 56 | 60 | ns |
| Histology (%) | |||
| Serous | 10 (38) | 25 (83) | <0.001 |
| Endometrioid | 7 (27) | 1 (3) | |
| Mucinous | 2 (8) | 1 (3) | |
| Clear Cell | 4 (15) | 2 (7) | |
| Mixed | 3 (12) | --- | |
| Carcinosarcoma | --- | 1 (3) | |
| Other | --- | --- | |
| Treatment Approach (%) | |||
| Primary Surgery | 25 (96) | 26 (87) | -------- |
| NACTa | 1 (4) | 4 (13) | |
| Surgical Cytoreduction (%) | |||
| Optimal | 26 (100) | 18 (60) | -------- |
| Suboptimal | 0 (0) | 9 (30) | |
Neoadjuvant chemotherapy
With additional IRB approval, a separate set of 32 patients with advanced stage disease based on treatment modality, i.e., neoadjuvant chemotherapy (NACT) or primary surgical cytoreduction was identified; one patient was excluded due to inadequate cellular material with equivocal staining.
VCAM-1 IHC
Archived paraffin tissue blocks corresponding to each patient were obtained, sectioned and stained for VCAM-1 by the Biorepository Tissue Research Facility at UVA using human-specific anti-VCAM-1 antibodies (Abcam) according to the manufacturer’s instruction. Expression was scored as positive (>50%) or negative (<50%) with 3+ intensity. Immunohistochemical staining of mouse tissue was performed by the Pathology Core at the UVA using anti-VCAM antibody specific for mouse (Santa Cruz, SC-1504) at 5 ug/ml concentration.
Cell Lines
SKOV3ip1 cells, a platinum-resistant human ovarian cancer cell line, were grown in RPMI1640 supplemented with 15% fetal bovine serum (FBS). A2780 (platinum sensitive) and A2780Cis (platinum resistant) ovarian cancer cells were grown in RPMI1640 supplemented with 10% FBS, 2 mM L-glutamine and for the A2780Cis, 1 μM cisplatin every 2–3 passages. LP9 mesothelial cells (Coriell Repository) were grown in 1:1 Medium 199 in Earle BSS:MCDB110 supplemented with 15% FBS, 2 mM L-glutamine, 10 ng/ml EGF and 0.4 μg/ml hydrocortisone.
Western Blot Analysis
LP9 cells treated with increasing concentrations of carboplatin (UVA pharmacy) up to 1 μg/ml for 24 hours or with 1 μg/ml for increasing periods of time up to 72 hours were lysed in supplemented RIPA buffer (50 mM Hepes, 0.15 M NaCl, 2 mM EDTA, 0.1% Nonidet P 40, and 0.05% sodium deoxycholate, pH 7.2) containing protease inhibitors (Roche protease cocktail) and 1 mM Na3VO4, 40 mM NaF, and 10 mM Na4P2O7. Proteins (10–25 μg of lysate) were resolved on 8% SDS-PAGE gels, transferred to nitrocellulose, and blotted with anti-human VCAM-1 or anti-actin antibodies followed by incubation with HRP-conjugated secondary antibodies and visualization by ECL (Amersham Biosciences). Films were scanned and VCAM-1 signal intensity determined using ImageJ and normalizing the VCAM-1 signal to actin for each sample.
Quantitative RT-PCR
RNA was extracted from treated LP9 cells using TRIzol reagent (Invitrogen) and cDNA generated with iScript cDNA synthesis kit (Bio-Rad). Quantitative RT-PCR was performed using the Step One Plus Real-Time PCR system (Applied Biosystems), primers specific for human VCAM-1 - Forward, CTTAAAATGCCTGGGAAGATGGT and Reverse, GTCAATGAGACGGAGTCACCAAT, or glucuronidase beta (GUSB; internal PCR control) - Forward, CCGACTTCTCTGACAACCGAC and Reverse, AGCCGACAAAATGCCGCAGACG – and Absolute Blue Syber Green ROX mix (Thermo Scientific). Data were analyzed using the Δ-Δ CT method.
VCAM-1 Peptide
Synthesis of a SPECT imaging agent with specificity for VCAM-1 has been previously described (9–11). A tetrameric VCAM-1 targeted peptide (tVCAM-4 (βAKTLLPTPGGS(PEG5000))KKKDOTAβA-NH2)) (11) was synthesized (CS Bio Company, Menlo Park, CA) for SPECT/CT imaging by chelating radioactive indium to the DOTA. For Indium labeling, the peptide (100 μg) was dissolved in 20 μl PBS and then diluted in 300 μl ammonium acetate buffer (0.1M, pH 5.5). Indium chloride (5mCi in water; Cardinal Health, VA) was mixed with the peptide and allowed to equilibrate with mixing at 40°C for 10 min.
