Abstract
Medical device infections frequently require combination therapy. Beta-lactams combined with glycopeptides/lipopeptides are bactericidal against methicillin-resistant Staphylococcus aureus (MRSA). Novel macrowell kill-curve methods tested synergy between ceftaroline or cefazolin plus daptomycin, vancomycin, or rifampin against biofilm-producing MRSA. Ceftaroline combinations demonstrated the most pronounced bacterial reductions. Ceftaroline demonstrated greatest kill with daptomycin (4.02 ± 0.59 log10 CFU/cm2), compared to combination with vancomycin (3.36 ± 0.35 log10 CFU/cm2) or rifampin (2.68 ± 0.61 log10 CFU/cm2). These data suggest that beta-lactam combinations are useful against MRSA biofilms.
TEXT
Staphylococcus aureus is the most common cause of hospital-acquired infections and the second leading cause of catheter-related bloodstream infections (1, 2). Biofilm-associated medical device infections (MDIs) represent a serious health care issue due to increased morbidity, mortality up to 25%, and additional costs ranging from $1,000 to $50,000 per event depending on severity (3, 4).
Increased rates of treatment failure in MDIs are attributed, in part, to biofilm formation on the prosthetic material (5). Biofilm-embedded cells exhibit phenotypes of decreased susceptibility to most antimicrobials than those of less-dense planktonic cells (6). Lack of antimicrobial penetration into the biofilm matrix, differences in metabolic activity of bacterial cells between the different biofilm layers, and drug resistance in biofilm-embedded cells are thought to play a significant role in reduced antimicrobial response and subsequent treatment failure (7, 8). The most common approach to overcoming biofilm-mediated nonsusceptibility is combination therapy (9, 10). Rifampin is frequently combined with standard therapy for the management of staphylococcal MDIs, due to its ability to penetrate biofilm and its activity against both dividing and stationary cells (11–13). Despite the routine use of combination therapy, MDIs continue to be associated with poor clinical response.
Ceftaroline is a broad-spectrum cephalosporin that demonstrates potent activity against S. aureus, including methicillin-resistant S. aureus (MRSA). Ceftaroline has demonstrated synergy with vancomycin and daptomycin, with new data suggesting that ceftaroline may be more active against daptomycin-nonsusceptible S. aureus (DNS) and vancomycin-intermediate S. aureus (VISA) than against vancomycin-susceptible S. aureus (VSSA) due to the “seesaw effect” (14, 15). Additionally, ceftaroline may decrease the attraction of biofilm cells to prosthetic materials due to an alteration in cell membrane charge (16, 17). Prosthetic materials such as polystyrene and glass have slightly negative surface charges (16). Ceftaroline appears to lower cell surface charge (17), and this change in net surface charge may potentially decrease the attraction of biofilm-producing organisms to prosthetic material. Additionally, the lower cell surface charge favors increased daptomycin binding but also appears to demonstrate a cell wall thinning effect, potentially allowing for improved vancomycin binding. Therefore, we evaluated the activity of ceftaroline, alone and in combination, for synergy against biofilm-producing MRSA. Cefazolin combinations were analyzed as a comparator to determine if the potential synergy was related to the seesaw effect or the inherent MRSA activity of ceftaroline.
MIC determinations by broth microdilution (BMD) per CLSI guidelines and biofilm MIC (BMIC) determinations per the Calgary method were performed on 20 clinical MRSA bloodstream isolates against ceftaroline, daptomycin, cefazolin, vancomycin, and rifampin (18, 19). For susceptibility profiles, see Table 1. Daptomycin (Cubist Pharmaceuticals, Lexington, MA) and cefazolin, vancomycin, and rifampin (Sigma Chemical Company, St. Louis, MO) were purchased commercially. Ceftaroline powder was provided by Forest Laboratories (New York, NY). Strains were proven to produce biofilm by biofilm quantification techniques utilizing well-described biofilm-forming (NRSA101 and ATCC 35556) and non-biofilm-forming (ATCC 12228) strains as previously described (20, 21).
TABLE 1.
