Abstract
Background
Among patients with heart failure (HF), anxiety symptoms may co-exist with depressive symptoms. However, the extent of overlap and risk factors for anxiety symptoms have not been thoroughly described.
Purpose
To describe the coexistence of anxiety and depressive symptoms, and to determine the predictors of anxiety symptoms in patients with HF.
Methods
The sample consisted of 556 outpatients with HF (34% female, 62±12 years, 54% NYHA class III/IV) enrolled in a multicenter HF quality of life registry. Anxiety symptoms were assessed with the Brief Symptom Inventory-anxiety subscale. Depressive symptoms were measured with the Beck Depression Inventory-II (BDI). We used a cut-point of 0.35 to categorize patients as having anxiety symptoms or no anxiety symptoms. Logistic regression was used to determine whether age, gender, minority status, educational level, functional status, comorbidities, depressive symptoms, and antidepressant use were predictors of anxiety symptoms.
Results
One-third of patients had both depressive and anxiety symptoms. There was a dose-response relationship between depressive symptoms and anxiety symptoms; higher levels of depressive symptoms were associated with a higher level of anxiety symptoms. Younger age (OR= 0.97, p = .004, 95% CI 0.95–0.99) and depressive symptoms (OR = 1.25, p < .001, 95% CI 1.19–1.31) were independent predictors of anxiety symptoms.
Conclusions
Patients with HF and depressive symptoms are at high risk for experiencing anxiety symptoms. Clinicians should assess these patients for comorbid anxiety symptoms. Research is needed to test interventions for both depressive and anxiety symptoms.
Keywords: Cardiovascular, depressive disorder, anxiety disorder, heart failure
Patients with HF frequently report symptoms of anxiety.1 Anxiety is a negative emotion that occurs in response to perceived threats. Sources of anxiety can be internal or from outside sources, and perceived threats can be real or imagined.2 On average, patients with HF have much higher anxiety levels than healthy older adults.1 Surprisingly few researchers have examined the relationship between anxiety and health outcomes in patients with HF. However, several researchers have reported that the presence of anxiety symptoms is an independent predictor of worsening functional status,3 poorer health-related quality of life,4 and more frequent re-hospitalizations.
In addition to experiencing anxiety symptoms, one-third of all patients with heart failure (HF) experience depressive symptoms,6 which increase the risk for both poor health-related quality of life4, 7 and shorter event-free survival.6 Depressive symptoms can be defined as symptoms of anhedonia or low mood, accompanied by negative physical symptoms related to activity, appetite, and sleep and/or negative cognitive symptoms related to ability to concentrate, low self-worth, and pessimism about the future. Depressive symptoms may exist with or without the presence of clinical depression,8 but they may differ from clinical depression in the number, combination, and duration of symptoms, and in the degree to which symptoms interfere with daily functioning.
It is possible that many patients with HF have co-existing symptoms of anxiety and depression, as both are known to coexist in individuals with and without chronic disease.9 However, there has been little systematic quantitative research about the coexistence of these two symptom domains in patients with HF. In a recent systematic review of qualitative research,10 patients with HF and depressive symptoms disclosed that they were anxious about many things, including: the future, comorbidities, the unpredictable nature of HF, pain, hospital readmissions, medical procedures, the likelihood of a shortened life span, and the possibility of dying in the middle of the night. One patient with HF described his fears about an uncertain future: 8
“I just feel, you know, next week I might not be here…that’s my initial sort of fear, you know, oh my God, how much longer have I got? (p. 276)”
Although many patients with HF experience symptoms of anxiety, others do not. Little is known about characteristics of patients with and without anxiety symptoms, and which independent risk factors may predispose patients with HF to anxiety. Furthermore, although it is likely that anxiety and depressive symptoms are intertwined in patients with HF, we have very little information about the coexistence of these two symptom domains. Therefore, the specific aims of this study were to: 1) describe the characteristics of patients with and without anxiety symptoms, 2) determine the extent to which anxiety and depressive symptoms coexist in patients with HF, 3) determine whether depressive symptoms are an independent predictor of the presence of anxiety symptoms
Methods
Design and Sample
This investigation was a cross-sectional, secondary data analysis of data from the Heart Failure Quality of Life registry for patients with HF. A detailed summary of registry methods has been previously published.11, 12 The present subset (N = 556) is made up of a convenience sample of subjects who had data on both depressive symptoms and anxiety symptoms. Of registry sites, three collected the desired variables. Outpatients were recruited from academic medical centers and community-based clinics in three Southeastern and Midwestern states in the U.S.
Each of the registry studies conducted at these sites had similar inclusion and exclusion criteria. Patients were eligible for inclusion if they had a diagnosis of chronic HF, preserved or non-preserved systolic function, optimization on HF medications, taking stable medication doses for 3 months, and English-speaking. Patients were excluded for a myocardial infarction or unstable angina within 3 months, cognitive impairment that precluded the ability to provide informed consent, placement at a skilled nursing facility, or severe psychiatric impairment other than depression or anxiety.
