Abstract
Over the past two decades, thousands of studies have demonstrated that Blacks receive lower quality medical care than Whites, independent of disease status, setting, insurance, and other clinically relevant factors. Despite this, there has been little progress towards eradicating these inequities. Almost a decade ago we proposed a conceptual model identifying mechanisms through which clinicians’ behavior, cognition, and decision making might be influenced by implicit racial biases and explicit racial stereotypes, and thereby contribute to racial inequities in care. Empirical evidence has supported many of these hypothesized mechanisms, demonstrating that White medical care clinicians: (1) hold negative implicit racial biases and explicit racial stereotypes, (2) have implicit racial biases that persist independently of and in contrast to their explicit (conscious) racial attitudes, and (3) can be influenced by racial bias in their clinical decision making and behavior during encounters with Black patients. This paper applies evidence from several disciplines to further specify our original model and elaborate on the ways racism can interact with cognitive biases to affect clinicians’ behavior and decisions and in turn, patient behavior and decisions. We then highlight avenues for intervention and make specific recommendations to medical care and grant-making organizations.
Keywords: Racial Inequity, Health Care Disparities, Racial Bias, Providers, Racism, Stereotypes, Discrimination, Interracial Interaction
Of all forms of inequity, injustice in healthcare is the most shocking and inhumane.
—Martin Luther King, Jr., National Convention of the Medical Committee for Human Rights, Chicago (1966)
INTRODUCTION
Over the past two decades, thousands of studies have demonstrated that Black2 adults and children are less likely to receive appropriate, guideline-concordant, and cutting-edge medical care than their White counterparts, independent of disease status and other clinically relevant factors. These inequities are mediated through and persist independently of Blacks’ lower access to health insurance, lower average socioeconomic status (SES), and lower access to care at high-performing medical-care facilities (Moy et al., 2005; Smedley et al., 2003). Furthermore, high SES, private health insurance, high-performing health plans, and receipt of care at high-performing hospitals and clinics, while beneficial, do not consistently afford the same quality of medical care to Black patients as they do White patients (Eberly et al., 2010; Epstein et al., 2010). The massive evidence of racial inequities in care and outcomes reveals deeply entrenched institutional racism in the U.S. health-care system. Institutional racism refers to a set of organizational practices that create unequal outcomes between groups on the basis of their race or ethnicity. It does not necessarily imply conscious intent and can occur outside the awareness of organizational members. Institutional racism is shaped by, and reinforces, societal racism, defined here as a pattern of deeply entrenched and culturally sanctioned beliefs, practices, and policies which, regardless of intent, serve to provide or defend the advantages of Whites and disadvantages to groups assigned to other racial or ethnic categories.
The medical professions have a historical commitment to principles of fairness, equity, and distributive justice. Over the past decade every influential organization with a stake in medical-care delivery has responded to evidence about racial inequity in medical care by acknowledging and condemning it. There has been an avalanche of policy statements, reports, and publications, and a great deal of private foundation and public funding targeted towards addressing institutional racism in medical care. While this response represents significant improvement over the doubt, denial, and silence that characterized the policy and medical leadership fifteen years ago, there has been very little actual progress towards eliminating racial inequities in medical care (Kelley et al., 2005; Le Cook et al., 2009).
Clinician bias is one of several contributors to racial inequalities in care and outcomes (Fincher et al., 2004). Bias includes generally negative feelings and evaluations of individuals because of their group membership (prejudice), overgeneralized beliefs about the characteristics of group members (stereotypes), and inequitable treatment (discrimination). These biases may be conscious and intentional (explicit) or unconscious and automatically activated (implicit). Explicit biases have traditionally been assessed with self-report measures whereas implicit biases are usually assessed with validated tests of unconscious associations (e.g., the Implicit Association Test (Greenwald et al., 2009)).
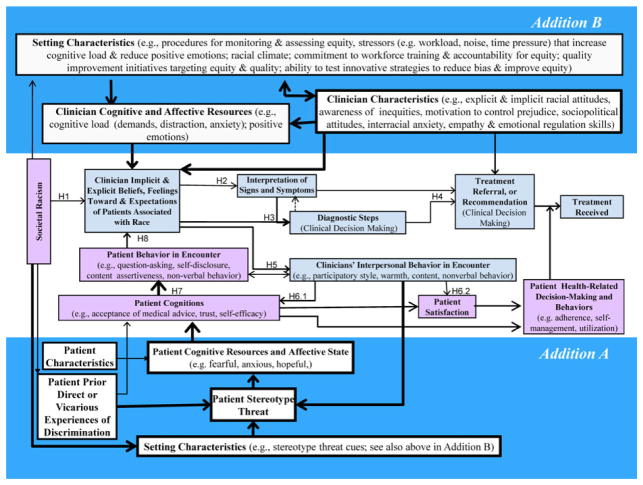
Almost a decade ago we proposed a conceptual model, shown in the center of Figure 1, that suggested a set of hypothesized mechanisms through which clinicians’ behavior, cognition, and decision making might be influenced by patient race to contribute to racial inequities in care (van Ryn and Fu, 2003). While still understudied, empirical evidence has supported the hypothesized mechanisms, demonstrating that White clinicians: (1) hold negative implicit racial biases and explicit racial stereotypes, (2) have implicit racial biases that persist independently of and in contrast to their explicit (conscious)racial attitudes, and (3)can be influenced by racial bias in their clinical decision making and behavior during encounters with Black patients (Cooper 2008; Green et al., 2007a; Hirsh et al., 2010; Penner et al., 2010; Sabin et al., 2008; van Ryn and Burke, 2000; van Ryn et al., 2006; White-Means et al., 2009). Despite the evidence that health professionals are (however unintentionally) perpetuating discriminatory practices, there has been little action and minimal progress toward eliminating the clinician contribution to racial inequities in care. Why has there been so little progress in response to evidence of pervasive and grave injustice?
Fig. 1.
Writing this paper led us to examine our own contribution to the lack of progress in rectifying this situation. While there are a variety of factors that impede action, our own framing and discourse on this topic may have impeded public support for policy solutions to eradicate racial inequities in care. In examining the impact of “patient race” on clinicians’ implicit cognitive processes, we may have inadvertently reinforced a sense of the problem as a property of the patients (“their” race) and the solution outside health professionals’ control (uncontrolled cognitive processes). The emphasis on unconscious processes may have lowered feelings of moral responsibility and accountability for rectifying unjust practices.
To a large extent, our prior emphasis on the role of implicit bias, an unconscious and automatic process, was, while grounded in theory and existing research, intentional and strategic. We wished to work effectively within the existing sociopolitical structure of medical care. When we first started presenting the concept that clinicians’ actions were perpetuating institutionalized racism to physician audiences in the 1990s, many in the audience reacted negatively, expressing hostility, mistrust, and dismissal of the topic. While intellectual doubt and criticism is productive when it creates interest in and advances discourse on a problem, strong negative arousal and aversion is rarely productive. Thus, we chose to use terms like “the impact of race” (van Ryn and Fu, 2003; van Ryn et al., 2006) rather than emphasizing the role of racism, in the hopes of reaching our target audience and creating openness to the need for change.
We have, however, continued to struggle with the possibility that our efforts to work within the power structure of the medical professions may have helped perpetuate the very problem we have been addressing. Using language such as “the impact of patient race” rather than “the impact of societal racism” on clinician cognition, behavior, and clinical decision making may have deflected discourse from the ways in which group stereotypes and institutional arrangements are products of racism and serve to reinforce racial inequality (Jost and Banaji, 1994; Sidanius et al., 2001). This strategy ignored the sociopolitical function of racism and may have failed to fully and unquestionably communicate the clinical professions’ moral responsibility for eliminating injustices embedded within their own institutions and clinical practice patterns. Hence here we have shifted our framing of the problem, from “the impact of patient race …” to the more accurate “impact of racism … on clinician cognitions, behavior, and clinical decision making.” The fact that automatic and frequently unconscious processes are in play reduces blame but not responsibility. Bioethical principles of justice and benevolence require medical-care systems and clinicians to do everything in their power to prevent these processes from causing unjust and harmful inequities in care.
