Abstract
SUMMARY
Prosthetic joint infection (PJI) is a tremendous burden for individual patients as well as the global health care industry. While a small minority of joint arthroplasties will become infected, appropriate recognition and management are critical to preserve or restore adequate function and prevent excess morbidity. In this review, we describe the reported risk factors for and clinical manifestations of PJI. We discuss the pathogenesis of PJI and the numerous microorganisms that can cause this devastating infection. The recently proposed consensus definitions of PJI and approaches to accurate diagnosis are reviewed in detail. An overview of the treatment and prevention of this challenging condition is provided.
INTRODUCTION
Joint replacement is a life-enhancing procedure for millions of people worldwide each year. Successful joint replacement provides pain relief, restores function and independence, and improves patient quality of life. While already a frequently performed procedure, the incidence of prosthesis implantation is expected to continue to rise. In the United States alone, there were 332,000 total hip and 719,000 total knee arthroplasties performed in 2010 (1). The numbers are projected to reach 572,000 and 3.48 million by 2030 for hips and knees, respectively (2). In Europe, a larger number of patients undergo primary hip arthroplasty than knee arthroplasty (3, 4). In addition to hip and knee replacement, shoulder, elbow, and ankle arthroplasties are now available. The total number of patients with existing arthroplasties in place continues to increase.
While the majority of joint arthroplasties provide pain-free function, a minority of patients will experience device failure and will require additional surgery at some point during the life of the device. Reasons for aseptic failure include loosening at the bone-cement interface, periprosthetic fracture, fracture of the prosthetic material itself, wear, implant malposition, dislocation-instability, or materials fatigue. Prosthetic joint infection (PJI), also referred to as periprosthetic infection, is defined as infection involving the joint prosthesis and adjacent tissue. Advances in the understanding of the epidemiology, diagnosis, management, and prevention of PJI over the last quarter century have led to improvement in outcomes for this challenging infection.
EPIDEMIOLOGY
Incidence
While the number of joint arthroplasties being implanted has risen and will continue to rise, the dynamics of the incidence of PJI are unclear. Several investigators have reported an increasing incidence of PJI in hip and knee arthroplasties. Using the Nationwide Inpatient Sample, the annual PJI incidence rate in the United States, expressed as a percentage of the total number of arthroplasties performed, increased from 1.99 to 2.18% for hip arthroplasties and from 2.05 to 2.18% for knee arthroplasties from 2001 to 2009 (5). Similarly, the Nordic Arthroplasty Register Association found an increase in the cumulative 5-year revision rate for infection in hip arthroplasties, rising from 0.46% during the period from 1995 to 1999 to 0.71% during 2005 to 2009 (6). However, a smaller population-based study from 1969 to 2007 using the Rochester Epidemiology Project to examine 75 PJIs in 7,367 joints did not find an increase over the duration of the study (7). The cumulative incidences of infection were 0.5, 0.8, and 1.4% at 1, 5, and 10 years, respectively, after primary hip or knee arthroplasty, with the overall unadjusted incidence rate, determined by using a standardized denominator, being 1.5 infections per 1,000 person-joint-years. The greatest risk period was the first 2 years, during which time 60 to 70% of infections occurred, a finding that has been observed in other studies (8, 9). The authors of the population-based study hypothesized that the stability in the incidence over the nearly 40-year time span was due to increased patient morbidity and risk factors for infection, counterbalanced by improvements in aseptic techniques, surgical skills, and infection prevention and control measures (7). While it is unclear if the incidence per person-joint-years is increasing or not, the absolute number of PJI cases will surely increase due to the increasing number of primary implantations being performed and the cumulative number of arthroplasties that remain in place.
The percentage of shoulder and elbow arthroplasties that become infected is based mainly on single-center studies and systematic reviews. Shoulder arthroplasty appears to carry an infection rate similar to those of hip and knee prostheses, with infection complicating 0.8 to 1.1% of primary arthroplasties (10, 11). In contrast, a systematic review of elbow arthroplasties found that 3.3% become infected (12). The reasons for the apparent higher infection rate may include the increased number of patients with rheumatoid arthritis receiving elbow arthroplasties (13) and the limited soft tissue envelope surrounding the elbow.
Economic Impact
The economic impact of PJI is significant. The overall cost to the American health care system to treat PJI was $566 million in 2009 alone, a number that is projected to reach $1.62 billion in 2020 (5). However, this figure is likely a gross underestimate, as this survey included only the estimated hospital cost, neglecting many other direct and indirect costs.
The cost of treating each individual PJI depends in part on the treatment strategy utilized. The cost of a single revision surgery for PJI is higher than the cost of revision for noninfectious reasons, with postulated reasons including prolonged procedure duration, increased blood loss, increased use of bone allograft, and increased complications (14). More complicated treatment strategies involving multiple individual surgeries further increase this cost compared to the cost of only a single surgery. For example, using a debridement-and-retention protocol, the cost to treat a single PJI is approximately 3-fold the cost of the primary implantation (15). In comparison, the average costs of one- and two-stage arthroplasty exchanges are 3.4 and 6 times higher, respectively, than the cost of primary implantation (16). Importantly, this does not include the indirect societal costs of the prolonged immobility of patients undergoing two-stage arthroplasty exchange. However, the cost of prolonged oral antimicrobials with single-surgery strategies is also not included in these studies, which may partially offset the difference.
Risk Factors
Risk factors for hip and knee infection.
Obesity has been associated with an increased risk of infection in many (9, 17–25) but not all (26) studies. A body mass index (BMI) threshold of 35 is most commonly used. Possible reasons for the increased risk with obesity include prolonged operative duration (27) and the presence of other comorbidities. However, obesity has remained an independent risk factor after adjustment for other covariates in several studies (18, 23). In contrast, a low BMI (<25) was associated with increased risk of PJI in another study, hypothesized to reflect nutritional reserve, immunosuppression, and underlying rheumatoid arthritis (28).
Diabetes mellitus has also been associated with an increased risk of PJI (18, 19, 21, 29). Interestingly, a recent study observed that perioperative hyperglycemia at the time of primary knee or hip arthroplasty was associated with an increased risk of subsequent PJI, even in patients without diabetes mellitus (30). This may be due to increased biofilm formation in the presence of elevated levels of glucose, as seen in in vitro models (31); impaired leukocyte function; or microvascular changes in patients with diabetes, which may influence wound healing and the development of superficial surgical site infections. However, not all studies have demonstrated a clear link between diabetes and PJI (17, 26), and some studies that have shown an increased risk grouped diabetes mellitus with other immunocompromising conditions (24).
Rheumatoid arthritis, exogenous immunosuppressive medications, and malignancy have been associated with an increased risk of PJI in various studies (9, 21, 22, 26, 32–36). Indeed, the infection rate for patients with rheumatoid arthritis is reportedly as high as 2.3% in the first year (33). Often, it is difficult to separate the relative contribution of the underlying illness, the accompanying comorbid conditions, and the therapy used. In one study, when rheumatoid arthritis, systemic immunosuppression, diabetes mellitus, chronic kidney disease, and malignancy were included in one category denoting global immunosuppression, the risk of PJI increased 2.2-fold (24). Biologic disease-modifying antirheumatic drugs (DMARDs) that inhibit tumor necrosis factor alpha or interleukin-6 (IL-6) increase the risk of surgical site infection after joint arthroplasty, but the limited number of patients studied does not permit a conclusion about their impact on PJI (37, 38). The American College of Rheumatology and the British Society for Rheumatology recommend withholding tumor necrosis factor alpha inhibitors around the time of arthroplasty surgery or revision (39, 40). In practice, the management of biologic and nonbiologic DMARDs during joint arthroplasty or PJI treatment is varied and should be individualized. One strategy is to withhold biologic DMARDs for one cycle before and resume them 1 or 2 weeks after joint arthroplasty surgery (41). While limited data suggest that it may be safe to continue nonbiologic DMARDs through joint arthroplasty (42, 43), methotrexate may be withheld when there is concern for wound healing problems. It may be impossible or impractical to eliminate the effects of leflunomide, given its long half-life. In patients undergoing treatment for PJI, weekly methotrexate and biologic DMARDs should be withheld for one or two therapy cycles prior to surgery. With most surgical strategies, nonbiologic DMARDs can be resumed once the surgical incision is healed. The decision regarding when to reinitiate biologic DMARDs depends on the surgical strategy used to treat PJI. With a two-stage arthroplasty exchange, biologic DMARDs should be held at least until the incision is healed following the second stage. With debridement with implant retention and one-stage arthroplasty exchange procedures, one approach is to reinitiate biologic DMARDs once the patient is on suppressive antimicrobial therapy (after the initial course of antimicrobials). For individual patients, the impact of altering DMARDs on the underlying rheumatic disease should be weighed against the impact on infection. The half-life of each agent, which can vary significantly, needs to be considered. It should also be acknowledged that patients with active rheumatologic disease may need to be “bridged” with corticosteroids while not receiving DMARDs, a practice that may negate, at least in part, any beneficial effect of withholding DMARDs. The appropriate perioperative management of these agents deserves further study.
The incidence of infection following arthroplasty revision surgery is higher than that following primary implantation (10, 24–26, 29, 35, 44, 45). Postulated reasons for this include prolonged operating time during the revision surgery or unrecognized infection at the time of revision, with subsequent recrudescence. The abnormal soft tissue envelope may also be a contributing factor.
Additional factors have been associated with an increased risk of hip or knee PJI in unadjusted models or in selected studies. Some of these factors include male gender (6, 8, 20, 36, 46, 47), smoking (21), antecedent bacteremia (during the previous year) (48), and antecedent septic arthritis of the index joint (26). The biological plausibility for some of these factors, such as gender, is uncertain. In contrast, the effect of smoking on tissue blood flow and oxygenation at the time of surgery is biologically plausible. A recently demonstrated association between a polymorphism in the gene encoding interleukin-1β and a higher risk of PJI suggests an interesting new area of research in the era of individualized medicine (49).
Perioperative factors may also impact the risk of PJI. Older data suggest that metal-to-metal hinged-knee prostheses are more frequently infected than metal-to-plastic prostheses (35). Large case-control and registry-based studies have found no difference between cemented and uncemented arthroplasties (26, 36), although cemented arthroplasties have the theoretical advantage of allowing local antimicrobial drug delivery for primary prevention of PJI. Several postoperative complications are associated with an increased risk of PJI, including hematoma, superficial surgical site infection, wound drainage, and wound dehiscence (9, 22, 24, 26, 48). Accordingly, prevention of surgical site infection through perioperative antimicrobial prophylaxis, meticulous surgical techniques, and infection control practices is critically important and is discussed in Prevention, below. A prolonged procedure duration is associated with an increased risk of PJI (8, 25, 26, 44, 46, 47), with a 9% increase in risk for each additional 15-min increment (18). This may be due to an increased time available for microbial contamination of the joint or may be a surrogate for other comorbidities, such as obesity, or both. Postoperative myocardial infarction and atrial fibrillation have been associated with a higher risk of infection as well, with a possible common mechanism of aggressive anticoagulation leading to subclinical hematoma formation (9). Allogeneic blood transfusion, even with leukocyte reduction, is associated with an increased risk of surgical site infection and PJI, while autologous transfusion does not appear to carry the same risk (9, 26, 50, 51). This has been hypothesized to be related to the immunomodulatory effects of transfusion. Perioperative infection at a distant site, including the urinary or respiratory tract, is associated with an increased risk of PJI (9, 21, 24), presumably due to transient bacteremia from the distant infection site during this high-risk time period. This is supported by an animal model showing that a lower level of bacteremia is necessary to initiate infection in the immediate postoperative period than 3 weeks later (52). However, asymptomatic pyuria or bacteriuria, in the absence of urinary tract infection, does not appear to be associated with the development of PJI (53–55). These data suggest that preoperative screening of asymptomatic patients by urinalysis would result in added expense, potential antimicrobial exposure, and a delay in surgery, without improving outcomes. Patients should instead be carefully evaluated for historical signs or symptoms suggestive of urinary tract infection at the preoperative visit and managed accordingly.
Risk factors for shoulder and elbow infection.
There are more limited data available on risk factors for PJI after shoulder and elbow arthroplasty. Presumably, the same systemic host risk factors that increase the risk of PJI in hip and knee arthroplasty, including rheumatoid arthritis, immunosuppression, and malignancy, would carry a risk in these arthroplasties. A large prospective study of 1,349 patients following shoulder arthroplasty found that only prior joint trauma was a risk factor for PJI, while a trend was seen for a higher BMI (10). However, there were only 14 cases of PJI in this study, and a limited number of risk factors was examined. Another small study found a higher risk of PJI in men (56). Age, gender, underlying joint disease, and type of arthroplasty were not associated with an increased risk of PJI in a study of 27 elbow arthroplasty infections occurring in 358 patients (13).
Composite risk scores.
Composite risk scores attempt to aggregate a number of factors into one, more easily applied variable. The National Nosocomial Infections Surveillance (NNIS) System surgical score includes the length of the surgical procedure, the American Society of Anesthesiologists (ASA) preoperative assessment score, and surgical wound classification for each procedure. In one large case-control study, the highest NNIS score was correlated with a 5-fold-increased odds of infection, a finding that persisted after multivariate analysis (26). An elevated ASA score alone, estimating the burden of systemic disease, has also been associated with an increased risk of infection (9, 17, 18, 24).
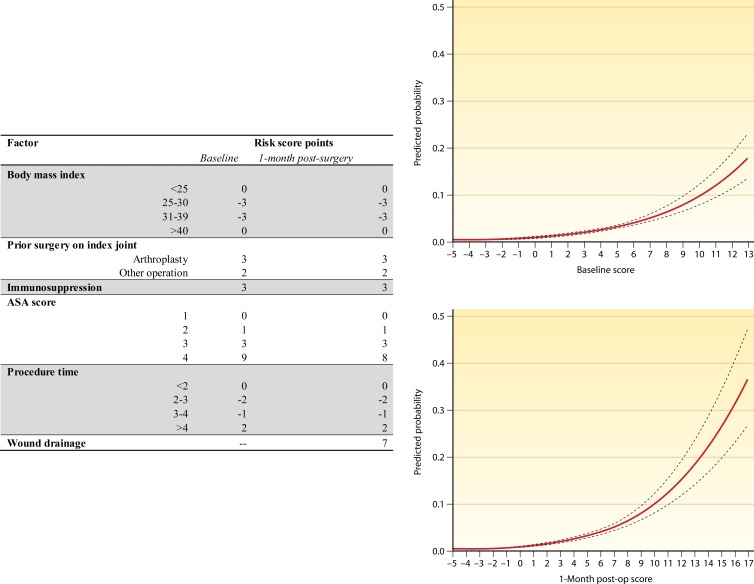
The Mayo PJI score, while not fully validated, is a numerical score to predict PJI based on assessment at the time of joint arthroplasty implantation or 1 month later (Fig. 1) (28). It was developed by using multivariable regression models from a large case-control study. The baseline score at the time of arthroplasty includes an abnormal BMI (either high or low), prior operation or arthroplasty on the joint, immunosuppression, ASA score, and procedure duration, with various point values being assigned to each component. It is noteworthy that the definition of immunosuppression used is broad, including malignancy, corticosteroid/immunosuppressive therapy, diabetes mellitus, and history of chronic kidney disease. The 1-month postoperative risk score includes wound drainage as well. These scores, although not fully validated for PJI, have the potential to help identify high-risk individuals at the time of surgery.
FIG 1.
The Mayo prosthetic joint infection risk score. The baseline or 1-month postsurgery score is calculated, and the predicted probability of PJI is determined by using the accompanying curve. (Reproduced from reference 28 with permission.)
CLINICAL MANIFESTATIONS
The clinical manifestations of PJI vary depending upon the virulence of the organism, the mode of initiation of infection, the host immune response, the soft tissue structure surrounding the joint, and the joint involved. Commonly reported signs or symptoms of PJI include pain, joint swelling or effusion, erythema or warmth around the joint, fever, drainage, or the presence of a sinus tract communicating with the arthroplasty (7, 57–59). The presence of a sinus tract is considered by most investigators to be definitive evidence of PJI, leading to its inclusion as definitive evidence of PJI in several consensus documents (60–62), as discussed in Diagnosis, below.
In general, pain seems to be the most frequently reported clinical manifestation, with case series reporting between 79 and 100% of patients with this finding (7, 58, 63–66). However, a study by Peel and colleagues found that pain was present in only 42% of patients, while drainage from the surgical wound was the most frequent finding in 72% of patients (57). This likely reflects the fact that 90% of the patients in this study were within 3 months of implantation, suggesting that the mechanism of infection initiation dictates some of the clinical presentation. This is corroborated by several studies that found that the presence of soft tissue damage, such as an open wound, sinus tract, or abscess, was more common in patients with contiguous or perioperatively acquired Staphylococcus aureus PJI than in those with hematogenously acquired S. aureus infection (59, 63). In contrast, systemic signs or symptoms such as fever or chills were significantly more common in patients with hematogenous PJI.
Clinical findings that raise or lower the pretest probability of PJI are helpful and may alter the diagnostic tests ordered, if a Bayesian approach to diagnosis is used. For example, a patient with multiple findings consistent with PJI, such as pain, effusion, periarticular warmth or erythema, and fever, may be considered to have a pretest probability of PJI exceeding 20%. The diagnostic algorithm for this patient may be markedly different from those for patients presenting with pain as the only potential manifestation of infection, where the pretest probability may be closer to the population-based risk of 0.5 to 1.5% (7). Unfortunately, there have been no large, well-performed studies comparing the abilities of different clinical findings to predict PJI. Presumably, the vast majority of patients who present with PJI or aseptic failure will have pain, so this is not likely a useful discriminating symptom. The presence of swelling and erythema around a knee arthroplasty is found in a significantly higher percentage of patients with infection than in those undergoing revision for aseptic reasons (58), but the diagnostic odds associated with this finding are unknown. It is therefore up to the evaluating clinician to estimate the pretest probability of PJI and decide upon the most appropriate diagnostic testing strategy for each individual, based on the patient's constellation of clinical symptoms and risk factors for infection. The PJI risk score mentioned above may assist in the estimation of the pretest probability of PJI (28).
Classification Schemes
There are several useful classification schemes for PJI. The first is simply based on the time to infection, classified as early, delayed, or late onset. Early-onset PJI occurs <3 months after the last surgery. These infections are most commonly initiated at the time of operation, through intraoperative contamination, as discussed below, and are caused by relatively virulent microorganisms. Delayed-onset PJI occurs after 3 months but before 12 or 24 months. Different authors have used different time points to differentiate between delayed- and late-onset PJIs. However, regardless of the cutoff used, the common theme is that these infections are also typically acquired at the time of surgery but are caused by less virulent microorganisms such that the overt presentation of infection does not occur within the first 3 months. Late-onset PJI, occurring >12 to 24 months after surgery, is frequently due to hematogenous infection but may also be due to extremely indolent infection initiated at the time of surgery.
Another classification scheme was popularized by Tsukayama in the 1990s (67, 68). This scheme divides PJIs into four categories, based partly on the time since operation and also on the presumed mode of infection. The first category is positive intraoperative cultures, in which a patient undergoing revision for presumed aseptic failure is found to have a positive intraoperative culture. Some patients falling into this category do not truly have PJI. For example, in one paper using this classification scheme, only 1 out of 31 patients with this type of infection had acute inflammation determined by histopathology (67). Early postoperative infection that occurs within the first month after surgery is the second category. This is similar to early-onset PJI in the first classification scheme. The third category is late chronic PJI, which occurs >1 month after the index operation and is typically associated with an indolent course. This category encompasses many of the patients in both the delayed- and late-onset PJI categories in the other classification scheme. The final category of infection is acute hematogenous infection. This classification scheme is useful in determining medical and surgical management. Both early postoperative infection and acute hematogenous infection may be amenable to a debridement and implant retention procedure, while two-stage arthroplasty exchange would be preferable for late chronic infection. Issues regarding the selection of a medical-surgical treatment strategy are discussed in Treatment, below.
Finally, McPherson and colleagues proposed a staging system for PJI that categorizes not only the type of infection but also the host (69, 70), with some similarity to the Cierny-Mader staging system for osteomyelitis (71). This system includes three of the four types of infection in the system of Tsukayama et al. (67), early postoperative infection, hematogenous infection, and late chronic infection, which are graded as type I, II, or III. The systemic host status is graded as A (uncompromised), B (compromised), or C (significant compromise), corresponding to a number of factors, including the presence of neutropenia, low CD4 T-cell count, or age of >80 years. Finally, the local extremity is graded as 1 (uncompromised), 2 (compromised), or 3 (significantly compromised), corresponding to the presence of local chronic active infection, soft tissue loss, or the presence of a fistula or subcutaneous abscess, among other factors. This system allows more individualized treatment decisions and prognostic information. Among patients undergoing resection for infected hip arthroplasty, there was a positive correlation between the host grade and likelihood of reimplantation and a negative correlation between the host grade and amputation or death (70). However, a subsequent large study of knee arthroplasty infection did not find a correlation between this staging system and the likelihood of infection recurrence (72).
PATHOGENESIS
Initiation of Infection
The majority of PJIs occurring within 1 year of surgery are initiated through the introduction of microorganisms at the time of surgery. This can occur through either direct contact or aerosolized contamination of the prosthesis or periprosthetic tissue. Once in contact with the surface of the implant, microorganisms colonize the surface of the implant. A significant factor in this process is the low inoculum of microorganisms needed to establish infection in the presence of the prosthetic material. For example, <102 CFU of S. aureus are necessary to establish infection if inoculated at the time of a hip hemiarthroplasty in a rabbit model, compared with 104 CFU when no implant is placed (52). This difference is explained by biofilm formation in the case of the foreign body (see “Role of Biofilm,” below).
Contiguous spread of infection from an adjacent site is the second mechanism by which infection can be initiated. In the early postoperative time period, superficial surgical site infection can progress to involve the prosthesis, due to incompletely healed superficial and deep fascial planes. However, contiguous spread may also occur later if the normal tissue plane is again disrupted through trauma or surgery at an adjacent location. Erosion of the implant through an impaired soft tissue envelope may also predispose patients to a late onset of contiguous infection. This may occur in patients with elbow prostheses and underlying rheumatoid arthritis who may have an adjacent rheumatoid nodule or thin skin due to chronic corticosteroid use.
Finally, the prosthesis remains at risk of hematogenous seeding throughout the life of the arthroplasty. Overall, PJI resulting from a remote site of infection is rare. In 551 remote infections occurring in 6,101 hip and knee arthroplasties, only 7 documented hematogenous PJIs were diagnosed (25). Arthroplasty infection occurred in 5 (6%) of the 81 patients with documented bacteremia. However, some pathogens present a significantly higher risk than others. S. aureus is a frequently isolated pathogen in cases of hematogenous PJI, and several small studies have suggested that S. aureus bacteremia is associated with a 30 to 40% risk of hematogenous seeding of in situ arthroplasties (73–75). This risk, compared with the 3 to 10% risk of infection of native joints during S. aureus bacteremia, highlights the importance of prosthetic material in hematogenous PJI (76–78). Coagulase-negative staphylococci, Streptococcus species, Enterococcus species, and aerobic Gram-negative bacilli also play an important role in this setting (9, 79–81). In one series, Streptococcus species were found with the same frequency as S. aureus (82). In the majority of hematogenous infections, bacteremia and symptoms of PJI occur almost simultaneously. However, for some less commonly encountered microorganisms, there may be a prolonged time interval between bloodstream infection and PJI-associated symptoms (83). The timing of bacteremia is important, with a lower inoculum of bacteria being required for infection at the time of prosthesis implantation than 3 weeks later, as demonstrated in an animal model (52). This may be related to increased blood flow in the immediate postoperative period.
Role of Biofilm
Biofilms are complex communities of microorganisms embedded in an extracellular matrix that forms on surfaces. They may be monomicrobial or polymicrobial, but even monomicrobial biofilms, especially those that are long-standing, may consist of subpopulations of the same organism with different phenotypic and/or genotypic characteristics. Some organism types grow together better than others in biofilms, which may impact the species found in polymicrobial biofilms. Mixed-population biofilms, whether monomicrobial or polymicrobial, may not be made up of equal proportions of their components, and their subpopulations may be differentially affected by antimicrobial agents and/or the host immune system, rendering them challenging to detect in the clinical laboratory. Besides growing on the surface of foreign bodies, some associated organisms have the ability to persist intracellularly, although they are not considered “traditional” intracellular pathogens. The biofilm growth state is not static but rather consists of “stages,” including attachment of microbial cells to a surface, initial growth on the surface, maturation of the biofilm, and, ultimately, detachment. Mature biofilms have a multicellular nonhomogeneous structure in which their component microbial cells may communicate with one another (e.g., through quorum sensing), and different subpopulations may have different functions, together supporting the whole biofilm and rendering biofilms somewhat analogous to a multicellular organism. While the biofilm phenotype evolved long before the advent of medical devices and in response to a need to grow on surfaces other than medical devices, the ability to form biofilms equips certain bacteria and fungi with the capacity to cause medical device-associated infections, including PJI. Biofilm formation also explains why some normal flora organisms traditionally considered “harmless” become pathogens when they grow in the presence of foreign bodies.
The extracellular matrix component of biofilms is composed of polysaccharides, proteins, and/or extracellular DNA, and its composition and amount vary between and even within organism types. In the biofilm state, bacteria are protected from antimicrobials and the host immune system (84), making treatment of infection difficult without a biofilm-directed treatment strategy, which today mandates surgical intervention, in many cases including prosthesis removal, to achieve a cure. The reduced antimicrobial susceptibility of bacteria in biofilms is related to their low growth rate, the presence of resistant bacterial subpopulations (so-called “persisters”), and a microenvironment within the biofilm that impairs antimicrobial activity (85, 86). Select antimicrobial agents such as rifampin may have activity against certain types of biofilms (e.g., staphylococcal biofilms).
While biofilms have long been implicated in PJI, viable bacteria living within biofilms have only recently been visualized ex vivo on removed prosthetic components (87). Given the importance of biofilms in the pathogenesis of PJI, several investigators have hypothesized that the presence of key gene loci involved in biofilm formation may discriminate between pathogens and contaminants when organisms are isolated from the site of a prosthetic joint. In several species of staphylococci, for example, polysaccharide intercellular adhesion, encoded by the ica genes, contributes to biofilm extracellular matrix. Despite the findings of some investigators that the ica genes in staphylococci are associated with PJI (88), several other investigators have shown that ica genes are not required for PJI (89, 90). Complicating this situation, definitive evidence correlating luxuriant in vitro biofilm formation for a particular organism type with its propensity to cause PJI is lacking (and there may be variability in biofilm growth between in vitro biofilm assays). Arguably, the formation of a nonluxuriant biofilm may be advantageous to an organism growing on the surface of an implant, enabling its persistence without robustly triggering the host immune system.
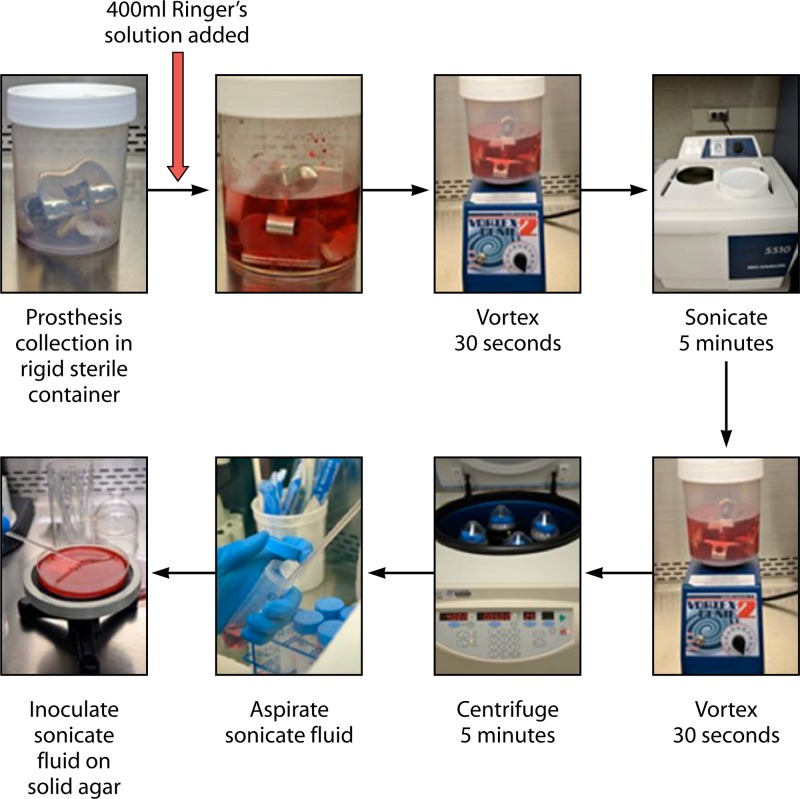
Beyond implications of biofilm formation for PJI pathogenesis and treatment, biofilm formation impacts the diagnosis of PJI. In particular, especially in delayed- and late-onset PJIs, the implicated organisms are concentrated on the surface of the prosthesis, limiting the sensitivity of periprosthetic tissue and fluid cultures. One strategy to overcome this limitation is to sample the prosthesis surface itself, for example, using device vortexing-sonication.
Propagation of Infection
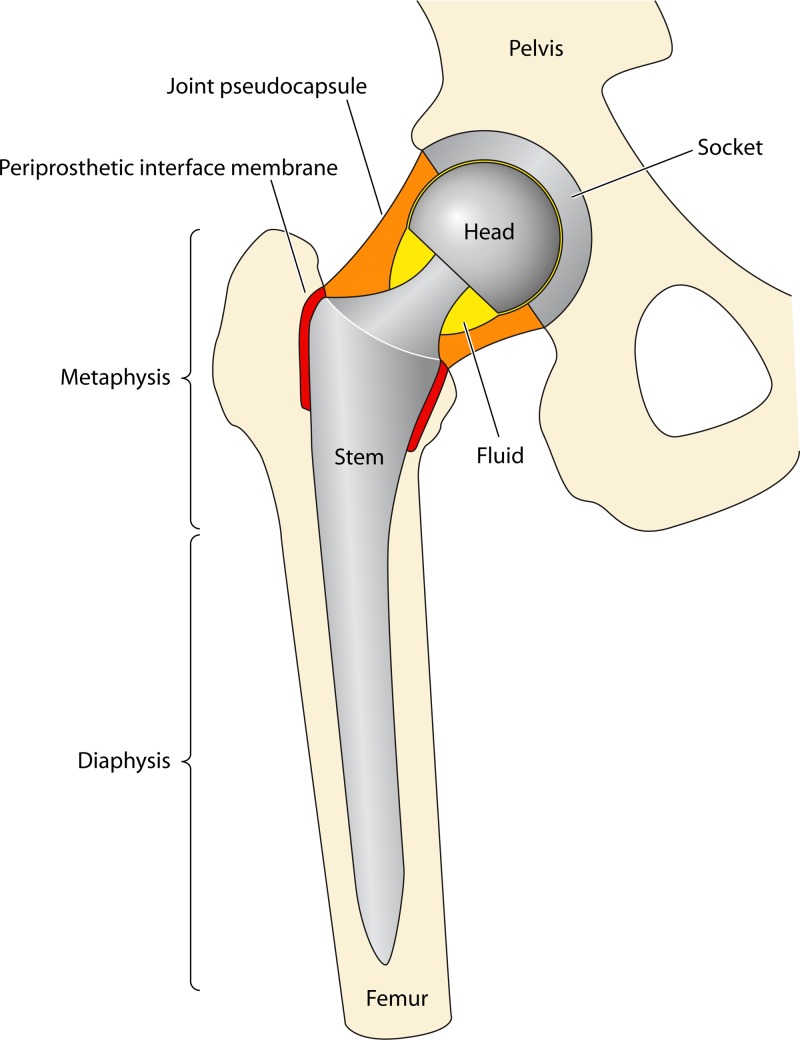
Animal models are useful to understand the progression of infection once it has been established. One such model is a rabbit model of knee arthroplasty infection, in which a high inoculum of S. aureus is introduced into the joint space shortly after implantation (91). This is conceptually analogous to intraoperative contamination of the prosthesis, although the inoculum is much higher in the animal model. Initially, infection is confined to the joint space, where histology demonstrates large granulomas with neutrophils and abscess formation. The infection then spreads to the adjacent metaphysis, with only the upper one-third of the metaphysis being involved at 3 weeks. If allowed to continue, infection ultimately goes on to involve the entire metaphysis of the periprosthetic bone as well as the adjacent portion of the diaphysis. It is unclear whether this process is the same for hematogenous PJI. Hematogenous long bone osteomyelitis is thought to initiate at the metaphysis (92). It is therefore possible that hematogenous PJI begins in the metaphysis and subsequently progresses to involve the arthroplasty. It is not clear if this is the mechanism of infection or if this theoretical difference would have any impact on the diagnosis and treatment of PJI. Figure 2 demonstrates the location of a hip prosthesis in relation to the anatomical structures discussed above. The periprosthetic interface membrane and joint pseudocapsule are discussed in “Periprosthetic Tissue,” below.
FIG 2.
Schematic showing a total hip arthroplasty in place, with relevant structures highlighted.
MICROBIOLOGY
Relative Frequency of Microorganisms
In order to make appropriate empirical antimicrobial decisions before culture results are known, the common microbiological causes of PJI reported in the literature should be examined. The microbiological results of 14 large studies including >2,400 patients with hip or knee arthroplasty infection are collectively presented in Table 1 (24, 26, 57, 79, 93–102). These studies represent a spectrum of surgical strategies, countries, and time points. Gram-positive cocci are involved in the majority of hip and knee PJIs in all of the studies examined. This is driven largely by infection with S. aureus and coagulase-negative staphylococci, which contribute to between 50 and 60% of PJIs, while streptococci and enterococci together account for only approximately 10% of cases. The proportions of PJIs caused by S. aureus and coagulase-negative Staphylococcus species appear to be relatively equal when these studies are evaluated in aggregate but vary in certain situations, as detailed below. Aerobic Gram-negative bacilli are involved in <10% of cases of knee and hip PJI. This has implications for the perioperative antimicrobial management of these patients. The proportion of culture-negative infections is higher than that reported in previous reviews of the literature, in which 6% of hip and knee PJIs were culture negative (57). In the studies included, the percentage varied from 5 to 34% (96, 101). This wide variation is likely related to a number of factors that differed between the studies, including the use of preoperative antimicrobials, the definition of a positive culture result, whether a positive culture represented contamination, and the number and type of specimens obtained for microbiological diagnosis.
TABLE 1.
Common causes of prosthetic joint infection
| Infection | % of patients with prosthetic joint infection |
|||||
|---|---|---|---|---|---|---|
| Hip and knee |
Hipc | Kneec | Shoulderd | Elbowe | ||
| All time periodsa | Early infectionb | |||||
| Staphylococcus aureus | 27 | 38 | 13 | 23 | 18 | 42 |
| Coagulase-negative Staphylococcus | 27 | 22 | 30 | 23 | 41 | 41 |
| Streptococcus species | 8 | 4 | 6 | 6 | 4 | 4 |
| Enterococcus species | 3 | 10 | 2 | 2 | 3 | 0 |
| Aerobic Gram-negative bacilli | 9 | 24 | 7 | 5 | 10 | 7 |
| Anaerobic bacteria | 4 | 3 | 9 | 5 | ||
| Propionibacterium acnes | 24 | 1 | ||||
| Other anaerobes | 3 | 0 | ||||
| Culture negative | 14 | 10 | 7 | 11 | 15 | 5 |
| Polymicrobial | 15 | 31 | 14 | 12 | 16 | 3 |
| Other | 3 | |||||
Data from 1,979 hip and 1,427 knee PJIs from the Mayo Clinic Prosthetic Joint Infection Database (E. F. Berbari, personal communication).
Identification of the likely cause of early-onset PJI is particularly important given that these infections are more frequently treated with a debridement procedure where the implant is not removed. In 637 patients with early-onset hip or knee arthroplasty infection (defined as infection onset less than 1 or 3 months after surgery, depending on the study), there were several notable differences in this group compared to patients from all time periods (Table 1) (67, 97, 98, 103–107). S. aureus and aerobic Gram-negative bacilli together contributed to 60% of the early-onset infections. The increased virulence of these microorganisms likely leads to the onset of symptoms within the first several months. However, coagulase-negative staphylococci remain important pathogens in this setting. The number of patients with polymicrobial infection is also higher in this time period, possibly reflecting inoculation with multiple microorganisms at the time of surgery or contiguous spread from the surgical incision. In contrast, delayed-onset PJI (from 3 months to 1 to 2 years after implantation) typically involves inoculation with less virulent microorganisms at the time of surgery, such that coagulase-negative staphylococci and enterococci are more common, while it is less typical for aerobic Gram-negative bacilli to be isolated (108). Late-onset PJI (>1 to 2 years after implantation) are often due to hematogenous seeding from infection at another site; S. aureus predominates in this setting, as discussed above (73, 74, 109). Less commonly, late-onset PJI may be due to relatively avirulent microorganisms implanted at the time of surgery.
There are certain notable differences with regard to the joint that is infected, as shown in Table 1. Hip and knee arthroplasties comprise the largest numbers of PJIs. A large single-institution database from the Mayo Clinic suggests that patients with hip arthroplasty have a lower frequency of S. aureus than coagulase-negative staphylococcal infection, compared to those with infected knee arthroplasties, where the two types of staphylococci are relatively equal (E. F. Berbari, personal communication). Anaerobic bacteria, including Propionibacterium acnes, are more frequently identified in hip than in knee arthroplasty infections. However, shoulder arthroplasty infection is much more commonly caused by P. acnes than PJIs of other joint types (56, 110–116). Coagulase-negative staphylococci are more frequently identified than S. aureus in shoulder infection as well. S. aureus and coagulase-negative staphylococci cause over three-quarters of elbow arthroplasty infections (13, 117–120).
Causative Microorganisms
S. aureus.
S. aureus is an important pathogen as a result of its virulence and frequency. In addition to being a leading cause of PJI, it is one of the common causes of serious invasive infections, including nosocomial and health care-associated bloodstream infections, which can subsequently lead to PJI (121, 122). Indwelling prosthetic devices (123), injection drug use, receipt of hemodialysis, rheumatoid arthritis, diabetes, and S. aureus nasal colonization are all associated with an increased risk of invasive infection (124). Accordingly, patients with S. aureus PJI frequently have multiple medical comorbidities (59), with diabetes being present in 30 to 40% (125) and rheumatoid arthritis being present in 10 to 20% (63, 126) of patients.