Measurement
Anxiety symptoms
Anxiety was measured with the Brief Symptom Inventory (BSI) anxiety subscale.13 This is a 6 item questionnaire that assesses the presence and intensity of anxiety symptoms. Patients are asked to endorse how much they were distressed (0 = none at all, 3 = extremely) by nervousness or shakiness inside, suddenly scared for no reason, feeling fearful, feeling tense or keyed up, spells of terror or panic, and feeling so restless you can’t sit still. Item scores are summed and averaged. According to published norms, the mean anxiety level of healthy adults is 0.35, and the mean level of psychiatric inpatients and outpatients is 1.7. Researchers have shown that the BSI anxiety subscale has good evidence for reliability and validity in patients who are acutely ill. The BSI has demonstrated excellent psychometric properties in patients with HF,14 and it performs better than the more commonly used Spielberger State-Trait Index.15
Depressive symptoms
Depressive symptoms were measured with the Beck Depression Inventory-II (BDI). This is a 21 item questionnaire in which patients report the presence and severity of symptoms of depression. Patients who score a 14 or greater are classified as having clinically significant depressive symptoms. Patients can also be categorized as having none to minimal symptoms (0–13), mild symptoms (14–19), moderate symptoms (20–28) or severe symptoms (29–63). Researchers have found good evidence for reliability and validity of the BDI-II in both medical and non-medical populations.16, 17
Functional status
In patients with HF, worse functional status is closely related to higher levels of anxiety3 and depressive symptoms.6 We measured functional status with the New York Heart Association (NYHA) functional class and the Duke Activity Status Index (DASI). NYHA class is a provider-rated indicator of functional status, based on the patient’s subjective self-report of symptoms. On the basis of a clinical interview, patients are classified from I to IV, with I indicating no symptoms, and IV indicating HF symptoms occur even at rest.18 The DASI is a 12-item survey that measures functional capacity for various activities of daily living.19 Total scores are calculated using a weighted score for each activity; lower total scores indicate worse functional status.
Other variables of interest
We used patient interviews to collect information on age, sex, race/ethnicity, marital status, and education level. Chart reviews were used to collect information on smoking status, ejection fraction, and medications. Medications were confirmed by visually checking pill bottle prescriptions. Height and weight were measured during the baseline visit. Data on comorbidities, were collected by patient interview using the Charlson Comorbidity Index.20, 21
Protocol
Each of the individual studies was approved by local institutional review boards. The review board at the primary author’s institution approved all secondary data analyses with the HF registry as an exempt protocol. The investigation conformed to the principles outlined in the Declaration of Helsinki. Patients were recruited in the outpatient setting and completed written informed consent and baseline assessments at General Clinical Research Centers. After completion of each study, data were de-identified and combined into a single HF registry database at the primary author’s institution.
Data analysis
Data analysis was conducted using SPSS v. 20 (SPSS Inc, Chicago). A p value of less than .05 was considered significant. Patient characteristics were described using means and standard deviations or frequency distributions. A cut-point of 0.35 on the BSI-anxiety subscale was used to divide patients into anxiety symptoms or no anxiety symptoms, and the cut-point of 14 on the BDI-II was used to divide patients into depressive symptoms or no depressive symptoms. Patients were also categorized as having: 1) both anxiety symptoms and depressive symptoms, 2) anxiety symptoms alone, 3) depressive symptoms alone, and 4) symptom-free. Differences in demographic and clinical variables between groups were compared with independent t-tests, analysis of variance, and chi-square tests of association.
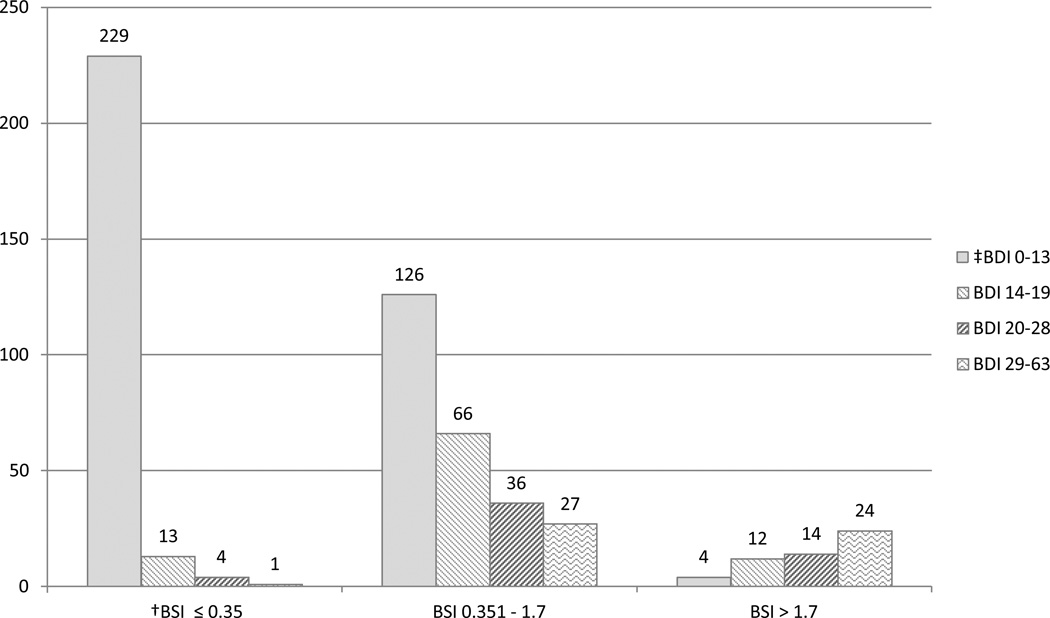
To further examine the relationship between severity of anxiety symptoms and severity of depressive symptoms, we divided the sample into several sub-groups and used chi-square tests of association to determine differences between these groups. To do so, we used the cut-points of 0.35 and 1.7 on the BSI to form 3 groups: 1) below the mean anxiety level of healthy adults (0 to 0.35), 2) in between the mean anxiety level of healthy adults and the mean level of psychiatric outpatients (0.36 to 1.7), and 3) above the mean anxiety level of psychiatric outpatients (>1.7). We also used BDI-II cut-points to label patients as having none to minimal (0–13), mild (14–19), moderate (20–28), and severe (29–63) depressive symptoms.