This paper applies evidence from several disciplines to further specify our original model of the way racism interacts with common human social cognitive processes to affect clinicians’ behavior and decisions and, in turn, patient behavior and decisions, with special attention to modifiable factors, leverage points, and avenues for intervention. We apply the existing evidence to concrete action steps in a set of recommendations for medical care organizations and leaders.
REVISED MODEL OF THE HYPOTHESIZED MECHANISMS THROUGH WHICH RACISM INFLUENCES CLINICIANS TO CREATE INEQUITIES IN CARE
The model we explicated in earlier work can be found in the center of Figure 1 and in the corresponding hypotheses in Table 1. Because this portion of the model has been discussed thoroughly elsewhere, we refer the reader to an earlier article (van Ryn and Fu, 2003) and focus here on new material. In this model, the impact of societal racism is seen to be pervasive and its influence on the health-care encounter and outcomes is seen to be moderated by the setting of the encounter (health-care organization and clinic environment) as well as interpersonal and individual (clinician and patient) factors.
Table 1.
Summary of Core Hypotheses in the Previously Published Model, Presented in the Center of Figure 1 (adapted from van Ryn and Fu, 2003)
| Arrow Label | Hypothesis |
|---|---|
| H1 | Societal racism interacts with clinicians’ perception of patient race and common social-cognitive processes to influence clinicians’ implicit and explicit beliefs about, feelings towards, and expectations of patients independent of other patient and clinician characteristics. |
| H2 | Clinicians’ implicit and explicit beliefs about, feelings towards, and expectations of patients create a framework through which clinicians interpret signs and symptoms. |
| H3 | Clinicians’ implicit and explicit beliefs about, feelings towards, and expectations of patients and their interpretation of signs and symptoms then influences the diagnostic steps they take including questions asked and tests ordered. |
| H4 | Clinicians’ beliefs about and expectations of patients, interpretation of signs and symptoms, diagnostic steps and interpretation of findings influences their referral and treatment recommendations. |
| H5 | Clinicians’ interpersonal behaviors in clinical encounters are influenced by their beliefs about, feelings towards, and expectations of the patient. |
| H6 | Clinicians’ interpersonal behavior in clinical encounters will influence patient cognitions associated with acceptance of medical advice, trust, and self-efficacy as well as patient satisfaction. |
| H7 | Patient cognitions will influence patient behavior in the encounter. |
| H8 | Patient behavior in the encounter will influence clinicians’ implicit and explicit beliefs about, feelings towards, and expectations of patients independently of other patient and clinician characteristics. |
We added two constellations of hypothesized mediators and moderators of the effect of societal racism on clinician behavior and decision making. Addition A, in the bottom part of the model, focuses on patient factors. Addition B focuses on clinician characteristics. Both influence each other and are affected by setting characteristics (medical-care organization and policies, and clinical environment) and we apply this evidence to specific recommendations for action in medical care organizations.
Addition A, shown in the lower third of Figure 1, adds the concept of stereotype threat to our previous model. Stereotype threat occurs as a result of environmental or interpersonal cues that signal that an individual may be at risk of a situational threat of judgment or mistreated based on personal characteristics. It may be experienced explicitly or implicitly (triggered outside of awareness). In a conversation with Henry Louis Gates, Jr., Claude Steele explains:
Stereotype threat … refers to being in a situation or doing something for which a negative stereotype about one of your identities—your age, your race, your gender—is relevant to you. You know then that you could be seen and treated in terms of that stereotype. . . . as a member of this society, I know that your mind knows a number of negative stereotypes … and that if you wanted to—or even without thinking about it very much—you could judge me in terms of those bad stereotypes (Gates and Steele, 2009, pp. 251–252).
Over 300 experiments have been published in peer-reviewed journals demonstrating that experiencing stereotype threat can significantly reduce performance on cognitive and social tasks; increase anxiety, frustration, disappointment, and sadness; and generate coping strategies that may have undesirable effects (Burgess et al., 2010; Schmader et al., 2008; Steele and Aronson, 1995). Although there have been no published studies of stereotype threat in clinical settings, the robust findings in other arenas may have powerful implications for medical care.3 Table 2 provides the most important and well-replicated findings regarding the impact of stereotype threat, as well as their implication for minority patients in clinical settings.
Table 2.
Potential Consequences of Stereotype Threat for Patients (adapted from Burgess et al., 2010)
| Demonstrated Effects of Stereotype Threat in Research Conducted in Nonmedical Domains | Potential Implications for Patient and Encounter |
|---|---|
| Lowered working memory capacity and cognitive performance. | Diminished ability to process information and follow treatment instructions. |
| Lowered performance expectations and self-control. | Lowered self-efficacy regarding ability to adhere to treatment. |
| Lowered effort. | Lowered motivation to adhere to recommendations. |
| Increased anxiety and physiological arousal. | Impaired communication skills during encounters, reducing fluency, self-disclosure, and response to clinicians’ questions. |
| Caused discounting of the importance or validity of feedback. | Patients experiencing stereotype threat might be more likely to discount clinicians’ recommendations. |
| Caused avoidance of and disengagement from situations in which the threat occurs. | If going to the doctor engenders feelings of inferiority, the patient might be more likely to avoid those experiences. |
| Resulted in low identification with the domain within which they consistently experience the threat. | Reduced motivation to adhere to medication, diet, and lifestyle recommendations. |
| Caused individuals to (unintentionally and largely unconsciously) behave in ways that confirmed group stereotypes. | May reinforce clinicians’ racial stereotypes, increasing the possibility that clinician will be influenced by racial bias. |
Addition A also describes how clinicians’ interpersonal behavior and clinical setting characteristics may potentiate stereotype threat, impair patients’ cognitive resources, cognition, and behavior, and in turn reinforce negative clinician attitudes, potentially creating a negative spiral (Street et al., 2007). Many studies have shown that clinicians’ interpersonal behavior influences patient behaviors, including communication, adherence, and health care utilization (Roter, 2000; Stewart et al., 2000; Street et al., 2007). When clinician behavior is influenced by racial bias, it may induce stereotype threat among patients. This may in turn negatively impact patient communication, adherence, and utilization, such that the original racial bias becomes a self-fulfilling prophecy. Patients’ prior experiences of disrespect and discrimination, which are associated with higher treatment dropout, lower participation in screening, avoidance of health care, delays in seeking help and filling prescriptions, and lower ratings of health-care quality, may amplify this negative cycle (Blanchard and Lurie, 2004; Hausmann et al., 2008; Lee et al., 2009; Sorkin et al., 2010). Clinical settings, and the structures and cultures embodied within them, have the potential to exacerbate or mitigate stereotype threat and its negative consequences.
It is important to note that disparities in performance between stigmatized and nonstigmatized groups have been reduced or eliminated when stereotype threat is alleviated (Spencer et al., 1999). It is possible to create environments in which people feel safe from negative stereotypes (Steele 1992). Table 3 provides a set of recommendations for heath-care environments that were adapted and slightly expanded on from those made by Burgess et al. (2010).
Table 3.
