Abstract
Strenuous physical activity has been linked to pelvic floor disorders in women. Using a novel wireless intra-vaginal pressure transducer, intra-abdominal pressure was measured during diverse activities in a laboratory. Fifty-seven women performed a prescribed protocol using the intra-vaginal pressure transducer. We calculated maximal, area under the curve and first moment of the area intra-abdominal pressure for each activity. Planned comparisons of pressure were made between levels of walking and cycling and between activities with reported high pressure in the literature. Findings indicate variability in intra-abdominal pressure amongst individuals doing the same activity, especially in activities that required regulation of effort. There were statistically significant differences in maximal pressure between levels of walking, cycling and high pressure activities. Results for area under the curve and first moment of the area were not always consistent with maximal pressure. Coughing had the highest maximal pressure, but had lower area under the curve and first moment of the area compared to most activities. Our data reflect novel findings of maximal, area under the curve and first moment of the area measures of intra-abdominal pressure, which may have clinical relevance for how physical activity relates to pelvic floor dysfunction.
Keywords: EXERCISE, PELVIC FLOOR, STRENUOUS ACTIVITY, AREA UNDER THE CURVE, FIRST MOMENT OF AREA
Introduction
Evidence has emerged to suggest that strenuous physical activity increases the risk for pelvic floor disorders, such as pelvic organ prolapse and urinary incontinence (Chiaffarino et al., 1999; Hendrix et al., 2002; Jørgensen, Hein, & Gyntelberg, 1994; Woodman et al., 2006). There is great need to establish methods to assess this evidence. Defining ‘strenuous’ is for the most part subjective; in the pelvic floor literature, strenuous usually refers to activities that are thought to significantly elevate intra-abdominal pressure (Guttormson, Tschirhart, Boysen, & Martinson, 2008; Nygaard, Hamad, & Shaw, 2013; Weir, Nygaard, Wilken, Brandt, & Janz, 2006). Efforts to measure intra-abdominal pressure during activities have been limited by the need for invasive catheters that must be connected via short tethers to laboratory equipment, as well as by lack of standardisation in defining maximal intra-abdominal pressure. Existing studies that approximate intra-abdominal pressure during certain physical activities by means of vesical, rectal and nasogastric transducers reveal that the range of pressure during specific activities across studies is large, with little concordance in peak intra-abdominal pressures across studies (Nygaard et al., 2013).
To explore the association between physical activity and intra-abdominal pressure, our group developed a novel wireless intra-vaginal pressure transducer to measure intra-abdominal pressure during activities (Coleman et al., 2012). The new intra-vaginal pressure transducer has documented criterion validity (Hsu et al., 2012) and allows for the assessment of diverse activities across a range of intensities and body positions, since the measurement of intra-abdominal pressure is not constrained by wired technology as in previous work (Cobb et al., 2005; Guttormson et al., 2008; Weir et al., 2006).
The most common measurement of intra-abdominal pressure during physical activities found in the literature is maximal pressure. Descriptions of how maximal intra-abdominal pressure is calculated vary or are absent from literature to date. We have described standardised methods for assessing maximal pressure during physical activity (Hamad et al., 2013). However, other qualities of intra-abdominal pressure besides maximal pressure may also be relevant to understanding the impact of strenuous activities on conditions such as pelvic floor disorders. Area under the curve reflects both amplitude and duration of pressure but lacks sensitivity in distinguishing long duration/low pressure activities from short duration/ high pressure activities. First moment of the area overcomes this limitation of traditional area under the curve measurement by placing greater emphasis on the amplitude of pressure than on duration and is expressed as cmH2O2·s. We propose that adding area under the curve and first moment of the area to maximal measurement of intra-abdominal pressure may ultimately further the understanding of links between physical activity and pelvic floor disorders.
The primary aim of this study is to describe maximal, area under the curve, and first moment of the area intra-abdominal pressures obtained using our newly developed, wireless intra-vaginal pressure transducer during a wide variety of common exercise and routine physical activities performed in an exercise science laboratory. Secondary aims are to compare pressure measures between select activities with varying levels of intensity and to compare pressure measures obtained during specific strenuous activities (lifting, sit-ups and running) and coughing, as the latter is the standard for eliciting high intra-abdominal pressure in clinical urodynamic studies.
Methods
Participants were 57 women aged 18 to 54 years that reported engaging in vigorous exercise at least three times per week. Women were excluded if they had a positive response to any question on the Physical Activity Readiness Questionnaire (Thomas, Reading, & Shephard, 1992), were currently pregnant, six months post partum, or had a current injury that would prohibit the completion of the exercise protocol. A major research University’s Institutional Review Board, which conforms to the declaration of Helsinki, approved study procedures and all participants provided written informed consent.
Assessment of Intra-abdominal pressure
A complete description of the intra-vaginal pressure transducer used in this study as well as evidence for its criterion validity and feasibility of use are detailed elsewhere (Coleman et al., 2012; Hsu et al., 2012). In brief, the intra-vaginal pressure transducer includes a pressure sensor sealed inside a tampon-sized gel-filled capsule, a tether made of flexible polymer tubing that provides an atmospheric pressure reference and also allows for transducer removal, and an antenna for communicating pressure data wirelessly to a base station located in the laboratory.
Laboratory Protocol
The exercise protocol was completed in a Human Performance Laboratory at a major research University. Participants reported to the laboratory in light exercise clothes. Height and weight were obtained without shoes. After voiding their bladders, women were instructed to insert the transducer into the upper vagina in a manner similar to inserting a tampon. The external antenna was then taped to the abdomen at or slightly above the anterior superior iliac spine.
The standardised activity protocol consisted of 31 activities that included clinical assessments, light, moderate and vigorous intensity exercise tasks and routine household activities. Activity sessions were completed on days when participants were not menstruating and were done in the same temperature controlled indoor laboratory. Each woman completed the exercise protocol on two separate occasions. Although the criterion validity of the intra-vaginal pressure transducer was confirmed in controlled, urogynaecology dynamics testing (Hsu et al., 2012), we were interested in assessing the reproducibility of intra-abdominal pressure as measured by the transducer during this activity protocol (analysis in progress).