Finally, hierarchical logistic regression was used to determine the independent predictors of anxiety symptom status. The independent variables entered consisted of block 1) Demographics: age, gender, minority status, education level; block 2) HF severity and comorbidities: NYHA class, DASI score, total comorbidity score: and block 3) Psychological variables: depressive symptoms and antidepressant use. These variables were chosen based on finding significant differences during bivariate analyses that compared patients with and without anxiety symptoms (Table 2).
Table 2.
Comparison of patients with and without anxiety symptoms*
| Characteristic | No anxiety (n =247) | Anxiety (n = 309) | p |
|---|---|---|---|
| Age, mean ± SD, yrs | 63.6 ± 11.5 | 60.6 ± 12.5 | .003 |
| Female, % | 28.3 | 37.9 | .018 |
| †Minority, % | 29.1 | 43 | .001 |
| Live alone, % | 28.0 | 24.3 | .313 |
| Married, % | 57.5 | 61.2 | .380 |
| LVEF, mean ± SD, % | 35.3 ± 14.6 | 37.7 ± 15.0 | .076 |
| Body mass index, mean ± SD | 31.1 ± 7.7 | 29.8 ± 7.2 | .036 |
| NYHA functional class, % | |||
| Class I | 11.8 | 5.5 | <.001 |
| Class II | 47.2 | 30.1 | |
| Class III | 33.7 | 45.0 | |
| Class IV | 7.3 | 19.4 | |
| Duke Activity Status Index, mean ± SD | 18.8 ± 14.3 | 9.6 ± 11.2 | <.001 |
| Education level, % | |||
| Less than high school | 17.0 | 32.9 | <.001 |
| High school graduate | 27.1 | 20.2 | |
| Some college or higher | 55.9 | 46.9 | |
| Heart failure etiology, % | |||
| Ischemic | 50.6 | 54.6 | .253 |
| Idiopathic | 19.9 | 14.6 | |
| Other | 29.5 | 30.8 | |
| Comorbidity, % | |||
| History of MI | 50.4 | 61.8 | .008 |
| History of CABG | 27.6 | 19.9 | .033 |
| Atrial fibrillation | 44.3 | 38.7 | .187 |
| Biventricular pacemaker | 31.8 | 29.2 | .505 |
| ICD | 12.9 | 7.0 | .021 |
| History of stroke | 15.0 | 24.4 | .006 |
| Diabetes mellitus | 42.9 | 39.0 | .346 |
| COPD | 14.2 | 16.0 | .573 |
| Total Comorbidity Score | 2.92 ± 1.69 | 3.32 ± 1.93 | .01 |
| Medications, % | |||
| ACE inhibitor | 73.0 | 64.1 | .027 |
| Beta-blocker | 87.8 | 83.3 | .136 |
| Diuretic | 75.5 | 71.0 | .237 |
| Digoxin | 25.0 | 32.8 | .049 |
| ARB | 19.4 | 25.4 | .097 |
| Antidepressants | 12.9 | 25.8 | <.001 |
p values were calculated using independent t-tests for continuous variables and the chi-square test of association for categorical variables, bolded values highlight the statistically significant differences;
Minorities were defined as non-Caucasians (almost all minorities were African American)
LVEF = Left ventricular ejection fraction, NYHA = New York Heart Association functional class, MI = myocardial infarction, CABG = coronary artery bypass graft, ICD = implanted cardiac defibrillator, COPD = chronic obstructive pulmonary disease, ACE = angiotensin converting enzyme, ARB = angiotensin receptor blocker
Results
Sample characteristics
Sample characteristics are described in Table 1. The final sample consisted of 556 outpatients with HF. One-third of the sample was female, and 36% were minorities. Approximately half of the sample (54%) was classified as NYHA functional status class III or IV, while 46% had NYHA Class I or II HF. Most of the patients were married (60%) and lived with someone (70%), and 74% had at least a high school education (12 years of school).