Strategies for Creating “Identity-Safe” Clinical Environments and Reducing Stereotype Threat, Translated from Findings in Nonmedical Domains (adapted from Burgess et al., 2010)
| Recommendation | Examples |
|---|---|
| Actively and intentionally communicate an inclusive, respectful and welcoming environment. | Place cues in the physical environment, such as décor that includes:
|
| Elicit the patient’s values and strengths in any way that results in patient self-affirmation. | When recommending significant health behavior change, clinician asks the patient about a time in her life in which she has dealt with a significant challenge, and encourages her to discuss the qualities within herself that helped her overcome it. |
| Invoke high standards and communicate confidence in the patient’s ability to meet those standards. | Clinician emphasizes that she is setting “a high bar” for the patient because she is confident that he will be able to be successful (e.g., at behavior change, at achieving health-related goals). |
| Provide external attributions for the patient’s anxiety and difficulties (to prevent anxiety from affecting patient’s sense of competence). | Check in with a patient who seems anxious and distracted, reassuring him that such feelings are something many if not most patients feel at times. |
Addition B highlights the role of individual clinician factors in mediating and moderating the impact of societal racism on clinicians’ beliefs, attitudes, and expectations of patients, and points to setting factors that can be targeted to reduce inequities in care. It reflects a large body of evidence regarding situational and contextual factors as well as stable characteristics of individuals that influence the likelihood that racial (and other) biases will be activated and adversely affect judgment and behavior. We first review relevant clinician factors and then apply the evidence on contextual factors to recommendations to medical organizations regarding strategies that can create identify-safe environments and assist clinicians in their goal of providing high-quality and equitable care.
Clinician Characteristics
Racial Bias
Like the general population, clinicians vary widely in their levels of both implicit and explicit racial biases. Moreover, implicit and explicit biases are only weakly correlated (Dovidio et al., 2001). Most Whites are low in explicit and high in implicit prejudice, although there are Whites who are consistently low in both forms of bias (i.e., both explicit and implicit) and those who are high in both. The combination of high explicit with low implicit bias is rare.
High Explicit And Implicit Racial Bias
To our knowledge there have been no representative studies of clinicians to ascertain the proportion who are high on contemporary measures of explicit racial bias. Little is known about the impact of explicit racism on provision of care. Two sociopolitical orientations have been shown to predict explicit biases in numerous studies: Social Dominance Orientation (SDO) and Medical Authoritarianism (MA), an offshoot of Right Wing Authoritarianism (RWA). SDO represents the degree to which people value hierarchically structured relationships among social groups, such as the dominance of Whites over Blacks (Pratto et al., 1994). RWA reflects the level of belief in traditional authority structures. MA is specific to the health-care context; it has been found to predict medical students’ tendencies to stereotype and make negative attributions about patients from stigmatized groups and, unfortunately, appears to increase over the course of medical education (Merrill et al., 1995).
High levels of explicit bias (as predicted by SDO, RWA, and MA) among clinicians may be difficult to change, so interventions that effectively limit how these personal orientations translate into bias in clinical decision making and behavior are needed. In our prior work we advocated interventions that appealed to clinicians’ prosocial motivations to provide the highest quality of care for all patients. However, appeals to such prosocial motivations may be less effective for clinicians who do not have egalitarian standards (Monteith et al., 2010). Even for those who do, efforts to address explicit bias should be approached cautiously. Concerns about appearing biased can actually accentuate stereotypic thinking (stereotype rebound (Monteith et al., 1998)) and interfere with communication and rapport (Goff et al., 2008). Instead, bias might be more effectively reduced among clinicians high in SDO or RWA by emphasizing universal application of norms, rules, and guidelines. In fact, clinicians high on RWA and MA may be particularly likely to be compliant with guidelines (Burgess et al., Forthcoming; Phelan et al., 2009). For this group, then, guideline-driven quality improvement efforts may be the most effective pathway to more equitable care.
Low Implicit and Explicit Racial Bias
There is a subset of White clinicians who are low on both implicit and explicit racial bias measures. Sabin et al. (2008; 2009) examined a large sample of physicians and found that a small minority of White physicians did not have an implicit pro-White bias, that women physicians had lower levels of pro-White implicit bias than male physicians, and Hispanic and Asian physicians had levels of pro-White implicit bias that were similar to White physicians. Black physicians, on average, did not show a systematic implicit preference for either White Americans or Blacks. Furthermore, implicit bias may differ by specialty and or site; Penner et al. (2010) found that their sample of fifteen family medicine clinicians working in an inner city had less implicit pro-White bias than other clinician samples.
Low Explicit and High Implicit Racial Bias
Dovidio and Gaertner (2004) use the term aversive racism to describe people who have low levels of explicit bias and high levels of implicit bias—because consciously egalitarian people experience the idea that they are racially biased as aversive. White aversive racists are more likely to experience anxiety and discomfort than hostility when interacting with Blacks. Because explicit bias affects verbal behavior and implicit bias influences nonverbal behavior, the combination of high implicit and low explicit bias has negative implications for clinician-patient encounters. For example, Whites with high implicit racial biases and low explicit bias were found to have less direct eye contact with Blacks than with Whites (Dovidio et al., 1997b). Clinicians may be aware that what they say is consistent with their explicitly egalitarian attitudes but unaware of the way their implicit biases influence their nonverbal behaviors (McConnell and Leibold, 2001). The lack of correspondence between nonverbal behavior and verbal friendliness may lead to suspicions of duplicity among Black patients because inconsistency between positive overt expressions and negative subtle displays is generally perceived to reflect deceitfulness (Dovidio et al., 2008). Consistent with this finding, Black patients were least satisfied with their medical encounter when physicians were relatively high on implicit but low on explicit bias compared to every other combination, including clinicians who were high on both explicit and implicit bias (Penner et al., 2010). Reducing this adverse consequence of the combination of high implicit and low explicit bias may be achieved through efforts to increase clinicians’ awareness, motivation, and skills, as well as decrease interracial anxiety, as described below.
Awareness of Racial Inequities
In order to create a felt need and motivation for change, clinicians must be aware of both overall racial inequities in care as well as their own potential to be biased in their care of patients (Smith et al., 2007). The Kaiser Family Foundation (KFF)2002 National Survey of Physicians found that only 25% of White physicians versus 77% of Black physicians believed that patients are treated unfairly due to their race or ethnicity very or somewhat often (KFF 2002). A few years later, a 2005 survey of approximately 2000 physicians found that 55% of White physicians agreed that minority patients generally receive lower quality care than White patients, 21% were unsure, and 24% disagreed (AMA 2005). Furthermore, a recent qualitative study of twenty-six doctors and nurses found the majority questioned the validity of studies reporting disparities (Clark-Hitt et al., 2010). Clearly, more effective strategies are needed to ensure the majority of clinicians are aware of this problem.
Personal Bias Awareness
Clinicians who are aware of inconsistencies between their subtly biased behaviors and egalitarian attitudes may be more likely to “correct” for potential bias in the short term and be more motivated to engage in self-regulatory processes that can inhibit even subtle expressions of bias in the longer term (Devine and Monteith, 1993). Consistent with this notion, Perry and Murphy (2011) found that, in a stressful interracial context, Whites who felt that they may harbor subtle racial biases toward Blacks (what they have termed “bias awareness”) responded with more guilt and willingness to dedicate time to activities aimed at improving racial diversity than did Whites with low bias awareness. Thus, clinicians’ bias awareness may affect their willingness to participate in bias reduction interventions.
Motivation to Control Prejudice
Contrary to early fears about the uncontrollable automaticity of implicit bias, a number of studies have found that people who are high on internal motivation to control prejudice and have sufficient cognitive resources can be very successful at limiting the impact of implicit biases (Monteith et al., 2010; Plant and Devine, 2009). With sufficient cognitive resources and practice, people are able to focus on the unique qualities of individuals, rather than on the groups they belong to, in forming impressions of and behaving toward others.