In patients treated with a variety of surgical techniques, fever was present in only a small minority of patients (125), while fever is more common in patients with acute infection treated with debridement with prosthesis retention (63). Concomitant bacteremia occurs in 10 to 60% of cases of PJI (59, 63, 125–128), with higher rates in patients treated with debridement with prosthesis retention (127) than in patients with resection arthroplasty (128). Infection occurs at all time periods after implantation, but delayed-onset infection appears to occur less often than infection in early or late time periods (125). The initial presentation is typically an acute infection, but a number of authors report symptoms lasting up to several years, likely secondary to prior attempts at treatment (128, 129). Additionally, one small case series suggested that small-colony-variant S. aureus may cause a more indolent presentation following prior attempts at treatment (130).
Coagulase-negative Staphylococcus species.
A number of species comprise the group of microorganisms referred to as the coagulase-negative staphylococci. Many are ubiquitous members of the human microbiome found on the skin. Because of the historical challenges in identifying the specific species within this group, much of the PJI literature does not refer to individual species, and therefore, the relative pathogenicity of these microorganisms is unclear.
Staphylococcus epidermidis is the most frequently identified member of this group (131). This species causes PJI primarily through its ability to adhere to prosthetic materials and produce biofilm, although other more typical virulence factors have been identified more recently (132, 133). Other species that have been reported to cause PJI include Staphylococcus simulans (134), Staphylococcus caprae (135), and Staphylococcus lugdunensis (136). With the exception of S. lugdunensis, oxacillin resistance is found in the majority of PJI-associated coagulase-negative staphylococci (137).
Coagulase-negative Staphylococcus species can cause PJI at any time after an arthroplasty has been placed. This group of organisms is the second most common cause of early-onset PJI, in which the presentation typically includes wound drainage, local skin changes, and pain. They are also one of the most frequent causes of delayed- or late-onset PJI, where pain may be the only manifestation. Whether different species within this group have different clinical manifestations or risk factors remains to be determined.
S. lugdunensis.
One coagulase-negative Staphylococcus species, S. lugdunensis, is unique from other members of this group. This organism produces a bound coagulase (rather than the free coagulase found in S. aureus) and may be misidentified by the use of latex agglutination testing (138) and some commercial systems (139). This organism exhibits positive pyrrolidonyl arylamidase (PYR) and ornithine decarboxylase reactions (138) and is easily identified by using matrix-assisted laser desorption ionization–time of flight mass spectroscopy (131). S. lugdunensis is unique in its antimicrobial susceptibility profile, with susceptibility to penicillin being found in up to three-quarters of isolates due to the absence of β-lactamase production (138). This is in contrast to other Staphylococcus species, where β-lactamase production is common (137).
S. lugdunensis is capable of causing severe systemic and local infections similar to those caused by S. aureus (136, 140, 141). The largest case series of PJI due to S. lugdunensis to date included 28 episodes of PJI in 22 patients over a 9-year period at the Mayo Clinic (142). Nearly one-third of the patients had a urogenital abnormality, which is compatible with the high frequency of inguinal colonization reported for this organism (143). Arthroplasty infection with S. lugdunensis frequently presents with acute onset of pain and swelling, although the small number of reported cases limits this generalization (136, 144).
Streptococcus species.
Streptococcus is a diverse genus that has a prominent role in human disease but causes <10% of joint arthroplasty infections. A number of beta-hemolytic Streptococcus species cause PJI, including Lancefield groups A (145–147), B (148–153), C (154–156), and G (145, 157, 158). Streptococcus gallolyticus subsp. gallolyticus (formerly Streptococcus bovis biotype I) may cause PJI and is also associated with underlying colorectal neoplasia (159–163); an evaluation for occult colorectal malignancy or polyps should occur when this organism is identified. Viridans group streptococci are uncommon causes of PJI (145, 158), even after invasive procedures, such as upper endoscopy, that might be expected to lead to infection with these microorganisms (164). Streptococcus pneumoniae is also a rare cause of PJI (83, 165–167).
Several small case series suggest that group B and G streptococci may be the most common streptococci to cause PJI (145, 158). These infections are typically acute in nature, with at least half of patients presenting with fever and systemic symptoms (152, 158). A similar presentation may be expected with all of the beta-hemolytic streptococci. Group B streptococci most frequently cause delayed- or late-onset PJI, and most patients have one or more comorbidities, including obesity, malignancy, or diabetes mellitus (152). The infection is presumed to be hematogenous in a majority of patients, with the genitourinary tract, gastrointestinal (GI) tract, and skin being the most frequent sources (148, 149). Accordingly, up to 50% of patients may be bacteremic at the time of PJI symptom onset (158). Patients with PJI caused by group G streptococci often have remote sites of infection, such as cellulitis (158). The majority of patients with bacteremia due to this organism are older men with skin infection (168), findings also seen in one small series of patients with PJI due to this organism (158).
Enterococcus species.
While rare causes of PJI overall, enterococci are found in up to 12 to 15% of patients with early-onset PJI, often as part of polymicrobial infections (103, 104). There has been one large study of 50 episodes of monomicrobial enterococcal PJI occurring over a 30-year period (169). The source of the infecting organism was not described but was presumably hematogenous seeding from the gastrointestinal or urinary tract. In contrast to early-onset enterococcal PJI, which occurs as part of a polymicrobial infection, the majority of these patients presented late after arthroplasty implantation, with a prolonged duration of symptoms, compatible with the less virulent nature of enterococci. Fever was less common than joint pain or the presence of a sinus tract, and only one of these patients had concomitant bacteremia. The species was not reported, so the relative importance of different species of Enterococcus is unknown.
Aerobic Gram-negative bacilli.
Much like enterococci, aerobic Gram-negative bacilli are more common in early-onset PJI, where they are found in up to 45% of infections in some studies (103, 104). They also play a prominent role in polymicrobial infections (170) and may be a cause of hematogenous infection, which tends to be monomicrobial (80). In most studies, the most commonly isolated aerobic Gram-negative bacillus is Escherichia coli (171–174), although in one large study, it was Pseudomonas aeruginosa (175). Non-E. coli Enterobacteriaceae make up the majority of the remaining pathogens. Due to the virulence of many aerobic Gram-negative bacilli, an acute presentation is commonly observed. Patients with PJI caused by aerobic Gram-negative bacilli tend to be older than those with PJI caused by Gram-positive bacteria (175). Additionally, one small study reported that aerobic Gram-negative bacilli were more likely to occur in a hip rather than a knee prosthesis (171), possibly due to the proximity of the hip to the gastrointestinal tract. A subsequent study suggested that a hip hemiarthroplasty is at higher risk than a total hip arthroplasty, but this may reflect the increased proportion of early-onset PJIs in the hemiarthroplasty group (176).
P. acnes.
P. acnes is a relatively low-virulence, anaerobic, Gram-positive bacillus normally found on the human skin and sebaceous glands. This microorganism is typically inoculated at the time of surgery. As mentioned above, P. acnes more frequently causes infection of shoulder arthroplasties than of other joints, a finding presumably related to the proximity to the axilla. This is a challenging organism in clinical practice, given that it may be more difficult to isolate and may have fewer associated clinical manifestations of infection than other bacteria. For example, many patients with P. acnes PJI have normal preoperative erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) values, even when rigorous nonmicrobiological findings suggestive of infection are present (56). Additionally, acute inflammation is not uniformly present (177). As discussed in Diagnosis, below, with this organism (and others), a positive culture may represent true infection or contamination, highlighting the importance of proper specimen collection for culture (including multiple tissue cultures and/or semiquantitative implant cultures). For these reasons, interpretation of the literature on P. acnes PJI is somewhat challenging, given that a standardized definition of overall PJI has only recently been proposed and given that it is unknown how well it applies to P. acnes PJI.
Patients with infection due to P. acnes typically have a very indolent clinical course, with pain often being the only manifestation of infection. Other findings, such as a sinus tract, may be present as well, but this is the exception rather than the rule (56, 178). Male gender is more common in patients with P. acnes PJI (56, 179–181). Interestingly, in one outbreak investigation, patients undergoing shoulder surgery were more likely to develop P. acnes infection if they underwent the first procedure of the day (180); the reason for this finding is unclear.
Other anaerobic bacteria.
Other anaerobic bacteria reported in PJIs include Clostridium species, Bacteroides fragilis, Peptostreptococcus species, and Actinomyces species. The most frequent setting in which anaerobic bacteria (except P. acnes) cause PJI is as part of a polymicrobial infection, with anaerobes being present in 12% of polymicrobial infections in one series (170). Clostridium PJI typically occurs in patients with underlying gastrointestinal disease. Clostridium difficile, typically thought of as being localized to the intestine, has been identified in hip (182), knee (183), and shoulder (184) PJIs. Similar to S. gallolyticus subsp. gallolyticus, there is an association between Clostridium septicum PJI and intestinal malignancy (185, 186). Clostridium perfringens PJI has been identified following acute cholecystitis (187). In each of these cases, the presumed mechanism of infection was hematogenous seeding from the GI tract. In contrast, direct communication between a perforated colonic diverticulum and a hip arthroplasty has been reported with Bacteroides fragilis (188). Peptostreptococcus species are associated with periodontal disease and have been anecdotally implicated in dental work-associated PJI (189, 190). However, a large rigorous case-control study failed to demonstrate an overall association between dental procedures and PJI (24).
In contrast to other anaerobic infections, which may exist as part of a polymicrobial infection (170, 186), infections due to Actinomyces species are nearly uniformly monomicrobial (191–195). The clinical presentation is typically indolent, as in other Actinomyces infections. Dental work (195, 196) and intravenous (i.v.) drug use (193) are reported associations but are not necessarily present in all cases.
Polymicrobial infection.
Polymicrobial PJI occurs in up to 35% of early-onset infections, compared to <20% of infections occurring at any time point after arthroplasty implantation (26, 97, 103, 104). One series found that 56% of all polymicrobial PJIs occurred within the first 90 days of implantation, compared to only 29% of monomicrobial PJIs (170). Enterococcus species, S. aureus, and aerobic Gram-negative bacilli, including P. aeruginosa, are the most frequently isolated bacteria, each being present in more than one-quarter of infections (57, 170).
Rheumatoid arthritis (57), a higher comorbidity index (174), age of >65 years, and wound drainage and dehiscence after surgery (170) are more common in polymicrobial than in monomicrobial infections. Accordingly, a clinical presentation of infection in the early postoperative period in an older patient with surgical wound dehiscence should prompt consideration of a polymicrobial infection.
Other bacteria.
Case reports and a small case series have described a myriad of other less common bacterial causes of PJI. Several Corynebacterium species have been implicated as a cause of PJI (197–200). Certain species, such as Corynebacterium jeikeium, are notable for resistance to multiple antibiotics (201, 202). While classically associated with meningoencephalitis in older and immunocompromised individuals, Listeria monocytogenes PJI presents predominantly as a subacute infection and was associated with central nervous system infection in only 1 of 34 patients in a large case series (203).
Zoonotic organisms cause PJI infrequently and typically occur in patients with a geographic or exposure risk for the pathogen. While infection with Brucella species is one of the most common zoonoses worldwide (204) and can cause native osteoarticular infection, it is an uncommon cause of PJI, typically occurring in areas of high endemicity (205–208). Pasteurella multocida PJI is an acute infection with regional lymphadenopathy (209) that typically occurs shortly after a scratch, lick, or bite from a cat or dog on the ipsilateral limb distal to the arthroplasty (210–221). P. multocida infection without a compatible exposure history is uncommon but has been reported (222). An appropriate epidemiologic and exposure history was also absent in the only reported case of PJI due to Coxiella burnetii (223).
Two recent exhaustive reviews of unusual causes of PJI provide a good reference for those seeking further description (224, 225).
Mycobacteria.
The Mycobacterium tuberculosis complex remains a leading cause of morbidity and mortality worldwide, with bone and joint infection occurring in >10% of extrapulmonary M. tuberculosis complex cases in developed countries (226). In developed countries, the M. tuberculosis complex is a distinctly uncommon cause of PJI, accounting for only 0.3% of cases in one series (227). However, patients for whom joint arthroplasty is performed in a joint with prior M. tuberculosis complex septic arthritis have up to a 31% risk of subsequent M. tuberculosis complex PJI (228). PJI can also occur in patients without a history of active or latent tuberculosis (229, 230), typically involving either the hip or knee, with one case series suggesting that the hip is more commonly involved (227). Two clinical presentations have been described (230). In the first presentation, M. tuberculosis complex infection of the native joint is discovered surreptitiously at the time of the initial arthroplasty (231). These patients can be treated with standard antituberculous combination chemotherapy, with prosthesis salvage being reported (232). The second presentation is typically one of indolent infection occurring several months or more after arthroplasty placement, in which a sinus tract is often present. Symptoms classically associated with other M. tuberculosis complex infections, such as fever, anorexia, or weight loss, are uncommon (227). These patients frequently require resection of the prosthesis in combination with antimycobacterial therapy to achieve cure. Diagnosis may be delayed, particularly if there is no history of active or latent tuberculosis (229).
Nontuberculous mycobacteria rarely cause PJI. In a single institutional series spanning 38 years, only eight patients with PJI caused by rapidly growing mycobacteria were identified (233). Swelling and joint pain were present in seven of the eight patients, while fever was present in only three patients. The knee was the most common site of infection, and seven of the eight patients were immunocompetent. In contrast, PJI due to the Mycobacterium avium complex has been reported primarily for immunocompromised patients with HIV/AIDS (234) or solid organ transplants (235–237). The mechanism of infection is presumably hematogenous in M. avium complex PJI (234).
Fungi.
Fewer than 1% of PJI cases are caused by fungi. Among these, Candida species are found in at least 80% of cases (238, 239). Concomitant bacterial infection occurs in 15 to 20% of cases. The individual Candida species may be related to geographic differences, with Candida albicans causing the majority of infections in one multicenter American study (239) and Candida parapsilosis being the most frequently isolated species in a single-center experience from Southeast Asia (238). Aspergillus species (239–242), dimorphic fungi (243, 244), pigmented yeast (239), dematiaceous fungi (239), and other filamentous fungi (245) have all been rarely reported in PJIs.
The majority of fungal PJIs occur after revision arthroplasty (239, 246). Prior bacterial PJI, preceding antimicrobial use, immunosuppressive therapy, and diabetes have been suggested as risk factors (246, 247). However, the relative importance of these risk factors compared to those identified in patients with bacterial PJI is unknown. Interestingly, several of the reported cases of Aspergillus PJI have occurred in immunocompetent individuals, unlike pulmonary infection, which occurs more often in immunocompromised subjects (241, 242). Fungal PJI typically presents with subacute or chronic pain and joint swelling, with fever being uncommon (239, 246, 247).
Culture-negative infection.
Patients with culture-negative PJI have nonmicrobiological evidence of infection, such as periprosthetic purulence, acute inflammation determined by histopathology, or a sinus tract communicating with the joint, in the absence of identified causative microorganisms. Culture-negative PJI may be due to the inability to recover an organism known to cause PJI as a result of prior antimicrobial therapy, an inadequate use of available microbiological methods, or an inability to detect a recognized PJI pathogen using currently available diagnostic methods. Alternately, culture-negative PJI may be due to previously unrecognized causes of PJI that are not readily identifiable through currently used techniques. Both of these assertions are plausible and supported by the literature (29, 223, 248). Strict withholding of antimicrobials prior to surgery and improvements in microbiological techniques may decrease the number of culture-negative infections. A final possibility is that some cases currently classified as PJI are not truly infections (i.e., misclassification based on current diagnostic schemes).
The frequency of culture-negative PJI varies from 5 to 35% (96, 101), depending on the study, but the true proportion is likely closer to 7 to 15%. Culture-negative PJI is typically of delayed or late onset, with only 15% occurring within the first 3 months after arthroplasty implantation (66). In one large study, a culture-negative PJI diagnosis was made a median of 3 1/2 years after implantation (249).
The most important risk factor for culture-negative PJI is antecedent antimicrobial therapy (66). A history of a previous PJI, postoperative wound drainage, or vascular insufficiency is also associated with culture-negative PJI. The clinical presentation of culture-negative PJI is similar to that of culture-positive PJI, with pain being the most frequently reported symptom, followed by joint swelling, erythema, or warmth. The median duration of symptoms is approximately 100 days prior to diagnosis (249).
DIAGNOSIS
The diagnosis of PJI is based upon a combination of clinical findings, laboratory results from peripheral blood and synovial fluid, microbiological data, histological evaluation of periprosthetic tissue, intraoperative inspection, and, in some cases, radiographic results. There is no one test or finding that is 100% accurate for PJI diagnosis. Test characteristics and relative costs of commonly available tests shown in Table 2 may assist clinicians in choosing the most appropriate diagnostic approach for each individual patient. The general approach to PJI diagnosis is 2-fold. First, the question as to whether or not the joint is infected must be answered; second, if PJI is present, the causative microorganism(s) must be identified, and, in most cases, its antimicrobial susceptibility must be determined. Test performance may vary with joint type and also with timing post-arthroplasty implantation; where data are available that addresses this, they will be presented.
TABLE 2.
Test characteristics and relative costs of several preoperative tests for diagnosis of prosthetic joint infectionb
| Test | Joint(s) | Threshold value or finding | Sensitivity (%) | Specificity (%) | + LR | − LR | Diagnostic odds ratio | Cost | Description (reference) |
|---|---|---|---|---|---|---|---|---|---|
| Peripheral blood | |||||||||
| WBC | Hip and knee | 11,000 × 109 cells/litera | 45 | 87 | 3.5 | 0.6 | 5.5 | $ | MA of 1,796 patients in 15 studies (253) |
| CRP | Hip and knee | 10 mg/litera | 88 | 74 | 3.4 | 0.2 | 20.9 | $ | MA of 3,225 patients in 23 studies (253) |
| ESR | Hip and knee | 30 mm/ha | 75 | 70 | 2.5 | 0.4 | 7.0 | $ | MA of 3,370 patients in 25 studies (253) |
| IL-6 | Hip and knee | 10 pg/mla | 97 | 91 | 10.8 | 0.0 | 326.9 | $ | MA of 432 patients in 3 studies (253) |
| Procalcitonin | Hip and knee | 0.3 ng/ml | 33 | 98 | 16.5 | 0.7 | 24.1 | $ | Single study with 78 patients (262) |
| Imaging | |||||||||
| Plain radiograph | Hip | Lucency or periosteal new bone formation | 75 | 28 | 1.0 | 0.9 | 1.2 | $ | Single study with 65 patients (264) |
| Triple-phase bone scan | Late hip | Increased uptake in all 3 phases | 88 | 90 | 8.8 | 0.1 | 66.0 | $$$ | Single study with 46 patients (268) |
| Bone scan/labeled leukocyte scan | Late hip and knee | Incongruent images | 64 | 70 | 2.1 | 0.5 | 4.1 | $$$ | Single study with 166 patients (270) |
| FDG-PET scan | Hip and knee | Various | 82.1 | 86.6 | 6.1 | 0.2 | 29.6 | $$$$$ | MA of 11 studies with 635 patients (272) |
| Synovial fluid analysis | |||||||||
| Cell count | Knee | 1,100 cells/μl | 90.7 | 88.1 | 7.6 | 0.1 | 72.2 | $$ | Single study with 429 patients (273) |
| Neutrophil percentage | Knee | 64% | 95.0 | 94.7 | 17.9 | 0.1 | 339.5 | $$ | Single study with 429 patients (273) |
| Cell count | Hip | 4,200 cells/μl | 84.0 | 93.0 | 12.0 | 0.2 | 69.8 | $$ | Single study with 201 patients (276) |
| Neutrophil percentage | Hip | 80% | 84.0 | 82.0 | 4.7 | 0.2 | 23.9 | $$ | Single study with 201 patients (276) |
| Cell count | Knee (<6 wk after implantation) | 27,800 cells/μl | 84.0 | 99.0 | 84.0 | 0.2 | 519.7 | $$ | Single study with 146 patients (257) |
| Neutrophil percentage | Knee (<6 wk after implantation) | 89% | 84.0 | 69.0 | 2.7 | 0.2 | 11.7 | $$ | Single study with 146 patients (257) |
| Culture | Hip and knee | 72.0 | 95.0 | 14.4 | 0.3 | 48.9 | $$ | MA of 34 studies with 3,332 patients (293) |
Median threshold for studies included in the meta-analysis.
WBC, white blood cell count; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; IL-6, interleukin-6; + LR, positive likelihood ratio; − LR, negative likelihood ratio; MA, meta-analysis.
Diagnostic Criteria
For many years, research on PJI has been limited by a lack of standardized diagnostic criteria. This limitation must be considered when interpreting the PJI literature. Over the last several years, several groups, including the Infectious Diseases Society of America (IDSA) and the Musculoskeletal Infection Society (MSIS), have published proposed or accepted definitions for the diagnosis of PJI (60–62). Although the definitions vary, a recent study showed a high concordance between the IDSA and MSIS definitions of PJI (250). Additionally, the European Bone and Joint Infection Society (EBJIS), the American MSIS, and a number of other organizations from around the world recently held an international consensus meeting in an attempt to refine an international consensus definition of PJI (251).
The MSIS PJI definition is similar to the Duke criteria for endocarditis, with major or definitive criteria for PJI diagnosis as well as minor or supportive criteria (61). Definitive evidence of PJI is a sinus tract in communication with the prosthesis or an identical pathogen found in two separate periprosthetic tissue or fluid samples. The presence of four (or more) of six minor criteria can also fulfill a diagnosis of PJI. Like the MSIS definition, the IDSA definition of PJI also considers the presence of the sinus tract and two or more sterile site cultures with identical microorganisms to be definitive evidence of PJI (60). However, this definition additionally includes purulence without another known etiology as definitive evidence of PJI, while purulence is a minor criterion in the MSIS definition. Purulence has been removed from the International Consensus Meeting definition of PJI (251). If using the IDSA definition, exclusion of other causes of purulence, such as adverse reactions to metal debris, is necessary (252). The IDSA definition does not include inflammatory markers or synovial fluid cell counts and does not use the same major and minor formats as the MSIS definition. Rather, the IDSA definition provides other features that may support the diagnosis of PJI, such as growth of a virulent organism from a single culture or the finding of acute inflammation by periprosthetic tissue histopathology. Finally, each set of diagnostic criteria notes that PJI may be present in the absence of fulfilling all of the criteria. The diagnostic criteria for each group are shown in Table 3.
TABLE 3.
Proposed definitions for prosthetic joint infectiona
| Criterion | Definition of prosthetic joint infection |
|||||
|---|---|---|---|---|---|---|
| Musculoskeletal Infection Society |
International consensus |
Infectious Diseases Society of America |
||||
| Definitive evidence | Supportive evidence | Definitive evidence | Supportive evidence | Definitive evidence | Supportive evidence | |
| Sinus tract communicating with the prosthesis | x | x | x | |||
| Identical microorganisms isolated from 2 or more cultures | x | x | x | |||
| Purulence surrounding the prosthesis | x | x | ||||
| Acute inflammation upon histological examination of periprosthetic tissue | x | x | x | |||
| Single culture with any microorganism | x | x | ||||
| Single culture with a virulent microorganism | x | |||||
| Elevated synovial fluid leukocyte countb | x | x | ||||
| Elevated synovial fluid neutrophil percentage | x | x | ||||
| Elevated serum ESR and CRP values | x | x | ||||
The MSIS definition requires 4 supportive criteria; the International Consensus Meeting definition requires 3 supportive criteria. Data are from references 60, 61, and 251. ESR, erythrocyte sedimentation rate; CRP, C-reactive protein.
The International Consensus Meeting definition also includes a “++” result on the leukocyte esterase strip.
Peripheral Blood Tests
For the diagnosis of PJI, peripheral blood tests rely upon assessing the host response to the infecting pathogen. The peripheral white blood cell count is typically ordered as part of routine blood work at the time of initial evaluation but is limited by a low sensitivity of 45%, although the reported specificity of 87% may be useful in some situations (253).
Erythrocyte sedimentation rate and C-reactive protein.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels are the most frequently used inflammatory markers and are suggested as part of the diagnostic algorithm in IDSA (60) and American Academy of Orthopedic Surgeons (AAOS) (254) PJI documents, as well as being part of the minor diagnostic criteria in the MSIS statement (61). Both have the advantage of being widely available and inexpensive, with a rapid turnaround time in most laboratories. However, they are limited by their relative lack of specificity, a concern for patients with underlying inflammatory joint disease such as rheumatoid arthritis. CRP has a slightly better sensitivity and specificity than ESR (253). A meta-analysis of 3,225 patients in 23 studies by Berbari and colleagues found pooled sensitivity and specificity values for CRP of 88 and 74%, respectively (253). The thresholds used in those studies ranged from 0.3 to 13.5 mg/dl, with the most frequently used threshold being 10 mg/liter. That same meta-analysis evaluated 3,370 patients in 25 studies examining ESR and found pooled sensitivity and specificity values of 75 and 70%, respectively. Again, the threshold value in each of these papers varied from 12 to 40 mm/h, with the most commonly used threshold being 30 mm/h. In clinical practice, these tests are typically ordered together. The utility of these two tests performed together was evaluated in a study of 116 patients with and 180 patients without PJI, all undergoing knee arthroplasty revision surgery (255). When thresholds of 30 mm/h for ESR and 10 mg/liter for CRP levels were used, the combination of normal ESR and normal CRP values was 96% sensitive for ruling out PJI. The specificity of this combination, where either one or both tests were positive, was low, at 56%. In clinical practice, the specificity is likely even lower, given that this study excluded 32 patients who were considered to have confounding factors that might elevate values for the inflammatory markers. Nevertheless, the finding of normal ESR and CRP values is helpful for lowering the probability of PJI.
The time from last revision surgery and the joint involved influence the test performance characteristics for ESR and CRP, given the effect of surgery on these markers. A large retrospective study evaluated 1,962 patients who underwent revision surgery for either aseptic failure (1,689 patients) or PJI (273 patients, using MSIS definitions) (256). This study sought to determine the optimal thresholds for ESR and CRP values using receiver operating characteristic (ROC) curve analysis; the analysis was stratified by PJI type (early onset, defined as <4 weeks after arthroplasty, or delayed/late onset) and the joint involved (hip or knee). The optimal threshold values for early-onset PJI were similar for both joints, at 54.5 mm/h and 23.5 mg/liter for ESR and CRP, respectively. CRP was 87% sensitive and 94% specific, compared to 80 and 93%, respectively, for ESR. The threshold used was slightly higher than that in a previous study of early knee arthroplasty infections, which reported an optimal threshold of 16.6 mg/liter for CRP (257). However, that study did not find the determination of ESR to be useful in the early postoperative period. The optimal threshold for CRP in delayed/late-onset PJI was lower for hips than for knees, at 13.5 versus 23.5 mg/liter (256). The optimal thresholds for ESR in this group were 48.5 mm/h for hips and 46.5 mm/h for knees. The resulting test characteristics were not reported. These thresholds are higher than those reported in the majority of the papers included in the meta-analysis mentioned above (253). Determinations of ESR and CRP levels are less accurate for shoulder than for hip or knee arthroplasty infection, even when using ROC curve analysis to determine optimal thresholds for each joint (258). This may be related to the higher proportion of P. acnes infections in shoulder PJIs.
Interleukin-6.
Interleukin-6 (IL-6) is produced by stimulated monocytes and macrophages and is of interest in the diagnosis of PJI. One theoretical advantage of determining the serum IL-6 level is that it rapidly returns to normal shortly after joint arthroplasty, peaking the same day, with a mean half-life of only 15 h, compared to a half-life of 62 h for CRP (259). This could make it a useful marker in the early postoperative period as well as for differentiating other, more acute causes of elevated levels of inflammatory markers in patients with late PJI. The above-mentioned meta-analysis examined three studies, including 432 patients, that evaluated IL-6; there were pooled sensitivity and specificity values of 97 and 91%, respectively (253), using thresholds ranging from 10 to 12 pg/ml. Since that meta-analysis was reported, one additional series of 46 patients with hip arthroplasties found that an IL-6 threshold level of 9 pg/ml provided sensitivity and specificity of 81 and 77%, respectively (260). However, the definition of PJI was not explicitly detailed, and 13% of the noninfected group had growth from two or more specimens, suggesting that some patients may have been incorrectly classified. Finally, an additional study evaluated a number of different serum assays, including IL-6, in 20 patients with aseptic failure and 15 with staphylococcal PJI (261). A threshold value of 1.89 pg/ml was used, which is lower than those reported in previous studies, and the sensitivity of 46.7% was also discrepant from previous results. Given the lack of robust, consistent data, in addition to its less widespread availability than ESR and CRP tests, the IL-6 test is not currently part of standard clinical practice.
Procalcitonin.
Determination of serum procalcitonin levels has shown utility in other infections but has been investigated in only a small number of patients for diagnosis of PJI. One study involving 78 patients found that testing of serum procalcitonin levels was specific (98%) but insensitive (33%) (262). Because of its utility in other infectious diseases, this test is more widely available than the IL-6 test and may be helpful for patients thought to have noninfectious reasons for elevated ESR and CRP values. However, further data are necessary before it can be recommended.
Imaging
Plain radiographs.
Imaging may support the diagnosis of PJI in certain circumstances but rarely has a definitive role in PJI diagnosis. Plain radiographs are typically obtained in patients undergoing evaluation for possible PJI. They may help identify noninfectious causes for the presenting symptoms, including periprosthetic fracture, fracture of the arthroplasty material, or dislocation. Detection of periprosthetic lucency, loosening of the prosthesis components, effusion, adjacent soft tissue gas or fluid collection, or periosteal new bone formation may suggest infection but is neither sensitive nor specific (263). For example, a study of 65 patients with painful hip arthroplasties found that the presence of either lucency or periosteal new bone formation was 75% sensitive but only 28% specific for diagnosis of PJI (264). Periosteal new bone formation alone was 100% specific but occurred in only 16% of patients with PJI. Serial radiographs with progressively expanding lucency over several months may also suggest PJI. Plain radiographs also assist the surgeon with preoperative planning.
Advanced imaging studies.
Computed tomography (CT) and magnetic resonance imaging have the advantages of high spatial resolution and allow evaluation of signs of infection in the periprosthetic tissues. One study found that detection of joint distention upon CT imaging was highly sensitive (83%) and specific (96%) for suspected hip arthroplasty infection (264). However, the added benefit of these findings beyond history and physical examination findings is unclear. That same study found no difference in the evaluation of the bony structures compared to the use of plain radiographs. Furthermore, the use of these techniques is limited by imaging artifacts due to the presence of the metal prosthesis. In addition, magnetic resonance imaging can be performed only with certain metals, such as titanium or tantalum. Adjustments in the image acquisition parameters can lessen but not eliminate these artifacts.
Three-phase bone scintigraphy is one of the most widely utilized imaging techniques in the diagnosis of PJI. Using this technique, a radioactive isotope is attached to a compound that preferentially collects in bone. This compound will accumulate in areas of high metabolic activity and emit gamma rays that can be detected by a gamma camera. The intensity of uptake following injection of the radiopharmaceutical is measured at three different time points, corresponding to blood flow (immediate), blood pool (at 15 min), and late (at 2 to 4 h) time points (265). Uptake at the prosthesis interfaces at the blood pool and late time points suggests PJI. A limitation of this technique is the lack of specificity. Asymptomatic patients frequently have uptake detected by delayed-phase imaging in the first year or two after implantation (266). Given that the majority of PJIs occur within this time period (7), this lack of specificity, reportedly as low as 18%, is a limitation for the use of this technology (65). However, three-phase bone scintigraphy may be more useful for PJI occurring late after arthroplasty. A study of 92 patients undergoing evaluation for revision of hip arthroplasty a mean of 9 years after implantation found that increased uptake at both the second and third phases provided sensitivity and specificity of 68 and 76%, respectively (267). The fact that only a minority of these patients underwent revision limits comparison to a true diagnostic gold standard. Another study reported a sensitivity of 88% and a specificity of 90% for 46 patients a mean of 8.5 years after hip arthroplasty (268).
Other imaging modalities may be performed in conjunction with bone scintigraphy, in an effort to increase specificity. Radioactive 111In is frequently used to label autologous leukocytes, which are then injected, with images being obtained 24 h later. A positive scan is typically considered when there is uptake on the labeled leukocyte image, with absent or decreased uptake at the same location on the late-phase bone scan (269). A late-phase bone scan combined with a 111In leukocyte scan was 64% sensitive and 70% specific for detection of PJI in 166 revision knee or hip arthroplasties a median of 7 years after implantation (270). Other smaller studies using slightly different technologies have reported somewhat higher accuracies, with sensitivities ranging from 77 to 100% and specificities ranging from 86 to 91% (269, 271).
[18F]Fluoro-2-deoxyglucose positron emission tomography (FDG-PET) is widely used in cancer care and treatment and has emerged as a diagnostic modality for PJI. A meta-analysis of 11 studies involving 635 prosthetic hip and knee arthroplasties found that FDG-PET had pooled sensitivity and specificity values of 82.1 and 86.6%, respectively, for the diagnosis of PJI (272). A limitation of this technique is its high cost.
In general, the majority of patients with suspected PJI do not need an advanced imaging modality to make the diagnosis of PJI. However, for selected patients for whom further imaging is warranted, careful selection among the available tests is necessary. The cost, additional information that might be gained from the test, and time from the start of the test to the availability of results should be considered when making this decision. Additionally, discussion with a radiologist with special expertise in this area is helpful.
Synovial Fluid Analysis
Synovial fluid can be obtained through preoperative or intraoperative aspiration and provides valuable data for the diagnosis of PJI. Preoperative aspiration is recommended as part of the second step of evaluation for possible PJI in IDSA guidelines, following examination, CRP and ESR tests, and performance of plain radiography (60). Synovial fluid aspiration of a knee arthroplasty is easily performed in the office, but aspiration of a hip arthroplasty frequently requires fluoroscopic guidance. Synovial fluid is commonly sent for determination of nucleated cell counts and percentages of neutrophils and for bacterial culture. A number of other direct or indirect markers of infection are being investigated but are not widely used at this time.
Nucleated cell count and neutrophil differential.
Preoperative aspiration for determination of total nucleated cell counts and neutrophil percentages has high sensitivity and specificity for PJI. The threshold for a positive test is varied in different study populations and different joint types. One study evaluated 429 patients with knee arthroplasties, 161 of whom were diagnosed with infection (273). The time from last revision surgery in this study varied widely, from <2 months to >7 years. A threshold of 1,100 total nucleated cells per microliter provided sensitivity and specificity of 90.7 and 88.1%, respectively, while a threshold of 64% neutrophils had sensitivity and specificity of 95 and 95%, respectively. A smaller study of 133 patients (34 PJIs) with knee arthroplasties found that a slightly higher threshold of 1,700 total nucleated cells per microliter provided sensitivity and specificity of 94 and 88%, respectively (274). A similar threshold of 65% for the neutrophil percentage was determined, with slightly higher sensitivity and specificity values of 97 and 90%, respectively. In contrast to the previous study, this study included only patients at least 6 months from prior revision. Finally, a more recent study of 153 patients undergoing knee revision found that an even higher threshold of 3,000 total nucleated cells per microliter had sensitivity and specificity of 93 and 94%, respectively (275). A threshold of 75% neutrophils was 93% sensitive and 83% specific. There was, notably, no information provided as to the age of the arthroplasty at the time of aspiration. Based on the largest study to date (273), we suggest the use of thresholds of 1,100 total nucleated cells per microliter and 64% neutrophils for knee arthroplasties. However, neither MSIS nor IDSA diagnostic criteria include a specific threshold (60, 61), highlighting the fact that these results need to be interpreted for each individual patient. Further research should help clarify the optimal threshold.
Synovial fluid cell counts may be elevated due to hemarthrosis or postoperative inflammation in the time period shortly after primary implantation. In one study of 146 knee arthroplasties, the average total nucleated cell count obtained 17 days after surgery was 92,600 cells per microliter in patients with PJI, compared to 4,200 cells per microliter in those without (257). The optimal threshold, determined via ROC curve analysis, was 27,800 cells per microliter, which provided a sensitivity of 84% and a specificity of 99%. A threshold of 89% neutrophils provided an identical sensitivity of 84%, with a markedly lower specificity of 69%. These data may help to avoid reoperation in patients with a painful knee arthroplasty and modestly elevated cell counts in the early postoperative setting.
The optimal thresholds for synovial fluid total nucleated cell counts and neutrophil differential appear to be higher in hip than in knee arthroplasties, but the data supporting this are less robust. A study of 201 hips (55 PJIs) found that a total nucleated cell count of 4,200 cells per microliter provided sensitivity and specificity of 84 and 93%, respectively (276). A threshold of 80% neutrophils had sensitivity and specificity of 84 and 82%, respectively. The reason for the higher optimal threshold for hip arthroplasties found in this study than for knee arthroplasties in the above-mentioned studies may be due to the higher frequency of S. aureus (44%) in this cohort (276) than in the two cohorts with knee arthroplasties (20 to 24%) (273, 274). Infection with S. aureus is associated with a higher total nucleated cell count than infection with coagulase-negative staphylococci (274). A small study of 75 patients including both total knee and hip arthroplasty found a threshold similar to that used for knees in the above-described larger studies (277). Analysis of the 27 patients with hip arthroplasty in place suggested an optimal threshold of 1,715 cells per microliter. Finally, a more recent study of 810 patients (146 PJIs) with hip or knee arthroplasties found that a threshold of 3,450 cells per microliter was 91% sensitive and 93% specific (32). A neutrophil differential of 78% was 95% sensitive and 87% specific. Fifty-five percent of the joints in this study were hip arthroplasties, but the joint types were not analyzed separately. These conflicting data suggest that the optimal total nucleated cell count threshold for diagnosis of hip arthroplasty infection is unclear but may be <4,200 cells per microliter.
An important caveat in the majority of these studies is that patients with inflammatory causes of joint disease, such as rheumatoid arthritis, were excluded, which may preclude application of the results of these data to patients with such conditions. For such patients, a higher baseline nucleated cell count would be expected, and accordingly, the threshold values mentioned above would be expected to be less specific. One of the above-mentioned studies included 61 patients with and 810 patients without inflammatory arthritis and found no difference in test performance between the two groups of patients (32). A threshold of 3,444 cells/microliter demonstrated a sensitivity of 88% for patients with inflammatory arthritis. However, as expected, the specificity was lower for patients with inflammatory arthritis (80%) than for those without (93%). A cutoff of 75% neutrophils resulted in high sensitivity (100%) and specificity (82%) for patients with inflammatory arthritis. It should be noted that there were only 19 infections in the patients with inflammatory joint disease, so these results should be confirmed in larger studies.
Finally, failed metal-on-metal hip arthroplasties can give a falsely elevated synovial fluid cell count when using automated cell counters. This can be overcome by manually counting cell numbers, and the neutrophil percentage remains accurate for this group of patients, given that it is determined manually. The sensitivity and specificity of 80% neutrophils were 100% and 97%, respectively, in 39 patients with metal-on-metal hip arthroplasties (278). Recently presented data from this group suggest that the use of manual synovial fluid nucleated cell counts increases specificity, but these data have not yet been published. If possible, manual nucleated cell counts should be performed for patients with metal-on-metal hip arthroplasties. If manual nucleated cell counts are not available, the neutrophil differential appears to be more reliable.