Table 1.
Baseline characteristics for the total sample and comparison of patient characteristics* from each symptom group
| Characteristic | Overall (n = 556 ) |
No symptoms (n= 229) |
Anxiety alone (n= 130) |
Depressive symptoms alone (n = 18 ) |
Both anxiety and depressive symptoms (n = 179) |
p |
|---|---|---|---|---|---|---|
| Age, mean ± SD, yrs | 61.9 ± 12.2 | 64 ± 11.5 | 59.7 ± 12.5 | 58.9 ± 9.7 | 61.2 ± 12.5 | .005 |
| Female, % | 34 | 27 | 39 | 50 | 37 | .02 |
| Minority, % | 37 | 29 | 35 | 33 | 49 | <.001 |
| Lives alone, % | 26 | 28 | 26 | 33 | 23 | .63 |
| Married, % | 60 | 58 | 59 | 56 | 62 | .77 |
| LVEF, mean ± SD, % | 36.6 ± 14.9 | 34.6 ± 14.1 | 37.4 ± 14.9 | 44.5 ± 18.5 | 38 ± 15.2 | .016 |
| Body mass index, mean ± SD | 30.4 ± 7.4 | 31 ± 7.5 | 30.5 ± 7.3 | 32.9 ± 10.3 | 29.3 ± 7.1 | .06 |
| NYHA functional class, % | <.001 | |||||
| Class I | 8 | 12 | 9 | 6 | 3 | |
| Class II | 38 | 50 | 42 | 17 | 22 | |
| Class III | 40 | 32 | 39 | 61 | 49 | |
| Class IV | 14 | 7 | 11 | 17 | 26 | |
| Duke Activity Status Index, mean ± SD | 13.7 ± 13.5 | 19.4 ± 14.2 | 15.8 ± 12.9 | 11.3 ± 13.9 | 5.1 ± 7.1 | <.001 |
| Education level, % | <.001 | |||||
| Less than high school | 26 | 15 | 20 | 44 | 42 | |
| High school graduate | 23 | 26 | 20 | 39 | 20 | |
| Some college or higher | 51 | 59 | 60 | 17 | 38 | |
| Heart failure etiology, % | .77 | |||||
| Ischemic | 52 | 51 | 54 | 44 | 55 | |
| Idiopathic | 17 | 20 | 16 | 22 | 14 | |
| Other | 30 | 29 | 30 | 33 | 31 | |
| Comorbidity, % | ||||||
| History of MI | 57 | 50 | 57 | 56 | 65 | .02 |
| History of CABG | 23 | 29 | 25 | 6 | 16 | .004 |
| Atrial fibrillation | 41 | 45 | 37 | 39 | 40 | .54 |
| Biventricular pacemaker | 30 | 33 | 31 | 12 | 28 | .23 |
| ICD | 38 | 44 | 38 | 17 | 34 | .051 |
| History of stroke | 20 | 15 | 23 | 11 | 25 | .049 |
| Diabetes mellitus | 41 | 42 | 35 | 56 | 42 | .339 |
| COPD | 15 | 13 | 12 | 33 | 19 | .043 |
| Total comorbidity score | 3.14 ± 1.84 | 2.87 ± 1.69 | 3.08 ± 1.90 | 3.50 ± 1.62 | 3.49 ± 1.93 | .006 |
| Baseline medications,% | ||||||
| ACE inhibitor | 68 | 73 | 70 | 78 | 60 | .035 |
| Beta-blocker | 85 | 88 | 88 | 83 | 80 | .074 |
| Diuretic | 73 | 75 | 69 | 78 | 73 | .53 |
| Digoxin | 29 | 25 | 27 | 28 | 37 | .058 |
| ARB | 23 | 20 | 18 | 17 | 31 | .017 |
| Antidepressants | 20 | 11 | 25 | 39 | 26 | <.001 |
p values were calculated using analysis of variance for continuous variables and the chi-square test of association for categorical variables;
Minorities were defined as non-Caucasians (almost all minorities were African American)
LVEF = Left ventricular ejection fraction, NYHA = New York Heart Association functional class, MI = myocardial infarction, CABG = coronary artery bypass graft, ICD = implanted cardiac defibrillator, COPD = chronic obstructive pulmonary disease, ACE = angiotensin converting enzyme, ARB = angiotensin receptor blocker
Depressive and anxiety symptoms
The mean BDI-II score for the entire sample was 12.3 ± 9.7, and 35% of the sample (n = 197) had clinically significant depressive symptoms. Fifty-four of the patients with depressive symptoms were taking antidepressants (27.4%). Patients with depressive symptoms had fewer years of education (10.8 vs. 13.5, p < .001), worse DASI scores (18.1 vs. 5.7, p < .001) and higher total comorbidity score (3.5 vs. 2.9, p < .001) compared to patients who had no depressive symptoms. There were also higher proportions of patients with depressive symptoms who were minorities (48% vs. 31%, p < .001), NYHA Class III or IV (75% vs. 43%, p < .001) and had a history of myocardial infarction 64% vs. 53%, p = .007) or COPD (20% vs. 13%, p = .02). Fewer patients with depressive symptoms were taking angiotensin receptor blockers (19% vs. 30%, p = .004), beta blockers (80% vs. 88%, p = .009), or digoxin (36% vs. 26%, p = .01), and fewer had a history of coronary bypass surgery (15% vs. 28%, p < .001) or implanted cardioverter defibrillators (32% vs. 42%, p = .034) when compared to patients with no depressive symptoms.