Activities were performed in a laboratory equipped with a Quinton Q-Stress TM55 treadmill (Bothell, Washington, USA), a Monark 828E cycle ergometer (Vansbro, Sweden), exercise dumbbells, a 20.3 cm exercise step, and a variety of household items for lifting and carrying activities. Specific activities are shown in Tables 1, 2 and 3. Most activities in the laboratory protocol required 20 to 40 seconds to complete. For clinical assessments and lifting tasks, participants were instructed to do a prescribed number of repetitions. Participants did three repetitions each of coughing and seated and lying Valsalva manoeuvre, modified Superman trunk extension exercise and lifting and carrying tasks. For each level of seated shoulder press, participants were instructed to do eight repetitions and for jumping, each participant jumped in place 10 times. The remaining activities were completed in 30-second time intervals. Each laboratory session required about one hour to complete. The order of laboratory activities was consistent with a standard exercise protocol that involved gradual warm up progressing to higher intensity activities (walking, running, cycling), followed by easier tasks to reduce heart rate (stepping, sit to stand), lifting and carrying tasks, and ended with stretching. However, Valsalva manoeuvre and jumping were placed at the end of the protocol in the event they resulted in displacement of the sensor, which would have interrupted natural flow of the protocol.
Table 1.
Descriptive summary of intra-abdominal pressure (IAP) for urodynamic and aerobic activities
| ACTIVITY | N | Range Maximal IAP |
Median Maximal IAP (IQR) |
Range AUC | Median AUC (IQR) | Range FMA | Median FMA (IQR) |
|---|---|---|---|---|---|---|---|
| Clinical Assessments |
CmH2O |
CmH2O∙s |
CmH2O2∙s |
||||
| Coughing* | 53 | 37.6–199.9 | 90.5 (72.1–121.5) | 51.4–346.6 | 133 (107.9–190.4) | 483.4–16320.6 | 3298.9 (1908.3–6278) |
| Lying Valsalva* | 57 | 17.1–176.2 | 91.3 (67.9–108.8) | 420.9–2827.4 | 1356.7 (1054.6–1768.6) | 4190.4–155451.3 | 46468.2 (28364.2–69875.2) |
| Seated Valsalva* | 57 | 16.5–207.7 | 129.3 (106.5–153.2) | 680.7–4508 | 2076.8 (1569.2–2607.3) | 3993.7–325274.1 | 101405.5 (61625.9–143048.3) |
| Aerobic Activities | |||||||
| Walk 4.8km·h−1, 0% grade‡ | 57 | 15.3–36.6 | 24.6 (22.5–26.2) | 64.1–161.1 | 99.7 (92.3–115.4) | 299–1858.8 | 679.9 (573.8–893.9) |
| Walk 4.8 km·h−1, 7% grade‡ | 57 | 16.6–50.5 | 29.3 (26.2–31.8) | 69.3–177.6 | 112.9 (100.5–128.7) | 362.9–2582.3 | 933.9 (743.6–1162.5) |
| Walk 5.6 km·h−1, 7% Grade ‡ | 57 | 20.1–56.1 | 35 (31.4–39.4) | 93–223.1 | 146.1 (130.6–161.8) | 596.9–3552.2 | 1537.9 (1196.2–1845.9) |
| Walk 4.3 km·h−1, 0% grade, with 11.4 kg weight ‡ | 57 | 12.1–44.3 | 27 (24.1–30.5) | 58.1–195.8 | 106 (97.4–119.8) | 212.2–2638.3 | 767.9 (654.6–940.7) |
| Run 8–9.7 km·h−1, 0% grade‡ | 57 | 32.4–98.7 | 66.5 (56–74.1) | 116.7–361.4 | 265.4 (229.2–289.9) | 914.1–11224.1 | 5872.9 (4139.7–7039.9) |
| Stepping, 20 cm Step‡ | 57 | 21.4–48.2 | 30.4 (25.4–36.1) | 69.6–160.9 | 99.4 (84.1–116.9) | 349.7–1764 | 702.5 (484.8–996.3) |
| Seated cycling 300kg·m·min−1‡ | 57 | 4–16.5 | 8.1 (6.7–9.6) | 17.8–69.1 | 38.1 (31.5–45.3) | 21.4–321.8 | 97.3 (62.9–135.9) |
| Seated cycling 600 kg·m·min−1‡ | 57 | 5.4–20.6 | 10.8 (9.4–11.9) | 24.9–94.6 | 49.8 (43.8–54.5) | 39.7–584.7 | 163.6 (121.2–192.8) |
| Standing cycling 900 kg·m·min−1‡ | 57 | 14.5–66.9 | 41.6 (34.7–51.7) | 64.5–218.1 | 152.3 (130.2–180.4) | 260.2–4216.3 | 1866.5 (1280.9–2530) |
Note: N= number of participants to complete a given activity with adequate data; IAP= intra-abdominal pressure; AUC= Area under the curve, FMA= First moment of the area; IQR= Interquartile range; km·h−1 = kilometers per hour; kg·m·min−1 = kilogram meters per minute;
= 3 peak activities;
= 5 peak activities;
= 10 peak activities
Table 2.