Animal Models
All mouse experiments were performed in accordance with the policies and procedures established by the University of Virginia Animal Care and Use Committee. NCR nude mice (Taconic Laboratories) were injected intraperitoneally with 106 SKOV3ip1 (platinum resistant), A2780 (platinum sensitive; Sigma-Aldrich, Inc.) or A2780Cis (platinum resistant; Sigma-Aldrich, Inc.) cells suspended in 200 μL phosphate-buffered saline (PBS) as previously described (8). Control nude mice received a single IP injection of 200 μL PBS. Two, 3 and 4 weeks after SKOV3ip1 cell injection (n=3 per group), mice were imaged, euthanized and biodistribution of the labeled tetrameric synthetic peptide assessed. To evaluate VCAM-1 as a marker of chemosensitivity, a cohort of mice (n=9) was injected with SKOV3ip1 cells. Groups of 3 mice were imaged 2 weeks after tumor initiation, 8 hours after a single IP injection of 25 mg/kg carboplatin (administered 2 weeks after tumor initiation) or 2 days after carboplatin injection. Following each imaging session mice were euthanized and probe biodistribution determined. To evaluate the effects of long-term exposure to chemotherapy on VCAM-1 expression, one group of mice (n=9) was injected with A2780 (platinum sensitive cell line) and another (n=9) with A2780Cis (platinum resistant cell line). Mice were treated with 25 mg/kg carboplatin beginning 1 week after tumor initiation and continuing weekly thereafter. Cohorts of 3 mice per cell line were imaged one week after tumor initiation, just prior to treatment (week 0), then 1 and 2 weeks after initiation of treatment and 111In-tVCAM-4 uptake quantified via biodistribution.
Peptide Chelation
For indium labeling the peptide (100 µg) was dissolved in 10µl PBS, then for every 5mCi of indium, 5 µl was removed and added to an eppendorf tube containing 500µl ammonium acetate buffer (0.1M, pH 5.5). Indium chloride (Cardinal Health, VA) was added to the tub containing the peptide/ammonium acetate buffer and mixed in a thermomixer (1000 RPM, 40°C) for 10 minutes. After which the chelated peptide is removed and assessed for radiochemical purity using a Seppak (Waters Corp, MA), to pass RCP = ≥90% purity.
Imaging
Mice were injected with 1 mCi of 111In labeled tVCAM-4 (11) then imaged 4 hours after injection with a microSPECT/CT scanner designed and built at UVa. Computed tomography (CT) acquisition used 200 evenly spaced projections spanning 200 degrees over approximately 5 minutes. Pinhole single photon emission computed tomography (SPECT) scanning was then performed using 2 opposing gamma cameras simultaneously. The 2 cameras were fitted with 0.5 mm diameter tungsten pinholes. Sixty evenly spaced projection views per camera were obtained over 180 degrees, for a total of 120 views at 3-degree increments over 360 degrees. The SPECT acquisition time was approximately 45 minutes. The reconstructed CT voxel size was 0.082 × 0.082 × 0.082 mm on a 640 × 640 × 768 image matrix. The reconstructed SPECT voxel size was 0.65 × 0.65 × 0.65 mm on an 80 × 80 × 80 image matrix. All SPECT images were corrected for radioactivity decay but not for gamma ray attenuation.
Biodistribution
After mice were imaged via SPECT/CT, animals were sacrificed and their organs harvested and placed into pre-weighed Eppendorf tubes. Each tube was then reweighed to determine the weight of the organ and the radiation measured using a gamma counter. Data represent the mean ± standard deviation and are presented as dose injected per gram of tissue.
Statistical Analysis
The significance of mesothelial VCAM-1 expression in patients was analyzed using Chi-squared and Fisher exact tests. Animal experiments were analyzed using ANOVA followed by Bonferroni Correction for all combinations.
RESULTS
VCAM-1 is expressed preferentially on the mesothelium of ovarian cancer patients compared to women with benign disease (8), and inhibition of VCAM-1 function decreases mesothelial invasion, diminishes tumor burden and increases survival in a mouse model of metastatic ovarian cancer (8). Since mesothelial VCAM-1 regulates ovarian cancer metastasis, we examined the relationship between expression and tumor progression in an attempt to determine whether it would function as a marker of progression. Therefore, the association between peritoneal VCAM-1 expression and clinical parameters of disease including tumor stage, optimal cytoreduction, time to recurrence and overall outcome were investigated (Table 1). There was no significant difference in age or treatment approach between early (Stage I/II) and late (Stage III/IV) stage disease. As expected, the majority of late stage patients were diagnosed with serous papillary histological subtype and a greater proportion of them were sub-optimally cytoreduced (Table 1).