Skills
Several general interpersonal abilities are associated with lower racial bias. Both the cognitive and affective components of empathy ultimately produce more positive orientations toward another person and a greater interest in the other’s welfare (Batson et al., 1997); focusing on the other’s feelings engenders greater empathy than “being objective” (Batson et al., 1997). Perspective-taking (the cognitive component of empathy) has been shown to reduce bias toward a range of stigmatized groups, including Blacks, at least in the short term, and to inhibit the activation of unconscious stereotypes and prejudices (Dovidio et al., 1998, 2008; Galinsky and Moskowitz, 2000). Many studies have documented the positive effects of clinician empathy on patient satisfaction, self-efficacy, perceptions of control, emotional distress, adherence, and health outcomes (Burgess et al., 2007).
Recent research outside the medical domain suggests that clinicians who have good emotional regulation skills and experience positive emotion during clinical encounters may be less likely to categorize patients in terms of their racial, ethnic, or cultural group and more likely to view patients in terms of their individual attributes (Johnson and Fredrickson, 2005). They also use more inclusive social categories, so that people are more likely to view themselves as being part of a larger group (Dovidio et al., 1995, 1998). This can facilitate empathy and increase the capacity to see others as members of a common “ingroup” as opposed to “outgroup” (Dovidio et al., 1995; Dovidio and Gaertner, 2004; Gaertner and Dovidio, 2000) Likewise, partnership-building skills can reduce the likelihood that implicit bias will affect clinician behavior and decision making; clinicians who have skills at creating partnership with patients are more likely to develop a sense that their partner is on the same “team,” working together towards a common goal, and developing a common ingroup. This is also likely to reduce patients’ experiences of stereotype threat. Perceptions of common ingroup membership, of being on the same team, also facilitate perspective-taking (Dovidio et al., 2004) and affective empathy (Dovidio et al., 1997a).
Interracial Anxiety
Researchers have found that White people who sincerely want to behave in a non-prejudiced manner often manifest anxiety and heightened levels of arousal when interacting with minority or other stigmatized group members (Dovidio and Gaertner, 2004). Intergroup anxiety leads people to avoid intergroup contact, negatively impacts the nature and experience of intergroup interaction, interferes with effective communication, and may exacerbate negative feelings about members of the other group, which reinforces the desire to avoid such contact in the future (Plant and Butz, 2006). Furthermore, anxiety absorbs cognitive resources, so that interracial anxiety may produce lower-quality judgments and behavior. In addition, many of the nonverbal expressions of anxiety (e.g., averted gaze, closed posture) are similar to those associated with dislike, so anxiety may be interpreted as indicating racial prejudice (Dovidio et al., 2008). Nevertheless, intergroup anxiety is very different from racial prejudice or stereotypes and requires a different intervention.
In this section we reviewed characteristics of clinicians that have been shown in social-psychological studies to affect the likelihood of racial biases in behavior and decision making. Clinician characteristics such as awareness of racial bias, empathy, emotional regulation, and partnership-building skills are promising targets for intervention as they are mutable skills and have potential impacts on both bias and interracial anxiety. However, institutional racism is so entrenched that new behaviors are more likely to persist if supported by the social environment; interventions targeting clinician factors may be most successful if aimed at all personnel and embedded in overall organizational change.
Setting Factors and Recommendations to Medical Care Organizations
Evidence from a variety of disciplines points to a number of promising approaches to eradicating inequities in care.
Establish Ongoing Procedures for Monitoring and Assessing Equity in Care
Because many different elements contribute to individual assessments and decisions, bias is much more difficult to recognize in a specific instance than when information is aggregated across cases (Crosby et al., 1986). Systematically collecting data on race and other indicators of social position is necessary if care systems are to meet their obligation to self-assess, monitor, and evaluate the effectiveness of their strategies for eradicating inequities in care. Frameworks for data collection have been or are being developed that may prove very helpful for monitoring inequities (Newhouse 2009; Siegel et al., 2009). When inequities are found, providing targeted feedback, supporting creative solutions for remediation, and creating accountability for improvement may inspire the development of a number of innovative and effective correction strategies.
Reduce Stressors that Increase Clinicians’ Cognitive Load
Racial bias and stereotypes are more likely to influence cognitions and behaviors when individuals’ cognitive capacity is low or overtaxed (called “high cognitive load”). Furthermore, when cognitive capacity is taxed, memory is biased toward information that is consistent with stereotypes, and individuals are less able to override automatic processes of racial categorizing and stereotyping (Burgess 2010). Practice setting characteristics that create high cognitive load include productivity pressures, time pressure, high noise levels, inadequate staffing, poor feedback, inadequate supervision, inadequate training, high communication load, and overcrowding (Croskerry and Wears, 2002). Conversely, established routines, adequate time per patient and between patients, and sufficient staffing resources are protective factors (Burgess 2010). This recommendation is also responsive to evidence that physician stress and time pressure are associated with a greater likelihood of making errors and providing suboptimal patient care (Williams et al., 2007) and inappropriate prescribing (Tamblyn et al., 1997). Notably, a study of guideline implementation found that the only strategies that improved hypertension management were those designed to reduce physician time pressure and task complexity (Green et al., 2007b).
Improve Organizational Racial Climate
Racial (or diversity)climate has been defined as employees’ shared perceptions of the policies and practices that communicate the extent to which fostering diversity and eliminating discrimination is a priority in the organization (Pugh et al., 2008). The benefits of medical-school diversity have been shown to vary by the degree to which there was a positive climate for interracial interaction (Saha et al., 2008). In a recent national survey, over 70% of Black physicians reported experiencing racial discrimination in their workplace (Nunez-Smith et al., 2009). In another study, 62% of physicians reported that they had witnessed a patient receive poor quality health care because of the patient’s race or ethnicity (AMA 2005). These findings indicate medical-care organizational climates that are, perhaps subtly, tolerant of racism. Informal organizational norms that are supportive of racism potentiate the expression of implicit and explicit racial bias and can trigger patient stereotype threat.
Ensure Racial Diversity at All Levels of the Organizational Hierarchy and Promote Positive Intergroup Contact
A meta-analysis of 713 independent samples from 515 studies concluded that intergroup contact typically reduces intergroup prejudice and that institutional support for interaction can increase the benefits of intergroup contact. Contact can reduce future feelings of interracial anxiety and has been shown to generalize from the participants in the immediate contact situation to attitudes toward the entire out-group (Pettigrew and Tropp, 2008). A clinic setting with Black staff at all levels is less likely to trigger stereotype threat among Black patients and interracial anxiety among clinicians than one with little diversity or in which only jobs at lower levels of the organizational hierarchy have a diverse workforce (Purdie-Vaughns et al., 2008).
Mandate Appropriate and Effective Training Programs and Hold Clinicians and Staff Accountable for Skills and Knowledge
Improving the racial climate includes ensuring that all employees are aware of the impact of racism on quality of care, understand the evidence regarding disparities in care, recognize the impact of stereotype threat, appreciate the importance of respectful interactions, and recognize the potential for bias in their own behavior. Providing training and support for acquiring the skills described above (practicing perspective-taking, partnership building, and emotional regulation) can help clinicians reduce the impact of racism on the care they provide. It is worth noting that some “cultural competence” programs focus on these skills and these may be helpful models, pending evaluation results (Beach et al., 2005; Betancourt and Green, 2010).