Descriptive summary of intra-abdominal pressure (IAP) for household and lifting activities
| ACTIVITY | N | Range Maximal IAP |
Median Maximal IAP (IQR) |
Range AUC | Median AUC (IQR) | Range FMA | Median FMA (IQR) |
|---|---|---|---|---|---|---|---|
| Household Activities |
CmH2O |
CmH2O∙s |
CmH2O2∙s |
||||
| Erasing board, dusting ‡ | 57 | 4.2–25.3 | 9.5 (8–12.8) | 21.3–118.4 | 43.6 (37.4–60.8) | 28.5–821.8 | 146 (95.8–248) |
| Scrubbing floor on hands and knees‡ | 57 | 5.4–58.6 | 10.2 (8.1–13.9) | 25–253.8 | 43.9 (35.3–57.4) | 41.3–4297.5 | 135.7 (87.7–236.5) |
| Stand to sit† | 56 | 20.6–99.7 | 31.9 (28.4–39) | 87.3–342.9 | 141.3 (123–165.2) | 467.8–11214.2 | 1254.8 (960.5–1728.9) |
| Lifting Tasks | |||||||
| Lift 13.6 kg, floor to counter & back† | 57 | 17.1–62.6 | 34.5 (28.1–41.1) | 97.1–985.3 | 361.2 (286.2–461.1) | 579.5–16056.8 | 3822.3 (2272.2–4974.5) |
| Lift 18.2 kg, floor to counter & back† | 57 | 13.6–120 | 47.9 (37.6–59.7) | 40.8–1426.2 | 454.5 (371.1–621.3) | 217.3–32320.9 | 5828.5 (3958.9–9091.3) |
| Seated shoulder press, 3.6 kg† | 47 | 4–31.9 | 8.3 (6.2–12.8) | 37.4–311.5 | 76.5 (59.7–138.5) | 44.2–1528.2 | 206.4 (107.8–561.9) |
| Seated shoulder press, 4.5 kg† | 48 | 5.5–36.3 | 11.5 (8.1–15.2) | 31.3–361.5 | 108.7 (82.9–156.9) | 45.4–3917.7 | 372.1 (189.9–662.5) |
| Seated shoulder press, 5.5 kg † | 41 | 3.9–24.9 | 10.5 (7.7–13.8) | 11.5–190.2 | 100.7 (70.9–118.7) | 17.4–1113.2 | 290.8 (160.6–496.8) |
| Seated shoulder press, 6.8 kg† | 12 | 8.1–19.3 | 10.8 (9.5–14.7) | 43.8–163.3 | 99 (65.9–122) | 118.1–914.1 | 319.8 (178.3–479.9) |
| Seated shoulder press, 9.1 kg † | 9 | 10.4–36.5 | 18.8 (13.1–30.2) | 80–292.6 | 180.9 (90.2–208.8) | 282.3–2569.8 | 1046.7 (474.4–2062.7) |
Note: N= number of participants to complete a given activity with adequate data; IAP= intra-abdominal pressure; AUC= Area under the curve, FMA= First moment of the area; IQR= Inter-quartile range;
=3 peak activities;
=5 peak activities;
=10 peak activities
Table 3.
Descriptive summary of intra-abdominal pressure (IAP) for callisthenic and stretching activities
| Activity | N | Range Maximal IAP |
Median Maximal IAP (IQR) |
Range AUC | Median AUC (IQR) | Range FMA | Median FMA (IQR) |
|---|---|---|---|---|---|---|---|
| Callisthenic Activities |
CmH2O |
CmH2O∙s |
CmH2O2∙s |
||||
| Abdominal curl ups † | 57 | 6.5–82.3 | 18.5 (13.1–27.2) | 30.5–236.2 | 67 (50.4–87.8) | 56.8–4731.2 | 321.5 (171.6–680.9) |
| Full sit ups with feet held † | 57 | 13.9–128.5 | 60.4 (48.3–77.4) | 62.2–568.3 | 263 (226–307) | 259.7–20722.2 | 4526.6 (3440.4–6103.3) |
| Isometric side bridge † | 56 | 3–50.4 | 15.7 (11.7–19.9) | 14.2–227.7 | 68.2 (52.8–89) | 12.9–3423.4 | 308.1 (200.2–525.7) |
| Modified superman‡ | 56 | 10–45.4 | 19.9 (14.7–27.3) | 95.5–790.7 | 286.1 (217.7–365.1) | 338.5–8658.2 | 1809.4 (1054–2983.5) |
| Push-ups from knees‡ | 57 | 4–42.5 | 15.3 (11.2–20.3) | 19–165.2 | 72.3 (52.1–87.8) | 36.7–2184.9 | 357.3 (199.6–582.9) |
| Jumping ‡ | 55 | 25.7–153.9 | 91.2 (71.8–104.8) | 242–1516.6 | 627.8 (471.8–739.6) | 1904.9–51125.5 | 14903.8 (10363.2–19703.1) |
| Stretching Activities | |||||||
| Seated hamstring stretch ‡ | 57 | 4.2–21.9 | 9.4 (7.2–13.3) | 20–81 | 37 (30.4–52) | 29.4–519.3 | 126.7 (74.4–240.8) |
| Lower back stretch‡ | 57 | 2.5–10.4 | 6 (4.4–7.5) | 11.6–54.4 | 26.7 (20.3–34.3) | 9.7–231.9 | 59.5 (30.5–99.9) |
| Side lying quadriceps stretch‡ | 57 | 0.6–30.4 | 10.5 (8.1–13.1) | 2.9–126.7 | 40.6 (32.4–49) | 0.8–1518.3 | 204.8 (111–320.2) |
Note: N= number of participants to complete a given activity with adequate data; IAP= intra-abdominal pressure; AUC= Area under the curve, FMA= First moment of the area; IQR= Inter-quartile range;
=3 peak activities;
=5 peak activities;
=10 peak activities
In the final 54 participants, we measured intra-abdominal pressure during three pelvic floor muscle contractions (Kegel exercise) in the supine position at the end of the standard exercise protocol. This was done as a quality assurance measure, to ensure that the sensor was in the upper vagina approximating intra-abdominal pressure, and not in the lower vagina, measuring pelvic muscle contraction pressure (Bø & Finckenhagen, 2003; Bø & Sherburn, 2005; Hilde et al., 2013; Hsu et al., 2012). The typical range of pelvic muscle contraction strength in young and middle-aged women is 25 to 50 cmH2O (though with significant inter-individual variation, with ranges up to 120 cmH2O) and thus, if pressures generated during pelvic muscle contractions were generally low, it is likely that the transducer is indeed in the upper vagina.
There is no commonly accepted method of defining maximal pressure during activity. We considered many methods, explained in detail elsewhere (Hamad et al., 2013). We chose to measure maximal pressure as a function of the number of peaks that were representative of the highest pressures during activity. Activities were classified as three peak, five peak or ten peak activities (Summarised in Tables 1–3). We developed a computer program using Matlab software (R2009A, MathWorks; Natick, Massachusetts, USA) to identify peaks and troughs. In the event that a pressure tracing was not of sufficient duration (ie, the base station did not capture the entire activity segment through wireless transmission) to calculate maximal pressure on the basis of the assigned number of peaks, then the activity segment was considered unanalyzable. Maximal pressure from three peak activities was calculated as the mean of the difference between the three highest peaks and the three lowest troughs obtained from the pressure tracing for that activity. Maximal pressure from the five and ten peak activities were similarly calculated, but instead used the five highest and lowest or the ten highest and lowest pressure values. For calculation of area under the curve and first moment of the area, we used the three, five or ten trough average to generate a baseline and then calculated the area under the pressure tracing above that line. For activities that were performed for a 30 second time period, measures of area under the curve and first moment of the area were standardised to reflect 10 second time periods. For activities that were performed for a set number of repetitions, duration was not standardised since this could result in comparing activity segments of differing repetitions.