Synovial fluid leukocyte esterase.
Leukocyte esterase is an enzyme present in neutrophils. A colorimetric strip measuring leukocyte esterase is widely available as a point-of-care test to determine pyuria for the diagnosis of urinary tract infection. This test strip has recently been proposed as a point-of-care test for synovial fluid from either preoperative or operative aspirates. Two studies have evaluated this test for preoperative or intraoperative diagnosis of PJI in a total of 348 hip and knee arthroplasties (279, 280). A “++” reading provided 81% sensitivity and 100% specificity for both intraoperative and preoperative specimens in one of these studies (279). This study also found a strong correlation between results of the leukocyte esterase strip and the percentage of neutrophils. However, 17 patients were excluded from this analysis due to excessive blood in the synovial fluid sample. This limitation was also reported in the second study, where 29% of strips were unreadable due to blood, debris, or indeterminate results (280). For the use of a + or ++ result as a positive test, the sensitivity and specificity for diagnosis of PJI were 93 and 77%, respectively. The authors of this study did not report the test characteristics using just ++ as a positive result, but presumably, this would provide a higher specificity. The ultimate role of this test is unclear, but it has been included as supporting criteria in the International Consensus Meeting definition of PJI (251). It may be a useful adjunctive test to confirm the diagnosis of PJI intraoperatively when PJI is suspected but not confirmed during preoperative evaluation. The role of this test for screening at the time of routine revision for presumed aseptic failure or for reimplantation arthroplasty as part of a two-stage arthroplasty exchange for infection is unclear. However, due to the relatively low sensitivity and the availability of other rapid diagnostic tests with more data, such as frozen-section histological tests, it may not be the ideal test for this specific situation.
Other synovial fluid markers.
Several other markers, including those otherwise used in serum, show some promise for the diagnosis of PJI. In three studies evaluating synovial fluid CRP in a total of 188 patients, the sensitivities were similar among all three studies, ranging from 85 to 87%, but the specificities varied widely (281–283). Interestingly, the lowest specificity was reported when the highest cutoff (10 mg/liter) was used (71%) (283). The other two studies (evaluating 137 of the patients) used different cutoffs (3.6 and 9.5 mg/liter) but observed similar specificities of 98 and 95%, respectively (281, 282). The consistently high area under the ROC curve (0.92) from the two larger studies suggests that this is a promising test with high specificity. Determination of synovial fluid IL-6 levels has demonstrated variable sensitivity (69 to 100%) and high specificity (93 to 100%) (282–284). Determination of synovial fluid IL-1β levels demonstrated slightly lower sensitivity and specificity. One study found both IL-6 and IL-1β tests to be superior to synovial fluid cell counts, but the sensitivity and specificity of both markers were 100%, much higher than those reported in other studies (283). Synovial fluid procalcitonin has also been evaluated, but the only published study included only 14 subjects with prosthetic joints (285).
Antimicrobial peptides, such as α- and β-defensins, are produced as part of the innate immune response and are found in bone and synovial tissue, among other sites. Only one small screening study evaluating these markers has been published in the peer-reviewed literature (261). This may be a promising technology, but the data are in its infancy, and until further data are available, a recommendation for clinical use cannot be made.
Synovial fluid culture.
In addition to informing the diagnosis of PJI, preoperative synovial fluid culture is invaluable for early identification of the infecting pathogen(s) and determination of antimicrobial susceptibility. This information can inform the choice of perioperative antimicrobials and construction of antimicrobial-loaded polymethylmethacrylate (PMMA) and may impact the selection of a treatment strategy, if a particularly sensitive or resistant pathogen is present.
Aspirated fluid can be either inoculated into blood culture bottles at the time of collection or transported to the microbiology laboratory and inoculated onto solid and/or liquid media. Several large studies from the 1990s including a total of 567 patients undergoing hip arthroplasty revision performed aspiration and culture using only solid or liquid media and found widely varied sensitivities as low as 50%, with relatively consistent specificity ranging from 88 to 97% (286–288). In contrast, more recent studies have used aerobic and anaerobic blood culture bottles inoculated in the procedure suite. This method has the advantages of increased pathogen recovery and decreased risk of contamination when used with native joint synovial fluid (289). In a total of 306 joints (218 hips and 88 knees) undergoing revision, the sensitivity was consistently high, at 86 to 87%, with a specificity ranging from 95 to 100% (290–292). However, another large study of 250 patients with hip or knee arthroplasties found a lower sensitivity for synovial fluid culture of 66%, even with the use of blood culture bottles (29). The reason for the lower sensitivity in this study is not clear but may be related to the fact that 25% of patients had received antibiotics in the 2 weeks prior to aspiration. In contrast, in the previous studies, antibiotics were either stopped at least 2 or 3 weeks prior to aspiration (290, 292) or not reported (291). Additionally, the sensitivity of synovial fluid culture is higher for acute (91%) than for chronic (79%) PJI, which may be important in referral centers (291). This may be due to a number of factors, including a difference in the load of microorganisms, administration of antimicrobials before aspiration, and the infecting pathogen. Finally, a recent meta-analysis of 34 studies including 3,332 patients found a pooled sensitivity of 72% and a specificity of 95% for synovial fluid culture (293). Subgroup analysis was unrevealing but did not examine the method of culture. Based on the above-described data, synovial fluid culture is a helpful part of the preoperative evaluation for PJI. Synovial fluid should be inoculated directly into blood culture bottles, and antibiotics should be withheld at least 2 weeks prior to aspiration, whenever possible.
Periprosthetic Tissue
Preoperative periprosthetic tissue biopsy.
Testing of periprosthetic tissue is one of the most valuable components in the routine microbiological diagnosis of PJI. Samples of periprosthetic tissue are most often obtained at the time of revision surgery, but preoperative arthroscopic tissue biopsy may alternatively or additionally be performed. In a prospective study of 145 knee arthroplasties prior to revision, microbiology and histology results from preoperative tissue biopsy specimens were compared to results of synovial fluid and serum CRP tests (294). PJI, defined as at least 2 of 5 cultures with the same organism or a single positive culture along with histology showing acute inflammation, was present in 40 total knee arthroplasties. The sensitivity of biopsy was reported to be 100%, but this is expected, given that the definition of PJI was based primarily on the biopsy results. Given that many patients can be classified as infected based on a combination of data obtained through less invasive methods, the most useful contribution of a preoperative biopsy would be to define the causative microorganism(s) and antimicrobial susceptibility test results. Accordingly, the sensitivity and specificity for microbiology tests were 78% and 98%, respectively, for biopsy specimens, compared to 73% and 95%, respectively, for aspirated fluid. Another large study comparing preoperative synovial fluid aspiration and tissue biopsy in 273 patients with hip arthroplasty found that aspiration was more accurate (295). Several other studies have reported sensitivities of tissue biopsy ranging from 79 to 88% (296, 297). Given the lack of demonstrated superiority and the additional expense and possible complications of the involved procedure, preoperative biopsy is not routinely recommended.
Intraoperative periprosthetic tissue Gram staining.
Although periprosthetic tissue Gram staining theoretically offers the surgeon the ability to rapidly confirm or refute the diagnosis of PJI while in the operating room, in practice, it has a very low sensitivity and therefore offers little additional information. A number of studies have reported the sensitivity of tissue Gram staining to range from 0 to 27%, with a specificity of >98% (298–302). Importantly, patients with a positive Gram stain are frequently those for whom the diagnosis of PJI is not in question prior to surgery, such as those with a high synovial fluid cell count or elevated serum C-reactive protein levels (298). Given the availability of frozen sections for rapid intraoperative diagnosis of PJI, the poor test characteristics of tissue Gram staining, and the numerous other available preoperative tests, tissue Gram staining is not routinely recommended.
Intraoperative periprosthetic tissue culture.
Periprosthetic tissue culture is a valuable diagnostic tool for PJI. However, obtaining only a single tissue specimen for culture may create significant confusion, given the low sensitivity of a single specimen and the difficulty in interpreting potential contamination with low-virulence microorganisms, and should therefore be avoided. Over 30 years ago, Kamme and Lindberg recognized these challenges and found that pathogens could be distinguished from contaminants when five tissue specimens were obtained (303). Since that time, it has been repeatedly recognized that obtaining multiple tissue specimens for culture is ideal. Atkins and colleagues prospectively examined 297 patients, including 41 with PJIs, undergoing revision surgery (302). Using mathematical modeling, those authors determined that the ideal number of specimens is at least 5 or 6, with 3 or more specimens yielding an indistinguishable microorganism being the ideal cutoff. However, this threshold demonstrated a low sensitivity (65%). A subsequent study evaluated 122 patients for whom a mean of 4 samples per patient (range, 1 to 7) were sent to the microbiology laboratory (304). Using the same mathematical modeling from the study by Atkins et al., these authors determined that isolation of the same organism from three or more cultures out of five samples demonstrated the best test characteristics, with a sensitivity of 80% and a specificity of 97%. However, other investigators have used a threshold of two specimens yielding indistinguishable microorganisms in order to increase the sensitivity (94, 248), and this has been incorporated into PJI consensus documents (60, 61, 251). A single positive culture is often regarded as a contaminant, especially in the setting of a low-virulence organism. However, a single positive culture may be important, especially when virulent organisms (such as S. aureus, beta-hemolytic streptococci, or aerobic Gram-negative bacilli) are isolated or when the same organism is found in a different specimen type, such as synovial or sonicate fluid. Nevertheless, for the reasons mentioned above, submission of single tissue specimens for culture is not recommended.
The specific media used for culture of periprosthetic tissue have been examined to a limited extent. The majority of recent studies have used aerobic and anaerobic blood agar, and some have also used thioglycolate broth (248, 304). One recent large study involving 178 patients compared the sensitivities and specificities of four different culture media to a gold standard of acute inflammation in periprosthetic tissue (305). Culture using cooked meat broth (83%) or blood culture bottles (87%) was more sensitive than culture using fastidious anaerobic broth (57%) or solid-agar plates (39%). Specificity was 97 to 100% for each medium type. A limitation of this study is that only 23 PJI cases were included, and thioglycolate broth was not evaluated (305). Culture using aerobic and anaerobic conditions should be performed in all cases.
The optimal duration of incubation for periprosthetic tissue culture is of considerable debate and is particularly germane to the isolation of P. acnes. Traditionally, aerobic cultures are incubated for up to 4 days, and anaerobic cultures are incubated for up to 7 days; incubation beyond these points is thought to increase the number of contaminants. However, several studies have recently challenged this dogma. Schafer and colleagues incubated five periprosthetic tissue specimens per patient for 14 days and compared the time to detection of organisms with the diagnosis of PJI based on histology or identification of identical organisms in multiple tissue specimens (94). Aerobic cultures were performed by using blood agar, chocolate agar, and brain heart infusion broth, while anaerobic cultures were performed by using Schaedler agar and Schaedler broth. PJI was detected in 110 of 284 patients, but the detection rate was only 74% after 7 days of incubation. The microorganisms found in the second week of culture were predominantly Propionibacterium species, aerobic Gram-positive bacilli, and Peptostreptococcus species. Although contaminants were detected later than pathogens, with a median time to detection of 7 days, 52% of contaminants were grown within the first week. Based on these findings, the authors suggested that periprosthetic tissue should be cultured for 14 days. A subsequent paper specifically looked at P. acnes, primarily in patients undergoing revision of shoulder arthroplasty (177). These investigators incubated specimens from 198 surgeries for 28 days using blood, chocolate, and brucella agar and brain heart infusion broth and retrospectively determined the optimal duration of incubation. There were 19 infections involving P. acnes in this study, with all infected events being detected by 13 days. However, only approximately 20% of infections were detected by day 7, and nearly 30% of infections would not have been detected had extended incubation been applied only to anaerobic cultures. These authors suggested that both aerobic and anaerobic cultures should be incubated for 13 days. In contrast, a different study did not find an increase in detection of P. acnes infections when using anaerobic blood agar and anaerobic thioglycolate broth incubated for 14 compared to 7 days (306). Each of the 14 P. acnes infections in this study had at least two broth cultures that were positive by 7 days, and broth was more likely to be positive than were plate cultures by day 7 and overall. This may suggest a certain advantage of thioglycolate broth in this setting. At this time, the optimal duration of culture is unclear but likely depends in part on the medium that is used and not just on the incubation period.
Cultures obtained by using swabs.
Cultures obtained by using swabs have a limited role in the microbiological detection of PJI. While the presence of a sinus tract is considered definitive evidence of PJI (60, 61), swab culture of the drainage from the sinus tract is neither sensitive nor specific for the microbiological detection of PJI. Data from the literature on chronic osteomyelitis have classically been quoted as showing that the presence of S. aureus from a sinus tract culture is correlated with bone infection with the same organism. However, it should be recognized that the original paper that demonstrated this found S. aureus in only 44% of the sinus tracts from patients with osteomyelitis due to this organism (307). The utility of sinus tract swab culture has recently been evaluated in a prospective study of 55 patients with knee or hip arthroplasty and a draining wound (308). Among the 45 patients ultimately diagnosed with a PJI based on MSIS criteria, the concordance between superficial sinus tract culture and operative tissue culture was 53%. There was a nonsignificant trend toward a higher concordance rate for S. aureus than for other bacteria. There was no difference in the concordance rate based on acute versus chronic PJI, with numerically lower concordance in the acute PJI group. This is in contrast to a previous study of 56 patients with acute PJI that found a concordance of 80% (309); however, the definition of PJI was less rigidly defined in the second paper. Based on these data and the availability of more reliable microbiological information from preoperative joint aspiration, sinus tract culture cannot be recommended for PJI diagnosis or the definition of its microbiology.
Intraoperative cultures obtained via swabs are less accurate than tissue cultures. A recent prospective study compared intraoperative swabs from 117 patients undergoing revision arthroplasty and found that swab cultures obtained from the same site as tissue samples had lower sensitivity and specificity than tissue cultures (310). When using a cutoff of at least one positive specimen, the sensitivity and specificity of swab cultures were 70 and 89%, respectively, compared to 93 and 98%, respectively, for tissue cultures. The sensitivity was similar to that reported in another study of 150 patients undergoing revision, where sensitivities of swab and tissue cultures of 68 and 82%, respectively, were reported (291). The sensitivity of swab culture was particularly poor for patients with chronic PJI, at only 40%. Multiple operative tissues should be sent for culture; collection of multiple tissue specimens at revision arthroplasty should not be logistically challenging given the nature of the associated surgical procedure. Collection of swabs for culture is not recommended.
Histological analysis of periprosthetic tissue.
Histological evaluation demonstrating acute inflammation, evidenced by neutrophilic infiltrate on fixed or frozen tissue, is suggestive of PJI. The principle of pathological evaluation for PJI involves tissue sampling of the areas adjacent to the prosthesis that appear to be infected upon gross intraoperative inspection. The advantages of this technique are that it is unlikely to be changed with preoperative antibiotics, and with the use of frozen-section analysis, results are available to the surgeon in the operating room such that they can inform the surgical approach. The disadvantages of this technique include the need for a trained pathologist and variability in the definition of inflammation, depending on the pathologist interpreting the specimen. Additionally, it has been reported that some pathogens, such as P. acnes (178) and coagulase-negative staphylococci (311), may not consistently elicit a robust neutrophilic inflammatory response.
A frequently used definition of acute inflammation is the presence of at least 5 neutrophils per high-powered field, in at least 5 separate microscopic fields (312, 313). This criterion is included in one of the recent consensus definitions for PJI (61), while another consensus definition includes acute inflammation but does not specifically define it (60). An alternate system classifies the histological findings of the periprosthetic membrane into four different types (314). Type I or “wear-particle-induced” histology is defined by the presence of macrophages, multinucleated giant cells, and foreign-body particles. Type II or infectious histology is characterized by neutrophilic infiltrate and few foreign-body particles. Type III histology is the presence of both type I and II findings, while type IV histology is indeterminate. This system is less widely used but highlights the fact that the inflammatory response to infection may be present in conjunction with other histological findings.
Several anatomical sites for operative periprosthetic tissue biopsy have been classically used, including the joint pseudocapsule and the periprosthetic interface membrane between the prosthesis and the adjacent bone. A recent prospective study attempted to answer which is the most accurate site for histological diagnosis of PJI (315). Specimens from the pseudocapsule and periprosthetic interface membrane were obtained from 69 patients undergoing revision hip arthroplasty and compared to a definitive diagnosis of PJI, based on the presence of purulence around the prosthesis or two or more intraoperative cultures of the same organism. The sensitivity of the interface membrane was 83%, higher than that for the pseudocapsule, at 42%. The specificity was 98% for both specimen types. This sensitivity is similar to those reported in other studies that have evaluated the periprosthetic membrane (316). In contrast, the microbiological yield from the interface membrane does not appear to be superior to that from the pseudocapsule, based on one small study (315).
Frozen-section analysis is a valuable tool to support the diagnosis of PJI while the surgeon remains in the operating room, with results being available within 30 min, compared to one or more days for permanent histopathology (317). A recent meta-analysis of 26 studies involving >3,000 patients (796 PJIs) found that the presence of acute inflammation provided a high positive likelihood ratio of 12 (318). The absence of acute inflammation had a more modest negative likelihood ratio of 0.23. It should be recognized that there were multiple definitions of acute inflammation used in this meta-analysis. While this meta-analysis did not provide pooled sensitivity and specificity, these likelihood ratios suggest that frozen-section analysis is helpful to confirm or support the diagnosis of PJI in patients with an intermediate pretest probability of PJI. However, for the same patient with an intermediate pretest probability, the absence of acute inflammation will only modestly lower the posttest probability of PJI, and further data to exclude PJI would be necessary. For a patient with a low pretest probability of PJI, a negative frozen-section result may be sufficient to exclude this diagnosis.
Sonication of Removed Prosthetic Components
There has been considerable interest in developing methods to dislodge and culture bacteria living on the surface of prosthetic material. Smaller devices, such as intravenous catheters, can simply be rolled onto solid culture media. In contrast, the large size and complex three-dimensional shape of joint prostheses make this infeasible for routine clinical practice. Culturing of an entire implant in broth is not recommended due to the high rate of contamination, yielding false-positive results. There has been limited evaluation of mechanical removal or scraping of prostheses (319, 320). Sonication has emerged as a practical and effective method to dislodge biofilm and the associated bacteria from the surface of the implant. With this approach, low-frequency ultrasound waves pass through liquid surrounding the prosthesis, creating areas of high and low pressure (321). Microscopic bubbles are formed during the low-pressure stage and collapse during the high-pressure stage, releasing energy and liberating bacteria from the surface of the implant. The fluid surrounding the implant can then be submitted for culture or analyzed by culture-independent methods to detect bacteria.
Since first being widely published and recognized by Tunney and colleagues in the late 1990s, sonication protocols have undergone serial refinement. The first study utilizing a sonication protocol included 120 patients undergoing revision of hip arthroplasty (322). In this study, the femoral and acetabular components were aseptically placed into sterile bags and then into anaerobic jars for transport to the microbiology laboratory. The bags were filled with Ringer's lactate solution, placed into a sonication bath, and exposed to 5 min of sonication at 50 kHz. The sonicate fluid was then plated onto aerobic and anaerobic blood agar and incubated appropriately. This study demonstrated an increased yield with sonicate culture compared to tissue culture. However, the lack of a rigorous definition of PJI limited the interpretation and application of these data. A subsequent study of 78 patients with explanted hip or knee arthroplasties utilized a rigorous nonmicrobiological definition for PJI and demonstrated higher sensitivity than tissue culture by utilizing the protocol developed by Tunney and colleagues (323). However, the specificity for sonicate fluid was lower than that for tissue culture, due to bag leakage. These investigators subsequently modified this protocol in two important ways. First, a vortex step before sonication, in which the prosthesis and the surrounding fluid are placed onto a benchtop vortex device for 30 s, was added in an attempt to increase removal of bacteria from the prosthesis. Second, the implants were collected and sonicated in a rigid polypropylene container in an effort to decrease contamination. The resulting landmark study of 331 patients with hip and knee prostheses demonstrated a higher sensitivity (79%) than that of tissue culture (61%), along with a preserved specificity of 99% (248). This technique proved particularly useful for those patients receiving antimicrobial therapy in the 2 weeks prior to surgery, for whom the sensitivity of sonicate fluid was 75%, compared to 45% for tissue culture, a finding subsequently confirmed elsewhere (324). A team of Spanish investigators introduced a centrifugation step the following year, in an attempt to concentrate the removed bacteria and further increase the yield (325). However, this protocol used bags, and correspondingly, those authors observed a lower specificity. Finally, a small study in 2011 incorporated the use of solid containers, along with vortex and centrifugation steps, for removed elbow prostheses (117). Based on the advantages described above, this is the currently recommended protocol for sonication of explanted joint prostheses (Fig. 3).
FIG 3.
Prosthesis sonication protocol used in the Mayo Clinic Clinical Microbiology Laboratory. (Courtesy of David Lynch, reproduced with permission.)
Sonication has been performed on hip, knee, shoulder, elbow, and ankle prostheses, with a range of observed diagnostic accuracies. This may be influenced by differences in the specific sonication protocol used, the definition of PJI used, inclusion of osteosynthesis or nonjoint prostheses in individual studies, the threshold of colony counts per plate for a positive culture, chronicity of the infection, preoperative administration of antimicrobials, and the joint type in which the PJI occurred. The majority of studies over the last decade have demonstrated a higher sensitivity for culture of sonication fluid (62 to 94%) than periprosthetic tissue (54 to 88%) (29, 56, 117, 248, 315, 323–328). Studies that used a solid container to process prostheses have found specificities of 81 to 100% (29, 56, 117, 248, 315, 324, 326–328), compared to 43 to 87% for studies that used a bag (323, 325). The sensitivity for sonication of shoulder prostheses (66.7%) may be lower than that for hip or knee prostheses (72.9 to 78.5%), based on studies performed using nearly identical sonication protocols at the Mayo Clinic (29, 56, 248). The percentage of patients taking antimicrobials in the month prior to surgery was actually higher in the studies of knee and hip arthroplasties than in the study of shoulder arthroplasties. It is difficult to make any conclusions for elbow prostheses, given that only 36 patients were included in the largest study to date (117).
The optimal threshold to determine significant bacterial growth was examined in one of the earlier sonication studies. Without the use of a centrifugation concentration step, ROC curve analysis identified an optimal cutoff of 2 CFU per milliliter (248). However, the authors of this study considered that increasing the specificity by accepting a slight decrease in sensitivity was more clinically important and set the threshold at 10 CFU per milliliter. This provided a sensitivity of 79% and a specificity of 99%. Subsequent studies in the same institution, using a 100-fold concentration step, redefined a threshold of 200 CFU per milliliter (approximately equivalent to 2 CFU per milliliter of unconcentrated fluid) (56). Among the sonication studies that have reported threshold values for their methods, those using a concentration step have used a cutoff of 200 CFU per ml (29, 56, 117), while those not using a centrifugation step have reported threshold values ranging from 1 to 50 CFU per ml, with the majority using a cutoff of between 1 and 10 CFU per ml (107, 248, 324, 328). It should also be noted that the bacteria identified should be taken into account when considering a cutoff for significant growth. The presence of <10 CFU per ml of S. aureus or a member of the Enterobacteriaceae would less likely be considered a contaminant than finding the same quantity of a coagulase-negative Staphylococcus or a Propionibacterium species. Finally, it should be recognized that the use of solid rather than liquid media enables semiquantitative analysis, something that is not possible when a broth medium is used with sonicate fluid. The use of broth media is not recommended for sonicate fluid cultures due to the inability to distinguish contaminants from pathogens and the frequent presence of contaminants, given the size of the specimen collected, transported, and processed.
Vortexing of the prosthesis alone may be a viable alternative in laboratories in which sonication is not available. In vitro data suggest that vortexing alone can remove bacteria from biofilm-coated coupons (329). Portillo and colleagues prospectively compared the results of vortexing alone to the results of vortexing plus sonication of 135 removed prostheses (328). Using a cutoff of 50 CFU per milliliter (higher than what is traditionally used without a centrifugation step), there was a nonsignificant difference, with a 60% sensitivity for vortexing plus sonication, compared to a sensitivity of 40% for vortexing alone. This resulted in a specificity of 99% for both methods. However, when a cutoff of 1 CFU per milliliter was used, the sensitivities were nearly identical, at 69 and 71% for vortexing alone and vortexing plus sonication, respectively. This lower cutoff is similar to those of other published protocols of 1 to 10 CFU per milliliter, in which a centrifugation step is not used. Based on these cutoffs, vortexing of the prosthesis alone may be reasonable in laboratories that do not have the equipment or personnel to perform a full sonication protocol.
The role of sonication of the PMMA spacer at the second stage of a two-stage arthroplasty exchange is unclear. One study evaluated 55 patients undergoing a two-stage arthroplasty exchange for primarily hip or knee PJI and found a higher rate of clinical failure at 1 year in those with “subclinical infection” at the time of their second-stage procedure (330). Subclinical infection was defined as either a positive sonicate fluid culture from the spacer or two or more positive tissue specimens at the second-stage procedure. However, when examined individually, six of eight patients with a positive spacer sonicate culture developed clinical failure, compared to all six patients with positive tissue cultures. Another small study found that of six patients with positive spacer sonicate cultures, three had negative tissue cultures, suggesting some benefit to spacer sonication (331). However, further data are necessary before this can be recommended for all patients undergoing a two-stage arthroplasty exchange.
Additional testing of the sonicate fluid has been evaluated. Similar to periprosthetic tissue, Gram staining of sonicate fluid is insensitive (as low as 45%) but highly specific (248, 324). This is typically performed on sediment from centrifuged sonicate fluid but adds uncertain value. Immunofluorescence microscopy (56, 332) has been previously studied but is not in widespread use, due to the availability of nucleic acid amplification tests. PCR using sonicate fluid as well as synovial fluid and periprosthetic tissue is discussed below.
Molecular Diagnosis
The use of PCR technology in PJI diagnosis has the theoretical advantage of a rapid turnaround time and higher sensitivity than conventional microbiological methods, particularly for patients who have previously received antimicrobials. Broad-range PCR assays that identify nucleic acid sequences conserved across many bacterial species may permit the identification of bacteria previously not thought to cause PJI. Conversely, multiplex or multiassay PCR is limited to those organisms for which targeted primers are included. A rigorous definition of PJI is critical when evaluating the results of molecular diagnostic tests, given the risk of contamination at any point during the procedure. Some investigators use other microbiological tests as the primary way to define infection, to which molecular diagnostics are then compared. This practice introduces potential misclassification bias, particularly with false-positive cultures and culture-negative PJI, and limits the interpretation of some of the available data.
Synovial fluid and periprosthetic tissue.
Published studies using molecular diagnostics on synovial fluid and tissue samples have used primarily 16S rRNA PCR methods. This so-called “broad-range” approach uses PCR primers targeted at regions of the bacterial rRNA gene conserved across species. In general, this approach is limited by the inability to detect polymicrobial infection and requires an additional sequencing step for identification of the pathogen, a step which may yield an unreadable sequence in the case of polymicrobial infection if traditional sequencing methods are applied. Early studies of 16S rRNA gene PCR simply used Southern blotting to detect the presence or absence of bacterial DNA (333) but did not provide information as to the nature of the bacterium being detected. Although this study touted having no false-positive results, it was limited by the lack of a standard definition for PJI. Subsequent studies with 16S rRNA gene PCR have used restriction endonuclease analysis (334) or sequencing (335) of the amplified product for species identification. Both studies used a relatively specific diagnosis of PJI. One of these studies compared the results of PCR and culture of synovial fluid only and found a higher sensitivity for PCR (71%) than for culture on solid media and in broth (44%) for 101 patients (334). However, there was discordance between PCR and culture results in terms of the microbe detected in 17% of the samples that were positive by both techniques, which raises the possibility that some of the increased sensitivity observed for PCR may not be a true reflection of the test characteristics. Alternately, this may reflect limitations of the use of restriction endonuclease analysis for microorganism identification. Additionally, given the increased sensitivity of the more recently applied culture of synovial fluid in blood culture bottles, it is unclear how PCR would compare with synovial fluid cultured by this method. A second study using 16S rRNA gene PCR followed by sequencing examined multiple intraoperative tissue or synovial fluid specimens from 34 cases of PJI and 28 controls (335). The sensitivity for culture was 65%, compared to 91% for PCR, and concordant results were obtained for 62% of patients with PJI. These investigators reported only one PCR-positive result for the patients without PJI, suggesting a high specificity. However, a higher false-positive rate has been observed in other studies. A study of synovial fluid samples from 92 knee or hip revisions found a similarly high sensitivity of 92% but a poor specificity of only 74% (336). More recent studies have evaluated 16S rRNA gene PCR (304, 337). One study including 122 patients examined the impact of obtaining multiple specimens of synovial fluid or tissue and performing both culture and 16S rRNA gene PCR followed by sequencing (304). Those investigators found that when five samples were studied by PCR, detection of the same microorganism in two samples provided sensitivity and specificity of 94 and 100%, respectively. In comparison, the sensitivity and specificity for culture were 96 and 82%, respectively, when the same criteria were used. This suggests that it may be beneficial to test multiple specimens by PCR in order to increase the sensitivity and specificity, as is done for culture. However, the cost and labor to perform these additional PCRs may be prohibitive. Finally, Bergin and colleagues observed a 71% sensitivity and a 100% specificity for a reverse transcription-quantitative PCR of 16S rRNA in 64 patients (337). Species identification was not performed, limiting the interpretation of the results of this study.
Sonicate fluid.
Several studies have now evaluated broad-range 16S rRNA gene PCR or multiplex/multiassay PCR performed on sonicate fluid. This approach has the theoretical advantage of combining the previously observed increased sensitivity of sonication (248) with the increased sensitivity of PCR. However, broad-range PCR may be even more problematic in this setting, given the previously observed gross contamination with some sonication protocols that used bags to process prostheses (323). In one early sonication study, all of the sonicate fluids that were culture positive were also positive by 16S rRNA gene PCR (332). However, 40% of those samples that were culture negative were also positive by PCR. The implications of this finding are unclear, as a standard definition of PJI was not used in that study. A subsequent study used a modified commercially available 16S rRNA gene PCR assay on sonicate fluid (338). PCR was followed by hybridization to a nitrocellulose strip with probes specific for different species, allowing species identification without an additional sequencing step and providing the potential for detection of a polymicrobial infection. Among the 75 patients with prosthetic joints included in the study, there were 31 with clinically defined PJI. The sensitivity of PCR was 84%, modestly better than the observed 77% sensitivity for sonicate fluid culture. In contrast, the specificity of PCR was markedly lower (68%) than that of sonicate fluid culture (89%). The sensitivities for patients receiving antibiotics preoperatively were 80 and 70% for PCR and sonicate fluid culture, respectively. Finally, the largest study to date using 16S rRNA gene PCR on sonicate fluid included 366 patients (135 with PJIs) and found no difference in sensitivity (70%) or specificity (98%) between real-time 16S rRNA gene PCR performed on sonicate fluid and culture of synovial fluid, periprosthetic tissue, or sonicate fluid (339). A possible reason for the higher specificity reported in this study than in previous studies was the use of real-time PCR, which allowed those investigators use a defined crossing-point threshold for a positive PCR result, thereby decreasing the number of false-positive results. Additionally, this study made use of a specific software program to analyze mixed sequences and detect polymicrobial infection (RipSeq Mixed; Isentio AS, Bergen, Norway). Both of these advances are important considerations if 16S rRNA gene PCR is to be used on either sonicate fluid or other samples in future studies.
Multiplex or multipanel PCR assays may be more appropriate for sonicate fluid as a result of higher specificity. Two studies have used the SeptiFast (Roche Diagnostics, Basel, Switzerland) real-time multiplex PCR assay that was originally designed for detection of bloodstream infection (326, 340). This assay is not commercially available in the United States at this time. The sensitivity for PCR was 96 to 100%, compared to 59 to 67% for sonicate culture, in a total of 61 cases of PJI and 72 patients with aseptic failure. In patients taking antibiotics preoperatively, the sensitivity remained at 92 to 100% for PCR, while the sensitivity for culture dropped to 42 to 50%. However, this was a small study (47 patients) that excluded patients with PJI due to organisms not included in the panel, such as P. acnes and Corynebacterium species (326), limiting the real-world utility of this assay, particularly for shoulder arthroplasty infection. Additionally, specificity (100%) was accurately determined in only one study (86 patients), as the other study included only 10 patients without PJI (340). To address this problem, a different group of investigators designed a panel of 10 real-time PCR assays specifically targeting the bacteria that most frequently cause PJI (29). This large study, involving 434 patients (144 with PJIs), found that sonicate fluid PCR was more sensitive (77%) than tissue culture (70%) but not sonicate fluid culture (73%), compared to a nonmicrobiological definition of PJI. Conversely, the specificity of this PCR panel was high (98%), suggesting that if aseptic failure is due to indolent infections, as other investigators have suggested (341), it is not caused by organisms that commonly cause overt PJI. For the patients receiving antibiotics in the 2 weeks prior to surgery, PCR was 88% sensitive, compared to 70% sensitivity for tissue or sonicate fluid culture, suggesting a situation in which this technology may be particularly advantageous. Interestingly, there were five PJI patients with a negative PCR result who had growth of S. aureus from sonicate fluid and/or tissue cultures. The authors of that study reported that poor lysis of the particular S. aureus strains infecting these subjects, rather than inhibition, was the cause of these discordant results. Given the limitations of commercially available multiplex PCR assays designed for other purposes, multiplex PCR assays that include the most likely organisms causing PJI should be used for PJI diagnosis.
PCR electrospray ionization mass spectrometry (ESI-MS) has recently been evaluated for use with sonicate fluid and synovial fluid for the detection of PJI (342–344). This technology was commercialized by Abbott Laboratories (Abbott Park, IL) as the Plex-ID system. Using sonicate fluid, a large study of 431 patients found a significantly higher sensitivity for the Plex-ID BAC detection assay (77.6%) than for culture (69.7%) (342). This difference was even more marked among the patients who had received antimicrobials prior to surgery. However, the observed specificity was lower for the Plex-ID system (93.5%) than for culture (99.3%). The same system was used to evaluate synovial fluid; the sensitivity was numerically lower (81%) than that of synovial fluid culture (86%), and the specificity was also lower than that of culture, at 95 versus 100% (343). Abbott Laboratories no longer markets the Plex-ID PCR ESI-MS system. An earlier version of Abbott's ESI-MS platform, the Ibis T5000 Biosensor (Ibis Biosciences, Carlsbad, CA), correctly identified the pathogen in 17 of 18 culture-positive PJI cases (344). However, a very poor specificity was observed, with one or more organisms being identified in 50 of 57 noninfectious revisions and 5 of 7 primary arthroplasties, significantly limiting the application of this technology. Given these data, PCR ESI-MS may be useful in selected cases of PJI where the microbiological diagnosis remains undetermined by using conventional methods. Further refinements of this technology will hopefully improve the specificity.
TREATMENT
General Principles
Successful management of PJI requires surgical intervention and medical therapy in the majority of cases. While surgical management and immediate postoperative care occur in the hospital, in many hospitals, most of the antimicrobial treatment is given following hospital discharge. Accordingly, the best outcomes can be expected when a collaborative relationship exists between orthopedic surgeons, infectious disease physicians, nursing staff, outpatient antimicrobial therapy program coordinators, and other clinicians involved in the care of the patient.
The goals of PJI treatment are to eradicate the infection, restore pain-free function of the infected joint, and minimize PJI-related morbidity and mortality for the patient. Unfortunately, not all of these goals may be possible for every patient. The relative priorities for each individual patient for pain relief, restoration of function, avoidance of prolonged antimicrobial therapy, and unwillingness or inability to undergo surgery should be assessed and incorporated into the treatment plan.
Treatment success has been variably defined in the literature over the last 3 decades, which leads to some difficulty when making comparisons across different studies and management strategies. Death related to PJI is explicitly or implicitly included as a failure in all definitions. There was no PJI-related mortality in several large studies of exchange arthroplasty (93, 345), a mortality rate of 3 to 4% in large studies using debridement with implant retention (102, 103), and a mortality rate of 2% in large studies using different management strategies (97, 175). The PJI-related mortality rate in one large study of PJI managed with debridement with implant retention due to S. aureus was 7%, likely reflecting both the virulence of this organism and the concomitant acute onset of systemic infection (63). Some investigators simply define success as freedom from signs or symptoms of infection at the defined follow-up point, regardless of the required treatment (66, 104, 346). However, other studies are more restrictive in the definition of treatment success. Reasons for failure in other studies include the need for further revision surgery for any reason (101), additional or suppressive antimicrobials beyond the initial treatment course (125, 176), or a nonfunctional arthroplasty (67). A definition of treatment success following arthroplasty exchange has recently been proposed by an expert panel (Table 4) (347). In the associated document, success is defined as microbiological and clinical eradication of the infection without relapsed infection, freedom from subsequent surgical intervention for the same infection, and freedom from mortality related to the PJI. This paper also provides a temporal framework for treatment success. Short-term, midterm, and long-term results were defined as 2, 5, and 10 or more years after surgery, respectively. These definitions provide a guide for future investigators and may serve to unify the future body of evidence across studies. These definitions may also be useful for educating patients about the meaning and likelihood of a successful outcome prior to surgery.
TABLE 4.
Definition and classification of successful treatment of prosthetic joint infectiona
| Category | Description |
|---|---|
| Definition of successful treatment | Microbiological and clinical eradication of infection without relapsed infection |
| Freedom from subsequent surgical intervention for the same infection | |
| Freedom from mortality related to PJI | |
| Temporal classification of success | Short term (2 yr) |
| Midterm (5–10 yr) | |
| Long term (10 yr or more) |
Based on data from reference 347.
PJI can be treated by a number of different medical and surgical strategies, including open or arthroscopic debridement without removal of the prosthesis, resection of the prosthesis without reimplantation, resection of the prosthesis with reimplantation of a new prosthesis either at the time of removal (one-stage or direct arthroplasty exchange) or delayed by weeks to months (two-stage arthroplasty exchange), arthrodesis, amputation, or antimicrobial suppression without surgery. The goal of each surgical strategy is to remove all infected tissue and hardware or to decrease the burden of biofilm if any prosthetic material is retained, such that postoperative antimicrobial therapy can eradicate the remaining infection. Antibiotics should be withheld until multiple intraoperative specimens are sent for microbiological analysis, unless the patient requires antimicrobials to treat a systemic infection. The medical and surgical treatment strategies are outlined in Fig. 4 and are discussed in further detail below.