The overall mean BSI score was 0.72 ± 0.73, and 56% (n = 309) of the sample had anxiety levels above the mean level of anxiety in healthy adults. Approximately 10% of the patients in our sample had BSI scores higher than the mean anxiety level of psychiatric patients. Table 2 compares the characteristics between patients who were anxious and not anxious. Patients with symptoms of anxiety were more likely to be younger (61 vs. 64, p = .003), had a lower average BMI (30 vs. 31, p = .036), worse DASI scores (10 vs. 19, p = .001), and higher total comorbidity score (3.3 vs. 2.9, p = .01) compared to patients who were not anxious. Among patients who were anxious, there were higher proportions of women (38% vs. 28%, p = .018), minorities (43% vs. 29%, p < .001), NYHA Class III or IV (64% vs. 41%, p < .001), less than a high school education (33% vs. 17%, p < .001), comorbidities of stroke (24% vs. 15%, p = .006) or myocardial infarction (62% vs. 50%, p = .008), antidepressant use (26% vs. 13%, p < .001), and digoxin use (33% vs. 25%, p = .049 ), when compared with patients who were not anxious. There were fewer patients with anxiety symptoms taking angiotensin converting enzyme inhibitors (64% vs. 73%, p = .027) or who had implanted cardioverter defibrillators (7% vs. 13%, p = .021) when compared to patients without anxiety.
Of the total sample, 229 patients (41%) had neither depressive nor anxiety symptoms (symptom-free), 130 (23%) had anxiety symptoms alone, 18 (3%) had depressive symptoms alone, and 179 (32%) had both depressive symptoms and anxiety symptoms. The characteristics of these groups are compared in Table 1. Patients who had depressive symptoms, anxiety symptoms, or both, were younger and had a higher proportion with NYHA functional class III/IV compared to patients who were symptom-free. Patients who had both depressive and anxiety symptoms included a higher proportion of minorities, a lower average body mass index, and worse DASI and comorbidity scores than the 3 other groups.
Coexistence of anxiety and depressive symptoms
Anxiety and depressive symptoms frequently coexisted in this sample. Of the 309 patients with anxiety, 179 (58%) had comorbid depressive symptoms, while 130 (42%) had no depressive symptoms. Of the 197 patients with depressive symptoms, 179 (91%) had anxiety symptoms. There were also strong correlations between the BSI and BDI-II (r = .68, p < .001).
In Figure 1, we compare the proportion of patients with none to minimal, mild, moderate, and severe depressive symptoms among three categories of anxiety symptoms: 1) below the mean anxiety level of healthy adults, 2) in between the mean anxiety level of healthy adults and the mean level of psychiatric outpatients, and 3) above the mean anxiety level of psychiatric outpatients. There was a significant difference in the proportions of none, mild, moderate, and severe depressive symptoms among the different anxiety level groups (p < .001). Of those patients with no anxiety symptoms (BSI < 0.35), 92% had none to minimal depressive symptoms. Among those with anxiety symptoms above the mean of healthy adults but below the mean level of psychiatric patients (BSI >0.35 and <1.7), about half (49%) had none to minimal depressive symptoms, 26% had mild depressive symptoms, and 25% had moderate-severe depressive symptoms. In contrast, among patients with anxiety symptoms above the mean of psychiatric patients (BSI >1.7), the majority (70%) had moderate to severe symptoms of depression, 22% had mild symptoms of depression, and only 7% had none to minimal symptoms.
Figure 1.
Relationship between the level of anxiety symptoms and the level of depressive symptoms
*Data presented by number (n)
†BSI = Brief Symptom Inventory anxiety subscale; BSI ≤ 0.35: anxiety symptoms lower than the mean of healthy adults, BSI 0.351–1.7: anxiety symptoms higher than the mean anxiety level of healthy adults but lower than the mean level of psychiatric patients; BSI > 1.7: anxiety symptoms higher than the mean level of psychiatric patients
‡BDI = Beck Depression Inventory; BDI 0–13: none to minimal depressive symptoms; BDI 14–19: mild symptoms; BDI 20–28: moderate symptoms: BDI 29–63: severe symptoms
Regression Results
In the logistic regression model (Table 3), depressive symptoms were the strongest predictor of anxiety symptoms, after controlling for age, gender, minority status, education level, NYHA class, DASI scores, total comorbidity score, and antidepressant use. For every 1-point increase on the BDI-II, there was a 25% increase in the risk of experiencing anxiety symptoms. Age was the only other significant variable in the model, with younger age predicting the presence of anxiety symptoms. The model as a whole explained 49% of the variance in anxiety symptoms, with depressive symptoms by itself explaining 29% of variance.