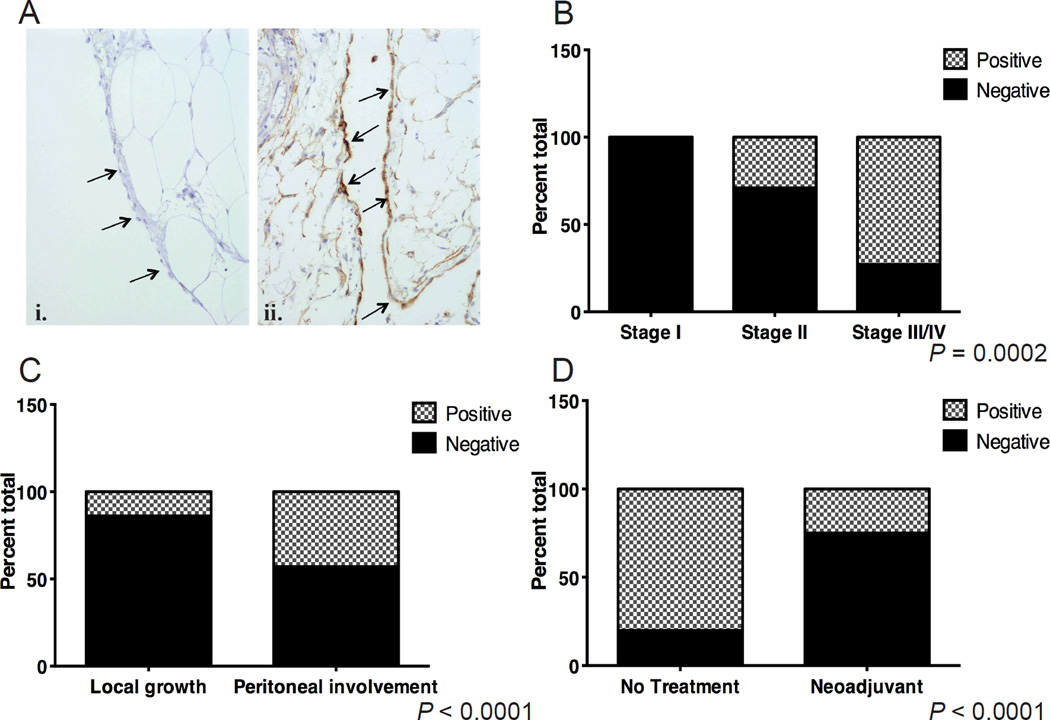
Biopsies of the peritoneum or omentum were examined for mesothelial VCAM-1 expression following IHC staining (Figure 1A). The incidence of VCAM-1 expression increased with tumor stage. None of the women diagnosed with Stage I ovarian cancer expressed VCAM-1, while VCAM-1 was detected in 4 of 14 (29%) Stage II patients and 16 of 22 (73%) of those with advanced stage (III/IV) disease (Figure 1B). To understand the discrepancies in VCAM-1 expression among Stage II or Stage III/IV patients, additional clinical and pathological features were reviewed. Stage II ovarian cancer is defined as spread within the pelvis (2). This definition includes the development of large tumors encompassing the primary site and adjacent tissues or the establishment of secondary tumor implants within the pelvis. Among the Stage II patients, 7 had secondary implants and 3 of those showed VCAM-1 expression; only 1 patient with adnexa-only disease showed VCAM-1 positivity (Figure 1C). Similarly, the majority of women with Stage III/IV disease, which is characterized by extensive implantation of tumors within the entire peritoneal cavity, expressed VCAM-1 (16 of 22, Figure 1B). These findings indicate that VCAM-1 expression is associated with peritoneal metastasis and expression is evident at the earliest indication of secondary tumor formation.
Figure 1. Peritoneal VCAM-1 expression among women with ovarian cancer.
(A) Representative histology of biopsies stained for VCAM-1 expression. Arrows indicate mesothelium. i, example of negative staining; ii, brown staining of mesothelium indicates positive reactivity. (B) Incidence of women with positive VCAM-1 staining of the mesothelium segregated by tumor stage. Omentum or peritoneal biopsies were stained for VCAM-1 using IHC. Specimens were scored positive if >50% of the mesothelial cells showed 3+ reactivity (stippled bars) or negative if <50% of the cells showed reactivity (solid grey). Data represent percent of total patients analyzed (P = 0.0002, Chi-squared test). Stage I, n=12, Stage II, n=14, Stage III/IV, n=22. (C) Percentage of specimens with VCAM-1 positivity among Stage II patients separated based on presence (peritoneal involvement, n=7) or absence (local growth, n=7) of secondary tumor implants within the pelvis (P < 0.0001, Fisher’s Exact test). (D) Percentage of VCAM-1 staining specimens from a set of matched Stage III patients who received upfront surgery (no treatment, n=18) or neoadjuvant chemotherapy (NACT, n=13) (P < 0.0001, Fisher’s Exact test).
Among the patients with Stage III/IV ovarian cancer, 6 of the 22 stained specimens lacked VCAM-1 reactivity. Evaluation of the clinical data from the Stage III/IV patients indicated that 18% (4 of 22) received neoadjuvant chemotherapy (Table 1), an option provided to women with excessive tumor burden in an attempt to optimize the chances of successful cytoreductive surgery. Interestingly, VCAM-1 staining was observed in just 1 patient who received neoadjuvant chemotherapy (data not shown). To more thoroughly evaluate the possibility that neoadjuvant chemotherapy alters VCAM-1 expression, a second set of patients including 18 undergoing primary cytoreductive surgery and 13 undergoing interval cytoreduction after neoadjuvant chemotherapy were evaluated. Analysis revealed significantly fewer women with mesothelial VCAM-1 expression following exposure to neoadjuvant chemotherapy as compared to primary surgery (15% (2 of 13) compared to 72% (13 of 18), respectively) (Figure 1D). Together, these observations indicate that in addition to the presence of VCAM-1 at the earliest stages of peritoneal spread (i.e., Stage II patients with secondary implants), expression is responsive to treatment. This observation implies that VCAM-1 is regulated directly by platinum agents. Alternatively, since neoadjuvant chemotherapy is provided to reduce tumor burden, its effect on VCAM-1 expression might not be direct but rather a result of the loss of tumor, thus offering the tantalizing hypothesis that VCAM-1 could be used to reflect tumor burden and identify patients responding to platinum-based treatment.