FIG 4.
Medical and surgical strategies for management of prosthetic joint infection. Outlined arrows indicate exchange of polyethylene components only, solid arrows indicate exchange of all arthroplasty components, and dotted arrows indicate exchange of cement spacer. The use of suppressive antimicrobials after DAIR or one-stage arthroplasty exchange is controversial. Management of PJI without surgery is not generally recommended. Abbreviations: DAIR, debridement, antibiotics, and implant retention; OSE, one-stage exchange; ALC, antimicrobial-loaded cement; PJI, prosthetic joint infection; IV, intravenous.
Debridement with Prosthesis Retention
Debridement with prosthesis retention is commonly referred to as a debridement, antibiotics, and implant retention (DAIR) procedure and should be performed by using open arthrotomy. The prior surgical incision is opened, followed by irrigation and debridement of any necrotic or infected soft tissue, removal of any encountered hematoma, and evacuation of any purulence surrounding the prosthesis. Debridement must be thorough and complete in order for this treatment strategy to succeed. Stability of the prosthesis is assessed intraoperatively, typically followed by removal and replacement of any exchangeable components such as the polyethylene liner or a modular femoral head. The entire joint is then aggressively irrigated and closed, typically over a drain (348, 349). Arthroscopic DAIR procedures have also been reported, but adequate debridement is more difficult, and outcomes may be suboptimal. One study found a >4-fold increase in the risk of treatment failure when arthroscopic debridement was performed compared to an open procedure (349). Open debridement should therefore be performed whenever possible.
Antimicrobial treatment with the DAIR procedure.
There is some variability in the antimicrobial treatment used in patients undergoing a DAIR procedure. For most patients, antimicrobials are held prior to surgery if the microbiology result is undetermined. Broad-spectrum therapy is typically indicated in the immediate postoperative period if the causative microorganism(s) and antimicrobial susceptibility test results are not known, given that the implant is retained. After pathogen identification and antimicrobial susceptibility are defined, antimicrobial therapy can be tailored. Most clinicians use intravenous antibiotics for the first 2 to 6 weeks following a DAIR procedure (102, 127, 348–351). Recent IDSA guidelines suggest that 4 to 6 weeks of intravenous therapy should be used with PJI due to organisms other than staphylococci or when rifampin combination therapy cannot be used (60). Antimicrobial treatment of staphylococcal PJI following a DAIR procedure is discussed below.
Many clinicians use oral antibiotic suppressive therapy for some period of time following the initial treatment course, given the difficulty in eradicating biofilm-associated organisms with retained hardware. This is supported by the finding that the risk of failure increases 4-fold after antimicrobials are stopped, with most failures occurring in the first 4 months after antimicrobials are stopped (349). Conversely, others suggest that therapy can be stopped in an asymptomatic patient with a normal CRP result and negative nuclear medicine imaging results (352). Due to false-positive nuclear medicine imaging results that may occur up to several years after revision, this is not common practice and is of uncertain value. There is debate among experts about the need for and duration of suppressive therapy (60). When suppression is used, the duration may be indefinite, or it may be limited to the initial months or the first year after surgery. High-quality data to support one particular antimicrobial strategy over another do not exist but may depend upon the virulence of the infecting pathogen, the antimicrobial therapy provided in the initial postoperative period, the antimicrobial susceptibility profile and availability of oral therapy, and the consequences if treatment failure occurs.
Selection of patients for a DAIR procedure.
Patients in whom the DAIR procedure is to be used should have a short duration of symptoms, a stable implant, and no sinus tract (60, 352–354). Ideally, the infecting pathogen should be susceptible to multiple antimicrobials (353), but this may not be known when this surgical strategy is selected. Surgery shortly after the onset of symptoms is associated with a lower likelihood of treatment failure (102, 355). Accordingly, early postoperative infections (occurring within the first month) or late acute hematogenous infections (with symptoms for <3 weeks) are most appropriate for this strategy. A well-fixed implant is necessary for adequate function following treatment of the infection. However, the presence of radiolucency surrounding the implant, in the absence of mechanical loosening, does not appear to predict treatment failure (102, 356). The presence of a sinus tract has been associated with an increased risk of treatment failure, likely reflective of the duration of symptoms and the quality of the soft tissue structures around the joint (102, 353).
There are several other notable risk factors for treatment failure. Infection with Staphylococcus species is associated with a high risk of treatment failure (82, 102, 348, 349, 351), likely driven by S. aureus (102, 349). Antimicrobial susceptibility is also important, with higher rates of failure for infection with methicillin-resistant S. aureus (MRSA) (105), vancomycin-resistant enterococci (105), and fluoroquinolone-resistant Gram-negative bacilli (172). Comorbidities, reflected by a high ASA score (351) or a compromised immune system (63, 353), may also increase the risk of treatment failure. Prior revision and arthroscopic debridement were predictive of treatment failure in one study (349).
Treatment success rates.
The treatment success rate of DAIR reported in the literature over the last 15 years ranges from 31 to 82% among infections with a variety of microorganisms (82, 102, 103, 105, 106, 348, 349, 351, 357–362). The success rate was 77% in one study of hip prosthesis infection reporting midterm results (358), but most other studies include only short-term follow-up results. Systematic reviews have found average treatment success rates of 33% for knee infection (353) and 52% for hip and knee infections (363). However, many of the studies included in these reviews likely did not include protocols using rifampin-based combination therapy, which offers benefit in PJIs caused by Staphylococcus species (350, 364), so they may not have ideally evaluated the outcome of DAIR. Overall, there does not appear to be a difference in treatment success between hip and knee arthroplasties (102, 103, 351). Treatment of shoulder arthroplasty infection using this method has been performed in a limited number of patients (103, 112, 349). While one study suggested that treatment of hip or knee PJI due to aerobic Gram-negative bacilli with a DAIR procedure is less successful than PJI due to other bacteria (175), several other studies found a success rate comparable to those for infections with other organisms (171, 365). This may be related to the use of fluoroquinolones, which appear to improve success rates with these organisms (172).
PJI due to staphylococci treated with the DAIR procedure.
Given the frequency with which staphylococci cause early-onset and late hematogenous PJIs, there has been significant work to try to define the optimal management of staphylococcal PJI treated with a DAIR procedure. A prolonged rifampin-based combination program seems to increase the cure rate when this surgical strategy is chosen, based on one small randomized controlled trial (364) and several observational studies (63, 350, 366). The combination of a fluoroquinolone and rifampin had particularly good efficacy against staphylococci in an experimental foreign-body infection model (367). The Staphylococcus species being treated as such should be susceptible to rifampin, and rifampin should not be used as monotherapy, because doing so easily selects for rifampin resistance; in addition, close attention must be paid to drug-drug interactions with this agent (368). For both S. aureus and coagulase-negative staphylococci, rifampin is typically given with an intravenous agent, most commonly a β-lactam or glycopeptide, for the initial 2 to 6 weeks. This is followed by continued rifampin combined with a fluoroquinolone to complete either a 6-month (knee) or a 3-month (hip, shoulder, and elbow) total duration of rifampin combination therapy (60). The longer duration of oral combination therapy is predicated on the often larger amount of soft tissue infection in knee arthroplasty infections. Some clinicians use a fluoroquinolone combined with rifampin even during the initial phase of therapy (63, 355, 369), a practice supported by both IDSA and International Consensus Meeting documents (60, 251). This has not been directly compared to the use of an initial period of intravenous antimicrobials. When rifampin cannot be administered, the initial period of intravenous antimicrobials should be at least 4 weeks. Among intravenous agents, cefazolin or antistaphylococcal penicillins are preferred over vancomycin for treatment of infection with methicillin-susceptible S. aureus (MSSA), based on data extrapolated from other infections with this pathogen (370). Although ceftriaxone may be an acceptable alternative in MSSA orthopedic infections (371), considerable debate continues regarding its role in the treatment of S. aureus PJI (60).
The success rate with the DAIR procedure for S. aureus appears to be lower than that for other organisms (82, 349). The largest study to date utilizing a debridement strategy for S. aureus PJI found short-term treatment success in only 55% of 345 patients using this surgical strategy (63). This study did not, however, use an algorithm-based approach for patient selection. The majority of patients (88%) received rifampin combination therapy in this study, but antimicrobial suppression after therapy was not routinely used and was in fact part of the definition of failure. More than 25% of patients failed while still receiving combination therapy, which suggests a high rate of failure, regardless of whether chronic suppression was ultimately used. Interestingly, patients with MRSA were more likely to fail during treatment, while failure in those with MSSA occurred more often after treatment, suggesting that antimicrobial suppression may be particularly important for those patients with MSSA PJI. However, the number of patients with MRSA PJI remaining at risk after treatment was very small, so it is difficult to know whether the rate of failure after treatment of these individuals would not also be significant. Other studies using combination therapy with rifampin and fluoroquinolone for S. aureus PJI have reported short-term treatment success rates ranging from 62 to 75% (355, 369), compared to a rate of 36% in an older study without rifampin (127). The short-term treatment success rate may be up to 80% when rifampin combination therapy is used in properly selected patients (125). The DAIR procedure for PJI due to coagulase-negative staphylococci is similar to that for PJI due to S. aureus, and the success rate appears to be higher than that for S. aureus PJI (102, 348, 349). Overall, existing data indicate that a DAIR procedure is an option for appropriately selected patients in whom rifampin-fluoroquinolone combination therapy is used for PJI due to staphylococci.
The treatment of PJI due to MRSA is challenging, and failure seems to be more common (103, 126) and occurs more often during antimicrobial therapy (63) than for MSSA PJI, at least in some studies. Even with the use of rifampin, small studies suggest that the short-term treatment success rates for MRSA using a DAIR protocol may be a dismal 18 to 33% (372, 373). While not available in the United States, fusidic acid appears to be a suitable companion to rifampin in place of a fluoroquinolone (373, 374). Other companion drugs that may be given with rifampin include trimethoprim-sulfamethoxazole and minocycline (368). Vancomycin remains the preferred intravenous antimicrobial for PJI due to MRSA, while daptomycin may be an option (375, 376). Animal models of MRSA foreign-body infection suggest that the addition of rifampin may be more effective than daptomycin monotherapy and may prevent the emergence of daptomycin resistance (377–379). However, there are no high-quality human studies to support this. Although prolonged use of linezolid is limited by bone marrow suppression, some studies suggest that it may be tolerated even up to several months in PJI treatment, but close monitoring of complete blood counts is recommended (380, 381).
Management after treatment failure.
Patients who fail a DAIR procedure typically ultimately undergo a two-stage arthroplasty exchange (351). In one study, only 66% of 83 patients with a DAIR procedure failure had successful eradication of knee arthroplasty infection after a single two-stage arthroplasty exchange, with 12% ultimately going on to have permanent resection, arthrodesis, or amputation (382). The authors of that study did not find any identifying factors in those patients with an ultimately successful outcome, other than a longer time period between the prior failed treatment and the two-stage arthroplasty exchange in the successful group. Another option for treatment of ongoing infection after a DAIR procedure is repeated debridement followed by chronic antimicrobial therapy. Unfortunately, the likelihood of success for a repeated DAIR procedure after prior failure is low.
One-Stage Arthroplasty Exchange
A one-stage arthroplasty exchange procedure, also referred to as a direct exchange procedure, is less frequently performed in the United States than two-stage arthroplasty exchange. Open arthrotomy and debridement are performed, followed by complete removal of the prosthesis and any PMMA present. Aggressive debridement in the hands of a highly skilled surgeon is critical to the success of this strategy. A new arthroplasty is implanted during the same procedure, typically using antimicrobial-loaded PMMA to fix the new arthroplasty in place. The choice of antimicrobials included in the PMMA is determined by the pathogen identified preoperatively or is empirical if the pathogen or its susceptibilities are unknown. The use of antimicrobials in cement for prosthesis fixation is discussed in Prevention, below.
Antimicrobial treatment with one-stage arthroplasty exchange.
There are several antimicrobial strategies used for a one-stage arthroplasty exchange. The most commonly used regimen includes 4 to 6 weeks of i.v. antibiotics, followed by 3 to 12 months of oral antibiotics (99, 383, 384). Some investigators have used only a short duration of i.v. antibiotics, limited to the immediate postoperative period, followed by oral antibiotics for 6 weeks to 6 months (93, 173, 385, 386). IDSA guidelines suggest a sequential antimicrobial program, including rifampin for PJI involving staphylococci, identical to that used with a debridement procedure (60). With other organisms, 4 to 6 weeks of intravenous or highly bioavailable oral antimicrobial therapy is recommended. Indefinite chronic antimicrobial suppression therapy is typically used, except after infection with aerobic Gram-negative bacilli treated with fluoroquinolones, in which there is some difference of opinion among experts regarding the need for long-term suppression.
Selection of patients for one-stage arthroplasty exchange.
While reported in a small number of cases in the literature on knee arthroplasty infection (387), a one-stage arthroplasty exchange is typically used only for patients with hip arthroplasty infection. Patients for whom a one-stage arthroplasty exchange is appropriate have adequate remaining bone stock, an identified pathogen that is susceptible to antimicrobials available orally and in PMMA, and surrounding soft tissue in good condition (60, 352). While most patients who require bone grafting are treated with a two-stage arthroplasty exchange, one small study reported a good outcome for those patients who were managed with one-stage arthroplasty exchange (388). More than 25% of the patients in that study also had a draining sinus and had a good result, similar to a previous study that found a high success rate for patients with a draining sinus (386). Nevertheless, patients with a sinus tract are typically treated with a two-stage arthroplasty exchange (60, 352, 354).
Treatment success rates.
In general, a one-stage arthroplasty exchange offers results comparable to those of a two-stage arthroplasty exchange and is superior to a DAIR procedure. However, there have been no randomized trials comparing these approaches, and variability between centers that perform predominately one-stage compared to two-stage arthroplasty exchanges limits comparison across studies. One large early study found a 77% success rate for hip arthroplasty infection among 583 patients (389). Other studies have found treatment success rates ranging from 84 to 100% (93, 99, 173, 362, 383, 386, 388, 390, 391). These rates are similar to those of a meta-analysis that found 87% freedom from reinfection among 375 patients undergoing one-stage arthroplasty exchanges (392). The same analysis found a 90% rate for those undergoing two-stage arthroplasty exchanges. The midterm success rate was 94% (388) and the long-term success rate was 91% (385) in several small studies of hip arthroplasty infection. One-stage exchange for shoulder arthroplasty infection resulted in short-term infection-free survival in 94 to 100% of patients in two small series of patients (114, 115). There are insufficient data on one-stage exchange in elbow arthroplasty infection.
Two-Stage Arthroplasty Exchange
A two-stage arthroplasty exchange, also referred to as a staged exchange, is considered to be the most definitive strategy in terms of infection eradication and preservation of joint function. This strategy involves at least two surgeries. In the first surgery, cultures are obtained, all infected tissue is debrided, and the components and PMMA are removed. An antimicrobial-impregnated PMMA spacer is typically implanted into the joint space prior to closure to deliver local antimicrobial therapy and maintain limb length. Pathogen-directed antimicrobial therapy is usually given intravenously for 4 to 6 weeks following the first stage. This is then followed by at least a 2- to 6-week antibiotic-free time period (101, 345), during which the patient is evaluated for any signs of ongoing infection, typically using inflammatory markers and synovial fluid aspiration. If there is evidence of ongoing infection, a repeat debridement procedure may be performed, typically followed by further antimicrobial therapy before attempted reimplantation. At the time of reimplantation, biopsy specimens are obtained for frozen-section and permanent histopathological examinations as well as culture. Frozen-section analysis allows the surgeon to assess for ongoing inflammation prior to implantation of a new prosthesis. If the result is negative, a new prosthesis is implanted, typically using antimicrobial-loaded PMMA. Patients are typically treated with intravenous antibiotics until the reimplantation cultures are finalized as negative. If reimplantation cultures are positive, antimicrobials are given for a variable amount of time.
Antimicrobial-loaded PMMA spacers.
Broadly speaking, there are two different types of spacers used during two-stage arthroplasty exchanges. Static spacers, also known as nonarticulating or block spacers, are typically handmade in the operating room in an attempt to fill the void in the bone left after removal of the prosthesis. In contrast, articulating spacers attempt to reapproximate the joint structure and provide superior range of motion and function while in place. Articulating spacers may be either commercially available preformed units or custom-molded spacers. They may be made completely of PMMA or may be a composite of PMMA, polyethylene, and metal (393, 394). Alternately, some studies have reported the use of resterilized prostheses as temporary spacers during a two-stage arthroplasty exchange (395), but this is not widely accepted (396).
Antimicrobial-loaded PMMA spacers serve two functions in a two-stage arthroplasty exchange. First, both articulating and static spacers provide mechanical support during the time in which the arthroplasty is removed. This preserves proper joint position, prevents muscle contractures, and enhances patient comfort between the first and second stages. However, complications can occur with both types of spacers, including bone loss with static spacers (397) and extensor mechanism damage and wound dehiscence with articulating spacers (398). While individual studies suggest a better functional outcome with articulating spacers (399, 400), a recent systematic review found no difference in the overall functional scores after reimplantation in knee prosthesis infection (401). However, that same review found that articulating spacers did provide a greater knee range of motion. The choice of an articulating or static spacer is a complex decision for the surgeon and is individualized to each patient.
The second function of antimicrobial-loaded PMMA spacers is to provide local antimicrobial therapy to augment systemic therapy during the time between the first and second stages. The local concentration of antimicrobials achieved at the site of infection can be much higher than that achievable with systemic therapy, without significant toxicity (402, 403). The antimicrobials must be heat stable, due to the exothermic reaction when PMMA polymerizes, and water soluble, in order to allow diffusion into the surrounding tissue (393). Two or more antimicrobials may be included in a single spacer in order to provide broad-spectrum coverage (402, 404). An aminoglycoside is often used in combination with vancomycin, even if the pathogen is known to be aminoglycoside resistant, given that the concentration of vancomycin in the synovial fluid surrounding the spacer at the time of reimplantation is more dependent on the amount of the aminoglycoside than the amount of vancomycin in the PMMA (402). While other antimicrobials, including β-lactams, macrolides, amphotericin B, and fluconazole, have been used in selected situations, vancomycin in combination with an aminoglycoside is most commonly used (96, 393, 405, 406). The amounts of antimicrobials mixed in 40 g of PMMA are typically 1 to 3 g of vancomycin and 1.2 to 4.8 g of gentamicin or tobramycin (400, 402, 406–408). It is generally accepted that spacers should use a high dose of antimicrobials, defined as at least 3.6 g of antimicrobials per 40 g of PMMA, compared to <1 g for low-dose PMMA used for prosthesis fixation (409). The use of lower-dose antimicrobial-loaded PMMA for arthroplasty implantation is discussed in Prevention, below.
Antimicrobial-loaded PMMA spacers are widely used during two-stage arthroplasty exchanges, although there are not robust data showing that they increase eradication of infection. One recent systematic review found no association between the amount of antimicrobials included in the spacer and the control of infection (410). However, this review included mainly case series data, with only one randomized trial (411). Additionally, there is concern that PMMA spacers may provide a surface for microbial adhesion that may actually be detrimental to the eradication of infection. Some investigators have suggested that antimicrobial-loaded PMMA spacers should not be used with certain microorganisms that are reported to be more persistent, such as bacteria with a small-colony-variant phenotype or fungi (130, 412). However, this suggestion is based on anecdotal experience. Until further data suggest that the mechanical benefits provided by antimicrobial-loaded PMMA spacers are outweighed by potential downsides, they will likely continue to be included as part of two-stage arthroplasty exchanges.
Antimicrobial treatment with two-stage arthroplasty exchanges.
As opposed to the DAIR or one-stage exchange procedure, combination therapy with rifampin is not typically used with two-stage arthroplasty exchanges, given that there is no retained or new hardware in place. The majority of patients receive pathogen-directed intravenous antibiotics for 4 to 6 weeks between the first and second stages. However, some centers report good outcomes with oral antibiotics administered for a similar duration (413). The need for any systemic antimicrobials has also been challenged. A two-stage arthroplasty exchange using an antibiotic-loaded PMMA spacer and no systemic antibiotics among 114 patients with hip arthroplasty resulted in an 88% midterm success rate (414). Coagulase-negative staphylococci made up nearly 50% of infections in this series, suggesting that patients in whom this is attempted might need to be carefully selected. Another small series of 30 patients reported 100% short-term success following treatment with only 5 days of postoperative intravenous antimicrobials, with “radical debridement” and reimplantation at the second stage an average of 16 weeks later (414). The successes reported in both studies are likely driven by an experienced surgeon using meticulous surgical techniques as well as by carefully timed reimplantation guided by inflammatory markers. On the other end of the antimicrobial treatment spectrum, there may be some role for antimicrobial therapy after reimplantation. One nonrandomized retrospective study found that patients with knee arthroplasty infection treated for 28 days with oral prophylactic antimicrobials following reimplantation had a numerically lower (4 versus 16%) rate of reinfection in the year after surgery (415). However, the statistical significance of this was not reported, and the number of patients was very small. In clinical practice, patients with a history of treatment failure, multiple serious comorbidities, complex arthroplasty, or limited bone stock, who may not be able to tolerate another revision surgery, or patients who have positive culture or histopathology results upon reimplantation are frequently treated with antimicrobial therapy after reimplantation. Treatment is individualized in these cases. In some cases, indefinite suppression may be administered.
Risk factors for treatment failure.
Risk factors for treatment failure following two-stage arthroplasty exchange can be broadly categorized into host-related factors, pathogen-related factors, or treatment-related factors. Local or systemic host factors with a higher risk for treatment failure or reinfection include lymphedema with knee arthroplasty infection (72), the presence of a sinus tract (416, 417), prior joint revision (345, 418), and rheumatoid arthritis (418). Culture-negative PJI and infection with MRSA have been associated with an increased risk of treatment failure (417). However, culture-negative PJI was not associated with treatment failure in a study in which the majority of patients were treated with two-stage arthroplasty exchanges (66), and some studies have not found an association between the infecting pathogen and treatment failure; notably, these studies are likely underpowered (72, 345, 419).
The overall treatment protocol, including the duration between the two stages, careful assessment for ongoing infection before reimplantation, and reimplantation microbiology results, is important in predicting treatment failure. Reimplantation within 2 weeks of resection has a low likelihood of success, particularly in patients infected with S. aureus or aerobic Gram-negative bacilli (420). Furthermore, a structured protocol where reimplantation is performed only if cultures are negative prior to the second-stage surgery may improve outcomes (421). Treatment with cefazolin (72) and the use of antibiotic-loaded PMMA upon reimplantation have each been associated with an increased likelihood of success (419) upon univariate analysis. At the time of reimplantation, patients with a positive culture from tissue or sonication of the PMMA spacer have a higher likelihood of subsequent treatment failure, regardless of symptoms at the time of reimplantation (330). However, the additional benefit of sonication of the spacer beyond tissue culture is not clear, as this process has not been evaluated in other studies. While often obtained prior to reimplantation, ESR and CRP results were not helpful in identifying persistently infected joints in one small study (100). Nevertheless, an evaluation for ongoing infection, including inflammatory markers, should be performed prior to reimplantation.
Treatment success rates.
Two-stage arthroplasty exchange is generally an effective strategy for managing PJI, with reported success rates in hip arthroplasty ranging from 87 to 100% (96, 99, 362, 407, 408, 414). A systematic review including 929 patients found a success rate of 89% (392). Long-term results of hip arthroplasty infection suggest that the success rate is nearly 90% as well (96). Knee arthroplasty infection treated with a two-stage arthroplasty exchange has a reported success rate ranging from 72 to 95% (72, 413, 417, 419, 422, 423). A separate systematic review found success rates of 82 to 100% (424). Midterm results suggest a success rate exceeding 90% for total knee infection (413). Significantly less robust data suggest similar short-term outcomes for shoulder arthroplasty infection treated with a two-stage arthroplasty exchange (112, 113, 425). Elbow arthroplasty infection remains difficult to treat even with a two-stage arthroplasty exchange, with a reported short-term success rate as low as 72% (118). This may be due to a larger number of patients with rheumatoid arthritis and greater soft tissue defects over the joint.
Infection with certain organisms may be more appropriate for two-stage arthroplasty exchanges than for other treatment strategies. Infection with Candida species or fungal organisms is more appropriate for this strategy or permanent resection rather than implant retention (238, 239, 246, 426). One study reported a success rate of 93% for infection control at short-term follow-up with 6 months of oral antifungal agents after reimplantation (238). However, this finding is in contrast to another similarly sized series that found that only two-thirds of patients undergoing resection for fungal PJI underwent reimplantation, with infection being controlled in fewer than half of them (239). This suggests that the prognosis of fungal PJI is guarded, even with two-stage arthroplasty exchange. Culture-negative PJI appears to be treated more successfully with two-stage arthroplasty exchange than with resection, based on the largest series to date, while the difference with a DAIR procedure was not significant (249). In that series, there was no difference in outcomes between patients who received narrow-spectrum therapy and those who received broad-spectrum therapy, but notably, this does not account for local broad-spectrum antimicrobial therapy from an antimicrobial-loaded PMMA spacer.
Failure after two-stage arthroplasty exchange.
Infection following prior two-stage arthroplasty exchange may be due to a relapse of infection with the prior infecting pathogen or infection with a new microorganism. One large study suggests that over two-thirds of these infections are actually new infections rather than relapses (427). This may implicate ongoing risk factors that led to development of the first PJI rather than a failure of medical or surgical therapy. The time to failure after prior two-stage arthroplasty exchange varies widely, with several large studies demonstrating median times to failure ranging from 9 months to over 3 years (72, 101, 427). Gram-positive organisms are the most common cause of infection after prior two-stage arthroplasty exchange (72, 101, 427, 428).
Options for management after prior two-stage exchange include antimicrobial suppression without surgical treatment, DAIR followed by antimicrobial suppression, repeat two-stage arthroplasty exchange, resection without reimplantation, arthrodesis, or amputation (72, 101, 428–430). As in other situations, management depends upon coexisting comorbidities, integrity of bone stock and soft tissue, and the patient's desire for and ability to undergo additional surgeries. If the patient is able and willing to attempt another two-stage arthroplasty exchange, this may be an option, but careful patient selection is critical, and data on outcomes with this strategy are very limited. Among patients who underwent a second full two-stage arthroplasty exchange, the rate of successful control of infection with preservation of the prosthesis ranged from 27 to 88% for knee and hip infections in small case series with fewer than 20 patients each (101, 429–434). Many of the other patients in these studies were treated with alternate strategies, suggesting that even when it is selectively attempted, reimplantation has an unpredictable outcome. Among those patients for whom a second two-stage arthroplasty exchange failed, the ultimate outcome was also variable and included amputation in some patients, a possibility that should be discussed with patients prior to treatment.
Arthroplasty Resection without Reimplantation
Resection without reimplantation is typically reserved as a salvage strategy to avoid amputation after prior failed treatment attempts or for patients who are not candidates for DAIR or one-stage arthroplasty exchange and cannot or do not want to undergo multiple surgeries. Alternatively, patients with other comorbidities that limit their functional abilities may elect to undergo resection without reimplantation, as a new prosthesis may not provide them with additional mobility. Some patients for whom a two-stage arthroplasty exchange is planned may ultimately not undergo reimplantation due to significant perioperative events following the first procedure or ongoing infection at the time of planned reimplantation. In this group of patients, an articulating or nonarticulating PMMA spacer may remain in place indefinitely. While typically considered a temporary measure, articulating spacers may provide reasonable function for long periods of time. In one small study of 18 patients in whom articulating spacers remained in place following hip or knee arthroplasty resection, there was freedom from infection and pain in 15 patients after a mean of 42 months (406). However, the long-term success of such a strategy is unknown.
Arthrodesis may be performed in patients following resection of a knee arthroplasty, but it is uncommonly performed in patients following hip arthroplasty resection. While some patients are able to ambulate after resection of a knee arthroplasty (435), arthrodesis may provide additional mechanical support to permit ambulation. Arthrodesis can be performed by using either an intramedullary nail or external fixation device, with limited data suggesting that external fixation may have a lower rate of successful union as well as recurrent infection (436). Resection of a hip arthroplasty, also known as a Girdlestone procedure, results in a high rate of infection control and pain relief (437, 438). However, patients are typically left with significant limb length discrepancies and need assistive devices for ambulation. A new prosthesis can potentially be placed at a later time point after the Girdlestone procedure, if deemed appropriate.
Antimicrobial treatments used following resection arthroplasty are similar to those used with a two-stage arthroplasty exchange, with most patients receiving a 4- to 6-week course of intravenous antimicrobials following resection. However, some patients may require a longer course of therapy. For example, if an infected nonunion occurs following knee arthrodesis, prolonged antimicrobial therapy may be warranted.
Amputation
Amputation is reserved for patients who have failed all other treatment options for PJI (439) or have life-threatening infections in which emergent source control is needed (440). Fortunately, amputation is a rare outcome after joint arthroplasty, performed to treat infection in only 0.1% of 18,443 primary knee arthroplasties performed in one large center (439). However, 14 to 25% of patients with failed two-stage arthroplasty exchange for knee arthroplasty infection ultimately have amputation performed (72, 101, 428, 430). These patients often require further irrigation and debridement, and only a minority are fitted with a prosthesis and regain their independence (439, 441). The duration of antimicrobial therapy depends on whether or not all infected tissue is removed. If the margin of amputation or disarticulation is separate from the infection, antimicrobials may be necessary for only 1 or 2 days in the postoperative period. However, this is not sufficient if any infected bone or soft tissue remains. For example, with long-stemmed femoral components, intramedullary osteomyelitis may remain proximal to the level of amputation. Alternately, acetabular osteomyelitis may remain after hip disarticulation. Treatment appropriate for chronic osteomyelitis may be warranted in either situation. The amount of soft tissue infection that remains must also be considered and treated appropriately.
Antimicrobial Treatment
Antimicrobial treatment alone.
One of the surgical strategies described above is typically required for treatment of PJI. However, antimicrobial therapy alone is sometimes attempted with a curative intent. Unfortunately, this often results in a delay in appropriate surgical management and confusion regarding the microbiological diagnosis. Nonsurgical management is not recommended. It should be considered only for those who are unable to undergo even a single surgical procedure (e.g., due to multiple comorbidities) or are unwilling to undergo surgery and who have a well-fixed prosthesis and infection with microorganisms that are susceptible to oral antibiotics. Such a strategy is likely to be more successful in those with early rather than delayed or chronic infection (442).
The optimal antimicrobial treatment program with a nonsurgical strategy is unknown. Typically, patients are given 4 to 6 weeks of pathogen-directed intravenous or highly bioavailable oral antimicrobials, based on antimicrobial susceptibilities determined by joint aspirate culture. This may be given as combination therapy with rifampin (442). Many patients will ultimately be placed on prolonged or indefinite oral antimicrobial suppression. The choice of the suppressive antimicrobial must take into account toxicity, oral bioavailability, cost, frequency of administration, drug interactions, and the need for ongoing therapeutic monitoring. Careful drug selection and patient counseling are particularly important, given that complications occur in >20% of patients receiving antimicrobial suppression (443).
Antimicrobial treatment of selected pathogens.
In general, antimicrobial therapy should be pathogen directed and guided by the results of antimicrobial susceptibility testing, where applicable. General principles for antimicrobial treatment apply, with priority given to the least toxic, most efficacious, narrow-spectrum antimicrobial regimen. In situations in which several agents are considered equivalent, cost and ease of administration should also be considered. In general, high-quality comparative studies to determine the optimal antimicrobial for each cause of PJI have not been done, and extrapolations from other literature must be made. Suggested agents for selected pathogens are found in Table 5. Dosing is not provided here but can be found in IDSA PJI management guidelines (http://www.idsociety.org/) (60); it should be adjusted for renal or hepatic function as applicable. With certain antimicrobials and pathogens, highly bioavailable oral antimicrobials may be an acceptable alternative to intravenous therapy and may also be more cost-effective and more acceptable to patients. When outpatient intravenous antimicrobials are administered, laboratory monitoring should be performed to evaluate for adverse drug effects, typically on a weekly basis (444). For example, a complete blood count with determination of differential, creatinine, and alanine aminotransferase values should be obtained each week for patients receiving intravenous nafcillin. Additionally, in our clinical practice, we monitor laboratory tests for patients on prolonged oral antimicrobial therapy at approximately 2, 4, 8, and 12 weeks, with yearly monitoring thereafter if the medication is well tolerated. For example, a complete blood count and differential, creatinine, potassium, and alanine aminotransferase values should be measured at these time points for patients receiving oral trimethoprim-sulfamethoxazole.
TABLE 5.
Suggested antimicrobials for treatment of PJIa
| Microorganism(s) | Preferred treatment | Alternate treatment | Combination therapyb |
|---|---|---|---|
| Methicillin-susceptible staphylococci | Cefazolin or nafcillin | Vancomycin, daptomycin, or linezolid | Rifampin for DAIR and one-stage exchange |
| Methicillin-resistant staphylococci | Vancomycin | Daptomycin or linezolid | Rifampin for DAIR and one-stage exchange |
| Penicillin-susceptible enterococci | Penicillin or ampicillin | Vancomycin, daptomycin, or linezolid | Consider aminoglycoside |
| Penicillin-resistant enterococci | Vancomycin | Daptomycin or linezolid | Consider aminoglycoside |
| Pseudomonas aeruginosa | Cefepime or meropenem | Ciprofloxacin or ceftazidime | Consider aminoglycoside or fluoroquinolone |
| Enterobacter species | Cefepime or ertapenem | Ciprofloxacin | No |
| Enterobacteriaceae | Beta-lactam or ciprofloxacin | No | |
| Beta-hemolytic streptococci | Penicillin or ceftriaxone | No | |
| Propionibacterium acnes | Penicillin or ceftriaxone | No |
All antimicrobials are to be given intravenously, except ciprofloxacin or linezolid. (Adapted from reference 60 by permission of Oxford University Press/Infectious Diseases Society of America.)
DAIR, debridement, antibiotics, and implant retention.
Selection of a Treatment Strategy
The treatment strategy is ultimately selected by the orthopedic surgeon, in conjunction with the patient, along with input from an infectious diseases physician as needed. Several authors and expert panels have suggested algorithms to help choose the appropriate treatment strategy for the individual patient (60, 352, 354, 445). These algorithms incorporate many of the criteria for selection and risk factors for failure detailed above. The main purpose of these algorithms is to identify patients who may be candidates for less intensive treatment strategies, such as DAIR or one-stage exchange procedures, rather than a two-stage arthroplasty exchange. Data suggest a higher success rate when an algorithm is followed (416, 446), although the success rate of the DAIR procedure remains at only 71% even in this setting (446). Algorithms are also helpful in identifying patients for whom permanent resection or arthrodesis, amputation, or medical therapy alone might be indicated.
PREVENTION
Identification and optimization of any modifiable risk factors prior to joint arthroplasty are central to the prevention of PJI. In diabetics, blood glucose control should be improved when possible. Smoking cessation should be strongly encouraged. Infections at other body sites should be diagnosed and managed prior to surgery. In general, the best approach is a careful, thoughtful surgery that is timed to reduce the impact of a patient's underlying risk factors.
The perioperative management of DMARDs around the time of arthroplasty implantation should be decided in conjunction with a rheumatologist, although the optimal management is not known.
Reduction of Skin Flora
Given the frequency with which S. aureus causes PJI, selective identification and decolonization of patients colonized with this organism have been proposed as a strategy to reduce surgical site infection or PJI after joint arthroplasty. Recent surgical site infection prevention guidelines recommend mupirocin nasal ointment for patients with S. aureus nasal colonization (447). However, the aggregate data on preoperative decolonization are mixed. A large, high-quality, randomized, double-blind, placebo-controlled trial demonstrated that a standard protocol of screening for S. aureus nasal colonization using PCR followed by a 5-day protocol of twice-daily nasal mupirocin and daily chlorhexidine bathing resulted in a nearly 80% reduction in deep surgical site infection across a number of different types of surgery (448). The reduction was most pronounced for patients undergoing cardiothoracic surgery, and there was a trend but no statistically significant difference in the subgroup of patients undergoing orthopedic surgery. Whether or not these results translate to a reduction in surgical site infection or PJI in joint arthroplasty, which has a low baseline rate of infection, is not clear. A similar protocol of nasal mupirocin and chlorhexidine bathing reduces nasal S. aureus colonization on the day of primary joint arthroplasty (449). It is not clear, however, whether this is effective in reducing surgical site infection or PJI. A systematic review including 19 studies using a variety of decolonization protocols in orthopedic surgeries (including joint arthroplasty) found decreases in surgical site infection ranging from 13 to 200% (450). However, this was a very heterogeneous group of studies, including studies that used universal decolonization compared to selective decolonization of patients with S. aureus colonization. A universal decolonization strategy in which screening is not performed and all patients undergo chlorhexidine bathing is another approach that avoids the logistical challenges of a targeted decolonization protocol and appears to be more successful in other settings (451). A recent Cochrane meta-analysis found no difference in surgical site infection rates between chlorhexidine bathing and placebo among >7,000 patients undergoing a variety of different orthopedic and nonorthopedic surgeries (452). This was a heterogeneous surgical population, and a number of different protocols were used. In primary joint arthroplasty, one recent nonrandomized, retrospective study found a decreased rate of surgical site infection with the use of chlorhexidine wipes the night before surgery (453). However, no difference was observed in another observational study using chlorhexidine wipes 1 h before surgery (454). Neither of these studies would be expected to result in the same reduction in bacterial burden on the skin as a more traditional 5-day decolonization protocol. The lack of a consistently observed benefit, the risk of selection of bacterial resistance to mupirocin or chlorhexidine, and the possibility of adverse reactions to either antiseptic must be considered prior to implementing this strategy.
Perioperative Antimicrobial Prophylaxis
Surgical site infection is a well-established risk factor for subsequent PJI (9, 22, 24, 26, 48), and perioperative antimicrobial prophylaxis for joint arthroplasty has been shown to reduce the risk of surgical site infection by >80% (455, 456). Many of the practices that are effective for other types of surgery apply to joint arthroplasty and are well outlined in recent surgical site infection guidelines (447). Because of its antistaphylococcal activity, availability, and cost, cefazolin is widely used, although glycopeptides have not been conclusively demonstrated to be inferior to cephalosporins and may be indicated for patients with known MRSA colonization (455). While the use of dual-antimicrobial prophylaxis with both cefazolin and vancomycin may be beneficial for patients with MRSA colonization, it does not appear to significantly decrease the incidence of surgical site infection overall (457).