Existing evidence suggests that with sufficient organizational support, skills training, and available cognitive resources, clinicians high on internal motivation to control prejudice and bias awareness will have considerable success at preventing racism from affecting the quality of care they provide. However, the strategies that will be effective with those who are low on internal motivation to control prejudice are less clear. Awareness that they will be evaluated on their ability to provide equitable care and periodic feedback on equity-related metrics might be very motivating for clinicians and staff. If whole teams or units are evaluated, social norms and pressures may also help clinicians in their goal to provide equitable and just care. A whole-unit (clinic or office) approach is important as nonclinician staff can have a significant effect on patients’ medical-care experiences (Barr and Wanat, 2005).
Carefully Implement Quality Improvement Initiatives, Decision Aids, and Reminder Systems
A number of quality improvement (QI) initiatives have been very successful at reducing inequities in care for a specific condition. Studies involving clinician reminder systems for provision of standardized services (mostly preventive) have had good outcomes (Beach et al., 2006). QI is likely to be most effective at reducing inequities when there is a clear consensus on the specific steps needed to diagnose and treat a condition and little opportunity for bias in the diagnostic processes. However, in some cases QI strategies have not closed gaps or have been applied unevenly so that White patients were more likely to receive and benefit from the initiative than Black patients (Olomu et al., 2010).
Partner with Grant Agencies and Researchers to Test Creative, Innovative Strategies
There are some very promising innovative strategies that may seem nonnormative in health care organizations, but have demonstrated impact in other settings that may generalize to clinical environments. Structuring clinician and patient opportunities for self-affirmation may reduce bias and stereotype threat. Self-affirmation treatments have been shown to decrease outgroup derogation, rejection of threatening information, and improve Whites’ understanding of racism (Burgess 2010).
Creating an environment in which positive images of Blacks are prominent, for example by filling clinics with artwork and brochures that show admired Blacks and/or Blacks in a positive context, has considerable potential. Evidence from several studies indicates that these strategies may lower both stereotype threat in patients and implicit biases in clinicians (Burgess et al., 2010a). Using stories (narrative fiction)to influence perceptions of social norms may be more effective at influencing implicit attitudes than current educational approaches. For example, a radio intervention in Rwanda using stories that portrayed intergroup cooperation changed perceptions of social norms as well as behaviors related to trust, empathy, and cooperation (Paluck 2009).
Summary
It has been eight years since we first proposed an integrated model of the way racism can influence clinician cognition, behavior, and clinical decision making. In this paper we have revised and more fully specified our prior conceptual model in light of recent literature. We made several key points and recommendations, summarized in Table 4. There are significant gaps in knowledge that, if addressed, might substantially advance our ability to make progress in eliminating inequities in health care; these are also listed in Table 4.
Table 4.
Summary of Recommendations and High Priority Research Questions
|
Recommendations
|
| Evaluate the racial climate, investigate reports of subtle or overt discrimination and unfair treatment, and identify and work to transform formal and informal norms that ignore and/or support racism. |
| Establish monitoring systems in which processes and outcomes of care can be compared by patient race. |
| Give care units and, where appropriate, individual clinicians, equity-specific targeted feedback. |
| When inequities are found, support creative solutions for remediation and create accountability for improvement. |
| Implement work policies and clinic procedures that protect clinicians from cognitive load and promote positive emotions. |
| Promote racial diversity at all levels of the organizational hierarchy and support positive intergroup contact. |
| Implement and evaluate training that ensures that clinicians have the knowledge and skills needed to prevent racial biases from affecting the quality of care they provide: self-awareness regarding implicit biases, perspective-taking skills, emotional-regulation skills, and partnership-building skills.
|
|
High Priority Research Questions
|
| What organizational factors have led a few medical care systems to self-assess, monitor, and develop strategies for reducing inequities in care? How can these factors be transferred to other organizations? |
| What medical training factors improve clinicians’ ability to protect against being influenced by racial bias in their interactions with patients and clinical decision making? |
| Will the benefits conferred by reductions in cognitive load and higher levels of positive emotion shown in other settings translate to lower racial bias in clinicians’ behavior and decision making? |
| What changes in reimbursement methodologies and organization of care delivery might promote clinicians’ ability to practice perspective-taking, emotional regulation, and partnership-building to reduce racial bias in encounters? |
| What patient strategies improve quality of care and reduce the likelihood that clinicians will be affected by implicit racial biases in encounters? What approaches will be most effective in promoting patient use of such strategies? |
CONCLUSION
There have been over two decades of consistent findings of racial inequities in medical care, including among children, the elderly, cancer patients, and veterans. What explanations are there for the deplorable lack of progress in addressing these morally reprehensible, unjust inequities? In our early writings we avoided using the term “racism” because we were concerned that automatic negative arousal in response to the concept of racism would undermine our effectiveness in drawing attention to the role of clinician bias in perpetuating inequities in care. We face a similar dilemma here. Critical Race Theory points to the way Whites view their social, cultural, and economic experiences as a norm that everyone should experience, rather than as an advantaged position. Explanations for inequality then focus on the failure of outgroups—in this case Blacks—to achieve normal social status (Delgado and Stefancic, 2001; Ford and Airhihenbuwa, 2010). This theory would explain our tendency to focus on Black patients’ mistrust and culture rather than White clinicians’ racism. However, the notion of “White privilege” is extremely uncomfortable to nonegalitarians and egalitarians alike and has been shown to create hostility and increase racially biased responses (Branscombe et al., 2006; Powell et al., 2005). Furthermore, the threat of appearing racist has been shown to trigger stereotype threat for Whites, resulting in higher levels of stereotype-confirming behavior (Goff et al., 2008).
As individuals and members of institutions in the society in which we live and work, we are all responsible for contributing to solutions and actively striving to eliminate racism. Thus we end with three questions. Why have we devoted so much attention to research and interventions that focus on Black patient mistrust, belief systems, communication and nonadherence and have focused so little on racial bias among clinicians? Why have we done so little to address the health-care-policy and societal factors that cause Blacks to get care at facilities that provide suboptimal quality of care? Are our current dominant approaches the right and appropriate responses given our lack of progress in rectifying the egregious inequities in health care?
Footnotes
The term Black refers to the socially constructed group category assigned to African Americans who were born in the United States and are largely the descendents of enslaved African ancestors. Other people with dark skin and/or Afrocentric features may be classified as Black by perceivers. The term White here refers to light-skinned individuals largely of European ancestry.
Burgess et al. (2010) provided an in-depth review of the literature on stereotype threat in light of implications for the clinical encounter and we refer the interested reader to that article as well as to the comprehensive Web site www.reducingsterotypethreat.org.
Contributor Information
Michelle van Ryn, Department of Family Medicine and Community Health, University of Minnesota.
Diana J. Burgess, Center for Chronic Disease Outcomes Research, Minneapolis VA Medical Center and Department of Medicine, University of Minnesota.
John F. Dovidio, Department of Psychology, Yale University
Sean M. Phelan, Department of Family Medicine and Community Health, University of Minnesota
Somnath Saha, Section of General Internal Medicine, Portland VA Medical Center and Division of General Internal Medicine and Geriatrics, Oregon Health and Science University.
Jennifer Malat, Department of Sociology, University of Cincinnati.
Joan M. Griffin, Center for Chronic Disease Outcomes Research, Minneapolis VA Medical Center and Department of Medicine, University of Minnesota.
Steven S. Fu, Center for Chronic Disease Outcomes Research, Minneapolis VA Medical Center and Department of Medicine, University of Minnesota.
Sylvia Perry, Department of Psychology, Yale University.
References
- American Medical Association (AMA) [accessed August 3, 2010];Quality Health Care for Minorities: Understanding Physicians’ Experiences: Physicians Are Becoming Engaged in Addressing Disparities: Preliminary Survey Brief. 2005 〈 http://www.ama-assn.org/ama/pub/physician-resources/public-health/eliminating-health-disparities/commission-end-health-care-disparities/quality-health-care-minorities-understanding-physicians.shtml〉.