Table 3.
Logistic regression model for the prediction of the presence of anxiety symptoms
| Block | Variable | Exp (β) | 95% CI | p value | R2 change | Total R2 |
|---|---|---|---|---|---|---|
| 1 | Age | .97 | .95–.99 | .003 | .088 | .088 |
| Female | 1.20 | .72–1.99 | .481 | |||
| Minority | 1.28 | .78–2.11 | .332 | |||
| Education: | ||||||
| HS education | 1.03 | .57–1.86 | .916 | |||
| Less than HS | .672 | .34–1.33 | .252 | |||
| 2 | NYHA Class III/IV | 1.05 | .63–1.77 | .851 | .137 | .225 |
| DASI | 1.0 | .98–1.02 | .671 | |||
| Comorbidity score | 1.03 | .91–1.18 | .628 | |||
| 3 | BDI-II | 1.25 | 1.19–1.31 | <.001 | .274 | .499 |
| Antidepressant use | 1.76 | .94–3.28 | .08 | |||
HS = High school (12 years education), NYHA = New York Heart Association functional class, DASI = Duke Activity Status Index, Comorbidity score = Charlson comorbidity index, BDI = Beck Depression Inventory-II
Discussion
In this study, we found that depressive and anxiety symptoms frequently co-exist in patients with HF. The vast majority of patients with depressive symptoms experienced comorbid anxiety symptoms, and more than half of patients with anxiety symptoms had comorbid depressive symptoms. Importantly, we found that as the severity of anxiety symptoms increased, there was a corresponding increase in the severity of depressive symptoms—suggesting a possible dose-response relationship between anxiety and depressive symptoms in patients with HF.
Using the BDI-II, we found that the prevalence of depressive symptoms in this sample was 35%. This prevalence is consistent with findings from a meta-analysis in which researchers reported that 33% of patients with HF have depressive symptoms as measured with questionnaires.5 We also found that 56% of our sample had BSI-anxiety scores above the mean of healthy adults, and 10% had scores higher than the average anxiety level of psychiatric patients. To our knowledge, ours is the only research team to use the BSI to measure anxiety in patients with HF, so it is not possible to compare the rates of anxiety we observed with other samples.
One of the unique findings of our study was that we were able to characterize the coexistence of depressive symptoms and anxiety symptoms. Although previous researchers have reported strong correlations between anxiety levels and depressive symptom levels in patients with HF, to our knowledge, only one small study has reported the extent of comorbidity. In 2005, Haworth et al.22 enrolled 100 mostly male outpatients with chronic systolic HF and determined the presence of generalized anxiety disorder (GAD) (11%) and depressive disorder (29%) using a structured clinical diagnostic interview. Approximately 9% of the sample had co-existing depressive disorder and GAD. Although other researchers have reported strong correlations between depressive symptoms and anxiety symptoms,23–25 and higher rates of mortality among patients who have both depressive symptoms and anxiety symptoms,26 none of these researchers reported the percentage of patients who experienced comorbid depression and anxiety versus those who experience depression or anxiety alone.
Although ours is the first study to more fully characterize the coexistence of depressive symptoms and anxiety symptoms in patients with HF, our results are consistent with findings from non-HF populations. For example, in a study of 479 psychiatric outpatients with major depressive disorder, Zimmerman et al. found that 57% of psychiatric outpatients with depression had a current, co-existing anxiety disorder, and an additional 14% had clinically significant anxiety symptoms that did not meet the diagnostic threshold for an anxiety disorder.27
Researchers have proposed two potential reasons for the high rates of comorbidity of depression and anxiety in the general population: symptom overlap and shared psychopathology.28 Symptom overlap means that patients may be labeled with anxiety or depression simply because they are experiencing several symptoms that fit into either category. According to the DSM-IV-TR, major depressive disorder and generalized anxiety disorder share 4 overlapping symptoms: difficulty sleeping, difficulty concentrating, fatigue, and psychomotor agitation/restlessness.29 In a study of 1,218 primary care patients with major depressive disorder, generalized anxiety disorder, or both, researchers found that patients with comorbid depression and anxiety endorsed significantly more of the 4 “overlapping” symptoms than patients with depression alone.28
Although researchers have found that symptoms of anxiety and depression overlap in primary care patients, it is unlikely that symptom overlap by itself would explain the high rates of coexisting anxiety and depressive symptoms found in our sample of HF patients. In the instruments that we used to measure anxiety and depressive symptoms, only one symptom—restlessness—was listed on both instruments. Researchers have proposed that high rates of comorbid anxiety and depression may be due instead to a shared psychopathology or underlying factors that predispose certain individuals to both depression and anxiety.28 For example, in twin studies, researchers have found a strong genetic link between anxiety and depression.30,31 However, this possibility has not been explored in patients with HF.