We chose to calculate pressure measures as the differences between highest and lowest peaks, that is, the net pressure, rather than as the difference between highest peaks and some arbitrary baseline (absolute pressure) because our clinical interest lies in understanding the degree to which certain activities increase intra-abdominal pressure. Additionally, using atmospheric pressure as a baseline reference would reflect resting intra-abdominal pressure for many activities on the lower end of our intensity range.
To describe pressures during these activities, we used data collected during the first exercise session. However, if data for a specific activity segment was incomplete or not able to be obtained, we used data from the second session for that specific activity. Reasons for an incomplete or absent data segment included: 1) participant was physically unable to complete a segment, 2) the sensor fell out of or into the lower vagina, or 3) the base station did not appropriately detect the signals from the sensor.
Data analysis
The sample size was calculated based on the ability to assess the reproducibility of the intra-vaginal pressure transducer. Fifty-six women were determined to be adequate to provide 80 % power to provide a 95 % confidence interval of width 0.1 for an expected intraclass correlation of 0.8, using Bonett’s correction and NQUERY software (Saugus, Massachusetts, USA).
We evaluated frequency distributions for each activity. Activities were generally normally distributed, though some were shifted to the right or left. We observed no bimodal distributions. We used descriptive statistics to describe the mean and median net maximal intra-abdominal pressure, area under the curve and first moment of the area. Given the large number of activities, we did not perform across activity comparisons. We selected a priori the following comparisons, which aimed to evaluate pressure differences in similar activities with varying intensities. These included: 1) walking at 4.8 km·h−1 on level grade vs walking at 4.8 km·h−1 on 7 % grade; 2) walking at 4.8 km·h−1 on level grade vs walking at 4.3 km·h−1 on level grade while carrying 11.4 kg (to mimic carrying a toddler); 3) seated cycling at 450 kg·m·min−1 vs moderate intensity seated cycling at 600 kg·m·min−1; 4) seated cycling at 600 kg·m·min−1 vs standing cycling at 900 kg·m·min−1, and 5) coughing, commonly assessed as a high pressure measure in clinical urogynaecology settings, to each of four activities performed in home or fitness settings that are assumed to have high intra-abdominal pressure: lifting and carrying 18.2 kg, abdominal curl ups, full sit ups, and running. Wilcoxon signed rank tests were used for these nine comparisons. Significance was accepted at p <.005 to adjust for multiple tests.
Standing absolute intra-abdominal pressure is known to increase with increases in body mass index (Cobb et al., 2005). To assess whether an association exists between body mass index and net maximal intra-abdominal pressure during a priori specified activities performed in the standing position, we used Spearman rank correlation coefficients to compare body mass index with intra-abdominal pressure for jumping, and lifting and carrying 18.2 kg. Finally, we assessed the correlation between age and intra-abdominal pressure for the same three activities using Spearman rank correlation coefficients. For Spearman correlations significance was accepted at p <.05. Wilconxon signed rank tests and Spearman correlation statistics were run with Matlab Statistics Package (Natick, Massachusetts, USA).
Results
We enrolled 60 women. Their mean age was 30.4 years (SD 9.3), mean body mass index 22.4 kg/m2 (SD 2.68) and 74 % were nulliparous. Of these 60 women, 57 women completed two sessions. Fifty-six had adequate data from the first session. One woman had unusually high pressures (up to ~200 cmH2O) during seated activities done in the first session. A pelvic examination done to rule out a pelvic mass or other abnormality was normal. Pressures during her second session were much lower and in the range of other participants; therefore we used data from this second session to describe her intra-abdominal pressures. Using her second session did not change mean values and only decreased the upper range limit of three activities done in the seated position. All, but six women retained the sensor in the upper vagina during all activities performed in both sessions. Four women stated that they felt the sensor fall down into the lower vagina during an activity session, while two stated that it fell out into their underwear.
The mean net rise in intra-abdominal pressure during pelvic muscle contraction in the supine position was 4.4 (SD 4.9) cmH2O. Despite being given specific instructions to only contract the pelvic floor muscles, seven women were observed to be straining during their attempt to contract the pelvic muscles; when we removed them from the analysis, the mean net rise in intra-abdominal pressure was 3.3 (SD 2.6) cmH2O. This small increase in pressure was statistically different (p<0.001) from the mean pressure assessed during supine baseline measurement (mean 1.7 SD 1.5 H2O).