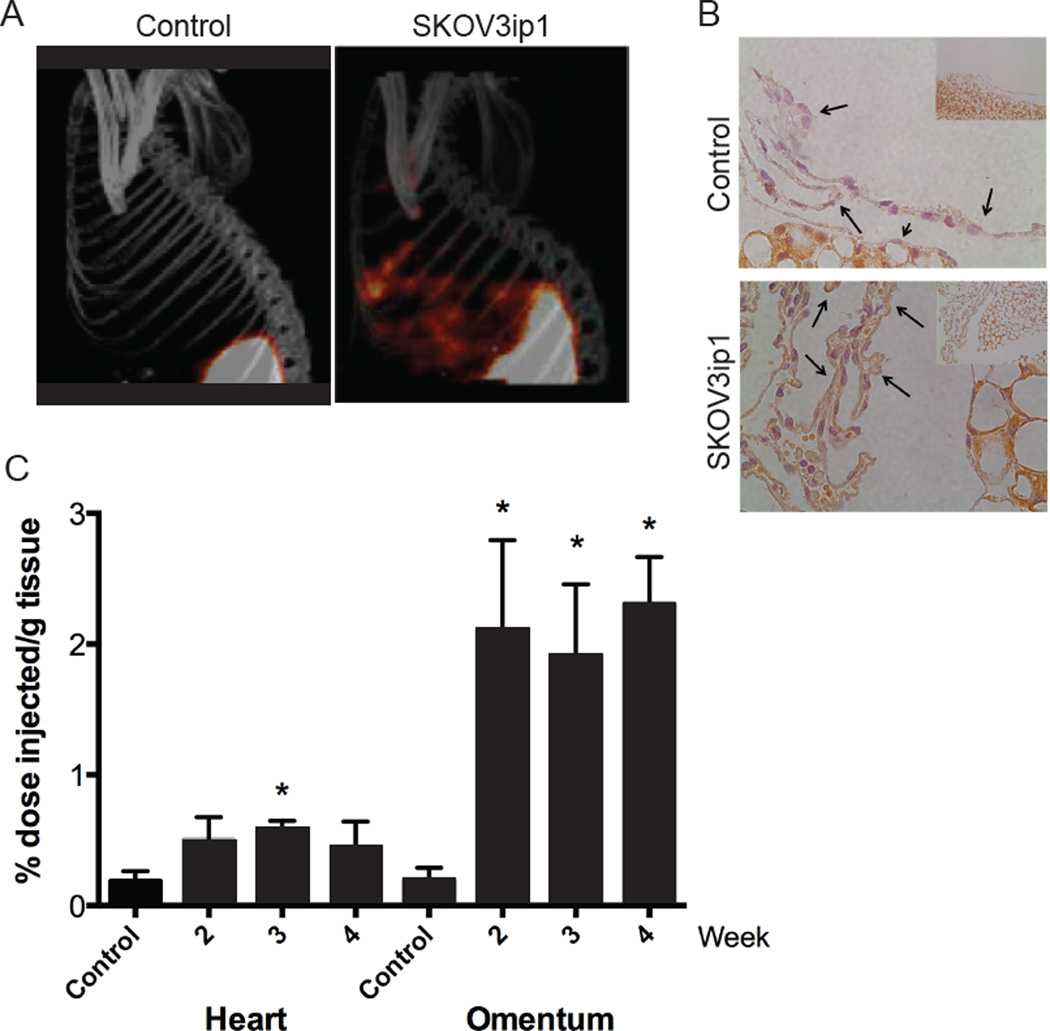
These possibilities were tested directly in a mouse model of peritoneal ovarian cancer metastasis using SPECT/CT with a VCAM-1-targeted 111Indium-labeled imaging agent (111In-tVCAM-4) (9–13). Previous work has demonstrated the specificity and high affinity of tVCAM-4 for VCAM-1 (11). Similar to the reported pharmacokinetic data for this probe, we observed the highest accumulation of probe in the kidney 4 hours post-injection (Supplemental Table). Using IHC, we previously reported that VCAM-1 is expressed on the mesothelium of tumor-bearing mice within 2 weeks of tumor initiation, a time when tumors are microscopic (8). Therefore, mice were injected intraperitoneally with SKOV3ip1 cells and imaged 2 weeks later using 111In-tVCAM-4 and SPECT/CT (Figure 2, Supplemental Figure 1). Imaging of tumor-bearing mice demonstrated diffuse intraperitoneal labeling in regions consistent with the omentum and mesentery (Figure 2A), primary sites of metastasis in the mouse model. In contrast, mice without tumors had kidney uptake (Figure 2A, left) consistent with kidneys being the primary route of clearance (10, 11). Correlative histology demonstrated the presence of VCAM-1 on the meosthelium of tumor bearing mice (Figure 2B). Confirmation of imaging was provided through biodistribution analysis of omentum, mesentery and associated tumors, as well as un-involved organs such as the heart. Omentum and mesentery from tumor bearing animals had a 10-fold higher accumulation of the VCAM-1 targeted agent than omentum and mesentery from control animals (Figures 2C). To determine the extent and duration of expression, mice were evaluated weekly following tumor initiation starting at 2 weeks. As indicated by biodistribution, maximal VCAM-1 expression is detected 2 weeks after tumor initiation, and remained elevated through the course of the experiment (4 weeks total, Figure 2C). With the exception of a slight, statistically significant increase 3 weeks after tumor initiation, levels of VCAM-1 probe uptake in the heart were unaffected between tumor bearing animals and control animals. Together, these observations validate the use of radiolabeled imaging probes to monitor VCAM-1 expression in a mouse model of peritoneal ovarian cancer metastasis and demonstrate that VCAM-1 is expressed early in the course of disease. However, expression does not mirror the kinetics of tumor growth; maximal VCAM-1 expression was observed with microscopic tumors and did not change as tumor burden continued to increase (data not shown).
Figure 2. Detection of mesothelial VCAM-1 expression in a mouse model of ovarian cancer peritoneal metastasis.