In our regression model, we found that only two predictors of anxiety status: depressive symptoms and younger age. Surprisingly, in contrast to what other researchers have reported, functional status (both NYHA class and DASI scores) and comorbidities did not predict anxiety symptoms. In Haworth et al.’s study of male outpatients with HF, predictors of generalized anxiety disorder were NYHA class, comorbidities, and a history of mental illness, with the strongest predictor being a history of mental illness. Overall, their model explained 29% of the variance and was 86% accurate in predicting classification of anxiety. Our results may differ from those of Haworth et al. because of our sample included women and patients with diastolic and systolic HF, and we used self-report instruments to measure anxiety instead of diagnostic interviews. We also included a more evenly distributed array of patients with NYHA Class I/II vs. III/IV Classes—54% of patients had NYHA Class III or IV HF, compared to 27% of patients with NYHA Class III/IV HF in Haworth et al.’s study.
Our finding of the frequent coexistence of anxiety and depression in patients with HF indicates a need for researchers to develop—and nurses and clinicians to utilize—interventions that can simultaneously treat both depression and anxiety. In their study on the comorbidity of depression and anxiety in psychiatric outpatients, Zimmerman et al. reported that the majority of patients with comorbid depression and anxiety expressed a desire to receive treatment for both conditions.27 Unfortunately, at this time, no research has been conducted testing interventions for the simultaneous treatment of depression and anxiety in patients with HF. However, a large body of evidence shows that cognitive behavior therapy, a non-pharmacological intervention, is effective for treating both depression and anxiety in the general population.32 Future investigators who test cognitive behavior therapy interventions in patients with HF should measure the effects of the intervention not only on depressive symptoms, but on symptoms of anxiety as well.
Our study was limited by its cross-sectional nature; as such we cannot make any inferences about causality of depression or anxiety. Our results are also limited by the use of instruments to measure self-reported anxiety and depressive symptoms rather than diagnostic interviews for major depressive disorder or generalized anxiety disorder. However, patients with HF frequently experience clinically significant depressive and anxiety symptoms that may not meet the diagnostic threshold for depressive disorder or generalized anxiety disorder, and we feel it is important to include a broad spectrum of anxiety and depressive symptoms in HF research. Finally, as this was a secondary data analysis, we did not have information on patients’ past psychiatric history, counseling sessions, or anti-anxiety medications. Future research on this topic should include measurement of patient’s lifetime history of anxiety and depression episodes, as well as information on past or current treatment with counseling or anti-anxiety medications.
Conclusions
Nearly one-third of outpatients with HF experienced coexisting symptoms of anxiety and depression. Patients at highest risk for experiencing anxiety symptoms include those who are younger and those who have depressive symptoms. It is important for nurses and other healthcare providers to recognize that there is a dose-response relationship between depressive symptoms and anxiety. If a patient has moderate to severe symptoms of depression, there is a strong likelihood that he or she is also experiencing anxiety symptoms. Future research is needed to identify interventions that are effective for treating both depressive symptoms and anxiety symptoms in patients with HF.
Implications for Practice.
Patients with heart failure have high rates of anxiety
Depression is the strongest predictor of anxiety in HF
Patients may need treatment for both depression and anxiety
Acknowledgements
Funding Sources: This research was supported by an American Association of Critical Care Nurses Phillips Medical Research award, the National Institutes of Health, National Institute of Nursing Research, K23 NR013480, R01 NR 008567, R01 NR 009280, the University of Kentucky General Clinical Research Center, M01RR02602, and the University of Kentucky College of Nursing Center for Biobehavioral Research on Self-Management, NINR, P20 NR 010679. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
There are no industry relationships to disclose.
References
- 1.Moser DK, Dracup K, Evangelista LS, et al. Comparison of prevalence of symptoms of depression, anxiety, and hostility in elderly patients with heart failure, myocardial infarction, and a coronary artery bypass graft. Heart Lung. 2010;39:378–385. doi: 10.1016/j.hrtlng.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moser DK. "The rust of life": Impact of anxiety on cardiac patients. Am J Crit Care. 2007;16:361–369. [PMC free article] [PubMed] [Google Scholar]
- 3.Shen BJ, Eisenberg SA, Maeda U, et al. Depression and anxiety predict decline in physical health functioning in patients with heart failure. Ann Behav Med. 2011;41:373–382. doi: 10.1007/s12160-010-9251-z. [DOI] [PubMed] [Google Scholar]
- 4.Moser DK, Heo S, Lee KS, Hammash M, et al. 'It could be worse ... Lot's worse! ' Why health-related quality of life is better in older compared with younger individuals with heart failure. Age and Ageing. 2013;42:626–632. doi: 10.1093/ageing/aft078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsuchihashi-Makaya M, Kato N, Chishaki A, et al. Anxiety and poor social support are independently associated with adverse outcomes in patients with mild heart failure. Circ J. 2009;73:280–287. doi: 10.1253/circj.cj-08-0625. [DOI] [PubMed] [Google Scholar]