- Barr DA, Wanat SF. Listening to Patients: Cultural and Linguistic Barriers to Health Care Access. Family Medicine. 2005;37(3):199–204. [PubMed] [Google Scholar]
- Batson CD, Polycarpou MP, Harmon-Jones E, Imhoff HJ, Mitchener EC, Bednar LL, Klein TR, Highberger L. Empathy and Attitudes: Can Feeling for a Member of a Stigmatized Group Improve Feelings toward the Group? Journal of Personality and Social Psychology. 1997;72(1):105–118. doi: 10.1037//0022-3514.72.1.105. [DOI] [PubMed] [Google Scholar]
- Beach MC, Gary TL, Price EG, Robinson K, Gozu A, Palacio A, Smarth C, Jenckes M, Feuerstein C, Bass EB, Powe NR, Cooper LA. Improving Health Care Quality for Racial/Ethnic Minorities: A Systematic Review of the Best Evidence Regarding Provider and Organization Interventions. BMC Public Health. 2006;6:104. doi: 10.1186/1471-2458-6-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, Smarth C, Jenckes MW, Feuerstein C, Bass EB, Powe NR, Cooper LA. Cultural Competence: A Systematic Review of Health Care Provider Educational Interventions. Medical Care. 2005;43(4):356–373. doi: 10.1097/01.mlr.0000156861.58905.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt JR, Green AR. Commentary: Linking Cultural Competence Training to Improved Health Outcomes: Perspectives from the Field. Academic Medicine. 2010;85(4):583–585. doi: 10.1097/ACM.0b013e3181d2b2f3. [DOI] [PubMed] [Google Scholar]
- Blanchard J, Lurie N. R-E-S-P-E-C-T: Patient Reports of Disrespect in the Health Care Setting and Its Impact on Care. Journal of Family Practice. 2004;53(9):721–730. [PubMed] [Google Scholar]
- Branscombe NR, Schmitt MT, Schiffhauer K. Racial Attitudes in Response to Thoughts of White Privilege. European Journal of Social Psychology. 2006;37(2):203–215. [Google Scholar]
- Burgess D, Van Ryn M, Dovidio J, Saha S. Reducing Racial Bias among Health Care Providers: Lessons from Social-Cognitive Psychology. Journal of General Internal Medicine. 2007;22(6):882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ. Are Providers More Likely to Contribute to Healthcare Disparities under High Levels of Cognitive Load? How Features of the Healthcare Setting May Lead to Biases in Medical Decision Making. Medical Decision Making. 2010;30(2):246–257. doi: 10.1177/0272989X09341751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Phelan S, Dovidio J, van Ryn M. The Effect of Medical Authoritarianism on Physicians’ Attitudes and Treatment Decisions for Chronic Pain. Journal of Applied Social Psychology Forthcoming. [Google Scholar]
- Burgess DJ, Warren J, Phelan S, Dovidio J, van Ryn M. Stereotype Threat and Health Disparities: What Medical Educators and Future Physicians Need to Know. Journal of General Internal Medicine. 2010;25(Supplement 2):S169–S177. doi: 10.1007/s11606-009-1221-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark-Hitt R, Malat J, Burgess D, Friedemann-Sanchez G. Doctors’ and Nurses’ Explanations for Racial Disparities in Medical Treatment. Journal of Health Care for the Poor and Underserved. 2010;21(1):386–400. doi: 10.1353/hpu.0.0275. [DOI] [PubMed] [Google Scholar]
- Commission to End Health Care Disparities. Preliminary Survey Brief: Physicians Are Becoming Engaged in Addressing Disparities. [accessed August 3, 2010];Quality Health Care for Minorities: Understanding Physicians’ Experiences. 2005 〈 http://www.ama-assn.org/ama/pub/physician-resources/public-health/eliminating-health-disparities/commission-end-health-care-disparities/quality-health-care-minorities-understanding-physicians.shtml〉.
- Cooper LA. College of Public Health and Health Professions Celebrating 50 Years. University of Florida; 2008. Overcoming Healthcare Disparities: The Role of Patient-Centered Care. [Google Scholar]
- Crosby F, Clayton S, Alksnis O, Hemker K. Cognitive Biases in the Perception of Discrimination: The Importance of Format. Sex Roles. 1986;14(122):637–646. [Google Scholar]
- Croskerry P, Wears RL. Safety Errors in Emergency Medicine. In: Markovchick VJ, Pons PT, editors. Emergency Medicine Secrets. 3. Philadelphia, PA: Hanley and Belfus; 2002. pp. 29–37. [Google Scholar]
- Davis MH, Soderlund T, Cole J, Gadol E, Kute M, Myers M, Weihing J. Cognitions Associated with Attempts to Empathize: How Do We Imagine the Perspective of Another? Personality and Social Psychology Bulletin. 2004;30:1625–1635. doi: 10.1177/0146167204271183. [DOI] [PubMed] [Google Scholar]
- Delgado R, Stefancic J. Critical Race Theory: An Introduction. New York: New York University Press; 2001. [Google Scholar]
- Devine PG, Monteith MJ. The Role of Discrepancy-Associated Affect in Prejudice Reduction. In: Mackie DM, Hamilton DL, editors. Affect, Cognition, and Steroetyping: Interactive Processes in Group Perception. New York: Academic Press; 1993. pp. 317–344. [Google Scholar]
- Dovidio JF, Gaertner L. Aversive Racism. In: Zanna Mark P., editor. Advances in Experimental Social Psychology. San Diego, CA: Academic Press; 2004. pp. 1–51. [Google Scholar]
- Dovidio John F, Gaertner Samuel L, Isen Alice M, Lowrance Robert. Group Representations and Intergroup Bias: Positive Affect, Similarity, and Group Size. Personality and Social Psychology Bulletin. 1995;21(8):856–865. [Google Scholar]
- Dovidio JF, Gaertner SL, Stewart TL, Esses VM, Ten Vergert M. From Intervention to Outcomes: Processes in the Reduction of Bias. In: Stephan WG, Vogt P, editors. Intergroup Relations Programs: Practice, Research, and Theory. New York: Teachers College Press; 2004. pp. 243–265. [Google Scholar]
- Dovidio JF, Gaertner SL, Validzic A. Intergroup Bias: Status, Differentiation, and a Common in-Group Identity. Journal of Personality and Social Psychology. 1998;75(1):109–120. doi: 10.1037//0022-3514.75.1.109. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Gaertner SL, Validzic A, Matoka K, Johnson B, Frazier S. Extending the Benefits of Recategorization: Evaluations, Self-Disclosure, and Helping. Journal of Experimental Social Psychology. 1997a;33(4):401–420. doi: 10.1006/jesp.1997.1327. [DOI] [PubMed] [Google Scholar]
- Dovidio J, Kawakami K, Beach K. Implicit and Explicit Attitudes: Examination of the Relationship Between Measures of Intergroup Bias. In: Brown R, Gaertner SL, editors. Blackwell Handbook of Social Psychology: Vol. 4. Intergroup Relations. Oxford, England: Blackwell; 2001. pp. 175–197. [Google Scholar]
- Dovidio J, Kawakami K, Johnson C, Johnson B, Howard A. The Nature of Prejudice: Automatic and Controlled Processes. Journal of Experimental Social Psychology. 1997b;33:510–540. [Google Scholar]
- Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and Distrust: The Implications of Psychological Processes for Understanding Racial Disparities in Health and Health Care. Social Science and Medicine. 2008;67(3):478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Eberly T, Davidoff A, Miller C. Managing the Gap: Evaluating the Impact of Medicaid Managed Care on Preventive Care Receipt by Child and Adolescent Minority Populations. Journal of Health Care for the Poor and Underserved. 2010;21(1):92–111. doi: 10.1353/hpu.0.0246. [DOI] [PubMed] [Google Scholar]