Athymic nude mice received an intraperitoneal (IP) injection of SKOV3ip1 cells or saline (control). (A) SPECT/CT imaging of 111In-tVCAM-4 peptide 4 hours after IP injection into saline control injected (left panel) or tumor-bearing (right panel) animals. Maximum intensity projection (MIP) images shown. (B) Correlative Histology. Following radioactive decay, the omentums were stained for VCAM-1 using IHC (60X images with 20X insert). Arrows indicate the mesothelium in each case. Top panel – saline injected control mouse; bottom panel – mouse with SKOV3ip1 tumor cells injected. (C) Kinetics of VCAM-1-In111 peptide distribution in the heart or omentum of athymic nude mice 2, 3 and 4 weeks after IP injection of SKOV3ip1 cells, n=3. Control animals were evaluated 2 weeks after PBS injection. Data represent mean ± standard deviation. p<0.05, 1-way ANOVA for heart or omentum samples; *p<0.05, Bonferroni’s Multiple Comparison Test, relative to PBS-injected control for each organ.
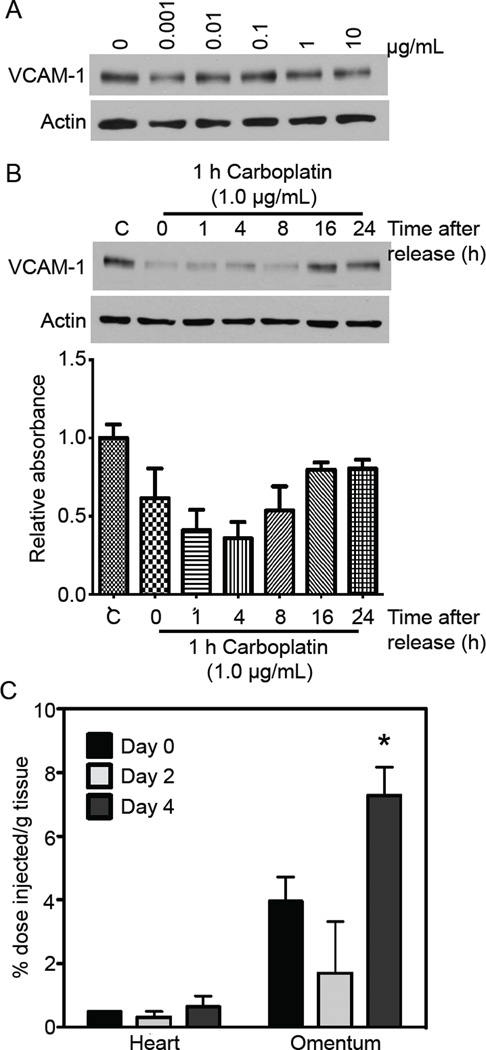
The retrospective patient data demonstrated a lower incidence of VCAM-1 expression among patients exposed to neoadjuvant chemotherapy. We considered two possibilities to account for this observation. First, mesothelial VCAM-1 expression is targeted directly by platinum agents, or second, metastatic ovarian cancer creates an environment that stimulates and maintains VCAM-1 expression in vivo, implying that expression reflects tumor responsiveness to chemotherapy. To determine whether carboplatin affects VCAM-1 expression directly, LP9 mesothelial cells, a primary human culture that constitutively expresses VCAM-1 and was isolated from a patient with ovarian cancer (14), were treated with increasing concentrations of carboplatin, a standard chemotherapy for the treatment of ovarian cancer. None of the concentrations tested altered VCAM-1 expression (Figure 3A) or cell viability (data not shown). However, patients are unlikely to be exposed to carboplatin continuously for 24 hours or more. Indeed, up to 80% of the injected dose is excreted within 24 hours (15). In an attempt to approach the in vivo cellular exposure, LP9 cells were pulsed with 1 μg/ml carboplatin for 1 hour and allowed to recover in fresh media for the indicated times (Figures 3B, Supplemental Figure 2). Within 1 hour following carboplatin exposure, VCAM-1 mRNA and protein levels decreased dramatically before returning to baseline levels 8–16 hours following exposure (Figure 3B, Supplemental Figure 2), where it remains elevated for up to 72 hours (data not shown). These observations indicate that carboplatin induces a transient decrease in VCAM-1 expression in cultured human mesothelial cells.
Figure 3. Carboplatin transiently diminishes mesothelial VCAM-1 expression.
(A) LP9 mesothelial cells were treated with the indicated concentrations of carboplatin for 24 hours prior to lysis and immunoblotting for VCAM-1 and actin (loading control). (B) LP9 cells were either untreated or exposed to 1 μg/ml carboplatin for 1 hr prior to release into fresh media. Lysates were blotted for VCAM-1 and actin. Following background subtraction, signal intensities for the VCAM-1 bands were normalized to actin and are expressed relative to the untreated control (C). (C) Nude mice harboring SKOV3ip1 tumors were imaged using SPECT/CT and the 111In-tVCAM-4 peptide 2 weeks post-tumor initiation to obtain baseline distribution values (0). Two days later (2), mice were imaged 8 hours after receiving an IP injection of 25 mg/kg carboplatin and 2 days later; 111In-tVCAM-4 peptide biodistribution presented as mean ± standard deviation.