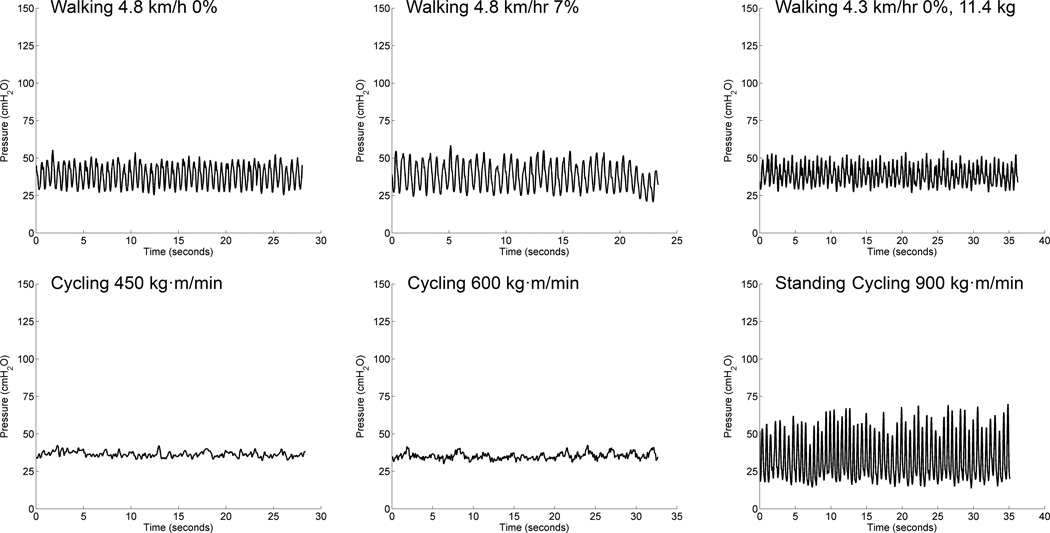
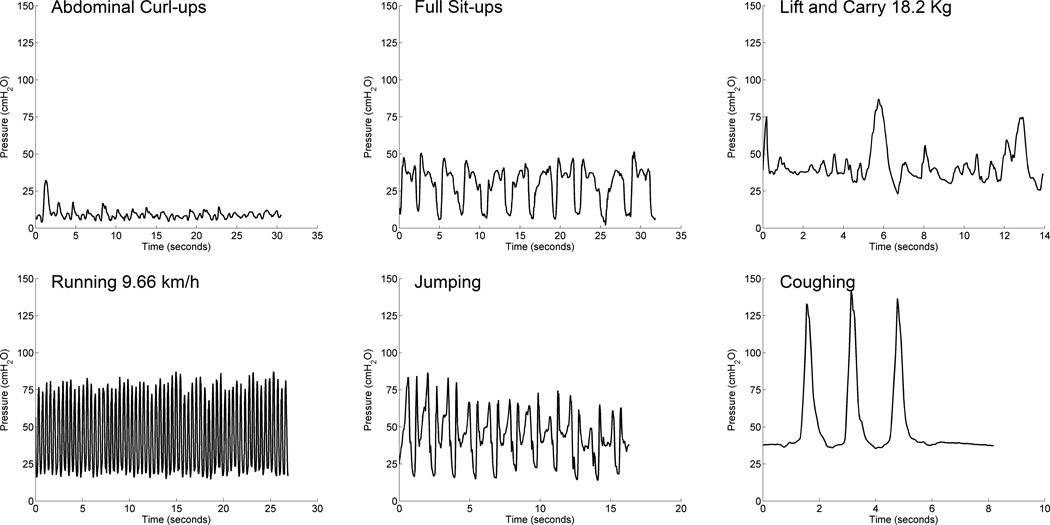
A descriptive summary of intra-abdominal pressures grouped by activity type is provided in Tables 1–3. Variability in response was evident in the wide range of pressure values. Sample pressure tracings for activities compared statistically are found in Figures 3 and 4.
Figure 3.
Representative pressure tracings for three levels of walking and for three levels of cycling.
Figure 4.
Representative pressure tracings for activities considered to result in high intra-abdominal pressure (IAP).
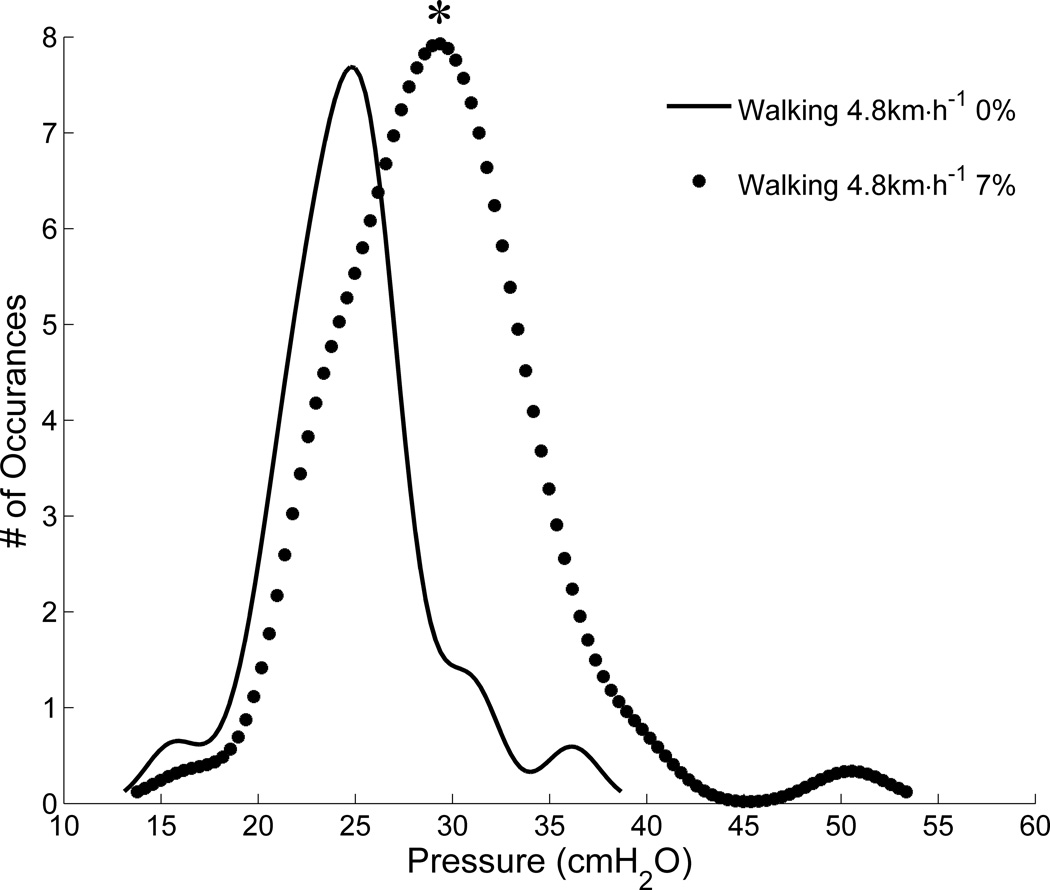
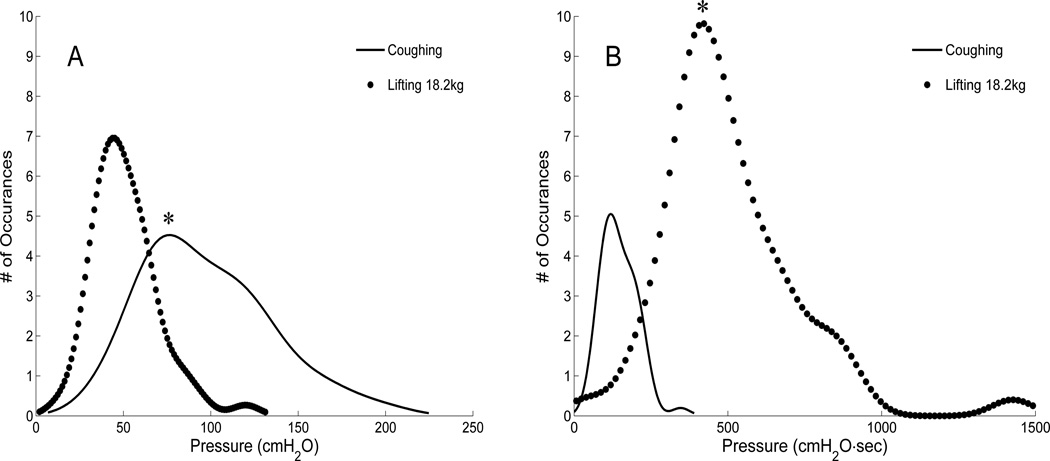
There were statistically significant (p<0.001) differences in median maximal intra-abdominal pressure between walking at 4.8 km·h−1 on level grade vs walking at 4.8 km·h−1 on 7 % grade and walking at 4.8 km·h−1 on level grade vs walking at 4.3 km·h−1 on level grade while carrying 11.4 kg (Table 1, Figure 1). However, only the differences in area under the curve and first moment of the area were statistically significant for walking on level versus walking at 7 % grade. There were no statistically significant differences between walking on level grade with and without carrying 11.4 kg for area under the curve or first moment of the area. For the levels of cycling, intra-abdominal pressure measured by median maximal, area under the curve and first moment of the area during seated cycling at 450 kg·m·min−1 was lower than seated cycling at 600 kg·m·min−1 which was lower than standing cycling at 900 kg·m·min−1 (Table 1). Coughing raised the median maximal intra-abdominal pressure more than lifting and carrying 18.2 kg, abdominal curl ups, full sit ups, and running; however, coughing was significantly lower than all of these activities except for abdominal curl ups for area under the curve. Coughing remained significantly higher than abdominal curl ups for area under the curve. For first moment of the area, results were similar to area under the curve, as coughing was lower than running and lifting and carrying 18.2 kg; was nearly significantly lower than full sit ups (p=0.0057) but remained higher than abdominal curl ups (Tables 1–3).
Figure 1.
Maximal intra-abdominal pressure (IAP) during walking at 7 % grade is higher than maximal intra-abdominal pressure (IAP) during walking on level grade. *p <0.0001.
There was a weak correlation between body mass index and maximal intra-abdominal pressure during jumping (r=0.28, p=.04) but no significant correlations between body mass index and maximal intra-abdominal pressure during lifting 18.2 kg (r=0.23, p=.09), age and maximal intra-abdominal pressure during lifting 18.2 kg (r=0.09, p=0.53) or age and maximal intra-abdominal pressure during jumping (r= −0.09, p=0.50).
Discussion
We describe intra-abdominal pressure for a range of activities using novel, wireless technology. High intra-abdominal pressure during exercise and other physical tasks done at work and in the home have been proposed to increase risk for pelvic floor disorders in women. To study this association, it is important to have valid tools to feasibly collect pressure data during activities that women may do and in typical manner that is not constrained by wired technology. While clinical urogynaecological assessments (coughing and Valsalva manoeuvre) are not usual household or leisure activities, we described these as well to provide a basis of comparison to typical exercise and household tasks.