Patients with a reported β-lactam allergy should be identified at the presurgical visit, and the nature and history of adverse reactions should be carefully evaluated. The majority of these patients can safely receive cefazolin for perioperative prophylaxis, reducing the use of alternate agents (458). Patients with a positive penicillin skin test or with a history compatible with a type I hypersensitivity reaction should not receive cefazolin; vancomycin or clindamycin is often used instead. When cefazolin is used, the first dose should be given within the 60 min prior to the incision in order to achieve optimal tissue concentrations, while vancomycin should be given 60 to 120 min prior (447). Adequate tissue and bone concentrations are maintained throughout surgery with a single preoperative dose, unless there is excessive blood loss or the procedure is longer than 4 h, in which case a second intraoperative dose should be given (459). A second dose of vancomycin is not necessary, unless the procedure lasts more than twice the expected half-life of the medication. Antimicrobial prophylaxis beyond 24 h postoperatively does not appear to be beneficial (460).
Perioperative antimicrobials are approached differently for patients undergoing arthroplasty revision. For patients undergoing revision for PJI, perioperative antimicrobials are typically withheld until operative cultures are obtained, unless antimicrobials are required for treatment of systemic infection (102). This is done to optimize the yield of intraoperative cultures to obtain a correct microbiological diagnosis. Administration of antimicrobials prior to revision for presumed aseptic failure may potentially decrease the detection of preoperatively occult PJI. However, data should conclusively demonstrate that the potential benefits of withholding antimicrobials outweigh the known benefits of correctly timed perioperative prophylaxis before this practice is widely adopted.
Laminar Airflow and Body Exhaust Suits
It would seem logical that creating “ultraclean” air within the operating room would decrease operative contamination and subsequent PJI, but this has not been the case. Laminar airflow, in which a positive-pressure ventilation system moves air at a uniform velocity through the operating room in either a horizontal or vertical flow pattern, results in a marked decrease in the amount of contaminated particles in the air (461). When combined with a body exhaust suit, early studies suggested a reduction in the rate of PJI in the first year after implantation (461). However, only 25% of patients in that early study received perioperative antimicrobials, and subsequent large studies have not shown a benefit when modern infection control practices are also used (17, 18, 26, 462). In fact, there was a correlation between the use of laminar airflow and body exhaust suits and subsequent revision for infection in the first 6 months among >85,000 primary arthroplasties in the New Zealand Joint Registry (462). However, these factors were not analyzed independently, and only limited multivariate analysis was performed. Overall, there do not appear to be robust data to support the use of these technologies when other more proven infection control measures are used.
Antimicrobial-Loaded PMMA at Prosthesis Implantation
The purpose of including antimicrobials in the PMMA used to secure the prosthesis is to prevent the development of infection following primary arthroplasty or aseptic revision or to give additional local antimicrobial therapy to continue treatment of established infection in arthroplasty exchanges for PJI. Smaller amounts of antimicrobials per 40 g of PMMA are used, typically 0.5 to 1 g of antimicrobials for primary arthroplasty implantation or aseptic revision and 1 to 2 g of antimicrobials for reimplantation following arthroplasty exchange for PJI (409). Commercially available products in the United States contain 0.5 to 1 g of antimicrobial per 40 g of PMMA. The decreased mechanical strength when larger amounts of antimicrobials are used (463) is not suitable for long-lasting prosthesis fixation.
In some countries, >90% of cemented primary arthroplasties are secured by using antimicrobial-loaded PMMA (6), despite a lack of high-level evidence to support the effectiveness of this practice. A meta-analysis of six nonrandomized studies found a nearly 50% reduction in deep infection among >20,000 primary or aseptic hip revision surgeries with this practice (464). However, some of the included studies did not use systemic perioperative antimicrobial prophylaxis (465). Two small, randomized modern studies using systemic antimicrobial prophylaxis found a decrease in deep infection in diabetics (466) and low-risk nondiabetics (467) undergoing primary knee arthroplasty with 2 g of cefuroxime in 40 g of PMMA. However, the rate of infection in the control arms was high in both studies, 13.5% in the diabetics and 3.1% in the nondiabetics, limiting the generalizability of these results to populations with lower rates of infection. A larger study that randomized 2,948 patients undergoing primary knee arthroplasty to receive erythromycin- and colistin-loaded PMMA or plain PMMA found no difference in the deep infection rates at 1 year (47). As acknowledged by the authors of that study, these results cannot be generalized to other, more frequently used antimicrobials. Until further data are available, the use of antimicrobial-loaded PMMA for primary prophylaxis for PJI will remain controversial (468).
Antimicrobial-loaded PMMA is used for prosthesis reimplantation in the majority of patients undergoing one-stage (93, 173, 385, 386, 388) or two-stage (128, 407, 417) arthroplasty exchanges. The data to support this practice are largely retrospective (419). There does not appear to be a lower risk of reinfection when an uncemented revision is performed for PJI (362).
Antimicrobial Prophylaxis Prior to Dental Procedures
For a number of years, the orthopedic surgery and dental communities recommended antimicrobial prophylaxis prior to dental procedures for some patients with in situ joint arthroplasties (469). This was based on anecdotal data (189, 190, 195, 196), cohort studies with small numbers of PJIs (190, 470), and extrapolation from clinical practice with endocarditis. More recent evidence from rigorous case-control studies suggests that there is no increased risk of PJI following either low- or high-risk dental procedures (24, 471). Furthermore, antimicrobial prophylaxis given before dental procedures does not decrease the risk of subsequent PJI (24). A finding that deserves special emphasis with patients is that there was a trend toward a lower risk of PJI in patients with good oral hygiene. These data have led the American Dental Association and the American Academy of Orthopedic Surgery to recommend that providers “consider changing the long-standing practice of routinely prescribing prophylactic antibiotic for patients with orthopedic implants who undergo dental procedures” (472). The available evidence does not support antimicrobial prophylaxis prior to dental procedures. Patients should instead be encouraged to maintain optimal oral hygiene through routine preventative dental visits rather than fear infection as a result of dental visits.
Antimicrobial prophylaxis is also not indicated for prevention of PJI in patients undergoing urologic or endoscopic gastrointestinal procedures. A recent case-control study found, however, that upper endoscopy with biopsy was associated with a 4-fold increase in subsequent PJI, even after multivariate adjustment for other risk factors (164). Other endoscopic procedures were not associated with an increased risk. This highlights the heterogenous nature of these procedures and suggests that the approach to prophylaxis needs to be individualized to each patient.
CONCLUSIONS AND A VIEW TO THE FUTURE
Joint arthroplasties are life-enhancing for millions of people around the world. The diagnosis and management of infections involving these devices require a specific approach, as summarized in this review. Several organizations have proposed classification schemes for PJI; it is anticipated that in the years to come, these will be refined based on emerging data. Significant advances have been made in defining the ideal approach to the diagnosis of PJI, and there are now PJI-specific diagnostic methods. Further improved diagnostics for PJI are anticipated over the years to come, and the pathogenesis of what is today referred to as “culture-negative PJI” will, hopefully, be better defined. Although large, high-quality, multi-institutional studies using a common language will ideally be necessary to more accurately identify the optimal approaches to treatment, the use of treatment algorithms available today yields overall acceptable success rates. Given the increasing numbers of individuals who will undergo joint replacement surgery in the years to come, laboratorians and clinicians should anticipate increasing numbers of PJIs. A great deal is now known about the epidemiology of PJI; future studies should use this knowledge to prospectively identify patients at high risk for infection with a view to its prevention. Finally, advances in the prevention of PJI will be needed to impact the anticipated increased number of PJI cases over the years to come.
ACKNOWLEDGMENTS
We are grateful to Douglas R. Osmon and Elie F. Berbari for thoughtful review of selected segments of the manuscript and to Tad M. Mabry for assistance with the design of Fig. 2.
R.P. is an employee of the Mayo Clinic and has the following interests to disclose: research funding/support from Astellas, Tornier, Pocared, Pradama, Pfizer, 3M, BioFire, and nanoMR; consulting for Thermo Fisher; patents for Bordetella pertussis-B. parapertussis PCR, an antibiofilm substance, and a device/method for sonication; royalties from Up-to-Date; and an editor stipend for the Journal of Clinical Microbiology. R.P. is supported by the National Institutes of Health (R01 AR 056647 and R01 AI 91594).
Biographies

Aaron Tande, M.D., received a B.A. from Macalester College in 2004 and a M.D. from the University of Minnesota Medical School in 2008. He completed his Internal Medicine residency at the Massachusetts General Hospital in Boston, MA. He is currently a Fellow in the Division of Infectious Diseases and an Instructor in Medicine at the Mayo Clinic in Rochester, MN. Following completion of his fellowship, he will be joining the faculty at the Mayo Clinic. His research interests include prosthetic joint infection and staphylococci, with a special interest in small-colony-variant staphylococci. His clinical interests include orthopedic infections and infections in patients with hematologic malignancies.

Robin Patel, M.D., graduated from Princeton University with a B.A. in 1985 and from McGill University with an M.D. in 1989. Thereafter, she completed a residency in Internal Medicine and fellowships in Clinical Microbiology and Infectious Diseases at the Mayo Clinic (Rochester, MN). In 1996, she joined the staff of the Mayo Clinic. She is currently Professor of Medicine and Professor of Microbiology, Director of the Clinical Bacteriology and the Infectious Diseases Research Laboratories, and Chair of the Division of Clinical Microbiology at the Mayo Clinic. She is board certified in Infectious Diseases (A.B.I.M.), Medical Microbiology/Public Health Microbiology (A.B.M.M.), and Medical Microbiology (A.B.P.) and is a Fellow of the American Academy of Microbiology. Her research focuses on medical biofilms, with a special interest in prosthetic joint infection. She also develops novel diagnostic assays and studies antimicrobial resistance. She has published over 250 articles and is the vice chair of the ICAAC Program Planning Committee and an associate editor for the Journal of Clinical Microbiology.
REFERENCES
- 1.Centers for Disease Control and Prevention. 2013. National hospital discharge survey: 2010 table, procedures by selected patient characteristics. Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf [Google Scholar]
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. 2007. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am. 89:780–785. 10.2106/JBJS.F.00222 [DOI] [PubMed] [Google Scholar]
- 3.Havelin LI, Fenstad AM, Salomonsson R, Mehnert F, Furnes O, Overgaard S, Pedersen AB, Herberts P, Karrholm J, Garellick G. 2009. The Nordic Arthroplasty Register Association: a unique collaboration between 3 national hip arthroplasty registries with 280,201 THRs. Acta Orthop. 80:393–401. 10.3109/17453670903039544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robertsson O, Bizjajeva S, Fenstad AM, Furnes O, Lidgren L, Mehnert F, Odgaard A, Pedersen AB, Havelin LI. 2010. Knee arthroplasty in Denmark, Norway and Sweden. Acta Orthop. 81:82–89. 10.3109/17453671003685442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. 2012. Economic burden of periprosthetic joint infection in the United States. J. Arthroplasty 27:61–65.e61. 10.1016/j.arth.2012.02.022 [DOI] [PubMed] [Google Scholar]
- 6.Dale H, Fenstad AM, Hallan G, Havelin LI, Furnes O, Overgaard S, Pedersen AB, Karrholm J, Garellick G, Pulkkinen P, Eskelinen A, Makela K, Engesaeter LB. 2012. Increasing risk of prosthetic joint infection after total hip arthroplasty. Acta Orthop. 83:449–458. 10.3109/17453674.2012.733918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsaras G, Osmon DR, Mabry T, Lahr B, St Sauveur J, Yawn B, Kurland R, Berbari EF. 2012. Incidence, secular trends, and outcomes of prosthetic joint infection: a population-based study, Olmsted county, Minnesota, 1969-2007. Infect. Control Hosp. Epidemiol. 33:1207–1212. 10.1086/668421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. 2010. Prosthetic joint infection risk after TKA in the Medicare population. Clin. Orthop. Relat. Res. 468:52–56. 10.1007/s11999-009-1013-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. 2008. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin. Orthop. Relat. Res. 466:1710–1715. 10.1007/s11999-008-0209-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh JA, Sperling JW, Schleck C, Harmsen W, Cofield RH. 2012. Periprosthetic infections after shoulder hemiarthroplasty. J. Shoulder Elbow Surg. 21:1304–1309. 10.1016/j.jse.2011.08.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van de Sande MA, Brand R, Rozing PM. 2006. Indications, complications, and results of shoulder arthroplasty. Scand. J. Rheumatol. 35:426–434. 10.1080/03009740600759720 [DOI] [PubMed] [Google Scholar]
- 12.Voloshin I, Schippert DW, Kakar S, Kaye EK, Morrey BF. 2011. Complications of total elbow replacement: a systematic review. J. Shoulder Elbow Surg. 20:158–168. 10.1016/j.jse.2010.08.026 [DOI] [PubMed] [Google Scholar]
- 13.Achermann Y, Vogt M, Spormann C, Kolling C, Remschmidt C, Wust J, Simmen B, Trampuz A. 2011. Characteristics and outcome of 27 elbow periprosthetic joint infections: results from a 14-year cohort study of 358 elbow prostheses. Clin. Microbiol. Infect. 17:432–438. 10.1111/j.1469-0691.2010.03243.x [DOI] [PubMed] [Google Scholar]
- 14.Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS. 2012. A financial analysis of revision hip arthroplasty: the economic burden in relation to the national tariff. J. Bone Joint Surg. Br. 94:619–623. 10.1302/0301-620X.94B5.27073 [DOI] [PubMed] [Google Scholar]
- 15.Peel TN, Dowsey MM, Buising KL, Liew D, Choong PF. 2013. Cost analysis of debridement and retention for management of prosthetic joint infection. Clin. Microbiol. Infect. 19:181–186. 10.1111/j.1469-0691.2011.03758.x [DOI] [PubMed] [Google Scholar]
- 16.Klouche S, Sariali E, Mamoudy P. 2010. Total hip arthroplasty revision due to infection: a cost analysis approach. Orthop. Traumatol. Surg. Res. 96:124–132. 10.1016/j.otsr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- 17.Namba RS, Inacio MC, Paxton EW. 2012. Risk factors associated with surgical site infection in 30,491 primary total hip replacements. J. Bone Joint Surg. Br. 94:1330–1338. 10.1302/0301-620X.94B10.29184 [DOI] [PubMed] [Google Scholar]
- 18.Namba RS, Inacio MC, Paxton EW. 2013. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J. Bone Joint Surg. Am. 95:775–782. 10.2106/JBJS.L.00211 [DOI] [PubMed] [Google Scholar]
- 19.Malinzak RA, Ritter MA, Berend ME, Meding JB, Olberding EM, Davis KE. 2009. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J. Arthroplasty 24:84–88. 10.1016/j.arth.2009.05.016 [DOI] [PubMed] [Google Scholar]
- 20.Dowsey MM, Choong PF. 2009. Obese diabetic patients are at substantial risk for deep infection after primary TKA. Clin. Orthop. Relat. Res. 467:1577–1581. 10.1007/s11999-008-0551-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peersman G, Laskin R, Davis J, Peterson M. 2001. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin. Orthop. Relat. Res. 392:15–23. 10.1097/00003086-200111000-00003 [DOI] [PubMed] [Google Scholar]
- 22.Peel TN, Dowsey MM, Daffy JR, Stanley PA, Choong PF, Buising KL. 2011. Risk factors for prosthetic hip and knee infections according to arthroplasty site. J. Hosp. Infect. 79:129–133. 10.1016/j.jhin.2011.06.001 [DOI] [PubMed] [Google Scholar]
- 23.Dowsey MM, Choong PF. 2008. Obesity is a major risk factor for prosthetic infection after primary hip arthroplasty. Clin. Orthop. Relat. Res. 466:153–158. 10.1007/s11999-007-0016-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berbari EF, Osmon DR, Carr A, Hanssen AD, Baddour LM, Greene D, Kupp LI, Baughan LW, Harmsen WS, Mandrekar JN, Therneau TM, Steckelberg JM, Virk A, Wilson WR. 2010. Dental procedures as risk factors for prosthetic hip or knee infection: a hospital-based prospective case-control study. Clin. Infect. Dis. 50:8–16. 10.1086/648676 [DOI] [PubMed] [Google Scholar]
- 25.Uckay I, Lubbeke A, Emonet S, Tovmirzaeva L, Stern R, Ferry T, Assal M, Bernard L, Lew D, Hoffmeyer P. 2009. Low incidence of haematogenous seeding to total hip and knee prostheses in patients with remote infections. J. Infect. 59:337–345. 10.1016/j.jinf.2009.08.015 [DOI] [PubMed] [Google Scholar]
- 26.Berbari EF, Hanssen AD, Duffy MC, Steckelberg JM, Ilstrup DM, Harmsen WS, Osmon DR. 1998. Risk factors for prosthetic joint infection: case-control study. Clin. Infect. Dis. 27:1247–1254. 10.1086/514991 [DOI] [PubMed] [Google Scholar]
- 27.Liabaud B, Patrick DA, Jr, Geller JA. 2013. Higher body mass index leads to longer operative time in total knee arthroplasty. J. Arthroplasty 28:563–565. 10.1016/j.arth.2012.07.037 [DOI] [PubMed] [Google Scholar]
- 28.Berbari EF, Osmon DR, Lahr B, Eckel-Passow JE, Tsaras G, Hanssen AD, Mabry T, Steckelberg J, Thompson R. 2012. The Mayo prosthetic joint infection risk score: implication for surgical site infection reporting and risk stratification. Infect. Control Hosp. Epidemiol. 33:774–781. 10.1086/666641 [DOI] [PubMed] [Google Scholar]
- 29.Cazanave C, Greenwood-Quaintance KE, Hanssen AD, Karau MJ, Schmidt SM, Gomez Urena EO, Mandrekar JN, Osmon DR, Lough LE, Pritt BS, Steckelberg JM, Patel R. 2013. Rapid molecular microbiologic diagnosis of prosthetic joint infection. J. Clin. Microbiol. 51:2280–2287. 10.1128/JCM.00335-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mraovic B, Suh D, Jacovides C, Parvizi J. 2011. Perioperative hyperglycemia and postoperative infection after lower limb arthroplasty. J. Diabetes Sci. Technol. 5:412–418. 10.1177/193229681100500231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seneviratne CJ, Yip JW, Chang JW, Zhang CF, Samaranayake LP. 2013. Effect of culture media and nutrients on biofilm growth kinetics of laboratory and clinical strains of Enterococcus faecalis. Arch. Oral Biol. 58:1327–1334. 10.1016/j.archoralbio.2013.06.017 [DOI] [PubMed] [Google Scholar]
- 32.Cipriano CA, Brown NM, Michael AM, Moric M, Sporer SM, Della Valle CJ. 2012. Serum and synovial fluid analysis for diagnosing chronic periprosthetic infection in patients with inflammatory arthritis. J. Bone Joint Surg. Am. 94:594–600. 10.2106/JBJS.J.01318 [DOI] [PubMed] [Google Scholar]
- 33.Bongartz T, Halligan CS, Osmon DR, Reinalda MS, Bamlet WR, Crowson CS, Hanssen AD, Matteson EL. 2008. Incidence and risk factors of prosthetic joint infection after total hip or knee replacement in patients with rheumatoid arthritis. Arthritis Rheum. 59:1713–1720. 10.1002/art.24060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ravi B, Escott B, Shah PS, Jenkinson R, Chahal J, Bogoch E, Kreder H, Hawker G. 2012. A systematic review and meta-analysis comparing complications following total joint arthroplasty for rheumatoid arthritis versus for osteoarthritis. Arthritis Rheum. 64:3839–3849. 10.1002/art.37690 [DOI] [PubMed] [Google Scholar]
- 35.Poss R, Thornhill TS, Ewald FC, Thomas WH, Batte NJ, Sledge CB. 1984. Factors influencing the incidence and outcome of infection following total joint arthroplasty. Clin. Orthop. Relat. Res. 182:117–126 [PubMed] [Google Scholar]
- 36.Jamsen E, Huhtala H, Puolakka T, Moilanen T. 2009. Risk factors for infection after knee arthroplasty. A register-based analysis of 43,149 cases. J. Bone Joint Surg. Am. 91:38–47. 10.2106/JBJS.G.01686 [DOI] [PubMed] [Google Scholar]
- 37.Kawakami K, Ikari K, Kawamura K, Tsukahara S, Iwamoto T, Yano K, Sakuma Y, Tokita A, Momohara S. 2010. Complications and features after joint surgery in rheumatoid arthritis patients treated with tumour necrosis factor-alpha blockers: perioperative interruption of tumour necrosis factor-alpha blockers decreases complications? Rheumatology 49:341–347. 10.1093/rheumatology/kep376 [DOI] [PubMed] [Google Scholar]
- 38.Momohara S, Kawakami K, Iwamoto T, Yano K, Sakuma Y, Hiroshima R, Imamura H, Masuda I, Tokita A, Ikari K. 2011. Prosthetic joint infection after total hip or knee arthroplasty in rheumatoid arthritis patients treated with nonbiologic and biologic disease-modifying antirheumatic drugs. Mod. Rheumatol. 21:469–475. 10.1007/s10165-011-0423-x [DOI] [PubMed] [Google Scholar]
- 39.Ding T, Ledingham J, Luqmani R, Westlake S, Hyrich K, Lunt M, Kiely P, Bukhari M, Abernethy R, Bosworth A, Ostor A, Gadsby K, McKenna F, Finney D, Dixey J, Deighton C. 2010. BSR and BHPR rheumatoid arthritis guidelines on safety of anti-TNF therapies. Rheumatology 49:2217–2219. 10.1093/rheumatology/keq249a [DOI] [PubMed] [Google Scholar]
- 40.Saag KG, Teng GG, Patkar NM, Anuntiyo J, Finney C, Curtis JR, Paulus HE, Mudano A, Pisu M, Elkins-Melton M, Outman R, Allison JJ, Suarez Almazor M, Bridges SL, Jr, Chatham WW, Hochberg M, MacLean C, Mikuls T, Moreland LW, O'Dell J, Turkiewicz AM, Furst DE. 2008. American College of Rheumatology 2008 recommendations for the use of nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis. Arthritis Rheum. 59:762–784. 10.1002/art.23721 [DOI] [PubMed] [Google Scholar]
- 41.Akkara Veetil BM, Bongartz T. 2012. Perioperative care for patients with rheumatic diseases. Nat. Rev. Rheumatol. 8:32–41. 10.1038/nrrheum.2011.171 [DOI] [PubMed] [Google Scholar]
- 42.Grennan DM, Gray J, Loudon J, Fear S. 2001. Methotrexate and early postoperative complications in patients with rheumatoid arthritis undergoing elective orthopaedic surgery. Ann. Rheum. Dis. 60:214–217. 10.1136/ard.60.3.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T, Ishii S. 2003. Examination of the risk of continuous leflunomide treatment on the incidence of infectious complications after joint arthroplasty in patients with rheumatoid arthritis. J. Clin. Rheumatol. 9:115–118. 10.1097/01.RHU.0000062514.54375.bd [DOI] [PubMed] [Google Scholar]
- 44.Fitzgerald RH, Jr, Nolan DR, Ilstrup DM, Van Scoy RE, Washington JA, II, Coventry MB. 1977. Deep wound sepsis following total hip arthroplasty. J. Bone Joint Surg. Am. 59:847–855 [PubMed] [Google Scholar]
- 45.Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J. 2005. Hospital resource utilization for primary and revision total hip arthroplasty. J. Bone Joint Surg. Am. 87:570–576. 10.2106/JBJS.D.02121 [DOI] [PubMed] [Google Scholar]
- 46.Ong KL, Kurtz SM, Lau E, Bozic KJ, Berry DJ, Parvizi J. 2009. Prosthetic joint infection risk after total hip arthroplasty in the Medicare population. J. Arthroplasty 24:105–109. 10.1016/j.arth.2009.04.027 [DOI] [PubMed] [Google Scholar]
- 47.Hinarejos P, Guirro P, Leal J, Montserrat F, Pelfort X, Sorli ML, Horcajada JP, Puig L. 2013. The use of erythromycin and colistin-loaded cement in total knee arthroplasty does not reduce the incidence of infection: a prospective randomized study in 3000 knees. J. Bone Joint Surg. Am. 95:769–774. 10.2106/JBJS.L.00901 [DOI] [PubMed] [Google Scholar]
- 48.Aslam S, Reitman C, Darouiche RO. 2010. Risk factors for subsequent diagnosis of prosthetic joint infection. Infect. Control Hosp. Epidemiol. 31:298–301. 10.1086/650756 [DOI] [PubMed] [Google Scholar]
- 49.Stahelova A, Mrazek F, Smizansky M, Petrek M, Gallo J. 2012. Variation in the IL1B, TNF and IL6 genes and individual susceptibility to prosthetic joint infection. BMC Immunol. 13:25. 10.1186/1471-2172-13-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Innerhofer P, Klingler A, Klimmer C, Fries D, Nussbaumer W. 2005. Risk for postoperative infection after transfusion of white blood cell-filtered allogeneic or autologous blood components in orthopedic patients undergoing primary arthroplasty. Transfusion 45:103–110. 10.1111/j.1537-2995.2005.04149.x [DOI] [PubMed] [Google Scholar]
- 51.Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, Cremers S, Abraham IL. 2003. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion 43:459–469. 10.1046/j.1537-2995.2003.00348.x [DOI] [PubMed] [Google Scholar]
- 52.Southwood RT, Rice JL, McDonald PJ, Hakendorf PH, Rozenbilds MA. 1985. Infection in experimental hip arthroplasties. J. Bone Joint Surg. Br. 67:229–231 [DOI] [PubMed] [Google Scholar]
- 53.Glynn MK, Sheehan JM. 1984. The significance of asymptomatic bacteriuria in patients undergoing hip/knee arthroplasty. Clin. Orthop. Relat. Res. 185:151–154 [PubMed] [Google Scholar]
- 54.Gou W, Chen J, Jia Y, Wang Y. 3 September 2013, posting date Preoperative asymptomatic leucocyturia and early prosthetic joint infections in patients undergoing joint arthroplasty. J. Arthroplasty [Epub ahead of print.] 10.1016/j.arth.2013.07.028 [DOI] [PubMed] [Google Scholar]
- 55.Cordero-Ampuero J, Gonzalez-Fernandez E, Martinez-Velez D, Esteban J. 2013. Are antibiotics necessary in hip arthroplasty with asymptomatic bacteriuria? Seeding risk with/without treatment. Clin. Orthop. Relat. Res. 471:3822–3829. 10.1007/s11999-013-2868-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Piper KE, Jacobson MJ, Cofield RH, Sperling JW, Sanchez-Sotelo J, Osmon DR, McDowell A, Patrick S, Steckelberg JM, Mandrekar JN, Fernandez Sampedro M, Patel R. 2009. Microbiologic diagnosis of prosthetic shoulder infection by use of implant sonication. J. Clin. Microbiol. 47:1878–1884. 10.1128/JCM.01686-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peel TN, Cheng AC, Buising KL, Choong PF. 2012. Microbiological aetiology, epidemiology, and clinical profile of prosthetic joint infections: are current antibiotic prophylaxis guidelines effective? Antimicrob. Agents Chemother. 56:2386–2391. 10.1128/AAC.06246-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Duff GP, Lachiewicz PF, Kelley SS. 1996. Aspiration of the knee joint before revision arthroplasty. Clin. Orthop. Relat. Res. 331:132–139. 10.1097/00003086-199610000-00018 [DOI] [PubMed] [Google Scholar]
- 59.Sendi P, Banderet F, Graber P, Zimmerli W. 2011. Clinical comparison between exogenous and haematogenous periprosthetic joint infections caused by Staphylococcus aureus. Clin. Microbiol. Infect. 17:1098–1100. 10.1111/j.1469-0691.2011.03510.x [DOI] [PubMed] [Google Scholar]
- 60.Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR. 2013. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 56(1):e1–e25. 10.1093/cid/cis803 [DOI] [PubMed] [Google Scholar]
- 61.Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG. 2011. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin. Orthop. Relat. Res. 469:2992–2994. 10.1007/s11999-011-2102-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Oussedik S, Gould K, Stockley I, Haddad FS. 2012. Defining peri-prosthetic infection: do we have a workable gold standard? J. Bone Joint Surg. Br. 94:1455–1456. 10.1302/0301-620X.94B11.30244 [DOI] [PubMed] [Google Scholar]
- 63.Lora-Tamayo J, Murillo O, Iribarren JA, Soriano A, Sanchez-Somolinos M, Baraia-Etxaburu JM, Rico A, Palomino J, Rodriguez-Pardo D, Horcajada JP, Benito N, Bahamonde A, Granados A, del Toro MD, Cobo J, Riera M, Ramos A, Jover-Saenz A, Ariza J. 2013. A large multicenter study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin. Infect. Dis. 56:182–194. 10.1093/cid/cis746 [DOI] [PubMed] [Google Scholar]
- 64.Tseng SW, Chi CY, Chou CH, Wang YJ, Liao CH, Ho CM, Lin PC, Ho MW, Wang JH. 2012. Eight years experience in treatment of prosthetic joint infections at a teaching hospital in Central Taiwan. J. Microbiol. Immunol. Infect. 45:363–369. 10.1016/j.jmii.2011.12.014 [DOI] [PubMed] [Google Scholar]
- 65.Magnuson JE, Brown ML, Hauser MF, Berquist TH, Fitzgerald RH, Jr, Klee GG. 1988. In-111-labeled leukocyte scintigraphy in suspected orthopedic prosthesis infection: comparison with other imaging modalities. Radiology 168:235–239 [DOI] [PubMed] [Google Scholar]
- 66.Malekzadeh D, Osmon DR, Lahr BD, Hanssen AD, Berbari EF. 2010. Prior use of antimicrobial therapy is a risk factor for culture-negative prosthetic joint infection. Clin. Orthop. Relat. Res. 468:2039–2045. 10.1007/s11999-010-1338-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tsukayama DT, Estrada R, Gustilo RB. 1996. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections. J. Bone Joint Surg. Am. 78:512–523 [DOI] [PubMed] [Google Scholar]
- 68.Tsukayama DT, Goldberg VM, Kyle R. 2003. Diagnosis and management of infection after total knee arthroplasty. J. Bone Joint Surg. Am. 85(Suppl 1):S75–S80 http://jbjs.org/article.aspx?articleid=26124 [DOI] [PubMed] [Google Scholar]
- 69.McPherson EJ, Tontz W, Jr, Patzakis M, Woodsome C, Holtom P, Norris L, Shufelt C. 1999. Outcome of infected total knee utilizing a staging system for prosthetic joint infection. Am. J. Orthop. 28:161–165 [PubMed] [Google Scholar]
- 70.McPherson EJ, Woodson C, Holtom P, Roidis N, Shufelt C, Patzakis M. 2002. Periprosthetic total hip infection: outcomes using a staging system. Clin. Orthop. Relat. Res. 403:8–15. 10.1097/00003086-200210000-00003 [DOI] [PubMed] [Google Scholar]
- 71.Cierny G, III, Mader JT, Penninck JJ. 2003. A clinical staging system for adult osteomyelitis. Clin. Orthop. Relat. Res. 414:7–24. 10.1097/01.blo.0000088564.81746.62 [DOI] [PubMed] [Google Scholar]
- 72.Kubista B, Hartzler RU, Wood CM, Osmon DR, Hanssen AD, Lewallen DG. 2012. Reinfection after two-stage revision for periprosthetic infection of total knee arthroplasty. Int. Orthop. 36:65–71. 10.1007/s00264-011-1267-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murdoch DR, Roberts SA, Fowler VG, Jr, Shah MA, Taylor SL, Morris AJ, Corey GR. 2001. Infection of orthopedic prostheses after Staphylococcus aureus bacteremia. Clin. Infect. Dis. 32:647–649. 10.1086/318704 [DOI] [PubMed] [Google Scholar]
- 74.Sendi P, Banderet F, Graber P, Zimmerli W. 2011. Periprosthetic joint infection following Staphylococcus aureus bacteremia. J. Infect. 63:17–22. 10.1016/j.jinf.2011.05.005 [DOI] [PubMed] [Google Scholar]
- 75.Tande AJ, Palraj B, Berbari E, Osmon D, Steckelberg J, Wilson WR, Sohail MR. 2013. Occult prosthetic joint infection (PJI) is rare in patients with Staphylococcus aureus bacteremia (SAB), abstr 814. Abstr. IDWeek 2013. [DOI] [PubMed] [Google Scholar]
- 76.Fowler VG, Jr, Olsen MK, Corey GR, Woods CW, Cabell CH, Reller LB, Cheng AC, Dudley T, Oddone EZ. 2003. Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch. Intern. Med. 163:2066–2072. 10.1001/archinte.163.17.2066 [DOI] [PubMed] [Google Scholar]
- 77.Lautenschlager S, Herzog C, Zimmerli W. 1993. Course and outcome of bacteremia due to Staphylococcus aureus: evaluation of different clinical case definitions. Clin. Infect. Dis. 16:567–573. 10.1093/clind/16.4.567 [DOI] [PubMed] [Google Scholar]
- 78.Ghanem GA, Boktour M, Warneke C, Pham-Williams T, Kassis C, Bahna P, Aboufaycal H, Hachem R, Raad I. 2007. Catheter-related Staphylococcus aureus bacteremia in cancer patients: high rate of complications with therapeutic implications. Medicine (Baltimore) 86:54–60. 10.1097/MD.0b013e318030d344 [DOI] [PubMed] [Google Scholar]
- 79.Lee J, Kang CI, Lee JH, Joung M, Moon S, Wi YM, Chung DR, Ha CW, Song JH, Peck KR. 2010. Risk factors for treatment failure in patients with prosthetic joint infections. J. Hosp. Infect. 75:273–276. 10.1016/j.jhin.2010.03.012 [DOI] [PubMed] [Google Scholar]
- 80.Rodriguez D, Pigrau C, Euba G, Cobo J, Garcia-Lechuz J, Palomino J, Riera M, Del Toro MD, Granados A, Ariza X. 2010. Acute haematogenous prosthetic joint infection: prospective evaluation of medical and surgical management. Clin. Microbiol. Infect. 16:1789–1795. 10.1111/j.1469-0691.2010.03157.x [DOI] [PubMed] [Google Scholar]
- 81.Chodos MD, Johnson CA. 2009. Hematogenous infection of a total knee arthroplasty with Klebsiella pneumoniae in association with occult adenocarcinoma of the cecum. J. Arthroplasty 24:158.e9–158.e13. 10.1016/j.arth.2007.12.018 [DOI] [PubMed] [Google Scholar]
- 82.Konigsberg BS, Valle CJ, Ting NT, Qiu F, Sporer SM. 3 September 2013, posting date Acute hematogenous infection following total hip and knee arthroplasty. J. Arthroplasty [Epub ahead of print.] 10.1016/j.arth.2013.07.021 [DOI] [PubMed] [Google Scholar]
- 83.Maniloff G, Greenwald R, Laskin R, Singer C. 1987. Delayed postbacteremic prosthetic joint infection. Clin. Orthop. Relat. Res. 223:194–197 [PubMed] [Google Scholar]
- 84.Donlan RM, Costerton JW. 2002. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 15:167–193. 10.1128/CMR.15.2.167-193.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Molina-Manso D, del Prado G, Ortiz-Perez A, Manrubia-Cobo M, Gomez-Barrena E, Cordero-Ampuero J, Esteban J. 2013. In vitro susceptibility to antibiotics of staphylococci in biofilms isolated from orthopaedic infections. Int. J. Antimicrob. Agents 41:521–523. 10.1016/j.ijantimicag.2013.02.018 [DOI] [PubMed] [Google Scholar]