- Epstein AJ, Gray BH, Schlesinger M. Racial and Ethnic Differences in the Use of High-Volume Hospitals and Surgeons. Archives of Surgery. 2010;145(2):179–186. doi: 10.1001/archsurg.2009.268. [DOI] [PubMed] [Google Scholar]
- Fincher C, Williams JE, Maclean V, Allison JJ, Kiefe CI, Canto J. Racial Disparities in Coronary Heart Disease: A Sociological View of the Medical Literature on Physician Bias. Ethnicity and Disease. 2004;14(3):360–371. [PubMed] [Google Scholar]
- Ford CL, Airhihenbuwa CO. Critical Race Theory, Race Equity, and Public Health: Toward Antiracism Praxis. American Journal of Public Health. 2010;100(Supplement 1):S30–S35. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaertner SL, Dovidio JF. Reducing Intergroup Bias: The Common Ingroup Identity Model. Philadelphia, PA: Psychology Press; 2000. [Google Scholar]
- Galinsky AD, Moskowitz GB. Perspective-Taking: Decreasing Stereotype Expression, Stereotype Accessibility, and In-Group Favoritism. Journal of Personality and Social Psychology. 2000;78(4):708–724. doi: 10.1037//0022-3514.78.4.708. [DOI] [PubMed] [Google Scholar]
- Gates H, Steele C. A Conversation with Claude M. Steele: Stereotype Threat and Black Achievement. Du Bois Review: Social Science Research on Race. 2009;6(2):251–271. [Google Scholar]
- Goff PA, Steele CM, Davies PG. The Space Between Us: Stereotype Threat and Distance in Interracial Contexts. Journal of Personality and Social Psychology. 2008;94(1):91–107. doi: 10.1037/0022-3514.94.1.91. [DOI] [PubMed] [Google Scholar]
- Gomez A, Dovidio JF, Huici C, Gaertner SL, Cuadrado I. The Other Side of We: When Outgroup Members Express Common Identity. Personality and Social Psychology Bulletin. 2008;34(12):1613–1626. doi: 10.1177/0146167208323600. [DOI] [PubMed] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit Bias among Physicians and Its Prediction of Thrombolysis Decisions for Black and White Patients. Journal of General Internal Medicine. 2007a;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green LA, Wyszewianski L, Lowery JC, Kowalski CP, Krein SL. An Observational Study of the Effectiveness of Practice Guideline Implementation Strategies Examined According to Physicians’ Cognitive Styles. Implementation Science. 2007b;2(1):41. doi: 10.1186/1748-5908-2-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and Using the Implicit Association Test: III. Meta-Analysis of Predictive Validity. Journal of Personality and Social Psychology. 2009;97(1):17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- Hausmann LR, Jeong K, Bost JE, Ibrahim SA. Perceived Discrimination in Health Care and Use of Preventive Health Services. Journal of General Internal Medicine. 2008;23(10):1679–1684. doi: 10.1007/s11606-008-0730-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh AT, Jensen MP, Robinson ME. Evaluation of Nurses’ Self-Insight into Their Pain Assessment and Treatment Decisions. Journal of Pain. 2010;11(5):454–461. doi: 10.1016/j.jpain.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson Kareem J, Fredrickson Barbara L. “We All Look the Same to Me”: Positive Emotions Eliminate the Own-Race Bias in Face Recognition. Psychological Science. 2005;16:875–881. doi: 10.1111/j.1467-9280.2005.01631.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jost JT, Banaji MR. The Role of Stereotyping in System-Justification and the Production of False Consciousness. British Journal of Social Psychology. 1994;33:1–27. [Google Scholar]
- The Kaiser Family Foundation (KFF) [accessed July 10, 2010];National Survey of Physicians, Part I: Doctors on Disparities in Medical Care. 2002 Mar;:2. 〈 http://www.kff.org/minorityhealth/20020321a-index.cfm〉.
- Kelley E, Moy E, Stryer D, Burstin H, Clancy C. The National Healthcare Quality and Disparities Reports: An Overview. Medical Care. 2005;43(3 Supplement):I3–8. doi: 10.1097/00005650-200503001-00002. [DOI] [PubMed] [Google Scholar]
- King ML. Presentation at the Second National Convention of the Medical Committee for Human Rights; Chicago, IL. March 25.1966. [Google Scholar]
- Le Cook B, Mcguire TG, Zuvekas SH. Measuring Trends in Racial/Ethnic Health Care Disparities. Medical Care Research Review. 2009;66(1):23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Ayers SL, Kronenfeld JJ. The Association Between Perceived Provider Discrimination, Healthcare Utilization, and Health Status in Racial and Ethnic Minorities. Ethnicity and Disease. 2009;19(3):330–337. [PMC free article] [PubMed] [Google Scholar]
- McConnell AR, Leibold JM. Relations Between the Implicit Association Test, Explicit Racial Attitudes, and Discriminatory Behavior. Journal of Experimental Social Psychology. 2001;37:435–442. [Google Scholar]
- Merrill JM, Laux LF, Lorimor R, Thornby JI, Vallbona C. Authoritarianism’s Role in Medicine. American Journal of Medical Science. 1995;310(3):87–90. doi: 10.1097/00000441-199531030-00001. [DOI] [PubMed] [Google Scholar]
- Monteith MJ, Mark AY, Ashburn-Nardo L. The Self-regulation of Prejudice: Toward Understanding its Lived Character. Group Processes and Intergroup Relations. 2010;13:183–200. [Google Scholar]
- Monteith MJ, Sherman JW, Devine PG. Suppression as a Stereotype Control Strategy. Personal Social Psychology Review. 1998;2(1):63–82. doi: 10.1207/s15327957pspr0201_4. [DOI] [PubMed] [Google Scholar]
- Moy E, Dayton E, Clancy CM. Compiling the Evidence: The National Healthcare Disparities Reports. Health Affairs. 2005;24(2):376–387. doi: 10.1377/hlthaff.24.2.376. [DOI] [PubMed] [Google Scholar]
- Newhouse D. Service Score Segmentation of Diverse Populations to Improve Patient and Physician Satisfaction—A Multicase Quality Improvement Study. Permanente Journal. 2009;13(4):34–41. doi: 10.7812/tpp/09-069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunez-Smith M, Pilgrim N, Wynia M, Desai MM, Jones BA, Bright C, Krumholz HM, Bradley EH. Race/Ethnicity and Workplace Discrimination: Results of a National Survey of Physicians. Journal of General Internal Medicine. 2009;24(11):1198–1204. doi: 10.1007/s11606-009-1103-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olomu AB, Grzybowski M, Ramanath VS, Rogers AM, Vautaw BM, Chen B, Roychoudhury C, Jackson EA, Eagle KA. Evidence of Disparity in the Application of Quality Improvement Efforts for the Treatment of Acute Myocardial Infarction: The American College of Cardiology’s Guidelines Applied in Practice Initiative in Michigan. American Heart Journal. 2010;159(3):377–384. doi: 10.1016/j.ahj.2009.12.014. [DOI] [PubMed] [Google Scholar]
- Paluck EL. Reducing Intergroup Prejudice and Conflict Using the Media: A Field Experiment in Rwanda. Journal of Personality and Social Psychology. 2009;96(3):574–587. doi: 10.1037/a0011989. [DOI] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, Markova T. Aversive Racism and Medical Interactions with Black Patients: A Field Study. Journal of Experimental Social Psychology. 2010;46(2):436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry SP, Murphy MC. Responses to Prejudice Feedback on the Race Implicit Association Test and the Role of Bias Awareness. 2011. Forthcoming. [Google Scholar]