Broth microdilution and biofilm MICsa
| Strainb | MIC (mg/liter) of drug: |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CPT |
DAP |
CFZ |
RIF |
VAN |
||||||
| BMD | Biofilm | BMD | Biofilm | BMD | Biofilm | BMD | Biofilm | BMD | Biofilm | |
| 6242 | 1 | 2 | 0.25 | 8 | 16 | >64 | <0.0625 | >64 | 0.5 | 8 |
| 6246 | 1 | 2 | 0.125 | 2 | >64 | >64 | <0.0625 | >64 | 1 | 2 |
| 6911* | 1 | 2 | 2 | 4 | >64 | >64 | >32 | >64 | 2 | 8 |
| 5657 | 1 | 2 | 0.125 | 4 | >64 | >64 | <0.0625 | >64 | 1 | 8 |
| 5253 | 1 | 1 | 1 | 8 | 32 | >64 | <0.0625 | >64 | 2 | 16 |
| 5255 | 1 | 2 | 0.125 | 8 | 16 | >64 | <0.0625 | >64 | 0.5 | 16 |
| 5849* | 1 | 2 | 0.25 | 8 | 16 | >64 | <0.0625 | >64 | 0.5 | 8 |
| 5993 | 2 | 2 | 2 | 8 | 64 | >64 | >32 | >64 | 4 | 4 |
| 5995 | 0.5 | 0.5 | 4 | 16 | 64 | >64 | 0.5 | 64 | 4 | 32 |
| 5998 | 1 | 2 | 1 | 4 | >64 | >64 | 2 | >64 | 4 | 8 |
| 6000 | 0.25 | 0.5 | 4 | 8 | 32 | >64 | 8 | >64 | 4 | 16 |
| 6012* | 1 | 1 | 0.25 | 2 | 64 | >64 | <0.0625 | 2 | 0.5 | 2 |
| 6067* | 0.5 | 0.5 | 4 | 16 | >64 | >64 | 4 | >64 | 2 | 4 |
| 6072* | 1 | 1 | 4 | 16 | 64 | >64 | 4 | 8 | 1 | 2 |
| 6184* | 0.5 | 1 | 0.5 | 4 | 16 | >64 | <0.0625 | 16 | 0.5 | 8 |
| 6212* | 2 | 2 | 2 | 2 | >64 | >64 | <0.0625 | 32 | 1 | 2 |
| 6232 | 1 | 2 | 0.5 | 8 | >64 | >64 | <0.0625 | >64 | 1 | 8 |
| 6235 | 2 | 2 | 0.125 | 8 | >64 | >64 | <0.0625 | >64 | 1 | 4 |
| 6240 | 0.5 | 2 | 0.25 | 8 | 16 | >64 | <0.0625 | >64 | 1 | 8 |
| 6299 | 0.25 | 0.25 | 0.5 | 2 | 16 | >64 | <0.0625 | >64 | 4 | 8 |
Abbreviations: CPT, ceftaroline; DAP, daptomycin; CFZ, cefazolin; RIF, rifampin; VAN, vancomycin.
All strain designations begin with “R.” Asterisks indicate isolates proven to be heterogeneous VISA by modified population analysis.
After susceptibility determination, a previously undescribed, novel biofilm time-kill method was used to evaluate synergy against biofilm-embedded organisms. Three randomly selected representative strains (R6242, R6246, and R6911) were evaluated in duplicate. Briefly, 3-mm borosilicate beads were placed in 10% glucose-supplemented tryptic soy broth (GSTSB) inoculated with the test organism and incubated at 35°C, allowing for biofilm formation (22). After 24 h of incubation, GSTSB was aspirated and the beads were placed into macrowells containing Mueller-Hinton broth supplemented with 50 mg/liter of calcium due to the calcium-dependent mechanism of daptomycin (23). Antimicrobials were added at 1× the biofilm MIC for all agents unless the biofilm MIC was greater than free physiologic peak concentrations, in which case physiologic peaks were used. Beads were removed with sterile forceps at 0, 4, 8, and 24 h and placed into 1 ml of normal saline. Biofilm was recovered by three alternating 60-s cycles of vortexing and sonication at 20 Hz. Recovered biofilm cells were plated on tryptic soy agar and incubated for 24 h at 35°C. Synergy was defined as a ≥2-log10-CFU/cm2 reduction over the most active agent alone, and bactericidal activity was defined as a ≥3-log10-CFU/cm2 reduction from the starting inoculum (24). Antimicrobial exposures in biofilm time-kill assessments included ceftaroline, daptomycin, cefazolin, vancomycin, rifampin, ceftaroline plus daptomycin, ceftaroline plus vancomycin, ceftaroline plus rifampin, cefazolin plus daptomycin, cefazolin plus vancomycin, and cefazolin plus rifampin. Free peak synergistic concentrations were used for rifampin (2.1 mg/liter) and cefazolin (37 mg/liter) simulating dosages of 300 mg and 1,000 mg, as BMICs were higher than attainable drug concentrations. The targeted starting inoculum for all strains was ∼6.5 log10 CFU/cm2.