While treatment with carboplatin generates a direct albeit transient decrease VCAM-1 expression, the mesothelial cell line examined constitutively expresses VCAM-1, which is not observed in healthy women. Rather, VCAM-1 expression is induced in women with ovarian cancer peritoneal metastases (Figure 1). Moreover, the tumor microenvironment is much more complex than that achieved in cell culture. To determine whether carboplatin alters ovarian cancer-induced VCAM-1 expression in vivo, mice harboring platinum-resistant (SKOV3ip1 or A2780Cis) or platinum-sensitive (A2780) ovarian cancer cells were evaluated. First, the short-term effects of exposure to carboplatin on mesothelial VCAM-1 expression were determined. Two weeks following IP injection of SKOV3ip1 cells, mice (n=3) were imaged using the VCAM-1 targeted imaging agent to obtain baseline expression levels. Two days later, mice (n=6) were treated with carboplatin for 4 hours; three of the treated mice were injected with the VCAM-1 imaging agent and imaged 4 hours later. The remaining 3 mice were imaged 2 days after carboplatin administration. Treatment with carboplatin resulted in a slight decrease in biodistribution of 111In-tVCAM-4 to the omentum; however, this change was not statistically significant (Figure 3C). Within 2 days of treatment, VCAM-1 expression not only recovered to baseline, it was 50% greater. This observation demonstrates that carboplatin does not alter VCAM-1 expression in vivo in the presence of platinum-resistant tumors. Moreover, VCAM-1 expression increases above baseline within 2 days thus raising the possibility that ovarian cancer-dependent VCAM-1 expression in vivo is maintained by the continued presence of the tumor.
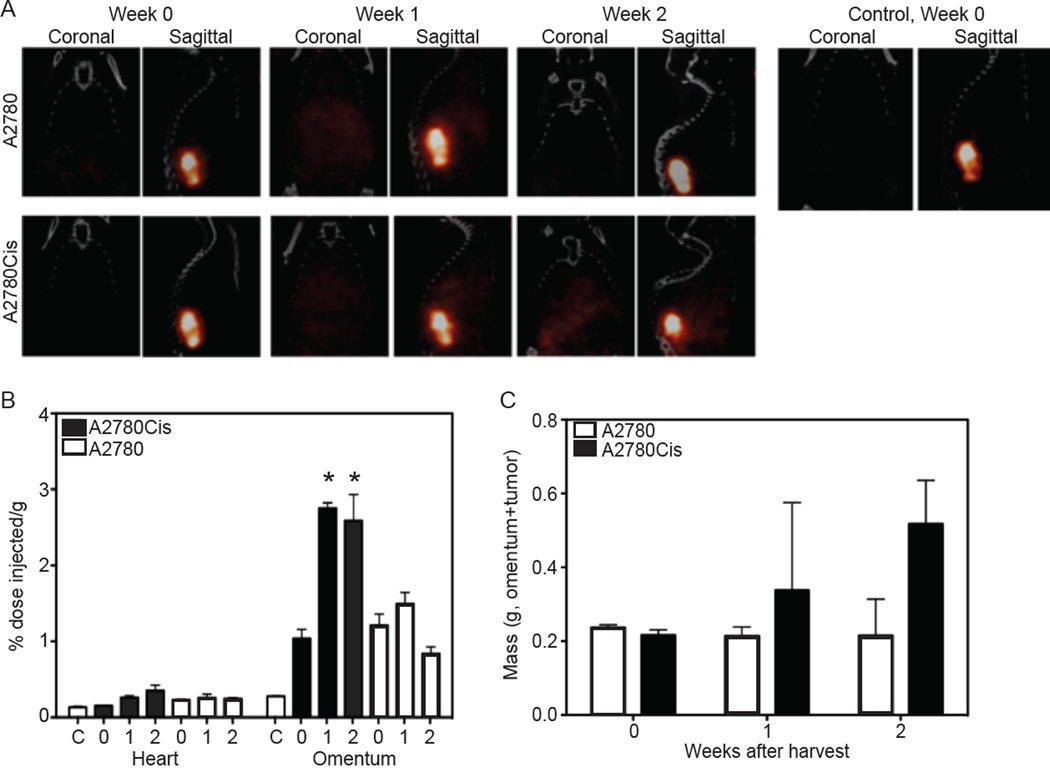
To test this hypothesis, platinum sensitive (A2780) or resistant (A2780Cis) ovarian cancer cells were employed to generate peritoneal tumors that were then treated with carboplatin and imaged. Baseline VCAM-1 expression (before carboplatin treatment) was determined using SPECT/CT one week after tumor initiation with each cell line (Figure 4A and Supplemental Figure 3, Week 0). Each group of mice was treated with 25 mg/kg carboplatin weekly and imaged one and two weeks following initial treatment just prior to subsequent weekly dosing. As shown in Figure 4 and Supplemental Figure 3, VCAM-1 expression was detected 1 week after tumor initiation in both models (week 0). Tumors in mice containing A2780Cis cells continued to grow in the presence of carboplatin (Figure 4C). Concomitantly, VCAM-1 expression in this model increased within 2 weeks of tumor initiation demonstrating a 2.5-fold increase in uptake of 111In-tVCAM-4 peptide after two weeks of carboplatin treatment (Figures 4A and 4B, Supplemental Figure 3). In contrast, omentum from animals with tumors generated from platinum sensitive A2780 cells had lower, although not statistically significant, levels of 111In-tVCAM-4 uptake after two weeks of treatment (Figures 4A and 4B, Supplemental Figure 3). These observations indicate that VCAM-1 expression kinetics can be monitored in vivo and that carboplatin treatment does not diminish VCAM-1 expression in mice harboring platinum-resistant tumors; however, expression is curbed when tumor growth is inhibited by platinum treatment.
Figure 4. Carboplatin indirectly regulates chronic mesothelial VCAM-1 expression by affecting tumor burden.