- 86.del Pozo JL, Patel R. 2007. The challenge of treating biofilm-associated bacterial infections. Clin. Pharmacol. Ther. 82:204–209. 10.1038/sj.clpt.6100247 [DOI] [PubMed] [Google Scholar]
- 87.Stoodley P, Nistico L, Johnson S, Lasko LA, Baratz M, Gahlot V, Ehrlich GD, Kathju S. 2008. Direct demonstration of viable Staphylococcus aureus biofilms in an infected total joint arthroplasty. A case report. J. Bone Joint Surg. Am. 90:1751–1758. 10.2106/JBJS.G.00838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Galdbart JO, Allignet J, Tung HS, Ryden C, El Solh N. 2000. Screening for Staphylococcus epidermidis markers discriminating between skin-flora strains and those responsible for infections of joint prostheses. J. Infect. Dis. 182:351–355. 10.1086/315660 [DOI] [PubMed] [Google Scholar]
- 89.Nilsdotter-Augustinsson A, Koskela A, Ohman L, Soderquist B. 2007. Characterization of coagulase-negative staphylococci isolated from patients with infected hip prostheses: use of phenotypic and genotypic analyses, including tests for the presence of the ica operon. Eur. J. Clin. Microbiol. Infect. Dis. 26:255–265. 10.1007/s10096-007-0281-9 [DOI] [PubMed] [Google Scholar]
- 90.Frank KL, Hanssen AD, Patel R. 2004. icaA is not a useful diagnostic marker for prosthetic joint infection. J. Clin. Microbiol. 42:4846–4849. 10.1128/JCM.42.10.4846-4849.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Belmatoug N, Cremieux AC, Bleton R, Volk A, Saleh-Mghir A, Grossin M, Garry L, Carbon C. 1996. A new model of experimental prosthetic joint infection due to methicillin-resistant Staphylococcus aureus: a microbiologic, histopathologic, and magnetic resonance imaging characterization. J. Infect. Dis. 174:414–417. 10.1093/infdis/174.2.414 [DOI] [PubMed] [Google Scholar]
- 92.Cremieux AC, Carbon C. 1997. Experimental models of bone and prosthetic joint infections. Clin. Infect. Dis. 25:1295–1302. 10.1086/516135 [DOI] [PubMed] [Google Scholar]
- 93.Raut VV, Siney PD, Wroblewski BM. 1995. One-stage revision of total hip arthroplasty for deep infection. Long-term followup. Clin. Orthop. Relat. Res. 321:202–207 [PubMed] [Google Scholar]
- 94.Schafer P, Fink B, Sandow D, Margull A, Berger I, Frommelt L. 2008. Prolonged bacterial culture to identify late periprosthetic joint infection: a promising strategy. Clin. Infect. Dis. 47:1403–1409. 10.1086/592973 [DOI] [PubMed] [Google Scholar]
- 95.Shukla SK, Ward JP, Jacofsky MC, Sporer SM, Paprosky WG, Della Valle CJ. 2010. Perioperative testing for persistent sepsis following resection arthroplasty of the hip for periprosthetic infection. J. Arthroplasty 25:87–91. 10.1016/j.arth.2010.05.006 [DOI] [PubMed] [Google Scholar]
- 96.Biring GS, Kostamo T, Garbuz DS, Masri BA, Duncan CP. 2009. Two-stage revision arthroplasty of the hip for infection using an interim articulated Prostalac hip spacer: a 10- to 15-year follow-up study. J. Bone Joint Surg. Br. 91:1431–1437. 10.1302/0301-620X.91B11.22026 [DOI] [PubMed] [Google Scholar]
- 97.Bengtson S, Knutson K. 1991. The infected knee arthroplasty. A 6-year follow-up of 357 cases. Acta Orthop. Scand. 62:301–311 [DOI] [PubMed] [Google Scholar]
- 98.Kim YH, Choi Y, Kim JS. 2011. Treatment based on the type of infected TKA improves infection control. Clin. Orthop. Relat. Res. 469:977–984. 10.1007/s11999-010-1425-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Klouche S, Leonard P, Zeller V, Lhotellier L, Graff W, Leclerc P, Mamoudy P, Sariali E. 2012. Infected total hip arthroplasty revision: one- or two-stage procedure? Orthop. Traumatol. Surg. Res. 98:144–150. 10.1016/j.otsr.2011.08.018 [DOI] [PubMed] [Google Scholar]
- 100.Kusuma SK, Ward J, Jacofsky M, Sporer SM, Della Valle CJ. 2011. What is the role of serological testing between stages of two-stage reconstruction of the infected prosthetic knee? Clin. Orthop. Relat. Res. 469:1002–1008. 10.1007/s11999-010-1619-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mahmud T, Lyons MC, Naudie DD, Macdonald SJ, McCalden RW. 2012. Assessing the gold standard: a review of 253 two-stage revisions for infected TKA. Clin. Orthop. Relat. Res. 470:2730–2736. 10.1007/s11999-012-2358-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Marculescu CE, Berbari EF, Hanssen AD, Steckelberg JM, Harmsen SW, Mandrekar JN, Osmon DR. 2006. Outcome of prosthetic joint infections treated with debridement and retention of components. Clin. Infect. Dis. 42:471–478. 10.1086/499234 [DOI] [PubMed] [Google Scholar]
- 103.Cobo J, Miguel LG, Euba G, Rodriguez D, Garcia-Lechuz JM, Riera M, Falgueras L, Palomino J, Benito N, del Toro MD, Pigrau C, Ariza J. 2011. Early prosthetic joint infection: outcomes with debridement and implant retention followed by antibiotic therapy. Clin. Microbiol. Infect. 17:1632–1637. 10.1111/j.1469-0691.2010.03333.x [DOI] [PubMed] [Google Scholar]
- 104.Peel TN, Cheng AC, Choong PF, Buising KL. 2012. Early onset prosthetic hip and knee joint infection: treatment and outcomes in Victoria, Australia. J. Hosp. Infect. 82:248–253. 10.1016/j.jhin.2012.09.005 [DOI] [PubMed] [Google Scholar]
- 105.Soriano A, Garcia S, Bori G, Almela M, Gallart X, Macule F, Sierra J, Martinez JA, Suso S, Mensa J. 2006. Treatment of acute post-surgical infection of joint arthroplasty. Clin. Microbiol. Infect. 12:930–933. 10.1111/j.1469-0691.2006.01463.x [DOI] [PubMed] [Google Scholar]
- 106.Westberg M, Grogaard B, Snorrason F. 2012. Early prosthetic joint infections treated with debridement and implant retention: 38 primary hip arthroplasties prospectively recorded and followed for median 4 years. Acta Orthop. 83:227–232. 10.3109/17453674.2012.678801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Puig-Verdie L, Alentorn-Geli E, Gonzalez-Cuevas A, Sorli L, Salvado M, Alier A, Pelfort X, Portillo ME, Horcajada JP. 2013. Implant sonication increases the diagnostic accuracy of infection in patients with delayed, but not early, orthopaedic implant failure. Bone Joint J. 95-B:244–249. 10.1302/0301-620X.95B2.30486 [DOI] [PubMed] [Google Scholar]
- 108.Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ. 2006. The incidence of deep prosthetic infections in a specialist orthopaedic hospital: a 15-year prospective survey. J. Bone Joint Surg. Br. 88:943–948. 10.1302/0301-620X.88B7.17150 [DOI] [PubMed] [Google Scholar]
- 109.Vilchez F, Martinez-Pastor JC, Garcia-Ramiro S, Bori G, Tornero E, Garcia E, Mensa J, Soriano A. 2011. Efficacy of debridement in hematogenous and early post-surgical prosthetic joint infections. Int. J. Artif. Organs 34:863–869. 10.5301/ijao.5000029 [DOI] [PubMed] [Google Scholar]
- 110.Coste JS, Reig S, Trojani C, Berg M, Walch G, Boileau P. 2004. The management of infection in arthroplasty of the shoulder. J. Bone Joint Surg. Br. 86:65–69. 10.1302/0301-620X.86B1.14089 [DOI] [PubMed] [Google Scholar]
- 111.Cuff DJ, Virani NA, Levy J, Frankle MA, Derasari A, Hines B, Pupello DR, Cancio M, Mighell M. 2008. The treatment of deep shoulder infection and glenohumeral instability with debridement, reverse shoulder arthroplasty and postoperative antibiotics. J. Bone Joint Surg. Br. 90:336–342. 10.1302/0301-620X.90B3.19408 [DOI] [PubMed] [Google Scholar]
- 112.Sperling JW, Kozak TK, Hanssen AD, Cofield RH. 2001. Infection after shoulder arthroplasty. Clin. Orthop. Relat. Res. 382:206–216. 10.1097/00003086-200101000-00028 [DOI] [PubMed] [Google Scholar]
- 113.Sabesan VJ, Ho JC, Kovacevic D, Iannotti JP. 2011. Two-stage reimplantation for treating prosthetic shoulder infections. Clin. Orthop. Relat. Res. 469:2538–2543. 10.1007/s11999-011-1774-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Klatte TO, Junghans K, Al-Khateeb H, Rueger JM, Gehrke T, Kendoff D, Neumann J. 2013. Single-stage revision for peri-prosthetic shoulder infection: outcomes and results. Bone Joint J. 95-B:391–395. 10.1302/0301-620X.95B3.30134 [DOI] [PubMed] [Google Scholar]
- 115.Ince A, Seemann K, Frommelt L, Katzer A, Loehr JF. 2005. One-stage exchange shoulder arthroplasty for peri-prosthetic infection. J. Bone Joint Surg. Br. 87:814–818. 10.1302/0301-620X.87B6.15920 [DOI] [PubMed] [Google Scholar]
- 116.Verhelst L, Stuyck J, Bellemans J, Debeer P. 2011. Resection arthroplasty of the shoulder as a salvage procedure for deep shoulder infection: does the use of a cement spacer improve outcome? J. Shoulder Elbow Surg. 20:1224–1233. 10.1016/j.jse.2011.02.003 [DOI] [PubMed] [Google Scholar]
- 117.Vergidis P, Greenwood-Quaintance KE, Sanchez-Sotelo J, Morrey BF, Steinmann SP, Karau MJ, Osmon DR, Mandrekar JN, Steckelberg JM, Patel R. 2011. Implant sonication for the diagnosis of prosthetic elbow infection. J. Shoulder Elbow Surg. 20:1275–1281. 10.1016/j.jse.2011.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cheung EV, Adams RA, Morrey BF. 2008. Reimplantation of a total elbow prosthesis following resection arthroplasty for infection. J. Bone Joint Surg. Am. 90:589–594. 10.2106/JBJS.F.00829 [DOI] [PubMed] [Google Scholar]
- 119.Yamaguchi K, Adams RA, Morrey BF. 1998. Infection after total elbow arthroplasty. J. Bone Joint Surg. Am. 80:481–491 [DOI] [PubMed] [Google Scholar]
- 120.Spormann C, Achermann Y, Simmen BR, Schwyzer HK, Vogt M, Goldhahn J, Kolling C. 2012. Treatment strategies for periprosthetic infections after primary elbow arthroplasty. J. Shoulder Elbow Surg. 21:992–1000. 10.1016/j.jse.2011.10.007 [DOI] [PubMed] [Google Scholar]
- 121.Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. 2004. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin. Infect. Dis. 39:309–317. 10.1086/421946 [DOI] [PubMed] [Google Scholar]
- 122.Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ. 2002. Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann. Intern. Med. 137:791–797. 10.7326/0003-4819-137-10-200211190-00007 [DOI] [PubMed] [Google Scholar]
- 123.Jensen AG, Wachmann CH, Poulsen KB, Espersen F, Scheibel J, Skinhoj P, Frimodt-Moller N. 1999. Risk factors for hospital-acquired Staphylococcus aureus bacteremia. Arch. Intern. Med. 159:1437–1444. 10.1001/archinte.159.13.1437 [DOI] [PubMed] [Google Scholar]
- 124.Jacobsson G, Dashti S, Wahlberg T, Andersson R. 2007. The epidemiology of and risk factors for invasive Staphylococcus aureus infections in western Sweden. Scand. J. Infect. Dis. 39:6–13. 10.1080/00365540600810026 [DOI] [PubMed] [Google Scholar]
- 125.Senneville E, Joulie D, Legout L, Valette M, Dezeque H, Beltrand E, Rosele B, d'Escrivan T, Loiez C, Caillaux M, Yazdanpanah Y, Maynou C, Migaud H. 2011. Outcome and predictors of treatment failure in total hip/knee prosthetic joint infections due to Staphylococcus aureus. Clin. Infect. Dis. 53:334–340. 10.1093/cid/cir402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Salgado CD, Dash S, Cantey JR, Marculescu CE. 2007. Higher risk of failure of methicillin-resistant Staphylococcus aureus prosthetic joint infections. Clin. Orthop. Relat. Res. 461:48–53. 10.1097/BLO.0b013e3181123d4e [DOI] [PubMed] [Google Scholar]
- 127.Brandt CM, Sistrunk WW, Duffy MC, Hanssen AD, Steckelberg JM, Ilstrup DM, Osmon DR. 1997. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin. Infect. Dis. 24:914–919. 10.1093/clinids/24.5.914 [DOI] [PubMed] [Google Scholar]
- 128.Brandt CM, Duffy MC, Berbari EF, Hanssen AD, Steckelberg JM, Osmon DR. 1999. Staphylococcus aureus prosthetic joint infection treated with prosthesis removal and delayed reimplantation arthroplasty. Mayo Clin. Proc. 74:553–558. 10.4065/74.6.553 [DOI] [PubMed] [Google Scholar]
- 129.Joulie D, Girard J, Mares O, Beltrand E, Legout L, Dezeque H, Migaud H, Senneville E. 2011. Factors governing the healing of Staphylococcus aureus infections following hip and knee prosthesis implantation: a retrospective study of 95 patients. Orthop. Traumatol. Surg. Res. 97:685–692. 10.1016/j.otsr.2011.05.013 [DOI] [PubMed] [Google Scholar]
- 130.Sendi P, Rohrbach M, Graber P, Frei R, Ochsner PE, Zimmerli W. 2006. Staphylococcus aureus small colony variants in prosthetic joint infection. Clin. Infect. Dis. 43:961–967. 10.1086/507633 [DOI] [PubMed] [Google Scholar]
- 131.Harris LG, El-Bouri K, Johnston S, Rees E, Frommelt L, Siemssen N, Christner M, Davies AP, Rohde H, Mack D. 2010. Rapid identification of staphylococci from prosthetic joint infections using MALDI-TOF mass-spectrometry. Int. J. Artif. Organs 33:568–574 http://www.artificial-organs.com/article/rapid-identification-of-staphylococci-from-prosthetic-joint-infections-using-maldi-tof-mass-spectrometry-ijao-10-00002 [DOI] [PubMed] [Google Scholar]
- 132.Fey PD, Olson ME. 2010. Current concepts in biofilm formation of Staphylococcus epidermidis. Future Microbiol. 5:917–933. 10.2217/fmb.10.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vuong C, Durr M, Carmody AB, Peschel A, Klebanoff SJ, Otto M. 2004. Regulated expression of pathogen-associated molecular pattern molecules in Staphylococcus epidermidis: quorum-sensing determines pro-inflammatory capacity and production of phenol-soluble modulins. Cell. Microbiol. 6:753–759. 10.1111/j.1462-5822.2004.00401.x [DOI] [PubMed] [Google Scholar]
- 134.Razonable RR, Lewallen DG, Patel R, Osmon DR. 2001. Vertebral osteomyelitis and prosthetic joint infection due to Staphylococcus simulans. Mayo Clin. Proc. 76:1067–1070. 10.4065/76.10.1067 [DOI] [PubMed] [Google Scholar]
- 135.Allignet J, Galdbart JO, Morvan A, Dyke KG, Vaudaux P, Aubert S, Desplaces N, el Solh N. 1999. Tracking adhesion factors in Staphylococcus caprae strains responsible for human bone infections following implantation of orthopaedic material. Microbiology 145(Part 8):2033–2042 [DOI] [PubMed] [Google Scholar]
- 136.Sampathkumar P, Osmon DR, Cockerill FR., III 2000. Prosthetic joint infection due to Staphylococcus lugdunensis. Mayo Clin. Proc. 75:511–512. 10.1016/S0025-6196(11)64220-1 [DOI] [PubMed] [Google Scholar]
- 137.Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, Beach M. 2001. Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin. Infect. Dis. 32(Suppl 2):S114–S132. 10.1086/320184 [DOI] [PubMed] [Google Scholar]
- 138.Tan TY, Ng SY, He J. 2008. Microbiological characteristics, presumptive identification, and antibiotic susceptibilities of Staphylococcus lugdunensis. J. Clin. Microbiol. 46:2393–2395. 10.1128/JCM.00740-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Mateo M, Maestre JR, Aguilar L, Cafini F, Puente P, Sanchez P, Alou L, Gimenez MJ, Prieto J. 2005. Genotypic versus phenotypic characterization, with respect to susceptibility and identification, of 17 clinical isolates of Staphylococcus lugdunensis. J. Antimicrob. Chemother. 56:287–291. 10.1093/jac/dki227 [DOI] [PubMed] [Google Scholar]
- 140.Murdoch DR, Everts RJ, Chambers ST, Cowan IA. 1996. Vertebral osteomyelitis due to Staphylococcus lugdunensis. J. Clin. Microbiol. 34:993–994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Patel R, Piper KE, Rouse MS, Uhl JR, Cockerill FR, III, Steckelberg JM. 2000. Frequency of isolation of Staphylococcus lugdunensis among staphylococcal isolates causing endocarditis: a 20-year experience. J. Clin. Microbiol. 38:4262–4263 http://jcm.asm.org/content/38/11/4262.long [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Shah NB, Osmon DR, Fadel H, Patel R, Kohner PC, Steckelberg JM, Mabry T, Berbari EF. 2010. Laboratory and clinical characteristics of Staphylococcus lugdunensis prosthetic joint infections. J. Clin. Microbiol. 48:1600–1603. 10.1128/JCM.01769-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.van der Mee-Marquet N, Achard A, Mereghetti L, Danton A, Minier M, Quentin R. 2003. Staphylococcus lugdunensis infections: high frequency of inguinal area carriage. J. Clin. Microbiol. 41:1404–1409. 10.1128/JCM.41.4.1404-1409.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Weightman NC, Allerton KE, France J. 2000. Bone and prosthetic joint infection with Staphylococcus lugdunensis. J. Infect. 40:98–99. 10.1053/jinf.1999.0563 [DOI] [PubMed] [Google Scholar]
- 145.Meehan AM, Osmon DR, Duffy MC, Hanssen AD, Keating MR. 2003. Outcome of penicillin-susceptible streptococcal prosthetic joint infection treated with debridement and retention of the prosthesis. Clin. Infect. Dis. 36:845–849. 10.1086/368182 [DOI] [PubMed] [Google Scholar]
- 146.Sprot H, Efstratiou A, Hubble M, Morgan M. 2012. Man's best friend? First report of prosthetic joint infection with Streptococcus pyogenes from a canine source. J. Infect. 64:625–627. 10.1016/j.jinf.2012.02.006 [DOI] [PubMed] [Google Scholar]
- 147.Ralph ED, Bourne RB. 1998. Toxic shock syndrome in association with group-A streptococcal infection of a knee joint after a total knee arthroplasty: a case report. J. Bone Joint Surg. Am. 80:96–98 [DOI] [PubMed] [Google Scholar]
- 148.Zeller V, Lavigne M, Leclerc P, Lhotellier L, Graff W, Ziza JM, Desplaces N, Mamoudy P. 2009. Group B streptococcal prosthetic joint infections: a retrospective study of 30 cases. Presse Med. 38:1577–1584. 10.1016/j.lpm.2009.02.026 [DOI] [PubMed] [Google Scholar]
- 149.Triesenberg SN, Clark NM, Kauffman CA. 1992. Group B streptococcal prosthetic joint infection following sigmoidoscopy. Clin. Infect. Dis. 15:374–375 [DOI] [PubMed] [Google Scholar]
- 150.Cunningham R, Walker C, Ridgway E. 1992. Prosthetic hip-joint infection associated with a penicillin-tolerant group B Streptococcus. J. Infect. 25:77–81 [DOI] [PubMed] [Google Scholar]
- 151.Duggan JM, Georgiadis G, VanGorp C, Kleshinski J. 2001. Group B streptococcal prosthetic joint infections. J. South. Orthop. Assoc. 10:209–214 [PubMed] [Google Scholar]
- 152.Sendi P, Christensson B, Uckay I, Trampuz A, Achermann Y, Boggian K, Svensson D, Widerstrom M, Zimmerli W. 2011. Group B Streptococcus in prosthetic hip and knee joint-associated infections. J. Hosp. Infect. 79:64–69. 10.1016/j.jhin.2011.04.022 [DOI] [PubMed] [Google Scholar]
- 153.Corvec S, Illiaquer M, Touchais S, Boutoille D, van der Mee-Marquet N, Quentin R, Reynaud A, Lepelletier D, Bemer P. 2011. Clinical features of group B Streptococcus prosthetic joint infections and molecular characterization of isolates. J. Clin. Microbiol. 49:380–382. 10.1128/JCM.00581-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kleshinski J, Georgiadis GM, Duggan JM. 2000. Group C streptococcal infection in a prosthetic joint. South. Med. J. 93:1217–1220 [PubMed] [Google Scholar]
- 155.Sundkvist T, von Essen R. 2002. Group C streptococcal infection in a prosthetic joint. South. Med. J. 95:107. [DOI] [PubMed] [Google Scholar]
- 156.Park MJ, Eun IS, Jung CY, Ko YC, Kim YJ, Kim CK, Kang EJ. 2012. Streptococcus dysgalactiae subspecies dysgalactiae infection after total knee arthroplasty: a case report. Knee Surg. Relat. Res. 24:120–123. 10.5792/ksrr.2012.24.2.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Pons M, Pulido A, Leal V, Viladot R. 1997. Sepsis due to group G Streptococcus after a total hip arthroplasty. A case report. Int. Orthop. 21:277–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Everts RJ, Chambers ST, Murdoch DR, Rothwell AG, McKie J. 2004. Successful antimicrobial therapy and implant retention for streptococcal infection of prosthetic joints. ANZ J. Surg. 74:210–214. 10.1111/j.1445-2197.2004.02942.x [DOI] [PubMed] [Google Scholar]
- 159.Emerton ME, Crook DW, Cooke PH. 1995. Streptococcus bovis-infected total hip arthroplasty. J. Arthroplasty 10:554–555. 10.1016/S0883-5403(05)80162-7 [DOI] [PubMed] [Google Scholar]
- 160.Liddle AD, Abram S, Iyer S, Andrade AJ. 2012. Streptococcus gallolyticus prosthetic joint infection associated with undiagnosed colonic malignancy. Knee Surg. Sports Traumatol. Arthrosc. 20:1069–1070. 10.1007/s00167-011-1646-2 [DOI] [PubMed] [Google Scholar]
- 161.Srivastava A, Walter N, Atkinson P. 2010. Streptococcus bovis infection of total hip arthroplasty in association with carcinoma of colon. J. Surg. Orthop. Adv. 19:125–128 http://www.datatrace.com/e-chemtracts/emailurl.html?http://www.newslettersonline.com/user/user.fas/s=563/fp=20/tp=37/19-2-8.pdf?T=open_article,50040306&P=article [PubMed] [Google Scholar]
- 162.Vince KG, Kantor SR, Descalzi J. 2003. Late infection of a total knee arthroplasty with Streptococcus bovis in association with carcinoma of the large intestine. J. Arthroplasty 18:813–815. 10.1016/S0883-5403(03)00268-7 [DOI] [PubMed] [Google Scholar]
- 163.Corredoira JC, Alonso MP, Garcia-Pais MJ, Rabunal R, Garcia-Garrote F, Lopez-Roses L, Lancho A, Coira A, Pita J, Velasco D, Lopez-Alvarez MJ, Tjalsma H, Varela J. 11 August 2013, posting date Is colonoscopy necessary in cases of infection by Streptococcus bovis biotype II? Eur. J. Clin. Microbiol. Infect. Dis. 10.1007/s10096-013-1940-7 [DOI] [PubMed] [Google Scholar]
- 164.Coelho-Prabhu N, Oxentenko AS, Osmon DR, Baron TH, Hanssen AD, Wilson WR, Steckelberg JM, Baddour LM, Harmsen WS, Mandrekar J, Berbari EF. 2013. Increased risk of prosthetic joint infection associated with esophago-gastro-duodenoscopy with biopsy. Acta Orthop. 84:82–86. 10.3109/17453674.2013.769079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wollner A, Gilon D, Mattan Y, Rubinow A, Pogrund H. 1989. Pneumococcal infection of a prosthetic hip joint. Int. Orthop. 13:135–136 [DOI] [PubMed] [Google Scholar]
- 166.Raad J, Peacock JE., Jr 2004. Septic arthritis in the adult caused by Streptococcus pneumoniae: a report of 4 cases and review of the literature. Semin. Arthritis Rheum. 34:559–569. 10.1016/j.semarthrit.2004.04.002 [DOI] [PubMed] [Google Scholar]
- 167.Brian SR, Kimbrough RC., III 2004. Salvage of a prosthetic knee joint infected with resistant pneumococcus. A case report. J. Bone Joint Surg. Am. 86:2302–2304 http://jbjs.org/article.aspx?articleid=26248 [DOI] [PubMed] [Google Scholar]
- 168.Sylvetsky N, Raveh D, Schlesinger Y, Rudensky B, Yinnon AM. 2002. Bacteremia due to beta-hemolytic Streptococcus group G: increasing incidence and clinical characteristics of patients. Am. J. Med. 112:622–626. 10.1016/S0002-9343(02)01117-8 [DOI] [PubMed] [Google Scholar]
- 169.El Helou OC, Berbari EF, Marculescu CE, El Atrouni WI, Razonable RR, Steckelberg JM, Hanssen AD, Osmon DR. 2008. Outcome of enterococcal prosthetic joint infection: is combination systemic therapy superior to monotherapy? Clin. Infect. Dis. 47:903–909. 10.1086/591536 [DOI] [PubMed] [Google Scholar]
- 170.Marculescu CE, Cantey JR. 2008. Polymicrobial prosthetic joint infections: risk factors and outcome. Clin. Orthop. Relat. Res. 466:1397–1404. 10.1007/s11999-008-0230-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Aboltins CA, Dowsey MM, Buising KL, Peel TN, Daffy JR, Choong PF, Stanley PA. 2011. Gram-negative prosthetic joint infection treated with debridement, prosthesis retention and antibiotic regimens including a fluoroquinolone. Clin. Microbiol. Infect. 17:862–867. 10.1111/j.1469-0691.2010.03361.x [DOI] [PubMed] [Google Scholar]
- 172.Jaen N, Martinez-Pastor JC, Munoz-Mahamud E, Garcia-Ramiro S, Bosch J, Mensa J, Soriano A. 2012. Long-term outcome of acute prosthetic joint infections due to Gram-negative bacilli treated with retention of prosthesis. Rev. Esp. Quimioter. 25:194–198 http://seq.es/seq/0214-3429/25/3/jaen.pdf [PubMed] [Google Scholar]
- 173.Raut VV, Orth MS, Orth MC, Siney PD, Wroblewski BM. 1996. One stage revision arthroplasty of the hip for deep Gram-negative infection. Int. Orthop. 20:12–14. 10.1007/s002640050019 [DOI] [PubMed] [Google Scholar]
- 174.Zmistowski B, Fedorka CJ, Sheehan E, Deirmengian G, Austin MS, Parvizi J. 2011. Prosthetic joint infection caused by Gram-negative organisms. J. Arthroplasty 26:104–108. 10.1016/j.arth.2011.03.044 [DOI] [PubMed] [Google Scholar]
- 175.Hsieh PH, Lee MS, Hsu KY, Chang YH, Shih HN, Ueng SW. 2009. Gram-negative prosthetic joint infections: risk factors and outcome of treatment. Clin. Infect. Dis. 49:1036–1043. 10.1086/605593 [DOI] [PubMed] [Google Scholar]
- 176.Lora-Tamayo J, Euba G, Ribera A, Murillo O, Pedrero S, Garcia-Somoza D, Pujol M, Cabo X, Ariza J. 2013. Infected hip hemiarthroplasties and total hip arthroplasties: differential findings and prognosis. J. Infect. 67:536–544. 10.1016/j.jinf.2013.07.030 [DOI] [PubMed] [Google Scholar]
- 177.Butler-Wu SM, Burns EM, Pottinger PS, Magaret AS, Rakeman JL, Matsen FA, III, Cookson BT. 2011. Optimization of periprosthetic culture for diagnosis of Propionibacterium acnes prosthetic joint infection. J. Clin. Microbiol. 49:2490–2495. 10.1128/JCM.00450-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Zeller V, Ghorbani A, Strady C, Leonard P, Mamoudy P, Desplaces N. 2007. Propionibacterium acnes: an agent of prosthetic joint infection and colonization. J. Infect. 55:119–124. 10.1016/j.jinf.2007.02.006 [DOI] [PubMed] [Google Scholar]
- 179.Lutz MF, Berthelot P, Fresard A, Cazorla C, Carricajo A, Vautrin AC, Fessy MH, Lucht F. 2005. Arthroplastic and osteosynthetic infections due to Propionibacterium acnes: a retrospective study of 52 cases, 1995-2002. Eur. J. Clin. Microbiol. Infect. Dis. 24:739–744. 10.1007/s10096-005-0040-8 [DOI] [PubMed] [Google Scholar]
- 180.Berthelot P, Carricajo A, Aubert G, Akhavan H, Gazielly D, Lucht F. 2006. Outbreak of postoperative shoulder arthritis due to Propionibacterium acnes infection in nondebilitated patients. Infect. Control Hosp. Epidemiol. 27:987–990. 10.1086/507287 [DOI] [PubMed] [Google Scholar]
- 181.Pottinger P, Butler-Wu S, Neradilek MB, Merritt A, Bertelsen A, Jette JL, Warme WJ, Matsen FA., III 2012. Prognostic factors for bacterial cultures positive for Propionibacterium acnes and other organisms in a large series of revision shoulder arthroplasties performed for stiffness, pain, or loosening. J. Bone Joint Surg. Am. 94:2075–2083. 10.2106/JBJS.K.00861 [DOI] [PubMed] [Google Scholar]
- 182.McCarthy J, Stingemore N. 1999. Clostridium difficile infection of a prosthetic joint presenting 12 months after antibiotic-associated diarrhoea. J. Infect. 39:94–96. 10.1016/S0163-4453(99)90110-X [DOI] [PubMed] [Google Scholar]
- 183.Pron B, Merckx J, Touzet P, Ferroni A, Poyart C, Berche P, Gaillard JL. 1995. Chronic septic arthritis and osteomyelitis in a prosthetic knee joint due to Clostridium difficile. Eur. J. Clin. Microbiol. Infect. Dis. 14:599–601. 10.1007/BF01690732 [DOI] [PubMed] [Google Scholar]
- 184.Ranganath S, Midturi JK. 2013. Unusual case of prosthetic shoulder joint infection due to Clostridium difficile. Am. J. Med. Sci. 346:422–423. 10.1097/MAJ.0b013e3182987d05 [DOI] [PubMed] [Google Scholar]
- 185.Burnell CD, Turgeon TR, Hedden DR, Bohm ER. 2011. Paraneoplastic Clostridium septicum infection of a total knee arthroplasty. J. Arthroplasty 26:666.e9-666.e11. 10.1016/j.arth.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 186.Economedes DM, Santoro J, Deirmengian CA. 2012. Clostridium septicum growth from a total knee arthroplasty associated with intestinal malignancy: a case report. BMC Infect. Dis. 12:235. 10.1186/1471-2334-12-235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wilde AH, Sweeney RS, Borden LS. 1988. Hematogenously acquired infection of a total knee arthroplasty by Clostridium perfringens. Clin. Orthop. Relat. Res. 229:228–231 [PubMed] [Google Scholar]
- 188.Bach BR, Jr, Ewald FC. 1985. Air in painful total hip arthroplasty: diagnosis and treatment. Clin. Orthop. Relat. Res. 193:146–149 [PubMed] [Google Scholar]
- 189.Bartz H, Nonnenmacher C, Bollmann C, Kuhl M, Zimmermann S, Heeg K, Mutters R. 2005. Micromonas (Peptostreptococcus) micros: unusual case of prosthetic joint infection associated with dental procedures. Int. J. Med. Microbiol. 294:465–470. 10.1016/j.ijmm.2004.10.001 [DOI] [PubMed] [Google Scholar]
- 190.LaPorte DM, Waldman BJ, Mont MA, Hungerford DS. 1999. Infections associated with dental procedures in total hip arthroplasty. J. Bone Joint Surg. Br. 81:56–59. 10.1302/0301-620X.81B1.8608 [DOI] [PubMed] [Google Scholar]
- 191.Hedke J, Skripitz R, Ellenrieder M, Frickmann H, Koller T, Podbielski A, Mittelmeier W. 2012. Low-grade infection after a total knee arthroplasty caused by Actinomyces naeslundii. J. Med. Microbiol. 61:1162–1164. 10.1099/jmm.0.030395-0 [DOI] [PubMed] [Google Scholar]
- 192.Rieber H, Schwarz R, Kramer O, Cordier W, Frommelt L. 2009. Actinomyces neuii subsp. neuii associated with periprosthetic infection in total hip arthroplasty as causative agent. J. Clin. Microbiol. 47:4183–4184. 10.1128/JCM.01249-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Zaman R, Abbas M, Burd E. 2002. Late prosthetic hip joint infection with Actinomyces israelii in an intravenous drug user: case report and literature review. J. Clin. Microbiol. 40:4391–4392. 10.1128/JCM.40.11.4391-4392.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ruhe J, Holding K, Mushatt D. 2001. Infected total knee arthroplasty due to Actinomyces naeslundii. Scand. J. Infect. Dis. 33:230–231. 10.1080/00365540151060987 [DOI] [PubMed] [Google Scholar]
- 195.Brown ML, Drinkwater CJ. 2012. Hematogenous infection of total hip arthroplasty with Actinomyces following a noninvasive dental procedure. Orthopedics 35:e1086–e1089. 10.3928/01477447-20120621-27 [DOI] [PubMed] [Google Scholar]
- 196.Strazzeri JC, Anzel S. 1986. Infected total hip arthroplasty due to Actinomyces israelii after dental extraction. A case report. Clin. Orthop. Relat. Res. 210:128–131 [PubMed] [Google Scholar]
- 197.Achermann Y, Trampuz A, Moro F, Wust J, Vogt M. 2009. Corynebacterium bovis shoulder prosthetic joint infection: the first reported case. Diagn. Microbiol. Infect. Dis. 64:213–215. 10.1016/j.diagmicrobio.2009.02.003 [DOI] [PubMed] [Google Scholar]
- 198.Cazanave C, Greenwood-Quaintance KE, Hanssen AD, Patel R. 2012. Corynebacterium prosthetic joint infection. J. Clin. Microbiol. 50:1518–1523. 10.1128/JCM.06439-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Roux V, Drancourt M, Stein A, Riegel P, Raoult D, La Scola B. 2004. Corynebacterium species isolated from bone and joint infections identified by 16S rRNA gene sequence analysis. J. Clin. Microbiol. 42:2231–2233. 10.1128/JCM.42.5.2231-2233.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.von Graevenitz A, Frommelt L, Punter-Streit V, Funke G. 1998. Diversity of coryneforms found in infections following prosthetic joint insertion and open fractures. Infection 26:36–38. 10.1007/BF02768750 [DOI] [PubMed] [Google Scholar]
- 201.Tleyjeh IM, Qutub MO, Bakleh M, Sohail MR, Virk A. 2005. Corynebacterium jeikeium prosthetic joint infection: case report and literature review. Scand. J. Infect. Dis. 37:151–153. 10.1080/00365540410020785 [DOI] [PubMed] [Google Scholar]
- 202.Yildiz S, Yildiz HY, Cetin I, Ucar DH. 1995. Total knee arthroplasty complicated by Corynebacterium jeikeium infection. Scand. J. Infect. Dis. 27:635–636. 10.3109/00365549509047081 [DOI] [PubMed] [Google Scholar]
- 203.Charlier C, Leclercq A, Cazenave B, Desplaces N, Travier L, Cantinelli T, Lortholary O, Goulet V, Le Monnier A, Lecuit M. 2012. Listeria monocytogenes-associated joint and bone infections: a study of 43 consecutive cases. Clin. Infect. Dis. 54:240–248. 10.1093/cid/cir803 [DOI] [PubMed] [Google Scholar]
- 204.Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. 2006. The new global map of human brucellosis. Lancet Infect. Dis. 6:91–99. 10.1016/S1473-3099(06)70382-6 [DOI] [PubMed] [Google Scholar]
- 205.Agarwal S, Kadhi SK, Rooney RJ. 1991. Brucellosis complicating bilateral total knee arthroplasty. Clin. Orthop. Relat. Res. 267:179–181 [PubMed] [Google Scholar]
- 206.Erdogan H, Cakmak G, Erdogan A, Arslan H. 2010. Brucella melitensis infection in total knee arthroplasty: a case report. Knee Surg. Sports Traumatol. Arthrosc. 18:908–910. 10.1007/s00167-010-1048-x [DOI] [PubMed] [Google Scholar]
- 207.Kasim RA, Araj GF, Afeiche NE, Tabbarah ZA. 2004. Brucella infection in total hip replacement: case report and review of the literature. Scand. J. Infect. Dis. 36:65–67. 10.1080/00365540310017456 [DOI] [PubMed] [Google Scholar]
- 208.Weil Y, Mattan Y, Liebergall M, Rahav G. 2003. Brucella prosthetic joint infection: a report of 3 cases and a review of the literature. Clin. Infect. Dis. 36:e81–e86. 10.1086/368084 [DOI] [PubMed] [Google Scholar]
- 209.Mehta H, Mackie I. 2004. Prosthetic joint infection with Pasturella multocida following cat scratch: a report of 2 cases. J. Arthroplasty 19:525–527. 10.1016/j.arth.2003.11.012 [DOI] [PubMed] [Google Scholar]
- 210.Antuna SA, Mendez JG, Castellanos JL, Jimenez JP. 1997. Late infection after total knee arthroplasty caused by Pasteurella multocida. Acta Orthop. Belg. 63:310–312 [PubMed] [Google Scholar]
- 211.Arvan GD, Goldberg V. 1978. A case report of total knee arthroplasty infected by Pasteurella multocida. Clin. Orthop. Relat. Res. 132:167–169 [PubMed] [Google Scholar]
- 212.Blanco JF, Pescador D, Martin JM, Cano C, Sanchez MD. 2012. Acute infection of total knee arthroplasty due to a cat scratch in a patient with rheumatoid arthritis. J. Clin. Rheumatol. 18:314–315. 10.1097/RHU.0b013e3182677175 [DOI] [PubMed] [Google Scholar]
- 213.Braithwaite BD, Giddins G. 1992. Pasteurella multocida infection of a total hip arthroplasty. A case report. J. Arthroplasty 7:309–310 [DOI] [PubMed] [Google Scholar]
- 214.Gabuzda GM, Barnett PR. 1992. Pasteurella infection in a total knee arthroplasty. Orthop. Rev. 21:601, 604-605. [PubMed] [Google Scholar]
- 215.Guion TL, Sculco TP. 1992. Pasteurella multocida infection in total knee arthroplasty. Case report and literature review. J. Arthroplasty 7:157–160 [DOI] [PubMed] [Google Scholar]
- 216.Heydemann J, Heydemann JS, Antony S. 2010. Acute infection of a total knee arthroplasty caused by Pasteurella multocida: a case report and a comprehensive review of the literature in the last 10 years. Int. J. Infect. Dis. 14(Suppl 3):e242–e245. 10.1016/j.ijid.2009.09.007 [DOI] [PubMed] [Google Scholar]
- 217.Heym B, Jouve F, Lemoal M, Veil-Picard A, Lortat-Jacob A, Nicolas-Chanoine MH. 2006. Pasteurella multocida infection of a total knee arthroplasty after a “dog lick.” Knee Surg. Sports Traumatol. Arthrosc. 14:993–997. 10.1007/s00167-005-0022-5 [DOI] [PubMed] [Google Scholar]