Our data reflect novel findings of intra-abdominal pressure in women. While most reports focus solely on maximal pressure, we included the calculation of maximal, area under the curve and first moment of the area expressions of intra-abdominal pressure. The area under the curve calculation equally weights time and amplitude of pressure while first moment of the area takes time into consideration but prioritises the amplitude of pressure. These measures provide new descriptive tools for evaluating intra-abdominal pressure during activity. Because our assessment of maximal pressure reflects a net and not an absolute pressure increase, the weak to non-significant relationship between intra-abdominal pressure during jumping and lifting and carrying 18.2 kg and body mass index is logical. In the relatively young group we tested, it does not appear that age is related to intra-abdominal pressure.
For many activities, the trends for area under the curve and first moment of the area were similar to those of maximal pressure. The differences in levels of cycling reflect this trend quite well. However, some activity comparisons revealed interesting variability. For walking, maximal pressure was significantly higher at 7 % grade and for walking with weight when compared to walking at level grade, yet area under the curve and first moment of the area were only different between the uphill walking condition and walking at level grade. The differences between walking on level grade and slightly slower walking while carrying 11.4 kg were not significant for area under the curve and first moment of the area. The time component for these activities was standardised and the amplitude differences reflected the entire area under a constructed line of maximal pressure. Therefore, the increase in grade was a greater influence on area under the curve and first moment of the area expressions of intra-abdominal pressure during walking than the addition of carrying weight similar to that of a toddler.
The activities performed in this study produce intra-abdominal pressures that vary considerably in rise time, peak pressure and duration. We have previously shown that the intra-vaginal pressure transducer is capable of measuring rapidly changing pressures without the overshoot or resonance that is typical of fluid filled systems (Coleman et al., 2010; Johnson, Rosenbluth, Nygaard, Parikh, & Hitchcock, 2009). These previous studies evaluated the pressure transducer response to both an impulse and swept sine wave and showed that the natural frequencies and damping coefficients were incalculable demonstrating no measurable overshoot during the swept sine or impulse tests.
The comparison of coughing to activities that are classically restricted in post-surgical patients revealed different trends in maximal, area under the curve and first moment of the area intra-abdominal pressure. While coughing is recognised as producing high maximal pressure, as we have demonstrated, the relatively short duration of coughing in our protocol (three maximal coughs in standing position) resulted in lower measures of area under the curve and first moment of the area than most comparisons. Because of amplitude differences, however, coughing remained significantly higher than abdominal curl ups for area under the curve and first moment of the area, despite curl ups having longer duration. We specifically examined area under the curve intra-abdominal pressure of coughing and lifting and carrying 18.2 kg since participants were directed to do each of these activities three times (Figure 2). The median maximal pressure was highest for coughing, but the area under the curve pressure was highest for the lifting task, because completing the lifting task involved sustained elevation of pressure over greater duration to complete the three repetitions.