Nude mice were injected with A2780 (n=3 per time point) or A2780Cis (n=3 per time point) cells or saline (control, n=2). One week following tumor initiation a group of mice was imaged to obtain baseline values; the remaining mice were treated with 25 mg/kg carboplatin weekly. A) SPECT/CT images were collected weekly starting 1 week after tumor initiation (week 0); weeks 0, 1 and 2 indicate time after carboplatin treatment. Representative coronal and sagittal MIP images of 111In-tVCAM-4 peptide obtained 4 hours after IP injection are depicted. (B) Biodistribution of 111In-tVCAM-4. Heart and omentum were removed from each cohort of mice weekly after carboplatin treatment (x-axis, 0=1 week tumor, no treatment) and the percent-injected dose of radioactivity per gram of tissue determined. n=3 for each cohort, C= control animals; 0, 1 and 2 indicate weeks after carboplatin treatment. p<0.05, 1-way ANOVA for omentum samples; *p<0.05, Bonferroni’s Multiple Comparison Test, relative to week 0, A2780 or A2780Cis, which were not different from each other. (C) The omentum (primary site of tumor deposition) and any visible tumors from the peritoneal cavity were removed and weighed. Data represent mean mass ± SEM (n=3); grey bars - A2780-tumored mice, black bars – A2780Cis-tumored mice.
DISCUSSION
This study demonstrates a potential role for VCAM-1 as a marker of ovarian cancer peritoneal metastasis and tumor responsiveness to platinum-based chemotherapy. Retrospective analysis of omental or peritoneal biopsies revealed an increased incidence of mesothelial VCAM-1 expression with increasing tumor stage such that expression was coincident with secondary tumor implantation. Additionally, the incidence of VCAM-1 expression was reduced among women who received neoadjuvant chemotherapy to reduce tumor burden prior to surgery. Using clinically relevant VCAM-1-targeted imaging probes and a mouse model of peritoneal ovarian cancer metastasis, maximal mesothelial VCAM-1 expression was detected with microscopic tumor burden. Importantly, VCAM-1 expression mirrored tumor response to platinum-based chemotherapy. VCAM-1 expression was negligible in mice bearing platinum-sensitive ovarian cancer cells following treatment with carboplatin; expression continued to increase and was maintained in mice harboring platinum-resistant tumors following treatment. Together, these observations support a role for VCAM-1 as an indicator of peritoneal ovarian cancer metastasis and responsiveness to platinum-based chemotherapy and offer the potential for VCAM-1 targeted imaging agents to change ovarian cancer clinical management.
The observation that VCAM-1 is expressed on the mesothelium of ovarian cancer patients at the earliest stage of secondary implantation (i.e., Stage II with secondary implants within the pelvis) raises the intriguing possibility that VCAM-1 could function as a marker of peritoneal metastasis. The ability to identify peritoneal metastasis early in the course of disease has implications for women at high-risk for developing ovarian cancer or those with Stage II disease where VCAM-1 expression might identify those at risk for progressing to Stage III ovarian cancer. Current methodology to evaluate VCAM-1 expression in patients relies on non-quantitative immunohistochemistry, which is limited further by the number of biopsies taken from each patient. Using a VCAM-1-specific imaging agent originally designed to monitor atherosclerosis (9–11), we observed maximal VCAM-1 expression in a mouse model of peritoneal ovarian cancer metastasis with microscopic tumor burden. Employing more quantitative imaging modalities such as PET (11) will improve the ability to demonstrate VCAM-1 as a marker of peritoneal metastasis.
In addition to indicating early metastasis, the ability to detect maximal mesothelial VCAM-1 expression with microscopic tumor burden has implications for monitoring women for recurrence. Following the initial successful treatment of metastatic ovarian cancer, which occurs for 80% of patients, the majority of them will recur within 2 years and eventually succumb to their disease (2). Current modalities to monitor women who have entered remission are ineffective. Serum CA125 is not a reliable predictor of recurrence, CT scans are unable to detect small and/or diffuse lesions that are likely to affect prognosis, and neither modality predicts the appropriate time to treat recurrent disease (5–7). Thus, imaging VCAM-1 may provide a more reliable indication as to when to initiate second-line therapy.
Our data demonstrating reduced incidence of VCAM-1 expression among women who received neoadjuvant chemotherapy together with the observation that VCAM-1 expression mirrors tumor response to carboplatin treatment implicate mesothelial VCAM-1 expression as a marker of tumor response to platinum-based chemotherapy. While carboplatin induced a direct, transient decrease in VCAM-1 expression in cultured mesothelial cells, the effect was lost in mice harboring platinum-resistant tumors. Importantly, VCAM-1 expression was able to differentiate platinum sensitive tumors from resistant ones within 1 week of treatment. The development of resistance to platinum-based chemotherapy is a major obstacle for the successful treatment of metastatic ovarian cancer. Unfortunately, to date this phenomenon is defined somewhat loosely based on retrospective data; patients are categorized as having platinum resistant disease only after having failed primary therapy with persistent disease or progression within 6 months of completion of therapy (16). The ability to objectively identify ovarian cancers that are resistant versus sensitive to platinum agents would provide a significant advance in the management of women with metastatic ovarian cancer. Importantly, a molecular indication of chemosensitivity could allow for earlier detection of platinum resistant disease to permit alterations in treatment regimen directed at the molecular behavior of disease. Moreover, it would potentially provide an opportunity to objectively identify women for inclusion in clinical trials and an ability to monitor their progress.