- 218.Kadakia AP, Langkamer VG. 2008. Sepsis of total knee arthroplasty after domestic cat bite: should we warn patients? Am. J. Orthop. 37:370–371 http://www.amjorthopedics.com/fileadmin/qhi_archive/ArticlePDF/AJO/037070370.pdf [PubMed] [Google Scholar]
- 219.Maradona JA, Asensi V, Carton JA, Rodriguez Guardado A, Lizon Castellano J. 1997. Prosthetic joint infection by Pasteurella multocida. Eur. J. Clin. Microbiol. Infect. Dis. 16:623–625. 10.1007/BF02447933 [DOI] [PubMed] [Google Scholar]
- 220.Miranda I, Angulo M, Amaya JV. 2013. Acute total knee replacement infection after a cat bite and scratch: a clinical case and review of the literature. Rev. Esp. Cir. Ortop. Traumatol. 57:300–305. 10.1016/j.recot.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 221.Takwale VJ, Wright ED, Bates J, Edge AJ. 1997. Pasteurella multocida infection of a total hip arthroplasty following cat scratch. J. Infect. 34:263–264. 10.1016/S0163-4453(97)94423-6 [DOI] [PubMed] [Google Scholar]
- 222.Stiehl JB, Sterkin LA, Brummitt CF. 2004. Acute Pasteurella multocida in total knee arthroplasty. J. Arthroplasty 19:244–247. 10.1016/j.arth.2003.08.004 [DOI] [PubMed] [Google Scholar]
- 223.Tande AJ, Cunningham SA, Raoult D, Sim FH, Berbari EF, Patel R. 2013. A case of Q fever prosthetic joint infection and description of an assay for detection of Coxiella burnetii. J. Clin. Microbiol. 51:66–69. 10.1128/JCM.02352-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Marculescu CE, Berbari EF, Cockerill FR, III, Osmon DR. 2006. Fungi, mycobacteria, zoonotic and other organisms in prosthetic joint infection. Clin. Orthop. Relat. Res. 451:64–72. 10.1097/01.blo.0000229337.21653.f2 [DOI] [PubMed] [Google Scholar]
- 225.Marculescu CE, Berbari EF, Cockerill FR, III, Osmon DR. 2006. Unusual aerobic and anaerobic bacteria associated with prosthetic joint infections. Clin. Orthop. Relat. Res. 451:55–63. 10.1097/01.blo.0000229317.43631.81 [DOI] [PubMed] [Google Scholar]
- 226.Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. 2009. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin. Infect. Dis. 49:1350–1357. 10.1086/605559 [DOI] [PubMed] [Google Scholar]
- 227.Berbari EF, Hanssen AD, Duffy MC, Steckelberg JM, Osmon DR. 1998. Prosthetic joint infection due to Mycobacterium tuberculosis: a case series and review of the literature. Am. J. Orthop. 27:219–227 [PubMed] [Google Scholar]
- 228.Su JY, Huang TL, Lin SY. 1996. Total knee arthroplasty in tuberculous arthritis. Clin. Orthop. Relat. Res. 323:181–187 [DOI] [PubMed] [Google Scholar]
- 229.Carrega G, Bartolacci V, Burastero G, Finocchio GC, Ronca A, Riccio G. 2013. Prosthetic joint infections due to Mycobacterium tuberculosis: a report of 5 cases. Int. J. Surg. Case Rep. 4:178–181. 10.1016/j.ijscr.2012.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Spinner RJ, Sexton DJ, Goldner RD, Levin LS. 1996. Periprosthetic infections due to Mycobacterium tuberculosis in patients with no prior history of tuberculosis. J. Arthroplasty 11:217–222. 10.1016/S0883-5403(05)80023-3 [DOI] [PubMed] [Google Scholar]
- 231.Gale DW, Harding ML. 1991. Total knee arthroplasty in the presence of active tuberculosis. J. Bone Joint Surg. Br. 73:1006–1007 [DOI] [PubMed] [Google Scholar]
- 232.Marmor M, Parnes N, Dekel S. 2004. Tuberculosis infection complicating total knee arthroplasty: report of 3 cases and review of the literature. J. Arthroplasty 19:397–400. 10.1016/j.arth.2003.10.015 [DOI] [PubMed] [Google Scholar]
- 233.Eid AJ, Berbari EF, Sia IG, Wengenack NL, Osmon DR, Razonable RR. 2007. Prosthetic joint infection due to rapidly growing mycobacteria: report of 8 cases and review of the literature. Clin. Infect. Dis. 45:687–694. 10.1086/520982 [DOI] [PubMed] [Google Scholar]
- 234.McLaughlin JR, Tierney M, Harris WH. 1994. Mycobacterium avium intracellulare infection of hip arthroplasties in an AIDS patient. J. Bone Joint Surg. Br. 76:498–499 [PubMed] [Google Scholar]
- 235.Gupta A, Clauss H. 2009. Prosthetic joint infection with Mycobacterium avium complex in a solid organ transplant recipient. Transpl. Infect. Dis. 11:537–540. 10.1111/j.1399-3062.2009.00433.x [DOI] [PubMed] [Google Scholar]
- 236.Isono SS, Woolson ST, Schurman DJ. 1987. Total joint arthroplasty for steroid-induced osteonecrosis in cardiac transplant patients. Clin. Orthop. Relat. Res. 217:201–208 [PubMed] [Google Scholar]
- 237.Vergidis P, Lesnick TG, Kremers WK, Razonable RR. 2012. Prosthetic joint infection in solid organ transplant recipients: a retrospective case-control study. Transpl. Infect. Dis. 14:380–386. 10.1111/j.1399-3062.2011.00708.x [DOI] [PubMed] [Google Scholar]
- 238.Hwang BH, Yoon JY, Nam CH, Jung KA, Lee SC, Han CD, Moon SH. 2012. Fungal peri-prosthetic joint infection after primary total knee replacement. J. Bone Joint Surg. Br. 94:656–659. 10.1302/0301-620X.94B5.28125 [DOI] [PubMed] [Google Scholar]
- 239.Azzam K, Parvizi J, Jungkind D, Hanssen A, Fehring T, Springer B, Bozic K, Della Valle C, Pulido L, Barrack R. 2009. Microbiological, clinical, and surgical features of fungal prosthetic joint infections: a multi-institutional experience. J. Bone Joint Surg. Am. 91(Suppl 6):142–149. 10.2106/JBJS.I.00574 [DOI] [PubMed] [Google Scholar]
- 240.Austin KS, Testa NN, Luntz RK, Greene JB, Smiles S. 1992. Aspergillus infection of total knee arthroplasty presenting as a popliteal cyst. Case report and review of the literature. J. Arthroplasty 7:311–314 [DOI] [PubMed] [Google Scholar]
- 241.Baumann PA, Cunningham B, Patel NS, Finn HA. 2001. Aspergillus fumigatus infection in a mega prosthetic total knee arthroplasty: salvage by staged reimplantation with 5-year follow-up. J. Arthroplasty 16:498–503. 10.1054/arth.2001.21505 [DOI] [PubMed] [Google Scholar]
- 242.Yilmaz M, Mete B, Ozaras R, Kaynak G, Tabak F, Tenekecioglu Y, Ozturk R. 2011. Aspergillus fumigatus infection as a delayed manifestation of prosthetic knee arthroplasty and a review of the literature. Scand. J. Infect. Dis. 43:573–578. 10.3109/00365548.2011.574294 [DOI] [PubMed] [Google Scholar]
- 243.Austen S, van der Weegen W, Verduin CM, van der Valk M, Hoekstra HJ. 2013. Coccidioidomycosis infection of a total knee arthroplasty in a nonendemic region. J. Arthroplasty 28:375.e13-375.e15. 10.1016/j.arth.2012.05.006 [DOI] [PubMed] [Google Scholar]
- 244.Koeter S, Jackson RW. 2006. Successful total knee arthroplasty in the presence of sporotrichal arthritis. Knee 13:236–237. 10.1016/j.knee.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 245.Lackner M, De Man FH, Eygendaal D, Wintermans RG, Kluytmans JA, Klaassen CH, Meis JF. 2011. Severe prosthetic joint infection in an immunocompetent male patient due to a therapy refractory Pseudallescheria apiosperma. Mycoses 54(Suppl 3):22–27. 10.1111/j.1439-0507.2011.02107.x [DOI] [PubMed] [Google Scholar]
- 246.Phelan DM, Osmon DR, Keating MR, Hanssen AD. 2002. Delayed reimplantation arthroplasty for candidal prosthetic joint infection: a report of 4 cases and review of the literature. Clin. Infect. Dis. 34:930–938. 10.1086/339212 [DOI] [PubMed] [Google Scholar]
- 247.Darouiche RO, Hamill RJ, Musher DM, Young EJ, Harris RL. 1989. Periprosthetic candidal infections following arthroplasty. Rev. Infect. Dis. 11:89–96. 10.1093/clinids/11.1.89 [DOI] [PubMed] [Google Scholar]
- 248.Trampuz A, Piper KE, Jacobson MJ, Hanssen AD, Unni KK, Osmon DR, Mandrekar JN, Cockerill FR, Steckelberg JM, Greenleaf JF, Patel R. 2007. Sonication of removed hip and knee prostheses for diagnosis of infection. N. Engl. J. Med. 357:654–663. 10.1056/NEJMoa061588 [DOI] [PubMed] [Google Scholar]
- 249.Berbari EF, Marculescu C, Sia I, Lahr BD, Hanssen AD, Steckelberg JM, Gullerud R, Osmon DR. 2007. Culture-negative prosthetic joint infection. Clin. Infect. Dis. 45:1113–1119. 10.1086/522184 [DOI] [PubMed] [Google Scholar]
- 250.Melendez D, Osmon D, Greenwood-Quaintance K, Hanssen AD, Patel R. 2013. Comparison of the Musculoskeletal Infection Society and Infectious Diseases Society of America diagnostic criteria for prosthetic joint infection, abstr 791. Abstr. IDWeek 2013. [Google Scholar]
- 251.Parvizi J, Gehrke T. 2013. Proceedings of the International Consensus Meeting on periprosthetic joint infection. Musculoskeletal Infection Society, Rochester, MN http://www.msis-na.org/international-consensus/ [Google Scholar]
- 252.Mikhael MM, Hanssen AD, Sierra RJ. 2009. Failure of metal-on-metal total hip arthroplasty mimicking hip infection. A report of two cases. J. Bone Joint Surg. Am. 91:443–446. 10.2106/JBJS.H.00603 [DOI] [PubMed] [Google Scholar]
- 253.Berbari E, Mabry T, Tsaras G, Spangehl M, Erwin PJ, Murad MH, Steckelberg J, Osmon D. 2010. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J. Bone Joint Surg. Am. 92:2102–2109. 10.2106/JBJS.I.01199 [DOI] [PubMed] [Google Scholar]
- 254.Della Valle C, Parvizi J, Bauer TW, Dicesare PE, Evans RP, Segreti J, Spangehl M, Watters WC, III, Keith M, Turkelson CM, Wies JL, Sluka P, Hitchcock K. 2010. Diagnosis of periprosthetic joint infections of the hip and knee. J. Am. Acad. Orthop. Surg. 18:760–770 http://www.jaaos.org/content/18/12/760.long [DOI] [PubMed] [Google Scholar]
- 255.Austin MS, Ghanem E, Joshi A, Lindsay A, Parvizi J. 2008. A simple, cost-effective screening protocol to rule out periprosthetic infection. J. Arthroplasty 23:65–68. 10.1016/j.arth.2007.09.005 [DOI] [PubMed] [Google Scholar]
- 256.Alijanipour P, Bakhshi H, Parvizi J. 2013. Diagnosis of periprosthetic joint infection: the threshold for serological markers. Clin. Orthop. Relat. Res. 471:3186–3195. 10.1007/s11999-013-3070-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Bedair H, Ting N, Jacovides C, Saxena A, Moric M, Parvizi J, Della Valle CJ. 2011. The Mark Coventry Award: diagnosis of early postoperative TKA infection using synovial fluid analysis. Clin. Orthop. Relat. Res. 469:34–40. 10.1007/s11999-010-1433-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Piper KE, Fernandez-Sampedro M, Steckelberg KE, Mandrekar JN, Karau MJ, Steckelberg JM, Berbari EF, Osmon DR, Hanssen AD, Lewallen DG, Cofield RH, Sperling JW, Sanchez-Sotelo J, Huddleston PM, Dekutoski MB, Yaszemski M, Currier B, Patel R. 2010. C-reactive protein, erythrocyte sedimentation rate and orthopedic implant infection. PLoS One 5:e9358. 10.1371/journal.pone.0009358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Wirtz DC, Heller KD, Miltner O, Zilkens KW, Wolff JM. 2000. Interleukin-6: a potential inflammatory marker after total joint replacement. Int. Orthop. 24:194–196. 10.1007/s002640000136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Worthington T, Dunlop D, Casey A, Lambert R, Luscombe J, Elliott T. 2010. Serum procalcitonin, interleukin-6, soluble intercellular adhesin molecule-1 and IgG to short-chain exocellular lipoteichoic acid as predictors of infection in total joint prosthesis revision. Br. J. Biomed. Sci. 67:71–76 http://www.bjbs-online.org/article.asp?id=389 [DOI] [PubMed] [Google Scholar]
- 261.Gollwitzer H, Dombrowski Y, Prodinger PM, Peric M, Summer B, Hapfelmeier A, Saldamli B, Pankow F, von Eisenhart-Rothe R, Imhoff AB, Schauber J, Thomas P, Burgkart R, Banke IJ. 2013. Antimicrobial peptides and proinflammatory cytokines in periprosthetic joint infection. J. Bone Joint Surg. Am. 95:644–651. 10.2106/JBJS.L.00205 [DOI] [PubMed] [Google Scholar]
- 262.Bottner F, Wegner A, Winkelmann W, Becker K, Erren M, Gotze C. 2007. Interleukin-6, procalcitonin and TNF-alpha: markers of peri-prosthetic infection following total joint replacement. J. Bone Joint Surg. Br. 89:94–99 http://www.bjj.boneandjoint.org.uk/content/89-B/1/94.full.pdf [DOI] [PubMed] [Google Scholar]
- 263.Tigges S, Stiles RG, Roberson JR. 1994. Appearance of septic hip prostheses on plain radiographs. Am. J. Roentgenol. 163:377–380. 10.2214/ajr.163.2.8037035 [DOI] [PubMed] [Google Scholar]
- 264.Cyteval C, Hamm V, Sarrabere MP, Lopez FM, Maury P, Taourel P. 2002. Painful infection at the site of hip prosthesis: CT imaging. Radiology 224:477–483. 10.1148/radiol.2242010989 [DOI] [PubMed] [Google Scholar]
- 265.Glaudemans AW, Galli F, Pacilio M, Signore A. 2013. Leukocyte and bacteria imaging in prosthetic joint infection. Eur. Cells Mater. 25:61–77 http://www.ecmjournal.org/journal/papers/vol025/pdf/v025a05.pdf [DOI] [PubMed] [Google Scholar]
- 266.Rosenthall L, Lepanto L, Raymond F. 1987. Radiophosphate uptake in asymptomatic knee arthroplasty. J. Nucl. Med. 28:1546–1549 [PubMed] [Google Scholar]
- 267.Reinartz P, Mumme T, Hermanns B, Cremerius U, Wirtz DC, Schaefer WM, Niethard F, Buell U. 2005. Radionuclide imaging of the painful hip arthroplasty: positron-emission tomography versus triple-phase bone scanning. J. Bone Joint Surg. Br. 87:465–470. 10.1302/0301-620X.87B4.14954 [DOI] [PubMed] [Google Scholar]
- 268.Nagoya S, Kaya M, Sasaki M, Tateda K, Yamashita T. 2008. Diagnosis of peri-prosthetic infection at the hip using triple-phase bone scintigraphy. J. Bone Joint Surg. Br. 90:140–144. 10.1302/0301-620X.90B2.19436 [DOI] [PubMed] [Google Scholar]
- 269.Love C, Marwin SE, Tomas MB, Krauss ES, Tronco GG, Bhargava KK, Nichols KJ, Palestro CJ. 2004. Diagnosing infection in the failed joint replacement: a comparison of coincidence detection 18F-FDG and 111In-labeled leukocyte/99mTc-sulfur colloid marrow imaging. J. Nucl. Med. 45:1864–1871 http://jnm.snmjournals.org/content/45/11/1864.full.pdf [PubMed] [Google Scholar]
- 270.Teller RE, Christie MJ, Martin W, Nance EP, Haas DW. 2000. Sequential indium-labeled leukocyte and bone scans to diagnose prosthetic joint infection. Clin. Orthop. Relat. Res. 373:241–247. 10.1097/00003086-200004000-00029 [DOI] [PubMed] [Google Scholar]
- 271.Scher DM, Pak K, Lonner JH, Finkel JE, Zuckerman JD, Di Cesare PE. 2000. The predictive value of indium-111 leukocyte scans in the diagnosis of infected total hip, knee, or resection arthroplasties. J. Arthroplasty 15:295–300. 10.1016/S0883-5403(00)90555-2 [DOI] [PubMed] [Google Scholar]
- 272.Kwee TC, Kwee RM, Alavi A. 2008. FDG-PET for diagnosing prosthetic joint infection: systematic review and metaanalysis. Eur. J. Nucl. Med. Mol. Imaging 35:2122–2132. 10.1007/s00259-008-0887-x [DOI] [PubMed] [Google Scholar]
- 273.Ghanem E, Parvizi J, Burnett RS, Sharkey PF, Keshavarzi N, Aggarwal A, Barrack RL. 2008. Cell count and differential of aspirated fluid in the diagnosis of infection at the site of total knee arthroplasty. J. Bone Joint Surg. Am. 90:1637–1643. 10.2106/JBJS.G.00470 [DOI] [PubMed] [Google Scholar]
- 274.Trampuz A, Hanssen AD, Osmon DR, Mandrekar J, Steckelberg JM, Patel R. 2004. Synovial fluid leukocyte count and differential for the diagnosis of prosthetic knee infection. Am. J. Med. 117:556–562. 10.1016/j.amjmed.2004.06.022 [DOI] [PubMed] [Google Scholar]
- 275.Zmistowski B, Restrepo C, Huang R, Hozack WJ, Parvizi J. 2012. Periprosthetic joint infection diagnosis: a complete understanding of white blood cell count and differential. J. Arthroplasty 27:1589–1593. 10.1016/j.arth.2012.03.059 [DOI] [PubMed] [Google Scholar]
- 276.Schinsky MF, Della Valle CJ, Sporer SM, Paprosky WG. 2008. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J. Bone Joint Surg. Am. 90:1869–1875. 10.2106/JBJS.G.01255 [DOI] [PubMed] [Google Scholar]
- 277.Dinneen A, Guyot A, Clements J, Bradley N. 2013. Synovial fluid white cell and differential count in the diagnosis or exclusion of prosthetic joint infection. Bone Joint J. 95-B:554–557. 10.1302/0301-620X.95B4.30388 [DOI] [PubMed] [Google Scholar]
- 278.Wyles CC, Larson DR, Houdek MT, Sierra RJ, Trousdale RT. 2013. Utility of synovial fluid aspirations in failed metal-on-metal total hip arthroplasty. J. Arthroplasty 28:818–823. 10.1016/j.arth.2012.11.006 [DOI] [PubMed] [Google Scholar]
- 279.Parvizi J, Jacovides C, Antoci V, Ghanem E. 2011. Diagnosis of periprosthetic joint infection: the utility of a simple yet unappreciated enzyme. J. Bone Joint Surg. Am. 93:2242–2248. 10.2106/JBJS.J.01413 [DOI] [PubMed] [Google Scholar]
- 280.Wetters NG, Berend KR, Lombardi AV, Morris MJ, Tucker TL, Della Valle CJ. 2012. Leukocyte esterase reagent strips for the rapid diagnosis of periprosthetic joint infection. J. Arthroplasty 27:8–11. 10.1016/j.arth.2012.03.037 [DOI] [PubMed] [Google Scholar]
- 281.Parvizi J, McKenzie JC, Cashman JP. 2012. Diagnosis of periprosthetic joint infection using synovial C-reactive protein. J. Arthroplasty 27:12–16. 10.1016/j.arth.2012.03.018 [DOI] [PubMed] [Google Scholar]
- 282.Jacovides CL, Parvizi J, Adeli B, Jung KA. 2011. Molecular markers for diagnosis of periprosthetic joint infection. J. Arthroplasty 26:99–103.e101. 10.1016/j.arth.2011.03.025 [DOI] [PubMed] [Google Scholar]
- 283.Deirmengian C, Hallab N, Tarabishy A, Della Valle C, Jacobs JJ, Lonner J, Booth RE., Jr 2010. Synovial fluid biomarkers for periprosthetic infection. Clin. Orthop. Relat. Res. 468:2017–2023. 10.1007/s11999-010-1298-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Nilsdotter-Augustinsson A, Briheim G, Herder A, Ljunghusen O, Wahlstrom O, Ohman L. 2007. Inflammatory response in 85 patients with loosened hip prostheses: a prospective study comparing inflammatory markers in patients with aseptic and septic prosthetic loosening. Acta Orthop. 78:629–639. 10.1080/17453670710014329 [DOI] [PubMed] [Google Scholar]
- 285.Saeed K, Dryden M, Sitjar A, White G. 2013. Measuring synovial fluid procalcitonin levels in distinguishing cases of septic arthritis, including prosthetic joints, from other causes of arthritis and aseptic loosening. Infection 41:845–849. 10.1007/s15010-013-0467-2 [DOI] [PubMed] [Google Scholar]
- 286.Fehring TK, Cohen B. 1996. Aspiration as a guide to sepsis in revision total hip arthroplasty. J. Arthroplasty 11:543–547. 10.1016/S0883-5403(96)80107-0 [DOI] [PubMed] [Google Scholar]
- 287.Lachiewicz PF, Rogers GD, Thomason HC. 1996. Aspiration of the hip joint before revision total hip arthroplasty. Clinical and laboratory factors influencing attainment of a positive culture. J. Bone Joint Surg. Am. 78:749–754 [DOI] [PubMed] [Google Scholar]
- 288.Barrack RL, Harris WH. 1993. The value of aspiration of the hip joint before revision total hip arthroplasty. J. Bone Joint Surg. Am. 75:66–76 [DOI] [PubMed] [Google Scholar]
- 289.Hughes JG, Vetter EA, Patel R, Schleck CD, Harmsen S, Turgeant LT, Cockerill FR., III 2001. Culture with BACTEC Peds Plus/F bottle compared with conventional methods for detection of bacteria in synovial fluid. J. Clin. Microbiol. 39:4468–4471. 10.1128/JCM.39.12.4468-4471.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Ali F, Wilkinson JM, Cooper JR, Kerry RM, Hamer AJ, Norman P, Stockley I. 2006. Accuracy of joint aspiration for the preoperative diagnosis of infection in total hip arthroplasty. J. Arthroplasty 21:221–226. 10.1016/j.arth.2005.05.027 [DOI] [PubMed] [Google Scholar]
- 291.Font-Vizcarra L, Garcia S, Martinez-Pastor JC, Sierra JM, Soriano A. 2010. Blood culture flasks for culturing synovial fluid in prosthetic joint infections. Clin. Orthop. Relat. Res. 468:2238–2243. 10.1007/s11999-010-1254-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Roberts P, Walters AJ, McMinn DJ. 1992. Diagnosing infection in hip replacements. The use of fine-needle aspiration and radiometric culture. J. Bone Joint Surg. Br. 74:265–269 [DOI] [PubMed] [Google Scholar]
- 293.Qu X, Zhai Z, Wu C, Jin F, Li H, Wang L, Liu G, Liu X, Wang W, Zhang X, Zhu Z, Dai K. 2013. Preoperative aspiration culture for preoperative diagnosis of infection in total hip or knee arthroplasty. J. Clin. Microbiol. 51:3830–3834. 10.1128/JCM.01467-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Fink B, Makowiak C, Fuerst M, Berger I, Schafer P, Frommelt L. 2008. The value of synovial biopsy, joint aspiration and C-reactive protein in the diagnosis of late peri-prosthetic infection of total knee replacements. J. Bone Joint Surg. Br. 90:874–878. 10.1302/0301-620X.90B7.20417 [DOI] [PubMed] [Google Scholar]
- 295.Williams JL, Norman P, Stockley I. 2004. The value of hip aspiration versus tissue biopsy in diagnosing infection before exchange hip arthroplasty surgery. J. Arthroplasty 19:582–586. 10.1016/j.arth.2003.11.011 [DOI] [PubMed] [Google Scholar]
- 296.Sadiq S, Wootton JR, Morris CA, Northmore-Ball MD. 2005. Application of core biopsy in revision arthroplasty for deep infection. J. Arthroplasty 20:196–201. 10.1016/j.arth.2004.09.038 [DOI] [PubMed] [Google Scholar]
- 297.Meermans G, Haddad FS. 2010. Is there a role for tissue biopsy in the diagnosis of periprosthetic infection? Clin. Orthop. Relat. Res. 468:1410–1417. 10.1007/s11999-010-1245-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Morgan PM, Sharkey P, Ghanem E, Parvizi J, Clohisy JC, Burnett RS, Barrack RL. 2009. The value of intraoperative Gram stain in revision total knee arthroplasty. J. Bone Joint Surg. Am. 91:2124–2129. 10.2106/JBJS.H.00853 [DOI] [PubMed] [Google Scholar]
- 299.Chimento GF, Finger S, Barrack RL. 1996. Gram stain detection of infection during revision arthroplasty. J. Bone Joint Surg. Br. 78:838–839 [PubMed] [Google Scholar]
- 300.Johnson AJ, Zywiel MG, Stroh DA, Marker DR, Mont MA. 2010. Should Gram stains have a role in diagnosing hip arthroplasty infections? Clin. Orthop. Relat. Res. 468:2387–2391. 10.1007/s11999-009-1216-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Spangehl MJ, Masri BA, O'Connell JX, Duncan CP. 1999. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J. Bone Joint Surg. Am. 81:672–683 [DOI] [PubMed] [Google Scholar]
- 302.Atkins BL, Athanasou N, Deeks JJ, Crook DW, Simpson H, Peto TE, McLardy-Smith P, Berendt AR, OSIRIS Collaborative Study Group 1998. Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. J. Clin. Microbiol. 36:2932–2939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Kamme C, Lindberg L. 1981. Aerobic and anaerobic bacteria in deep infections after total hip arthroplasty: differential diagnosis between infectious and non-infectious loosening. Clin. Orthop. Relat. Res. 154:201–207 [PubMed] [Google Scholar]
- 304.Marin M, Garcia-Lechuz JM, Alonso P, Villanueva M, Alcala L, Gimeno M, Cercenado E, Sanchez-Somolinos M, Radice C, Bouza E. 2012. Role of universal 16S rRNA gene PCR and sequencing in diagnosis of prosthetic joint infection. J. Clin. Microbiol. 50:583–589. 10.1128/JCM.00170-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Hughes HC, Newnham R, Athanasou N, Atkins BL, Bejon P, Bowler IC. 2011. Microbiological diagnosis of prosthetic joint infections: a prospective evaluation of four bacterial culture media in the routine laboratory. Clin. Microbiol. Infect. 17:1528–1530. 10.1111/j.1469-0691.2011.03597.x [DOI] [PubMed] [Google Scholar]
- 306.Shannon SK, Mandrekar J, Gustafson DR, Rucinski SL, Dailey AL, Segner RE, Burman MK, Boelman KJ, Lynch DT, Rosenblatt JE, Patel R. 2013. Anaerobic thioglycolate broth culture for recovery of Propionibacterium acnes from shoulder tissue and fluid specimens. J. Clin. Microbiol. 51:731–732. 10.1128/JCM.02695-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Mackowiak PA, Jones SR, Smith JW. 1978. Diagnostic value of sinus-tract cultures in chronic osteomyelitis. JAMA 239:2772–2775 [DOI] [PubMed] [Google Scholar]
- 308.Tetreault MW, Wetters NG, Aggarwal VK, Moric M, Segreti J, Huddleston JI, III, Parvizi J, Della Valle CJ. 2013. Should draining wounds and sinuses associated with hip and knee arthroplasties be cultured? J. Arthroplasty 28:133–136. 10.1016/j.arth.2013.04.057 [DOI] [PubMed] [Google Scholar]
- 309.Cune J, Soriano A, Martinez JC, Garcia S, Mensa J. 2009. A superficial swab culture is useful for microbiologic diagnosis in acute prosthetic joint infections. Clin. Orthop. Relat. Res. 467:531–535. 10.1007/s11999-008-0553-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Aggarwal VK, Higuera C, Deirmengian G, Parvizi J, Austin MS. 2013. Swab cultures are not as effective as tissue cultures for diagnosis of periprosthetic joint infection. Clin. Orthop. Relat. Res. 471:3196–3203. 10.1007/s11999-013-2974-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Bori G, Soriano A, Garcia S, Gallart X, Mallofre C, Mensa J. 2009. Neutrophils in frozen section and type of microorganism isolated at the time of resection arthroplasty for the treatment of infection. Arch. Orthop. Trauma Surg. 129:591–595. 10.1007/s00402-008-0679-6 [DOI] [PubMed] [Google Scholar]
- 312.Mirra JM, Amstutz HC, Matos M, Gold R. 1976. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin. Orthop. Relat. Res. 117:221–240 [PubMed] [Google Scholar]
- 313.Feldman DS, Lonner JH, Desai P, Zuckerman JD. 1995. The role of intraoperative frozen sections in revision total joint arthroplasty. J. Bone Joint Surg. Am. 77:1807–1813 [DOI] [PubMed] [Google Scholar]
- 314.Morawietz L, Classen RA, Schroder JH, Dynybil C, Perka C, Skwara A, Neidel J, Gehrke T, Frommelt L, Hansen T, Otto M, Barden B, Aigner T, Stiehl P, Schubert T, Meyer-Scholten C, Konig A, Strobel P, Rader CP, Kirschner S, Lintner F, Ruther W, Bos I, Hendrich C, Kriegsmann J, Krenn V. 2006. Proposal for a histopathological consensus classification of the periprosthetic interface membrane. J. Clin. Pathol. 59:591–597. 10.1136/jcp.2005.027458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Bori G, Munoz-Mahamud E, Garcia S, Mallofre C, Gallart X, Bosch J, Garcia E, Riba J, Mensa J, Soriano A. 2011. Interface membrane is the best sample for histological study to diagnose prosthetic joint infection. Mod. Pathol. 24:579–584. 10.1038/modpathol.2010.219 [DOI] [PubMed] [Google Scholar]
- 316.Janz V, Wassilew GI, Hasart O, Matziolis G, Tohtz S, Perka C. 2013. Evaluation of sonicate fluid cultures in comparison to histological analysis of the periprosthetic membrane for the detection of periprosthetic joint infection. Int. Orthop. 37:931–936. 10.1007/s00264-013-1853-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Dodson CC, Craig EV, Cordasco FA, Dines DM, Dines JS, Dicarlo E, Brause BD, Warren RF. 2010. Propionibacterium acnes infection after shoulder arthroplasty: a diagnostic challenge. J. Shoulder Elbow Surg. 19:303–307. 10.1016/j.jse.2009.07.065 [DOI] [PubMed] [Google Scholar]
- 318.Tsaras G, Maduka-Ezeh A, Inwards CY, Mabry T, Erwin PJ, Murad MH, Montori VM, West CP, Osmon DR, Berbari EF. 2012. Utility of intraoperative frozen section histopathology in the diagnosis of periprosthetic joint infection: a systematic review and meta-analysis. J. Bone Joint Surg. Am. 94:1700–1711. 10.2106/JBJS.J.00756 [DOI] [PubMed] [Google Scholar]
- 319.Suda AJ, Kommerell M, Geiss HK, Burckhardt I, Zimmermann S, Zeifang F, Lehner B. 2013. Prosthetic infection: improvement of diagnostic procedures using 16S ribosomal deoxyribonucleic acid polymerase chain reaction. Int. Orthop. 37:2515–2521. 10.1007/s00264-013-2038-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Bjerkan G, Witso E, Nor A, Viset T, Loseth K, Lydersen S, Persen L, Bergh K. 2012. A comprehensive microbiological evaluation of fifty-four patients undergoing revision surgery due to prosthetic joint loosening. J. Med. Microbiol. 61:572–581. 10.1099/jmm.0.036087-0 [DOI] [PubMed] [Google Scholar]
- 321.Trampuz A, Osmon DR, Hanssen AD, Steckelberg JM, Patel R. 2003. Molecular and antibiofilm approaches to prosthetic joint infection. Clin. Orthop. Relat. Res. 414:69–88. 10.1097/01.blo.0000087324.60612.93 [DOI] [PubMed] [Google Scholar]
- 322.Tunney MM, Patrick S, Gorman SP, Nixon JR, Anderson N, Davis RI, Hanna D, Ramage G. 1998. Improved detection of infection in hip replacements. A currently underestimated problem. J. Bone Joint Surg. Br. 80:568–572 [DOI] [PubMed] [Google Scholar]
- 323.Trampuz A, Piper KE, Hanssen AD, Osmon DR, Cockerill FR, Steckelberg JM, Patel R. 2006. Sonication of explanted prosthetic components in bags for diagnosis of prosthetic joint infection is associated with risk of contamination. J. Clin. Microbiol. 44:628–631. 10.1128/JCM.44.2.628-631.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Holinka J, Bauer L, Hirschl AM, Graninger W, Windhager R, Presterl E. 2011. Sonication cultures of explanted components as an add-on test to routinely conducted microbiological diagnostics improve pathogen detection. J. Orthop. Res. 29:617–622. 10.1002/jor.21286 [DOI] [PubMed] [Google Scholar]
- 325.Esteban J, Gomez-Barrena E, Cordero J, Martin-de-Hijas NZ, Kinnari TJ, Fernandez-Roblas R. 2008. Evaluation of quantitative analysis of cultures from sonicated retrieved orthopedic implants in diagnosis of orthopedic infection. J. Clin. Microbiol. 46:488–492. 10.1128/JCM.01762-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Achermann Y, Vogt M, Leunig M, Wust J, Trampuz A. 2010. Improved diagnosis of periprosthetic joint infection by multiplex PCR of sonication fluid from removed implants. J. Clin. Microbiol. 48:1208–1214. 10.1128/JCM.00006-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Nguyen LL, Nelson CL, Saccente M, Smeltzer MS, Wassell DL, McLaren SG. 2002. Detecting bacterial colonization of implanted orthopaedic devices by ultrasonication. Clin. Orthop. Relat. Res. 403:29–37. 10.1097/00003086-200210000-00006 [DOI] [PubMed] [Google Scholar]
- 328.Portillo ME, Salvado M, Trampuz A, Plasencia V, Rodriguez-Villasante M, Sorli L, Puig L, Horcajada JP. 2013. Sonication versus vortexing of implants for diagnosis of prosthetic joint infection. J. Clin. Microbiol. 51:591–594. 10.1128/JCM.02482-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Kobayashi H, Oethinger M, Tuohy MJ, Procop GW, Bauer TW. 2009. Improved detection of biofilm-formative bacteria by vortexing and sonication: a pilot study. Clin. Orthop. Relat. Res. 467:1360–1364. 10.1007/s11999-008-0609-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Sorli L, Puig L, Torres-Claramunt R, Gonzalez A, Alier A, Knobel H, Salvado M, Horcajada JP. 2012. The relationship between microbiology results in the second of a two-stage exchange procedure using cement spacers and the outcome after revision total joint replacement for infection: the use of sonication to aid bacteriological analysis. J. Bone Joint Surg. Br. 94:249–253. 10.1302/0301-620X.94B2.27779 [DOI] [PubMed] [Google Scholar]
- 331.Mariconda M, Ascione T, Balato G, Rotondo R, Smeraglia F, Costa GG, Conte M. 2013. Sonication of antibiotic-loaded cement spacers in a two-stage revision protocol for infected joint arthroplasty. BMC Musculoskelet. Disord. 14:193. 10.1186/1471-2474-14-193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Tunney MM, Patrick S, Curran MD, Ramage G, Hanna D, Nixon JR, Gorman SP, Davis RI, Anderson N. 1999. Detection of prosthetic hip infection at revision arthroplasty by immunofluorescence microscopy and PCR amplification of the bacterial 16S rRNA gene. J. Clin. Microbiol. 37:3281–3290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Mariani BD, Martin DS, Levine MJ, Booth RE, Jr, Tuan RS. 1996. The Coventry Award. Polymerase chain reaction detection of bacterial infection in total knee arthroplasty. Clin. Orthop. Relat. Res. 331:11–22 [DOI] [PubMed] [Google Scholar]
- 334.Gallo J, Kolar M, Dendis M, Loveckova Y, Sauer P, Zapletalova J, Koukalova D. 2008. Culture and PCR analysis of joint fluid in the diagnosis of prosthetic joint infection. New Microbiol. 31:97–104 http://www.newmicrobiologica.org/PUB/allegati_pdf/2008/1/97.pdf [PubMed] [Google Scholar]
- 335.Vandercam B, Jeumont S, Cornu O, Yombi JC, Lecouvet F, Lefevre P, Irenge LM, Gala JL. 2008. Amplification-based DNA analysis in the diagnosis of prosthetic joint infection. J. Mol. Diagn. 10:537–543. 10.2353/jmoldx.2008.070137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Panousis K, Grigoris P, Butcher I, Rana B, Reilly JH, Hamblen DL. 2005. Poor predictive value of broad-range PCR for the detection of arthroplasty infection in 92 cases. Acta Orthop. 76:341–346 http://informahealthcare.com/doi/full/10.1080/00016470510030805 [PubMed] [Google Scholar]
- 337.Bergin PF, Doppelt JD, Hamilton WG, Mirick GE, Jones AE, Sritulanondha S, Helm JM, Tuan RS. 2010. Detection of periprosthetic infections with use of ribosomal RNA-based polymerase chain reaction. J. Bone Joint Surg. Am. 92:654–663. 10.2106/JBJS.I.00400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Esteban J, Alonso-Rodriguez N, del-Prado G, Ortiz-Perez A, Molina-Manso D, Cordero-Ampuero J, Sandoval E, Fernandez-Roblas R, Gomez-Barrena E. 2012. PCR-hybridization after sonication improves diagnosis of implant-related infection. Acta Orthop. 83:299–304. 10.3109/17453674.2012.693019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Gomez E, Cazanave C, Cunningham SA, Greenwood-Quaintance KE, Steckelberg JM, Uhl JR, Hanssen AD, Karau MJ, Schmidt SM, Osmon DR, Berbari EF, Mandrekar J, Patel R. 2012. Prosthetic joint infection diagnosis using broad-range PCR of biofilms dislodged from knee and hip arthroplasty surfaces using sonication. J. Clin. Microbiol. 50:3501–3508. 10.1128/JCM.00834-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Portillo ME, Salvado M, Sorli L, Alier A, Martinez S, Trampuz A, Gomez J, Puig L, Horcajada JP. 2012. Multiplex PCR of sonication fluid accurately differentiates between prosthetic joint infection and aseptic failure. J. Infect. 65:541–548. 10.1016/j.jinf.2012.08.018 [DOI] [PubMed] [Google Scholar]
- 341.Moojen DJ, van Hellemondt G, Vogely HC, Burger BJ, Walenkamp GH, Tulp NJ, Schreurs BW, de Meulemeester FR, Schot CS, van de Pol I, Fujishiro T, Schouls LM, Bauer TW, Dhert WJ. 2010. Incidence of low-grade infection in aseptic loosening of total hip arthroplasty. Acta Orthop. 81:667–673. 10.3109/17453674.2010.525201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Greenwood-Quaintance KE, Uhl JR, Hanssen AD, Sampath R, Mandrekar JN, Patel R. 29 November 2013. Diagnosis of prosthetic joint infection by use of PCR-electrospray ionization mass spectrometry. J. Clin. Microbiol. 10.1128/JCM.03217-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Melendez D, Uhl JR, Greenwood-Quaintance K, Hanssen A, Patel R. 2013. Molecular microbiologic detection of prosthetic joint infection (PJI) using the Abbott PLEX-ID system on synovial fluid, abstr 1844 Abstr. 113th Gen. Meet. Am. Soc. Microbiol. [Google Scholar]