- 6.Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 7.Dekker RL, Lennie TA, Albert NM, et al. Depressive symptom trajectory predicts 1-year health-related quality of life in patients with heart failure. J Card Fail. 2011;17:755–763. doi: 10.1016/j.cardfail.2011.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Judd LL, Akiskal HS, Zeller PJ, et al. Psychosocial disability during the long-term course of unipolar major depressive disorder. Arch Gen Psychiatry. 2000;57:375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- 9.Hirschfeld RM. The comorbidity of major depression and anxiety disorders: recognition and management in primary care. J Clin Psych. 2001;3:244–254. doi: 10.4088/pcc.v03n0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dekker RL. Patient perspectives about depressive symptoms in heart failure: a review of the qualitative literature. J Cardiovasc Nurs. 2012 doi: 10.1097/JCN.0b013e318273a5d6. Epub ahead of print 13 Nov 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riegel B, Moser DK, Rayens MK, et al. Ethnic differences in quality of life in persons with heart failure. J Card Fail. 2008;14:41–47. doi: 10.1016/j.cardfail.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 12.Riegel B, Moser DK, Glaser D, et al. The Minnesota living with heart failure questionnaire: sensitivity to differences and responsiveness to intervention intensity in a clinical population. Nurs Res. 2002;51:209–218. doi: 10.1097/00006199-200207000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Derogatis LP. Brief symptom inventory: Administration, scoring, and procedure manual. Minneapolis: National Compute Systems, Inc.; 1993. [Google Scholar]
- 14.Khalil AA, Hall LA, Moser DK, et al. The psychometric properties of the Brief Symptom Inventory depression and anxiety subscales in patients with heart failure and with or without renal dysfunction. Arch Psychiatr Nurs. 2011;25:419–429. doi: 10.1016/j.apnu.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Abu Ruz ME, Lennie TA, Riegel B, et al. Evidence that the Brief Symptom Inventory can be used to measure anxiety quickly and reliably in patients hospitalized for acute myocardial infarction. J Cardiovasc Nurs. 2010;25:117–123. doi: 10.1097/JCN.0b013e3181b56626. [DOI] [PubMed] [Google Scholar]
- 16.Grothe KB, Dutton GR, Jones GN, et al. Validation of the Beck Depression Inventory-II in a low-income african american sample of medical outpatients. Psychol Assess. 2005;17:110–114. doi: 10.1037/1040-3590.17.1.110. [DOI] [PubMed] [Google Scholar]
- 17.Whisman MA, Perez JE, Ramel W. Factor structure of the Beck Depression Inventory-second edition (BDI-II) in a student sample. J Clin Psychol. 2000;56:545–551. doi: 10.1002/(sici)1097-4679(200004)56:4<545::aid-jclp7>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 18.Mills RM, Jr, Haught WH. Evaluation of heart failure patients: objective parameters to assess functional capacity. Clin Cardiol. 1996;19:455–460. doi: 10.1002/clc.4960190603. [DOI] [PubMed] [Google Scholar]
- 19.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64:651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 20.Katz JN, Chang LC, Sangha O, et al. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.Haworth JE, Moniz-Cook E, Clark AL, et al. Prevalence and predictors of anxiety and depression in a sample of chronic heart failure patients with left ventricular systolic dysfunction. Eur J Heart Fail. 2005;7:803–808. doi: 10.1016/j.ejheart.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 23.Jiang W, Kuchibhatla M, Cuffe MS, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110:3452–3456. doi: 10.1161/01.CIR.0000148138.25157.F9. [DOI] [PubMed] [Google Scholar]
- 24.Riedinger MS, Dracup KA, Brecht ML. Quality of life in women with heart failure, normative groups, and patients with other chronic conditions. Am J Crit Care. 2002;11:211–219. [PubMed] [Google Scholar]
- 25.Friedmann E, Son H, Thomas SA, et al. Poor social support is associated with increases in depression but not anxiety over 2 years in heart failure outpatients. J Cardiovasc Nurs. 2013 doi: 10.1097/JCN.0b013e318276fa07. Epub ahead of print 14 Jan 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedmann E, Thomas SA, Liu F, et al. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152:940–948. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerman M, Chelminski I, McDermut W. Major depressive disorder and axis I diagnostic comorbidity. J Clin Psychiatry. 2002;63:187–193. doi: 10.4088/jcp.v63n0303. [DOI] [PubMed] [Google Scholar]
- 28.Zbozinek TD, Rose RD, Wolitzky-Taylor KB, et al. Diagnostic overlap of generalized anxiety disorder and major depressive disorder in a primary care sample. Depress Anxiety. 2012;29:1065–1071. doi: 10.1002/da.22026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 30.Roy MA, Neale MC, Pedersen NL, et al. A twin study of generalized anxiety disorder and major depression. Psychol Med. 1995;25:1037–1049. doi: 10.1017/s0033291700037533. [DOI] [PubMed] [Google Scholar]
- 31.Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychol Med. 2007;37:453–462. doi: 10.1017/S0033291706009135. [DOI] [PubMed] [Google Scholar]
- 32.Beck AT. The current state of cognitive therapy: A 40-year retrospective. Arch Gen Psychiatry. 2005;62:953–959. doi: 10.1001/archpsyc.62.9.953. [DOI] [PubMed] [Google Scholar]