CONCLUSION
VCAM-1 may serve as a sensitive indicator of ovarian cancer peritoneal metastasis and response to platinum-based chemotherapy. While additional studies are necessary to determine the prognostic implications of VCAM-1 expression among ovarian cancer patients, strategies designed to image mesothelial VCAM-1 expression in ovarian cancer patients offer the potential to improve management of women with this disease.
Supplementary Material
ACKNOWLEDGMENTS
Financial Support: J.M.S. was supported by Gynecologic Oncology Fellowship program; S.T., C.H., K.A.K., and J.K.S-D. were supported in part by a grant from the University of Virginia Women’s Oncology Research Fund and Cancer Center; T.A.R., J.C., C.H. and J.K.S-D were supported by NCI R01 CA142783.
We are grateful to the Molecular Imaging Core Facility, specifically Drs. Mark Williams and Kosta Popovic for their assistance with in vivo imaging, the Biorepository and Tissue Research Facility for assistance with obtaining and staining patient samples, and the Pathology Core for staining mouse tissues.
GRANT SUPPORT
Grants from UVA Women’s Oncology Research Fund and Cancer Center and NCI R01 CA142783 to J.K.S-D supported this work.
REFERENCES
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: a cancer journal for clinicians. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Ozols RF. Treatment goals in ovarian cancer. Int J Gynecol Cancer. 2005;15(Suppl 1):3–11. doi: 10.1111/j.1525-1438.2005.15351.x. [DOI] [PubMed] [Google Scholar]
- 3.Eisenhauer EL, Abu-Rustum NR, Sonoda Y, Aghajanian C, Barakat RR, Chi DS. The effect of maximal surgical cytoreduction on sensitivity to platinumtaxane chemotherapy and subsequent survival in patients with advanced ovarian cancer. Gynecol Oncol. 2008;108:276–281. doi: 10.1016/j.ygyno.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 4.Hou JY, Kelly MG, Yu H, et al. Neoadjuvant chemotherapy lessens surgical morbidity in advanced ovarian cancer and leads to improved survival in stage IV disease. Gynecol Oncol. 2007;105:211–217. doi: 10.1016/j.ygyno.2006.11.025. [DOI] [PubMed] [Google Scholar]
- 5.Rustin GJ, van der Burg ME, Griffin CL, et al. Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955): a randomised trial. Lancet. 2010;376:1155–1163. doi: 10.1016/S0140-6736(10)61268-8. [DOI] [PubMed] [Google Scholar]
- 6.Rustin GJ. Use of CA-125 to assess response to new agents in ovarian cancer trials. J Clin Oncol. 2003;21:187s–193s. doi: 10.1200/JCO.2003.01.223. [DOI] [PubMed] [Google Scholar]
- 7.Eisenhauer EA. Optimal assessment of response in ovarian cancer. Ann Oncol. 2011;22(Suppl 8):viii49–viii51. doi: 10.1093/annonc/mdr467. [DOI] [PubMed] [Google Scholar]
- 8.Slack-Davis JK, Atkins KA, Harrer C, Hershey ED, Conaway M. Vascular cell adhesion molecule-1 is a regulator of ovarian cancer peritoneal metastasis. Cancer Res. 2009;69:1469–1476. doi: 10.1158/0008-5472.CAN-08-2678. [DOI] [PubMed] [Google Scholar]
- 9.Kelly KA, Nahrendorf M, Yu AM, Reynolds F, Weissleder R. In vivo phage display selection yields atherosclerotic plaque targeted peptides for imaging. Mol Imaging Biol. 2006;8:201–207. doi: 10.1007/s11307-006-0043-6. [DOI] [PubMed] [Google Scholar]
- 10.Nahrendorf M, Jaffer FA, Kelly KA, et al. Noninvasive vascular cell adhesion molecule-1 imaging identifies inflammatory activation of cells in atherosclerosis. Circulation. 2006;114:1504–1511. doi: 10.1161/CIRCULATIONAHA.106.646380. [DOI] [PubMed] [Google Scholar]
- 11.Nahrendorf M, Keliher E, Panizzi P, et al. 18F-4V for PET-CT imaging of VCAM-1 expression in atherosclerosis. JACC Cardiovascular imaging. 2009;2:1213–1222. doi: 10.1016/j.jcmg.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly KA, Allport JR, Tsourkas A, Shinde-Patil VR, Josephson L, Weissleder R. Detection of vascular adhesion molecule-1 expression using a novel multimodal nanoparticle. Circ Res. 2005;96:327–336. doi: 10.1161/01.RES.0000155722.17881.dd. [DOI] [PubMed] [Google Scholar]
- 13.Kelly KA, Waterman P, Weissleder R. In vivo imaging of molecularly targeted phage. Neoplasia. 2006;8:1011–1018. doi: 10.1593/neo.06610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cannistra SA, Ottensmeier C, Tidy J, DeFranzo B. Vascular cell adhesion molecule-1 expressed by peritoneal mesothelium partly mediates the binding of activated human T lymphocytes. Exp Hematol. 1994;22:996–1002. [PubMed] [Google Scholar]
- 15.van der Vijgh WJ. Clinical pharmacokinetics of carboplatin. Clin Pharmacokinet. 1991;21:242–261. doi: 10.2165/00003088-199121040-00002. [DOI] [PubMed] [Google Scholar]
- 16.Markman M, Rothman R, Hakes T, et al. Second-line platinum therapy in patients with ovarian cancer previously treated with cisplatin. J Clin Oncol. 1991;9:389–393. doi: 10.1200/JCO.1991.9.3.389. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.