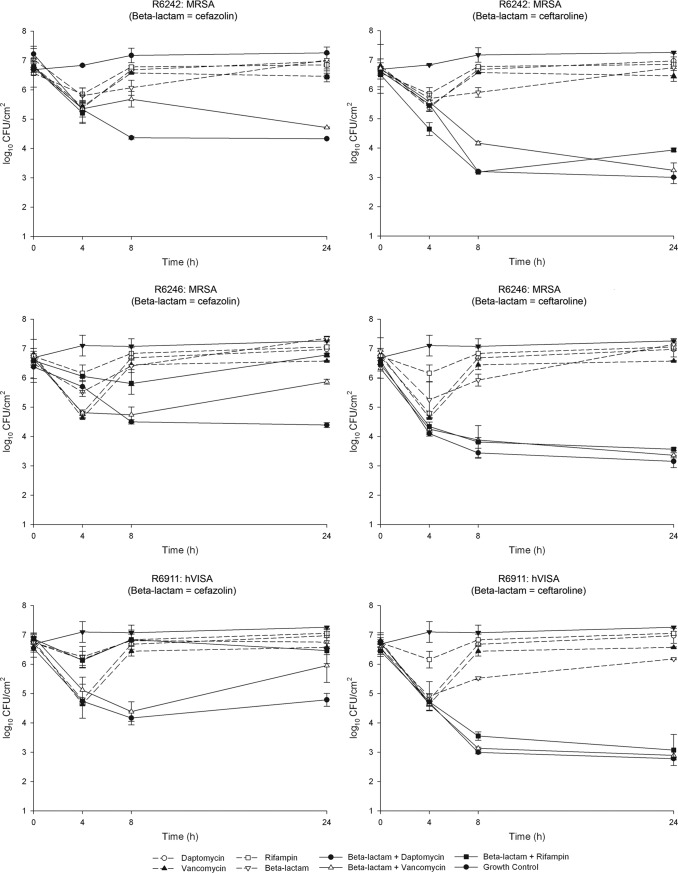
Biofilm MICs were up to 4-fold higher than BMD MICs for daptomycin and vancomycin, up to 1-fold higher for ceftaroline, at least 2-fold higher for cefazolin, and over 7-fold higher for rifampin (Table 1). In biofilm time-kill experiments, initial killing was seen for ceftaroline, daptomycin, vancomycin, and rifampin against all 3 strains within the first 4 h (Fig. 1). For all strains, single drug exposures did not result in sustained killing, with regrowth demonstrated within 8 h. All ceftaroline combinations produced greater reductions in colony counts against all strains evaluated than did cefazolin combinations (P < 0.05). Combinations of ceftaroline-daptomycin, ceftaroline-vancomycin, and ceftaroline-rifampin demonstrated synergy with average ± standard deviation values of 3.77 ± 0.45, 3.37 ± 0.35, and 2.68 ± 0.61 log10 CFU/cm2 reductions, respectively. Ceftaroline-rifampin was bactericidal against 2 of the 3 strains over the entire experiment (R6246 and R6911), while R6242 demonstrated regrowth at 24 h despite having the same MICs as the other 2 strains. Bactericidal activity was not observed with any cefazolin combination against any strain. Synergy was observed with cefazolin-daptomycin and cefazolin-vancomycin combinations for all strains.
FIG 1.
In vitro time-kill results with combinations including cefazolin (left) and ceftaroline (right) against isolates R6242 (top), R6246 (middle), and R6911 (bottom).
Upon review of the time-kills, combination biofilm MIC determinations were performed for the ceftaroline combinations to assess consistency of synergy across numerous strains with various susceptibilities. Cefazolin was not evaluated in BMICs due to less-pronounced activity in biofilm time kills. Combination BMIC determinations for daptomycin, vancomycin, and rifampin were performed for all 20 strains in the presence of ceftaroline at one-half the BMIC. In the presence of subinhibitory concentrations of ceftaroline, BMICs for daptomycin, vancomycin, and rifampin were 2 log2, 1 log2, and 2 log2 dilutions lower than those for the single agents, respectively. Though rifampin combinations appeared to lower the MIC 2 dilutions on average, the results were not consistent among all strains, with 9 isolates not exhibiting any reduction in MIC. The findings from the combination MIC determinations support the results observed from the time-kill curves.