- 344.Jacovides CL, Kreft R, Adeli B, Hozack B, Ehrlich GD, Parvizi J. 2012. Successful identification of pathogens by polymerase chain reaction (PCR)-based electron spray ionization time-of-flight mass spectrometry (ESI-TOF-MS) in culture-negative periprosthetic joint infection. J. Bone Joint Surg. Am. 94:2247–2254. 10.2106/JBJS.L.00210 [DOI] [PubMed] [Google Scholar]
- 345.Bejon P, Berendt A, Atkins BL, Green N, Parry H, Masters S, McLardy-Smith P, Gundle R, Byren I. 2010. Two-stage revision for prosthetic joint infection: predictors of outcome and the role of reimplantation microbiology. J. Antimicrob. Chemother. 65:569–575. 10.1093/jac/dkp469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Berbari EF, Osmon DR, Duffy MC, Harmssen RN, Mandrekar JN, Hanssen AD, Steckelberg JM. 2006. Outcome of prosthetic joint infection in patients with rheumatoid arthritis: the impact of medical and surgical therapy in 200 episodes. Clin. Infect. Dis. 42:216–223. 10.1086/498507 [DOI] [PubMed] [Google Scholar]
- 347.Diaz-Ledezma C, Higuera CA, Parvizi J. 2013. Success after treatment of periprosthetic joint infection: a Delphi-based international multidisciplinary consensus. Clin. Orthop. Relat. Res. 471:2374–2382. 10.1007/s11999-013-2866-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Koyonos L, Zmistowski B, Della Valle CJ, Parvizi J. 2011. Infection control rate of irrigation and debridement for periprosthetic joint infection. Clin. Orthop. Relat. Res. 469:3043–3048. 10.1007/s11999-011-1910-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Byren I, Bejon P, Atkins BL, Angus B, Masters S, McLardy-Smith P, Gundle R, Berendt A. 2009. One hundred and twelve infected arthroplasties treated with ‘DAIR' (debridement, antibiotics and implant retention): antibiotic duration and outcome. J. Antimicrob. Chemother. 63:1264–1271. 10.1093/jac/dkp107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.El Helou OC, Berbari EF, Lahr BD, Eckel-Passow JE, Razonable RR, Sia IG, Virk A, Walker RC, Steckelberg JM, Wilson WR, Hanssen AD, Osmon DR. 2010. Efficacy and safety of rifampin containing regimen for staphylococcal prosthetic joint infections treated with debridement and retention. Eur. J. Clin. Microbiol. Infect. Dis. 29:961–967. 10.1007/s10096-010-0952-9 [DOI] [PubMed] [Google Scholar]
- 351.Azzam KA, Seeley M, Ghanem E, Austin MS, Purtill JJ, Parvizi J. 2010. Irrigation and debridement in the management of prosthetic joint infection: traditional indications revisited. J. Arthroplasty 25:1022–1027. 10.1016/j.arth.2010.01.104 [DOI] [PubMed] [Google Scholar]
- 352.Leone S, Borre S, Monforte A, Mordente G, Petrosillo N, Signore A, Venditti M, Viale P, Nicastri E, Lauria FN, Carosi G, Moroni M, Ippolito G, GISIG Working Group on Prosthetic Joint Infections 2010. Consensus document on controversial issues in the diagnosis and treatment of prosthetic joint infections. Int. J. Infect. Dis. 14(Suppl 4):S67–S77. 10.1016/j.ijid.2010.05.005 [DOI] [PubMed] [Google Scholar]
- 353.Silva M, Tharani R, Schmalzried TP. 2002. Results of direct exchange or debridement of the infected total knee arthroplasty. Clin. Orthop. Relat. Res. 404:125–131. 10.1097/00003086-200211000-00022 [DOI] [PubMed] [Google Scholar]
- 354.Zimmerli W, Trampuz A, Ochsner PE. 2004. Prosthetic-joint infections. N. Engl. J. Med. 351:1645–1654. 10.1056/NEJMra040181 [DOI] [PubMed] [Google Scholar]
- 355.Barberan J, Aguilar L, Carroquino G, Gimenez MJ, Sanchez B, Martinez D, Prieto J. 2006. Conservative treatment of staphylococcal prosthetic joint infections in elderly patients. Am. J. Med. 119:993.e7-993.e10. 10.1016/j.amjmed.2006.03.036 [DOI] [PubMed] [Google Scholar]
- 356.Crockarell JR, Hanssen AD, Osmon DR, Morrey BF. 1998. Treatment of infection with debridement and retention of the components following hip arthroplasty. J. Bone Joint Surg. Am. 80:1306–1313 [DOI] [PubMed] [Google Scholar]
- 357.Odum SM, Fehring TK, Lombardi AV, Zmistowski BM, Brown NM, Luna JT, Fehring KA, Hansen EN. 2011. Irrigation and debridement for periprosthetic infections: does the organism matter? J. Arthroplasty 26:114–118. 10.1016/j.arth.2011.03.031 [DOI] [PubMed] [Google Scholar]
- 358.Sukeik M, Patel S, Haddad FS. 2012. Aggressive early debridement for treatment of acutely infected cemented total hip arthroplasty. Clin. Orthop. Relat. Res. 470:3164–3170. 10.1007/s11999-012-2500-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Choong PF, Dowsey MM, Carr D, Daffy J, Stanley P. 2007. Risk factors associated with acute hip prosthetic joint infections and outcome of treatment with a rifampin based regimen. Acta Orthop. 78:755–765. 10.1080/17453670710014527 [DOI] [PubMed] [Google Scholar]
- 360.Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. 1997. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J. Arthroplasty 12:426–433. 10.1016/S0883-5403(97)90199-6 [DOI] [PubMed] [Google Scholar]
- 361.Berdal JE, Skramm I, Mowinckel P, Gulbrandsen P, Bjornholt JV. 2005. Use of rifampicin and ciprofloxacin combination therapy after surgical debridement in the treatment of early manifestation prosthetic joint infections. Clin. Microbiol. Infect. 11:843–845. 10.1111/j.1469-0691.2005.01230.x [DOI] [PubMed] [Google Scholar]
- 362.Engesaeter LB, Dale H, Schrama JC, Hallan G, Lie SA. 2011. Surgical procedures in the treatment of 784 infected THAs reported to the Norwegian Arthroplasty Register. Acta Orthop. 82:530–537. 10.3109/17453674.2011.623572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Romano CL, Manzi G, Logoluso N, Romano D. 2012. Value of debridement and irrigation for the treatment of peri-prosthetic infections. A systematic review. Hip Int. 22(Suppl 8):S19–S24. 10.5301/HIP.2012.9566 [DOI] [PubMed] [Google Scholar]
- 364.Zimmerli W, Widmer AF, Blatter M, Frei R, Ochsner PE. 1998. Role of rifampin for treatment of orthopedic implant-related staphylococcal infections: a randomized controlled trial. Foreign-Body Infection (FBI) Study Group. JAMA 279:1537–1541 [DOI] [PubMed] [Google Scholar]
- 365.Martinez-Pastor JC, Munoz-Mahamud E, Vilchez F, Garcia-Ramiro S, Bori G, Sierra J, Martinez JA, Font L, Mensa J, Soriano A. 2009. Outcome of acute prosthetic joint infections due to Gram-negative bacilli treated with open debridement and retention of the prosthesis. Antimicrob. Agents Chemother. 53:4772–4777. 10.1128/AAC.00188-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Widmer AF, Gaechter A, Ochsner PE, Zimmerli W. 1992. Antimicrobial treatment of orthopedic implant-related infections with rifampin combinations. Clin. Infect. Dis. 14:1251–1253. 10.1093/clinids/14.6.1251 [DOI] [PubMed] [Google Scholar]
- 367.Widmer AF, Frei R, Rajacic Z, Zimmerli W. 1990. Correlation between in vivo and in vitro efficacy of antimicrobial agents against foreign body infections. J. Infect. Dis. 162:96–102. 10.1093/infdis/162.1.96 [DOI] [PubMed] [Google Scholar]
- 368.Forrest GN, Tamura K. 2010. Rifampin combination therapy for nonmycobacterial infections. Clin. Microbiol. Rev. 23:14–34. 10.1128/CMR.00034-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Vilchez F, Martinez-Pastor JC, Garcia-Ramiro S, Bori G, Macule F, Sierra J, Font L, Mensa J, Soriano A. 2011. Outcome and predictors of treatment failure in early post-surgical prosthetic joint infections due to Staphylococcus aureus treated with debridement. Clin. Microbiol. Infect. 17:439–444. 10.1111/j.1469-0691.2010.03244.x [DOI] [PubMed] [Google Scholar]
- 370.Tice AD, Hoaglund PA, Shoultz DA. 2003. Outcomes of osteomyelitis among patients treated with outpatient parenteral antimicrobial therapy. Am. J. Med. 114:723–728. 10.1016/S0002-9343(03)00231-6 [DOI] [PubMed] [Google Scholar]
- 371.Wieland BW, Marcantoni JR, Bommarito KM, Warren DK, Marschall J. 2012. A retrospective comparison of ceftriaxone versus oxacillin for osteoarticular infections due to methicillin-susceptible Staphylococcus aureus. Clin. Infect. Dis. 54:585–590. 10.1093/cid/cir857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Bradbury T, Fehring TK, Taunton M, Hanssen A, Azzam K, Parvizi J, Odum SM. 2009. The fate of acute methicillin-resistant Staphylococcus aureus periprosthetic knee infections treated by open debridement and retention of components. J. Arthroplasty 24:101–104. 10.1016/j.arth.2009.04.028 [DOI] [PubMed] [Google Scholar]
- 373.Siddiqui MM, Lo NN, Ab Rahman S, Chin PL, Chia SL, Yeo SJ. 2013. Two-year outcome of early deep MRSA infections after primary total knee arthroplasty: a joint registry review. J. Arthroplasty 28:44–48. 10.1016/j.arth.2012.04.007 [DOI] [PubMed] [Google Scholar]
- 374.Aboltins CA, Page MA, Buising KL, Jenney AW, Daffy JR, Choong PF, Stanley PA. 2007. Treatment of staphylococcal prosthetic joint infections with debridement, prosthesis retention and oral rifampicin and fusidic acid. Clin. Microbiol. Infect. 13:586–591. 10.1111/j.1469-0691.2007.01691.x [DOI] [PubMed] [Google Scholar]
- 375.Corona Perez-Cardona PS, Barro Ojeda V, Rodriguez Pardo D, Pigrau Serrallach C, Guerra Farfan E, Amat Mateu C, Flores Sanchez X. 2012. Clinical experience with daptomycin for the treatment of patients with knee and hip periprosthetic joint infections. J. Antimicrob. Chemother. 67:1749–1754. 10.1093/jac/dks119 [DOI] [PubMed] [Google Scholar]
- 376.Byren I, Rege S, Campanaro E, Yankelev S, Anastasiou D, Kuropatkin G, Evans R. 2012. Randomized controlled trial of the safety and efficacy of daptomycin versus standard-of-care therapy for management of patients with osteomyelitis associated with prosthetic devices undergoing two-stage revision arthroplasty. Antimicrob. Agents Chemother. 56:5626–5632. 10.1128/AAC.00038-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Saleh-Mghir A, Muller-Serieys C, Dinh A, Massias L, Cremieux AC. 2011. Adjunctive rifampin is crucial to optimizing daptomycin efficacy against rabbit prosthetic joint infection due to methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 55:4589–4593. 10.1128/AAC.00675-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.John AK, Baldoni D, Haschke M, Rentsch K, Schaerli P, Zimmerli W, Trampuz A. 2009. Efficacy of daptomycin in implant-associated infection due to methicillin-resistant Staphylococcus aureus: importance of combination with rifampin. Antimicrob. Agents Chemother. 53:2719–2724. 10.1128/AAC.00047-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Garrigos C, Murillo O, Euba G, Verdaguer R, Tubau F, Cabellos C, Cabo J, Ariza J. 2010. Efficacy of usual and high doses of daptomycin in combination with rifampin versus alternative therapies in experimental foreign-body infection by methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 54:5251–5256. 10.1128/AAC.00226-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Bassetti M, Vitale F, Melica G, Righi E, Di Biagio A, Molfetta L, Pipino F, Cruciani M, Bassetti D. 2005. Linezolid in the treatment of Gram-positive prosthetic joint infections. J. Antimicrob. Chemother. 55:387–390. 10.1093/jac/dki016 [DOI] [PubMed] [Google Scholar]
- 381.Nguyen S, Pasquet A, Legout L, Beltrand E, Dubreuil L, Migaud H, Yazdanpanah Y, Senneville E. 2009. Efficacy and tolerance of rifampicin-linezolid compared with rifampicin-cotrimoxazole combinations in prolonged oral therapy for bone and joint infections. Clin. Microbiol. Infect. 15:1163–1169. 10.1111/j.1469-0691.2009.02761.x [DOI] [PubMed] [Google Scholar]
- 382.Sherrell JC, Fehring TK, Odum S, Hansen E, Zmistowski B, Dennos A, Kalore N. 2011. The Chitranjan Ranawat Award: fate of two-stage reimplantation after failed irrigation and debridement for periprosthetic knee infection. Clin. Orthop. Relat. Res. 469:18–25. 10.1007/s11999-010-1434-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Ure KJ, Amstutz HC, Nasser S, Schmalzried TP. 1998. Direct-exchange arthroplasty for the treatment of infection after total hip replacement. An average ten-year follow-up. J. Bone Joint Surg. Am. 80:961–968 [DOI] [PubMed] [Google Scholar]
- 384.Buechel FF, Femino FP, D'Alessio J. 2004. Primary exchange revision arthroplasty for infected total knee replacement: a long-term study. Am. J. Orthop. 33:190–198 [PubMed] [Google Scholar]
- 385.Wroblewski BM. 1986. One-stage revision of infected cemented total hip arthroplasty. Clin. Orthop. Relat. Res. 211:103–107 [PubMed] [Google Scholar]
- 386.Raut VV, Siney PD, Wroblewski BM. 1994. One-stage revision of infected total hip replacements with discharging sinuses. J. Bone Joint Surg. Br. 76:721–724 [PubMed] [Google Scholar]
- 387.Whiteside LA, Peppers M, Nayfeh TA, Roy ME. 2011. Methicillin-resistant Staphylococcus aureus in TKA treated with revision and direct intra-articular antibiotic infusion. Clin. Orthop. Relat. Res. 469:26–33. 10.1007/s11999-010-1313-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Rudelli S, Uip D, Honda E, Lima AL. 2008. One-stage revision of infected total hip arthroplasty with bone graft. J. Arthroplasty 23:1165–1177. 10.1016/j.arth.2007.08.010 [DOI] [PubMed] [Google Scholar]
- 389.Buchholz HW, Elson RA, Engelbrecht E, Lodenkamper H, Rottger J, Siegel A. 1981. Management of deep infection of total hip replacement. J. Bone Joint Surg. Br. 63:342–353 [DOI] [PubMed] [Google Scholar]
- 390.Callaghan JJ, Katz RP, Johnston RC. 1999. One-stage revision surgery of the infected hip. A minimum 10-year followup study. Clin. Orthop. Relat. Res. 369:139–143 [DOI] [PubMed] [Google Scholar]
- 391.Hope PG, Kristinsson KG, Norman P, Elson RA. 1989. Deep infection of cemented total hip arthroplasties caused by coagulase-negative staphylococci. J. Bone Joint Surg. Br. 71:851–855 [DOI] [PubMed] [Google Scholar]
- 392.Lange J, Troelsen A, Thomsen RW, Soballe K. 2012. Chronic infections in hip arthroplasties: comparing risk of reinfection following one-stage and two-stage revision. A systematic review and meta-analysis. Clin. Epidemiol. 4:57–73. 10.2147/CLEP.S29025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Cui Q, Mihalko WM, Shields JS, Ries M, Saleh KJ. 2007. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J. Bone Joint Surg. Am. 89:871–882. 10.2106/JBJS.E.01070 [DOI] [PubMed] [Google Scholar]
- 394.Pitto RP, Spika IA. 2004. Antibiotic-loaded bone cement spacers in two-stage management of infected total knee arthroplasty. Int. Orthop. 28:129–133. 10.1007/s00264-004-0545-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Kalore NV, Maheshwari A, Sharma A, Cheng E, Gioe TJ. 2012. Is there a preferred articulating spacer technique for infected knee arthroplasty? A preliminary study. Clin. Orthop. Relat. Res. 470:228–235. 10.1007/s11999-011-2037-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Jamsen E, Sheng P, Halonen P, Lehto MU, Moilanen T, Pajamaki J, Puolakka T, Konttinen YT. 2006. Spacer prostheses in two-stage revision of infected knee arthroplasty. Int. Orthop. 30:257–261. 10.1007/s00264-006-0102-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Calton TF, Fehring TK, Griffin WL. 1997. Bone loss associated with the use of spacer blocks in infected total knee arthroplasty. Clin. Orthop. Relat. Res. 345:148–154 [PubMed] [Google Scholar]
- 398.Haddad FS, Masri BA, Campbell D, McGraw RW, Beauchamp CP, Duncan CP. 2000. The PROSTALAC functional spacer in two-stage revision for infected knee replacements. Prosthesis of antibiotic-loaded acrylic cement. J. Bone Joint Surg. Br. 82:807–812 http://www.bjj.boneandjoint.org.uk/content/82-B/6/807.long [DOI] [PubMed] [Google Scholar]
- 399.Emerson RH, Jr, Muncie M, Tarbox TR, Higgins LL. 2002. Comparison of a static with a mobile spacer in total knee infection. Clin. Orthop. Relat. Res. 404:132–138. 10.1097/00003086-200211000-00023 [DOI] [PubMed] [Google Scholar]
- 400.Freeman MG, Fehring TK, Odum SM, Fehring K, Griffin WL, Mason JB. 2007. Functional advantage of articulating versus static spacers in 2-stage revision for total knee arthroplasty infection. J. Arthroplasty 22:1116–1121. 10.1016/j.arth.2007.04.009 [DOI] [PubMed] [Google Scholar]
- 401.Voleti PB, Baldwin KD, Lee GC. 2013. Use of static or articulating spacers for infection following total knee arthroplasty: a systematic literature review. J. Bone Joint Surg. Am. 95:1594–1599. 10.2106/JBJS.L.01461 [DOI] [PubMed] [Google Scholar]
- 402.Masri BA, Duncan CP, Beauchamp CP. 1998. Long-term elution of antibiotics from bone-cement: an in vivo study using the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) system. J. Arthroplasty 13:331–338 [DOI] [PubMed] [Google Scholar]
- 403.Sterling GJ, Crawford S, Potter JH, Koerbin G, Crawford R. 2003. The pharmacokinetics of Simplex-tobramycin bone cement. J. Bone Joint Surg. Br. 85:646–649. 10.1302/0301-620X.85B5.13746 [DOI] [PubMed] [Google Scholar]
- 404.Penner MJ, Masri BA, Duncan CP. 1996. Elution characteristics of vancomycin and tobramycin combined in acrylic bone-cement. J. Arthroplasty 11:939–944. 10.1016/S0883-5403(96)80135-5 [DOI] [PubMed] [Google Scholar]
- 405.Cabo J, Euba G, Saborido A, Gonzalez-Panisello M, Dominguez MA, Agullo JL, Murillo O, Verdaguer R, Ariza J. 2011. Clinical outcome and microbiological findings using antibiotic-loaded spacers in two-stage revision of prosthetic joint infections. J. Infect. 63:23–31. 10.1016/j.jinf.2011.04.014 [DOI] [PubMed] [Google Scholar]
- 406.Choi HR, Freiberg AA, Malchau H, Rubash HE, Kwon YM. 13 August 2013, posting date The fate of unplanned retention of prosthetic articulating spacers for infected total hip and total knee arthroplasty. J. Arthroplasty [Epub ahead of print.] 10.1016/j.arth.2013.07.013 [DOI] [PubMed] [Google Scholar]
- 407.Stockley I, Mockford BJ, Hoad-Reddick A, Norman P. 2008. The use of two-stage exchange arthroplasty with depot antibiotics in the absence of long-term antibiotic therapy in infected total hip replacement. J. Bone Joint Surg. Br. 90:145–148. 10.1302/0301-620X.90B2.19855 [DOI] [PubMed] [Google Scholar]
- 408.Fleck EE, Spangehl MJ, Rapuri VR, Beauchamp CP. 2011. An articulating antibiotic spacer controls infection and improves pain and function in a degenerative septic hip. Clin. Orthop. Relat. Res. 469:3055–3064. 10.1007/s11999-011-1903-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Jiranek WA, Hanssen AD, Greenwald AS. 2006. Antibiotic-loaded bone cement for infection prophylaxis in total joint replacement. J. Bone Joint Surg. Am. 88:2487–2500. 10.2106/JBJS.E.01126 [DOI] [PubMed] [Google Scholar]
- 410.Iarikov D, Demian H, Rubin D, Alexander J, Nambiar S. 2012. Choice and doses of antibacterial agents for cement spacers in treatment of prosthetic joint infections: review of published studies. Clin. Infect. Dis. 55:1474–1480. 10.1093/cid/cis735 [DOI] [PubMed] [Google Scholar]
- 411.Cabrita HB, Croci AT, Camargo OP, Lima AL. 2007. Prospective study of the treatment of infected hip arthroplasties with or without the use of an antibiotic-loaded cement spacer. Clinics 62:99–108. 10.1590/S1807-59322007000200002 [DOI] [PubMed] [Google Scholar]
- 412.Trampuz A, Zimmerli W. 2005. Prosthetic joint infections: update in diagnosis and treatment. Swiss Med. Wkly. 135:243–251 http://www.smw.ch/docs/pdf200x/2005/17/smw-10934.pdf [DOI] [PubMed] [Google Scholar]
- 413.Silvestre A, Almeida F, Renovell P, Morante E, Lopez R. 2013. Revision of infected total knee arthroplasty: two-stage reimplantation using an antibiotic-impregnated static spacer. Clin. Orthop. Surg. 5:180–187. 10.4055/cios.2013.5.3.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.McKenna PB, O'Shea K, Masterson EL. 2009. Two-stage revision of infected hip arthroplasty using a shortened post-operative course of antibiotics. Arch. Orthop. Trauma Surg. 129:489–494. 10.1007/s00402-008-0683-x [DOI] [PubMed] [Google Scholar]
- 415.Zywiel MG, Johnson AJ, Stroh DA, Martin J, Marker DR, Mont MA. 2011. Prophylactic oral antibiotics reduce reinfection rates following two-stage revision total knee arthroplasty. Int. Orthop. 35:37–42. 10.1007/s00264-010-0992-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Betsch BY, Eggli S, Siebenrock KA, Tauber MG, Muhlemann K. 2008. Treatment of joint prosthesis infection in accordance with current recommendations improves outcome. Clin. Infect. Dis. 46:1221–1226. 10.1086/529436 [DOI] [PubMed] [Google Scholar]
- 417.Mortazavi SM, Vegari D, Ho A, Zmistowski B, Parvizi J. 2011. Two-stage exchange arthroplasty for infected total knee arthroplasty: predictors of failure. Clin. Orthop. Relat. Res. 469:3049–3054. 10.1007/s11999-011-2030-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Hirakawa K, Stulberg BN, Wilde AH, Bauer TW, Secic M. 1998. Results of 2-stage reimplantation for infected total knee arthroplasty. J. Arthroplasty 13:22–28. 10.1016/S0883-5403(98)90071-7 [DOI] [PubMed] [Google Scholar]
- 419.Hanssen AD, Rand JA, Osmon DR. 1994. Treatment of the infected total knee arthroplasty with insertion of another prosthesis. The effect of antibiotic-impregnated bone cement. Clin. Orthop. Relat. Res. 309:44–55 [PubMed] [Google Scholar]
- 420.Rand JA, Bryan RS. 1983. Reimplantation for the salvage of an infected total knee arthroplasty. J. Bone Joint Surg. Am. 65:1081–1086 [PubMed] [Google Scholar]
- 421.Mont MA, Waldman BJ, Hungerford DS. 2000. Evaluation of preoperative cultures before second-stage reimplantation of a total knee prosthesis complicated by infection. A comparison-group study. J. Bone Joint Surg. Am. 82:1552–1557 http://jbjs.org/article.aspx?articleid=24465 [DOI] [PubMed] [Google Scholar]
- 422.Goldman RT, Scuderi GR, Insall JN. 1996. 2-stage reimplantation for infected total knee replacement. Clin. Orthop. Relat. Res. 331:118–124. 10.1097/00003086-199610000-00016 [DOI] [PubMed] [Google Scholar]
- 423.Haleem AA, Berry DJ, Hanssen AD. 2004. Mid-term to long-term followup of two-stage reimplantation for infected total knee arthroplasty. Clin. Orthop. Relat. Res. 428:35–39. 10.1097/01.blo.0000147713.64235.73 [DOI] [PubMed] [Google Scholar]
- 424.Jamsen E, Stogiannidis I, Malmivaara A, Pajamaki J, Puolakka T, Konttinen YT. 2009. Outcome of prosthesis exchange for infected knee arthroplasty: the effect of treatment approach. Acta Orthop. 80:67–77. 10.1080/17453670902805064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Strickland JP, Sperling JW, Cofield RH. 2008. The results of two-stage re-implantation for infected shoulder replacement. J. Bone Joint Surg. Br. 90:460–465. 10.1302/0301-620X.90B4.20002 [DOI] [PubMed] [Google Scholar]
- 426.Kuiper JW, van den Bekerom MP, van der Stappen J, Nolte PA, Colen S. 2013. 2-stage revision recommended for treatment of fungal hip and knee prosthetic joint infections. Acta Orthop. 84:517–523. 10.3109/17453674.2013.859422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Zmistowski B, Tetreault MW, Alijanipour P, Chen AF, Della Valle CJ, Parvizi J. 2013. Recurrent periprosthetic joint infection: persistent or new infection? J. Arthroplasty 28:1486–1489. 10.1016/j.arth.2013.02.021 [DOI] [PubMed] [Google Scholar]
- 428.Hanssen AD, Trousdale RT, Osmon DR. 1995. Patient outcome with reinfection following reimplantation for the infected total knee arthroplasty. Clin. Orthop. Relat. Res. 321:55–67 [PubMed] [Google Scholar]
- 429.Pagnano MW, Trousdale RT, Hanssen AD. 1997. Outcome after reinfection following reimplantation hip arthroplasty. Clin. Orthop. Relat. Res. 337:192–204 [DOI] [PubMed] [Google Scholar]
- 430.Maheshwari AV, Gioe TJ, Kalore NV, Cheng EY. 2010. Reinfection after prior staged reimplantation for septic total knee arthroplasty: is salvage still possible? J. Arthroplasty 25:92–97. 10.1016/j.arth.2010.04.017 [DOI] [PubMed] [Google Scholar]
- 431.Azzam K, McHale K, Austin M, Purtill JJ, Parvizi J. 2009. Outcome of a second two-stage reimplantation for periprosthetic knee infection. Clin. Orthop. Relat. Res. 467:1706–1714. 10.1007/s11999-009-0739-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Mortazavi SM, O'Neil JT, Zmistowski B, Parvizi J, Purtill JJ. 2012. Repeat 2-stage exchange for infected total hip arthroplasty: a viable option? J. Arthroplasty 27:923–926.e1. 10.1016/j.arth.2011.11.006 [DOI] [PubMed] [Google Scholar]
- 433.Kalra KP, Lin KK, Bozic KJ, Ries MD. 2010. Repeat 2-stage revision for recurrent infection of total hip arthroplasty. J. Arthroplasty 25:880–884. 10.1016/j.arth.2009.12.010 [DOI] [PubMed] [Google Scholar]
- 434.Backe HA, Jr, Wolff DA, Windsor RE. 1996. Total knee replacement infection after 2-stage reimplantation: results of subsequent 2-stage reimplantation. Clin. Orthop. Relat. Res. 331:125–131. 10.1097/00003086-199610000-00017 [DOI] [PubMed] [Google Scholar]
- 435.Falahee MH, Matthews LS, Kaufer H. 1987. Resection arthroplasty as a salvage procedure for a knee with infection after a total arthroplasty. J. Bone Joint Surg. Am. 69:1013–1021 [PubMed] [Google Scholar]
- 436.Mabry TM, Jacofsky DJ, Haidukewych GJ, Hanssen AD. 2007. Comparison of intramedullary nailing and external fixation knee arthrodesis for the infected knee replacement. Clin. Orthop. Relat. Res. 464:11–15. 10.1097/BLO.0b013e31806a9191 [DOI] [PubMed] [Google Scholar]
- 437.Castellanos J, Flores X, Llusa M, Chiriboga C, Navarro A. 1998. The Girdlestone pseudarthrosis in the treatment of infected hip replacements. Int. Orthop. 22:178–181. 10.1007/s002640050236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Grauer JD, Amstutz HC, O'Carroll PF, Dorey FJ. 1989. Resection arthroplasty of the hip. J. Bone Joint Surg. Am. 71:669–678 [PubMed] [Google Scholar]
- 439.Sierra RJ, Trousdale RT, Pagnano MW. 2003. Above-the-knee amputation after a total knee replacement: prevalence, etiology, and functional outcome. J. Bone Joint Surg. Am. 85:1000–1004 http://jbjs.org/article.aspx?articleid=25935 [DOI] [PubMed] [Google Scholar]
- 440.Krijnen MR, Wuisman PI. 2004. Emergency hemipelvectomy as a result of uncontrolled infection after total hip arthroplasty: two case reports. J. Arthroplasty 19:803–808. 10.1016/j.arth.2004.01.008 [DOI] [PubMed] [Google Scholar]
- 441.Fedorka CJ, Chen AF, McGarry WM, Parvizi J, Klatt BA. 2011. Functional ability after above-the-knee amputation for infected total knee arthroplasty. Clin. Orthop. Relat. Res. 469:1024–1032. 10.1007/s11999-010-1577-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Pavoni GL, Giannella M, Falcone M, Scorzolini L, Liberatore M, Carlesimo B, Serra P, Venditti M. 2004. Conservative medical therapy of prosthetic joint infections: retrospective analysis of an 8-year experience. Clin. Microbiol. Infect. 10:831–837. 10.1111/j.1469-0691.2004.00928.x [DOI] [PubMed] [Google Scholar]
- 443.Segreti J, Nelson JA, Trenholme GM. 1998. Prolonged suppressive antibiotic therapy for infected orthopedic prostheses. Clin. Infect. Dis. 27:711–713. 10.1086/514951 [DOI] [PubMed] [Google Scholar]
- 444.Tice AD, Rehm SJ, Dalovisio JR, Bradley JS, Martinelli LP, Graham DR, Gainer RB, Kunkel MJ, Yancey RW, Williams DN. 2004. Practice guidelines for outpatient parenteral antimicrobial therapy. IDSA guidelines. Clin. Infect. Dis. 38:1651–1672. 10.1086/420939 [DOI] [PubMed] [Google Scholar]
- 445.Moran E, Byren I, Atkins BL. 2010. The diagnosis and management of prosthetic joint infections. J. Antimicrob. Chemother. 65(Suppl 3):iii45–iii54. 10.1093/jac/dkq305 [DOI] [PubMed] [Google Scholar]
- 446.Giulieri SG, Graber P, Ochsner PE, Zimmerli W. 2004. Management of infection associated with total hip arthroplasty according to a treatment algorithm. Infection 32:222–228. 10.1007/s15010-004-4020-1 [DOI] [PubMed] [Google Scholar]
- 447.Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA. 2013. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am. J. Health Syst. Pharm. 70:195–283. 10.2146/ajhp120568 [DOI] [PubMed] [Google Scholar]
- 448.Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vandenbroucke-Grauls CM, Roosendaal R, Troelstra A, Box AT, Voss A, van der Tweel I, van Belkum A, Verbrugh HA, Vos MC. 2010. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N. Engl. J. Med. 362:9–17. 10.1056/NEJMoa0808939 [DOI] [PubMed] [Google Scholar]
- 449.Chen AF, Heyl AE, Xu PZ, Rao N, Klatt BA. 2013. Preoperative decolonization effective at reducing staphylococcal colonization in total joint arthroplasty patients. J. Arthroplasty 28:18–20. 10.1016/j.arth.2013.03.036 [DOI] [PubMed] [Google Scholar]
- 450.Chen AF, Wessel CB, Rao N. 2013. Staphylococcus aureus screening and decolonization in orthopaedic surgery and reduction of surgical site infections. Clin. Orthop. Relat. Res. 471:2383–2399. 10.1007/s11999-013-2875-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Huang SS, Septimus E, Kleinman K, Moody J, Hickok J, Avery TR, Lankiewicz J, Gombosev A, Terpstra L, Hartford F, Hayden MK, Jernigan JA, Weinstein RA, Fraser VJ, Haffenreffer K, Cui E, Kaganov RE, Lolans K, Perlin JB, Platt R. 2013. Targeted versus universal decolonization to prevent ICU infection. N. Engl. J. Med. 368:2255–2265. 10.1056/NEJMoa1207290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Webster J, Osborne S. 2007. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst. Rev. 2007:CD004985. 10.1002/14651858.CD004985.pub3 [DOI] [PubMed] [Google Scholar]
- 453.Johnson AJ, Kapadia BH, Daley JA, Molina CB, Mont MA. 2013. Chlorhexidine reduces infections in knee arthroplasty. J. Knee Surg. 26:213–218. 10.1055/s-0032-1329232 [DOI] [PubMed] [Google Scholar]
- 454.Farber NJ, Chen AF, Bartsch SM, Feigel JL, Klatt BA. 2013. No infection reduction using chlorhexidine wipes in total joint arthroplasty. Clin. Orthop. Relat. Res. 471:3120–3125. 10.1007/s11999-013-2920-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.AlBuhairan B, Hind D, Hutchinson A. 2008. Antibiotic prophylaxis for wound infections in total joint arthroplasty: a systematic review. J. Bone Joint Surg. Br. 90:915–919. 10.2106/JBJS.G.00637 [DOI] [PubMed] [Google Scholar]
- 456.Hill C, Flamant R, Mazas F, Evrard J. 1981. Prophylactic cefazolin versus placebo in total hip replacement. Report of a multicentre double-blind randomised trial. Lancet i:795–796 [DOI] [PubMed] [Google Scholar]
- 457.Sewick A, Makani A, Wu C, O'Donnell J, Baldwin KD, Lee GC. 2012. Does dual antibiotic prophylaxis better prevent surgical site infections in total joint arthroplasty? Clin. Orthop. Relat. Res. 470:2702–2707. 10.1007/s11999-012-2255-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Park M, Markus P, Matesic D, Li JT. 2006. Safety and effectiveness of a preoperative allergy clinic in decreasing vancomycin use in patients with a history of penicillin allergy. Ann. Allergy Asthma Immunol. 97:681–687. 10.1016/S1081-1206(10)61100-3 [DOI] [PubMed] [Google Scholar]
- 459.Meter JJ, Polly DW, Jr, Brueckner RP, Tenuta JJ, Asplund L, Hopkinson WJ. 1996. Effect of intraoperative blood loss on the serum level of cefazolin in patients managed with total hip arthroplasty. A prospective, controlled study. J. Bone Joint Surg. Am. 78:1201–1205 [DOI] [PubMed] [Google Scholar]
- 460.Nelson CL, Green TG, Porter RA, Warren RD. 1983. One day versus seven days of preventive antibiotic therapy in orthopedic surgery. Clin. Orthop. Relat. Res. 176:258–263 [PubMed] [Google Scholar]
- 461.Lidwell OM, Lowbury EJ, Whyte W, Blowers R, Stanley SJ, Lowe D. 1982. Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. BMJ 285:10–14. 10.1136/bmj.285.6334.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.Hooper GJ, Rothwell AG, Frampton C, Wyatt MC. 2011. Does the use of laminar flow and space suits reduce early deep infection after total hip and knee replacement? The ten-year results of the New Zealand Joint Registry. J. Bone Joint Surg. Br. 93:85–90. 10.1302/0301-620X.93B1.24862 [DOI] [PubMed] [Google Scholar]
- 463.Lautenschlager EP, Jacobs JJ, Marshall GW, Meyer PR., Jr 1976. Mechanical properties of bone cements containing large doses of antibiotic powders. J. Biomed. Mater. Res. 10:929–938. 10.1002/jbm.820100610 [DOI] [PubMed] [Google Scholar]
- 464.Parvizi J, Saleh KJ, Ragland PS, Pour AE, Mont MA. 2008. Efficacy of antibiotic-impregnated cement in total hip replacement. Acta Orthop. 79:335–341. 10.1080/17453670710015229 [DOI] [PubMed] [Google Scholar]
- 465.Lynch M, Esser MP, Shelley P, Wroblewski BM. 1987. Deep infection in Charnley low-friction arthroplasty. Comparison of plain and gentamicin-loaded cement. J. Bone Joint Surg. Br. 69:355–360 [DOI] [PubMed] [Google Scholar]
- 466.Chiu FY, Lin CF, Chen CM, Lo WH, Chaung TY. 2001. Cefuroxime-impregnated cement at primary total knee arthroplasty in diabetes mellitus. A prospective, randomised study. J. Bone Joint Surg. Br. 83:691–695. 10.1302/0301-620X.83B5.11737 [DOI] [PubMed] [Google Scholar]
- 467.Chiu FY, Chen CM, Lin CF, Lo WH. 2002. Cefuroxime-impregnated cement in primary total knee arthroplasty: a prospective, randomized study of three hundred and forty knees. J. Bone Joint Surg. Am. 84:759–762 http://jbjs.org/article.aspx?articleid=25407 [PubMed] [Google Scholar]
- 468.Hanssen AD. 2004. Prophylactic use of antibiotic bone cement: an emerging standard—in opposition. J. Arthroplasty 19(Suppl 1):73–77. 10.1016/j.arth.2004.04.006 [DOI] [PubMed] [Google Scholar]
- 469.American Dental Association, American Academy of Orthopedic Surgeons. 2003. Antibiotic prophylaxis for dental patients with total joint replacements. J. Am. Dent. Assoc. 134:895–899. 10.14219/jada.archive.2003.0289 [DOI] [PubMed] [Google Scholar]
- 470.Waldman BJ, Mont MA, Hungerford DS. 1997. Total knee arthroplasty infections associated with dental procedures. Clin. Orthop. Relat. Res. 343:164–172 [PubMed] [Google Scholar]
- 471.Skaar DD, O'Connor H, Hodges JS, Michalowicz BS. 2011. Dental procedures and subsequent prosthetic joint infections: findings from the Medicare Current Beneficiary Survey. J. Am. Dent. Assoc. 142:1343–1351. 10.14219/jada.archive.2011.0134 [DOI] [PubMed] [Google Scholar]
- 472.Watters W, III, Rethman MP, Hanson NB, Abt E, Anderson PA, Carroll KC, Futrell HC, Garvin K, Glenn SO, Hellstein J, Hewlett A, Kolessar D, Moucha C, O'Donnell RJ, O'Toole JE, Osmon DR, Evans RP, Rinella A, Steinberg MJ, Goldberg M, Ristic H, Boyer K, Sluka P, Martin WR, III, Cummins DS, Song S, Woznica A, Gross L. 2013. Prevention of orthopaedic implant infection in patients undergoing dental procedures. J. Am. Acad. Orthop. Surg. 21:180–189. 10.5435/JAAOS-21-03-180 [DOI] [PubMed] [Google Scholar]