Figure 2.
A: Maximal intra-abdominal pressure (IAP) during 3 maximal coughs is greater than maximal intra-abdominal pressure (IAP) while lifting and carrying 18.2 kg. *p <0.0001 B: Area under the curve (AUC) intra-abdominal pressure (IAP) while lifting and carrying 18.2 kg is greater than AUC IAP during 3 maximal coughs. *p <0.0001.
Some of the intra-abdominal pressures during activities we tested have been described previously; our results fit in the range of others (Cobb et al., 2005; Essendrop, Hye-Knudsen, Skotte, Hansen, & Schibye, 2004; Gerten et al., 2008; Guttormson et al., 2008; Hagins, Pietrek, Sheikhzadeh, Nordin, & Axen, 2004; Weir et al., 2006), though it is important to note that the variability in intra-abdominal pressure between different studies is large and due in part to the variety of methods used for collecting intra-abdominal pressure as well as to multiple methods for calculating maximal pressure. Of greater clinical interest is the wide range of intra-abdominal pressures we found amongst different women doing the same activity. We found the greatest degree of variability in activities that were novel and/or required participants to control their effort. For example, walking on the treadmill exhibited little variability. Walking is a familiar activity and the speed and grade, which we presumed would be tolerable for all participants, afforded little opportunity for participants to regulate effort. On the other hand, Valsalva manoeuvre, jumping and standing cycling showed great variability. All required participants to exert effort based upon the instruction given and may have been novel to participants. Valsalva manoeuvre and jumping were to be performed at maximal effort. The cadence and resistance for standing cycling were set the same for all participants, but it was evident that many women did not normally do this activity.
Variability in intra-abdominal pressure for a given activity is of interest to clinicians especially for activities that may be restricted in the post-surgical patient or in those at risk for pelvic floor disorders. There is no established, data-based threshold of maximal intra-abdominal pressure that is used to guide activity restriction for safety purposes. Ideally, a population of women would be followed prospectively to determine their intra-abdominal pressure exposure and then determine risk for diagnosis of a pelvic floor disorder on the basis of that exposure, which is not practical. From laboratory studies such as this, a theoretical threshold could be established (for example, activities with median net intra-abdominal pressure > 60 cmH2O or some other cut-point) and activities that elevate intra-abdominal pressure above that threshold would be restricted. However, given the variability of intra-abdominal pressure, some women would be unnecessarily restricted from doing healthful activity. There is great need to better understand the causes of variability in intra-abdominal pressure with activity, so that personal activity restrictions can be made when appropriate, such as in the post-surgical patient. At present, we believe the large individual variation in intra-abdominal pressure prohibits generalised activity restriction recommendations.
This study has several strengths. We used a novel, wireless intra-vaginal pressure transducer with known validity. It was well tolerated, as evidenced by our low attrition rate. We describe a variety of activity-related intra-abdominal pressures with a relatively large sample size. All of the activities were standardised by using the same equipment and scripted descriptions with all participants. The activities we describe include clinically-relevant assessments as well as common exercise and household activities, some of which are typically restricted by clinicians. The addition of area under the curve and first moment of the area expressions of intra-abdominal pressure may provide more tools to assess potential relationships between strenuous physical activity and pelvic floor disorders.
Our study is not without limitations. We measured pressures in the upper vagina, which have been shown to approximate intra-abdominal pressure measured via rectal or bladder transducers (Al-Taher, Sutherst, Richmond, & Brown, 1987; James, Niblett, MacNaughton, & Shaldon, 1987). However, measuring intra-abdominal pressure from any cavity other than the actual intra-abdominal cavity adds some element of uncertainty. Measuring from the vagina likely adds unknown pressures from viscera, vaginal smooth muscle, and other unknown sources. Because we are interested in how and whether intra-abdominal pressure of varying magnitude impacts the pelvic floor, we believe it is important to assess pressures in the upper vagina or upper rectum, as these pressures would be most likely to transmit to the pelvic floor (that is, the forces exerted on the pelvic floor include not only intra-abdominal pressure but also upper vaginal and rectal forces). Based on the low net pressure rise observed while participants performed pelvic muscle contraction (3–5 cmH2O, rather than the 25–50 cmH2O rise in pressure seen during an actual pelvic muscle contraction), we think it is reasonable to assume that the sensor was generally measuring upper vaginal pressure and not pelvic muscle contraction strength, though it is possible that in some women it may have been. Additionally, our sample consisted of young, healthy and active women to decrease the risk of adverse events during exercise participation. The pressures we describe herein are not generalisable to older and less active women with chronic conditions. While we directly measured height and weight for body mass index (kg/m2) calculation, which has previously been shown to influence intra-abdominal pressure, assessment of body density and composition and other measures of physical fitness was beyond our scope, and in future research may explain some of the variability in pressure response to activity. Lastly, the time segments and specific repetitions for each of the activities in our protocol were relatively short for logistical purposes, which limit our ability to fully explore the meaningfulness of area under the curve and first moment of the area measures of intra-abdominal pressure.
Summary
The assessment of activity-induced intra-abdominal pressure and its potential link to pelvic floor disorders is not a topic routinely addressed in the exercise science literature. In order to explore this potential link, valid methods must be established to assess baseline and change in intra-abdominal pressure over time to determine whether certain activities increase risk for pelvic floor disorders. The descriptive information we provide may be especially relevant to educators and to those who provide exercise training for women in the context of fitness, clinical or research settings. Further research is needed to understand variability in intra-abdominal pressure amongst women before instituting exercise guidelines and activity restriction based on intra-abdominal pressure.
Footnotes
Conflict of Interest
No author of this manuscript has any conflicts of interest.