Almost 55,000 MDIs are reported annually by the Centers for Disease Control and Prevention (1). Biofilm production is a therapeutically challenging factor contributing to the complexity of MDIs, allowing organisms to persist despite what should be adequate drug exposures (14, 25). Combination therapy is often employed to combat these difficult-to-treat infections (26). Our results demonstrate that ceftaroline combinations appear efficacious at decreasing biofilm-embedded MRSA. Bactericidal activity was observed for all strains when ceftaroline was combined with either daptomycin or vancomycin. However, though they are the standard of care, rifampin combinations demonstrated slightly less activity for all strains, with regrowth noted in one strain, warranting further clinical consideration of other combinations. Cefazolin combinations appeared, overall, less efficacious than did ceftaroline combinations, with only minimal synergistic activity noted with daptomycin or vancomycin. Overall, combinations with beta-lactams may provide additional treatment options for MDIs with embedded biofilms. However, beta-lactams with inherent MRSA activity appear to produce a more pronounced effect. Additionally, we were able to validate a novel, inexpensive approach for testing antimicrobial activity and combination synergy against biofilm-embedded organisms. Further testing is warranted to determine the most effective regimen, differences between other prosthetic materials, and clinical applicability.
ACKNOWLEDGMENTS
We thank Forest Laboratories for providing ceftaroline powder.
M.J.R. has received grant support from, consulted for, or provided lectures for Cepheid, Cerexa, Cubist, Durata, Forest, Novartis, Theravance, and Trius and is supported in part by grant R21AI092055 from the NIAID. K.E.B., B.J.W., and J.P.M. have no conflicts of interest to disclose.
Footnotes
Published ahead of print 10 March 2014
REFERENCES
- 1.Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, Kallen A, Limbago B, Fridkin S, National Healthcare Safety Network (NHSN) Team and Participating NHSN Facilities 2013. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect. Control Hosp. Epidemiol. 34:1–14. 10.1086/668770 [DOI] [PubMed] [Google Scholar]
- 2.Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, Raad II, Rijnders BJA, Sherertz RJ, Warren DK. 2009. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 49:1–45. 10.1086/599376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch AS, Robertson GT. 2008. Bacterial and fungal biofilm infections. Annu. Rev. Med. 59:415–428. 10.1146/annurev.med.59.110106.132000 [DOI] [PubMed] [Google Scholar]
- 4.Rosenthal VD, Maki DG, Salomao R, Moreno CA, Mehta Y, Higuera F, Cuellar LE, Arikan OA, Abouqal R, Leblebicioglu H, International Nosocomial Infection Control Consortium 2006. Device-associated nosocomial infections in 55 intensive care units of 8 developing countries. Ann. Intern. Med. 145:582–591. 10.7326/0003-4819-145-8-200610170-00007 [DOI] [PubMed] [Google Scholar]
- 5.Khardori N, Yassien M. 1995. Biofilms in device-related infections. J. Ind. Microbiol. 15:141–147. 10.1007/BF01569817 [DOI] [PubMed] [Google Scholar]
- 6.Frank KL, Reichert EJ, Piper KE, Patel R. 2007. In vitro effects of antimicrobial agents on planktonic and biofilm forms of Staphylococcus lugdunensis clinical isolates. Antimicrob. Agents Chemother. 51:888–895. 10.1128/AAC.01052-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donlan RM, Costerton JW. 2002. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 15:167–193. 10.1128/CMR.15.2.167-193.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall-Stoodley L, Costerton JW, Stoodley P. 2004. Bacterial biofilms: from the natural environment to infectious diseases. Nat. Rev. Microbiol. 2:95–108. 10.1038/nrmicro821 [DOI] [PubMed] [Google Scholar]
- 9.Patel R. 2005. Biofilms and antimicrobial resistance. Clin. Orthop. Relat. Res. 437:41–47. 10.1097/01.blo.0000175714.68624.74 [DOI] [PubMed] [Google Scholar]
- 10.Mah TF, O'Toole GA. 2001. Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol. 9:34–39. 10.1016/S0966-842X(00)01913-2 [DOI] [PubMed] [Google Scholar]