- Pettigrew TF, Tropp LR. How Does Intergroup Contact Reduce Prejudice? Meta-Analytic Tests of Three Mediators. European Journal of Social Psychology. 2008;38(6):922–934. [Google Scholar]
- Phelan SM, van Ryn M, Wall M, Burgess D. Understanding Primary Care Physicians’ Treatment of Chronic Low Back Pain: The Role of Physician and Practice Factors. Pain Medicine. 2009;10(7):1270–1279. doi: 10.1111/j.1526-4637.2009.00717.x. [DOI] [PubMed] [Google Scholar]
- Plant EA, Butz DA. The Causes and Consequences of an Avoidance-Focus for Interracial Interactions. Personality and Social Psychology Bulletin. 2006;32(6):833–846. doi: 10.1177/0146167206287182. [DOI] [PubMed] [Google Scholar]
- Plant EA, Devine PG. The Active Control of Prejudice: Unpacking the Intentions Guiding Control Efforts. Journal of Personal Social Psychology. 2009;96(3):640–652. doi: 10.1037/a0012960. [DOI] [PubMed] [Google Scholar]
- Powell Adam A, Branscombe Nyla R, Schmitt Michael T. Inequality as Ingroup Privilege or Outgroup Disadvantage: The Impact of Group Focus on Collective Guilt and Interracial Attitudes. Personality and Social Psychology Bulletin. 2005;31(4):508–521. doi: 10.1177/0146167204271713. [DOI] [PubMed] [Google Scholar]
- Pratto Felicia, Sidanius Jim, Stallworth Lisa M, Malle Bertram F. Social Dominance Orientation: A Personality Variable Predicting Social and Political Attitudes. Journal of Personality and Social Psychology. 1994;67(4):741–763. [Google Scholar]
- Pugh SD, Dietz J, Brief AP, Wiley JW. Looking Inside and Out: The Impact of Employee and Community Demographic Composition on Organizational Diversity Climate. Journal of Applied Psychology. 2008;93(6):1422–1428. doi: 10.1037/a0012696. [DOI] [PubMed] [Google Scholar]
- Purdie-Vaughns V, Steele CM, Davies PG, Ditlmann R, Crosby JR. Social Identity Contingencies: How Diversity Cues Signal Threat or Safety for African Americans in Mainstream Institutions. Journal of Personality and Social Psychology. 2008;94(4):615–630. doi: 10.1037/0022-3514.94.4.615. [DOI] [PubMed] [Google Scholar]
- Roter D. The Medical Visit Context of Treatment Decision-Making and the Therapeutic Relationship. Health Expectations. 2000;3(1):17–25. doi: 10.1046/j.1369-6513.2000.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians’ Implicit and Explicit Attitudes About Race by MD Race, Ethnicity, and Gender. Journal of Health Care for the Poor and Underserved. 2009;20(3):896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Rivara FP, Greenwald AG. Physician Implicit Attitudes and Stereotypes About Race and Quality of Medical Care. Medical Care. 2008;46(7):678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- Saha S, Guiton G, Wimmers PF, Wilkerson L. Student Body Racial and Ethnic Composition and Diversity-Related Outcomes in U.S. Medical Schools. Journal of the American Medical Association. 2008;300(10):1135–1145. doi: 10.1001/jama.300.10.1135. [DOI] [PubMed] [Google Scholar]
- Schmader T, Johns M, Forbes C. An Integrated Process Model of Stereotype Threat Effects on Performance. Psychology Review. 2008;115(2):336–356. doi: 10.1037/0033-295X.115.2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidanius J, Levin S, Federico C, Pratto F. Legitimizing Ideologies: The Social Dominance Approach. In: Jost JT, Major B, editors. The Psychology of Legitimacy: Emerging Perspectives on Ideology, Justice, and Intergroup Relations. New York: Cambridge University Press; 2001. pp. 307–331. [Google Scholar]
- Bear Siegel BD, Andres E, Mead H. Measuring Equity: An Index of Health Care Disparities. Quality Managed Health Care. 2009;18(2):84–90. doi: 10.1097/01.QMH.0000349973.61836.41. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- Smith WR, Betancourt JR, Wynia MK, Bussey-Jones J, Stone VE, Phillips CO, Fernandez A, Jacobs E, Bowles J. Recommendations for Teaching About Racial and Ethnic Disparities in Health and Health Care. Annals of Internal Medicine. 2007;147(9):654–665. doi: 10.7326/0003-4819-147-9-200711060-00010. [DOI] [PubMed] [Google Scholar]
- Sorkin DH, Ngo-Metzger Q, De Alba I. Racial/Ethnic Discrimination in Health Care: Impact on Perceived Quality of Care. Journal of General Internal Medicine. 2010;25(5):390–396. doi: 10.1007/s11606-010-1257-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer SJ, Steele CM, Quinn DM. Stereotype Threat and Women’s Math Performance. Journal of Experimental Social Psychology. 1999;35:4–28. [Google Scholar]
- Steele CM. Race and the Schooling of Black Americans. The Atlantic Monthly. 1992;269(4):68–78. [Google Scholar]
- Steele CM, Aronson J. Stereotype Threat and the Intellectual Test Performance of African Americans. Journal of Personality and Social Psychology. 1995;69(5):797–811. doi: 10.1037//0022-3514.69.5.797. [DOI] [PubMed] [Google Scholar]
- Stewart M, Brown JB, Donner A, Mcwhinney IR, Oates J, Weston WW, Jordan J. The Impact of Patient-Centered Care on Outcomes. Journal of Family Practice. 2000;49(9):796–804. [PubMed] [Google Scholar]
- Street RL, Jr, Gordon H, Haidet P. Physicians’ Communication and Perceptions of Patients: Is It How They Look, How They Talk, or Is It Just the Doctor? Social Science and Medicine. 2007;65(3):586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamblyn R, Berkson L, Dauphinee WD, Gayton D, Grad R, Huang A, Isaac L, Mcleod P, Snell L. Unnecessary Prescribing of NSAIDs and the Management of NSAID-Related Gastropathy in Medical Practice. Annals of Internal Medicine. 1997;127(6):429–438. doi: 10.7326/0003-4819-127-6-199709150-00003. [DOI] [PubMed] [Google Scholar]
- van Ryn M, Burgess D, Malat J, Griffin J. Physicians’ Perceptions of Patients’ Social and Behavioral Characteristics and Race Disparities in Treatment Recommendations for Men with Coronary Artery Disease. American Journal of Public Health. 2006;96(2):351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M, Burke J. The Effect of Patient Race and Socio-Economic Status on Physicians’ Perceptions of Patients. Social Science and Medicine. 2000;50(6):813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- van Ryn M, Fu SS. Paved with Good Intentions: Do Public Health and Human Service Providers Contribute to Racial/Ethnic Disparities in Health? American Journal of Public Health. 2003;93(2):248–255. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White-Means S, Zhiyong Dong, Hufstader M, Brown LT. Cultural Competency, Race, and Skin Tone Bias among Pharmacy, Nursing, and Medical Students: Implications for Addressing Health Disparities. Medical Care Research Review. 2009;66(4):436–455. doi: 10.1177/1077558709333995. [DOI] [PubMed] [Google Scholar]
- Williams ES, Manwell LB, Konrad TR, Linzer M. The Relationship of Organizational Culture, Stress, Satisfaction, and Burnout with Physician-Reported Error and Suboptimal Patient Care: Results from the Memo Study. Health Care Management Review. 2007;32(3):203–212. doi: 10.1097/01.HMR.0000281626.28363.59. [DOI] [PubMed] [Google Scholar]