References
- 1.Al-Taher H, Sutherst JR, Richmond DH, Brown MC. Vaginal pressure as an index of intra-abdominal pressure during urodynamic evaluation. 1987:529–532. doi: 10.1111/j.1464-410x.1987.tb04870.x. [DOI] [PubMed] [Google Scholar]
- 2.Bø K, Finckenhagen HB. Is there any difference in measurement of pelvic floor muscle strength in supine and standing position? Acta Obstetricia et Gynecologica Scandinavica. 2003;82(12):1120–1124. doi: 10.1046/j.1600-0412.2003.00240.x. [DOI] [PubMed] [Google Scholar]
- 3.Bø K, Sherburn M. Evaluation of Female Pelvic-Floor Muscle Function and Strength. Physical Therapy. 2005;85(3):269–282. [PubMed] [Google Scholar]
- 4.Chiaffarino F, Chatenoud L, Dindelli M, Meschia M, Buonaguidi A, Amicarelli F, Parazzini F. Reproductive factors, family history, occupation and risk of urogenital prolapse. European Journal of Obstetrics & Gynecology and Reproductive Biology. 1999;82(1):63–67. doi: 10.1016/s0301-2115(98)00175-4. [DOI] [PubMed] [Google Scholar]
- 5.Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B. Normal intraabdominal pressure in healthy adults. Journal of Surgical Research. 2005;129(1):231–235. doi: 10.1016/j.jss.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 6.Coleman TJ, Hsu Y, Nygaard IE, Raynes J, Gordon K, Kumathe M, Hitchcock RW. Engineering in Medicine and Biology Society (EMBC), 2010 Annual International Conference of the IEEE. IEEE; 2010. A Gel filled intravaginal transducer for extended measurements of intra-abdominal pressure; pp. 1852–1855. [DOI] [PubMed] [Google Scholar]
- 7.Coleman TJ, Thomsen JC, Maass SD, Hsu Y, Nygaard IE, Hitchcock RW. Development of a wireless intra-vaginal transducer for monitoring intra-abdominal pressure in women. Biomedical Microdevices. 2012;14(1):347–355. doi: 10.1007/s10544-011-9611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Essendrop M, Hye-Knudsen CT, Skotte J, Hansen AF, Schibye B. Fast development of high intra-abdominal pressure when a trained participant is exposed to heavy, sudden trunk loads. Spine. 2004;29(1):94–99. doi: 10.1097/01.BRS.0000105528.37735.96. [DOI] [PubMed] [Google Scholar]
- 9.Gerten KA, Richter HE, Wheeler TL, Pair LS, Burgio KL, Redden DT, Hibner M. Intraabdominal pressure changes associated with lifting: implications for postoperative activity restrictions. American Journal of Obstetrics and Gynecology. 2008;198(3):306–e1. doi: 10.1016/j.ajog.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guttormson R, Tschirhart J, Boysen D, Martinson K. Are postoperative activity restrictions evidence-based? American Journal of Surgery. 2008;195(3):401–404. doi: 10.1016/j.amjsurg.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 11.Hagins M, Pietrek M, Sheikhzadeh A, Nordin M, Axen K. The effects of breath control on intra-abdominal pressure during lifting tasks. Spine. 2004;29(4):464–469. doi: 10.1097/01.brs.0000092368.90019.d8. [DOI] [PubMed] [Google Scholar]
- 12.Hamad N, Shaw J, Nygaard I, Coleman T, Hsu Y, Egger M, Hitchcock R. More complicated than it looks: the vagaries of calculating intra-abdominal pressure. Journal of Strength and Conditioning Research. 2013;27(11):3204–3215. doi: 10.1519/JSC.0b013e31828b8e4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the women’s health initiative: Gravity and gravidity. American Journal of Obstetrics and Gynecology. 2002;186(6):1160–1166. doi: 10.1067/mob.2002.123819. [DOI] [PubMed] [Google Scholar]
- 14.Hilde G, Stær-Jensen J, Siafarikas F, Engh ME, Brækken IH, Bø K. Impact of Childbirth and Mode of Delivery on Vaginal Resting Pressure Pelvic Floor Muscle Strength and Endurance. American Journal of Obstetrics and Gynecology. 2013;208(1):50.e.1–50.e.7. doi: 10.1016/j.ajog.2012.10.878. [DOI] [PubMed] [Google Scholar]
- 15.Hsu Y, Coleman TJ, Hitchcock RW, Heintz K, Shaw JM, Nygaard IE. Clinical evaluation of a wireless intra-vaginal pressure transducer. International Urogynecology Journal and Pelvic Floor Dysfunction. 2012:1–7. doi: 10.1007/s00192-012-1811-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.James ED, Niblett PG, MacNaughton JA, Shaldon C. The vagina as an alternative to the rectum in measuring abdominal pressure during urodynamic investigations. British Journal of Urology. 1987;60(3):212–216. doi: 10.1111/j.1464-410x.1987.tb05485.x. [DOI] [PubMed] [Google Scholar]
- 17.Johnson PJ, Rosenbluth EM, Nygaard IE, Parikh MK, Hitchcock RW. Development of a novel intra-vaginal transducer with improved dynamic response. Biomedical Microdevices. 2009;11(6):1213–1221. doi: 10.1007/s10544-009-9339-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jørgensen S, Hein H, Gyntelberg F. Heavy lifting at work and risk of genital prolapse and herniated lumbar disc in assistant nurses. Occupational Medicine. 1994;44(1):47–49. doi: 10.1093/occmed/44.1.47. [DOI] [PubMed] [Google Scholar]
- 19.Nygaard I, Hamad N, Shaw J. Activity restrictions after gynecologic surgery: is there evidence? International Urogynecology Journal. 2013;24(5):719–724. doi: 10.1007/s00192-012-2026-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas S, Reading J, Shephard RJ. Revision of the physical activity readiness questionnaire (PAR-Q) Canadian Journal of Sport Sciences. 1992;17(4):338–45. [PubMed] [Google Scholar]
- 21.Weir LF, Nygaard IE, Wilken J, Brandt D, Janz KF. Postoperative activity restrictions: any evidence? Obstetrics & Gynecology. 2006;107(1):305–309. doi: 10.1097/01.AOG.0000197069.57873.d6. [DOI] [PubMed] [Google Scholar]
- 22.Woodman PJ, Swift SE, O’Boyle AL, Valley MT, Bland DR, Kahn MA, Schaffer JI. Prevalence of severe pelvic organ prolapse in relation to job description and socioeconomic status: a multicenter cross-sectional study. International Urogynecology Journal. 2006;17(4):340–345. doi: 10.1007/s00192-005-0009-2. [DOI] [PubMed] [Google Scholar]