- 11.Perlroth J, Kuo M, Tan J, Bayer AS, Miller LG. 2008. Adjunctive use of rifampin for the treatment of Staphylococcus aureus infections: a systematic review of the literature. Arch. Intern. Med. 168:805–819. 10.1001/archinte.168.8.805 [DOI] [PubMed] [Google Scholar]
- 12.Blaser J, Vergeres P, Widmer AF, Zimmerli W. 1995. In vivo verification of in vitro model of antibiotic treatment of device-related infection. Antimicrob. Agents Chemother. 39:1134–1139. 10.1128/AAC.39.5.1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Widmer AF, Frei R, Rajacic Z, Zimmerli W. 1990. Correlation between in vivo and in vitro efficacy of antimicrobial agents against foreign body infections. J. Infect. Dis. 162:96–102. 10.1093/infdis/162.1.96 [DOI] [PubMed] [Google Scholar]
- 14.Werth BJ, Steed ME, Kaatz GW, Rybak MJ. 2013. Evaluation of ceftaroline activity against heteroresistant vancomycin-intermediate Staphylococcus aureus and vancomycin-intermediate methicillin-resistant S. aureus strains in an in vitro pharmacokinetic/pharmacodynamic model: exploring the “seesaw effect.” Antimicrob. Agents Chemother. 57:2664–2668. 10.1128/AAC.02308-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vidaillac C, Leonard SN, Rybak MJ. 2009. In vitro activity of ceftaroline against methicillin-resistant Staphylococcus aureus and heterogeneous vancomycin-intermediate S. aureus in a hollow fiber model. Antimicrob. Agents Chemother. 53:4712–4717. 10.1128/AAC.00636-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gross M, Cramton SE, Gotz F, Peschel A. 2001. Key role of teichoic acid net charge in Staphylococcus aureus colonization of artificial surfaces. Infect. Immun. 69:3423–3426. 10.1128/IAI.69.5.3423-3426.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Werth BJ, Sakoulas G, Rose WE, Pogliano J, Tewhey R, Rybak MJ. 2013. Ceftaroline increases membrane binding and enhances the activity of daptomycin against daptomycin-nonsusceptible vancomycin-intermediate Staphylococcus aureus in a pharmacokinetic/pharmacodynamic model. Antimicrob. Agents Chemother. 57:66–73. 10.1128/AAC.01586-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ceri H, Olson M, Morck D, Storey D, Read R, Buret A, Olson B. 2001. The MBEC assay system: multiple equivalent biofilms for antibiotic and biocide susceptibility testing. Methods Enzymol. 337:377–385. 10.1016/S0076-6879(01)37026-X [DOI] [PubMed] [Google Scholar]
- 19.Ceri H, Olson ME, Stremick C, Read RR, Morck D, Buret A. 1999. The Calgary biofilm device: new technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J. Clin. Microbiol. 37:1771–1776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stepanovic S, Vukovic D, Dakic I, Savic B, Svabic-Vlahovic M. 2000. A modified microtiter-plate test for quantification of staphylococcal biofilm formation. J. Microbiol. Methods 40:175–179. 10.1016/S0167-7012(00)00122-6 [DOI] [PubMed] [Google Scholar]
- 21.Christensen GD, Simpson WA, Younger JJ, Baddour LM, Barrett FF, Melton DM, Beachey EH. 1985. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J. Clin. Microbiol. 22:996–1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parra-Ruiz J, Vidaillac C, Rose WE, Rybak MJ. 2010. Activities of high-dose daptomycin, vancomycin, and moxifloxacin alone or in combination with clarithromycin or rifampin in a novel in vitro model of Staphylococcus aureus biofilm. Antimicrob. Agents Chemother. 54:4329–4334. 10.1128/AAC.00455-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Straus SK, Hancock REW. 2006. Mode of action of the new antibiotic for Gram-positive pathogens daptomycin: comparison with cationic antimicrobial peptides and lipopeptides. Biochim. Biophys. Acta 1758:1215–1223. 10.1016/j.bbamem.2006.02.009 [DOI] [PubMed] [Google Scholar]
- 24.American Society for Microbiology. 8. Instructions to authors. Antimicrob. Agents Chemother. 52:1–23. 10.1128/AAC.01407-07 [DOI] [Google Scholar]
- 25.Beenken KE, Blevins JS, Smeltzer MS. 2003. Mutation of sarA in Staphylococcus aureus limits biofilm formation. Infect. Immun. 71:4206–4211. 10.1128/IAI.71.7.4206-4211.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR, Infectious Diseases Society of America 2013. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 56:e1–e25. 10.1093/cid/cis803 [DOI] [PubMed] [Google Scholar]