Abstract
The discovery of chemoresistant cancer stem cells (CSCs) in carcinomas has created the need for therapies that specifically target these subpopulations of cells. Here we characterized a bispecific targeted toxin that is composed of two antibody fragments and a catalytic protein toxin allowing it to bind two CSC markers on the same cell and kill this resistant subpopulation. CD133 is a well-known CSC marker and has been successfully targeted and caused regression of head and neck squamous cell carcinoma (HNSCC) in vivo. To enable it to bind a broader range of CSCs, an anti-EpCAM scFv was added to create dEpCAMCD133KDEL, a deimmunized bispecific targeted toxin on a single amino acid chain. This bispecific potently inhibited protein translation and proliferation in vitro in three different types of carcinoma. Furthermore, in a CSC spheroid model dEpCAMCD133KDEL eliminated Mary-X spheroids, an inflammatory breast carcinoma. Finally, this bispecific also caused tumor regression in an in vivo model of HNSCC. This represents the first bispecific CSC targeted toxin and warrants further development as a possible therapy for carcinoma.
Keywords: Cancer stem cells, targeted toxins, immunotoxins, CD133, EpCAM, head and neck squamous cell carcinoma
Introduction
Epithelial cell adhesion molecule, or EpCAM, is an established cancer target for drug therapy and has many diverse roles in cancer cells such as cell signaling, proliferation, differentiation, and migration (1,2). Recently, interest has intensified since EpCAM has also been shown to be a direct target in the Wnt/β-catenin signaling pathway, a key pathway used by both cancer stem cells (CSCs) and normal adult stem cells that enables cells to self-renew and differentiate into multiple cell types. Mutations or disruptions in this pathway in normal stem cells can lead to excessive proliferation and stem cell self-renewal resulting in tumor formation (3,4). Unsurprisingly then, it has been shown that high levels of EpCAM expression correlates with increased tumorigenesis in a range of carcinomas including breast, colon, and head and neck squamous cell carcinoma (HNSCC) (5,6). All of this has made EpCAM an attractive marker for targeted therapy.
CD133 was originally discovered as a pentaspan membrane glycoprotein that was a marker for a population of hematopoietic stem cells (7). Now it is an established CSC marker in many carcinomas such as breast, colon, prostate, and HNSCC among others (8,9). Like EpCAM, CD133 is involved in the Wnt/β-catenin signaling pathway (10,11,12). We recently synthesized a new anti-CD133 monoclonal antibody (clone 7) that differs from other anti-CD133 antibodies in that it recognizes the extracellular domain and is cross-reactive with mouse CD133 (13). The scFv from this monoclonal antibody was used to construct a deimmunized anti-CD133 targeted toxin, called dCD133KDEL, which showed efficacy against HNSCC, breast, and ovarian carcinoma in vitro and in vivo (14,15,16). These findings validated our strategy of targeting CSC, which are critical in cancer cell self-renewal and drug refractory relapse.
Our laboratory has specialized in development of new biological drugs that are best described as bispecific targeted toxins because they consist of two cancer cell-directed ligands on the same molecule as a catalytic toxin (17,18,19,20). Because of the efficacy shown by a novel monospecific CD133- directed targeted toxin (14) and the promising results of clinical trials using a monospecific anti-EpCAM TT (21,22,23), we synthesized a novel bispecific TT using both anti-EpCAM and anti-CD133 scFvs. A targeted toxin is a biological drug consisting of a ligand specific for a given cell surface receptor conjugated to a catalytic protein toxin. TTs have been shown to be useful in cancer therapy and provide potent and selective toxicity in targeted cells. The first step in the mechanism of TT action is the binding of the ligand portion of the molecule to the specific receptor. The receptor then must be internalized. The TT then escapes from its vesicle into the cytosol where the toxin portion binds and inhibits its target. Pseudomonas exotoxin (PE) functions by ADP-ribosylation of EF2 thereby inhibiting translation and inducing cell death (24). In our studies, we used a genetically deimmunized variant of PE that was modified to include the lysosomal retention sequence and C-terminal signal Lys-Asp-Glu-Leu (KDEL) to enhance its potency (14,17,19,25).
In this article, we show that a novel bispecific CSC TT, dEpCAMCD133KDEL, potently inhibits multiple carcinoma lines in vitro, and causes regression in HNSCC tumors in vivo. This represents the first bispecific CSC targeting agent and warrants further development as a possible clinical adjunct for cancer therapy.
Materials and Methods
Construction of dEpCAMCD133KDEL
DNA of dEpCAMCD133KDEL was synthesized using DNA shuffling and DNA ligation techniques resulting in the fusion of genes encoding the humanized anti-EpCAM scFv from the antibody MOC31, anti-CD133 scFV from Clone 7, and a deimmunized truncated form of pseudomonas exotoxin 38 used previously (14,17,18,19). The resulting fusion DNA sequence contained (5’-3’) and NcoI restriction site, an ATG initiation codon, the EpCAM scFv, the CD133 scFv, a 7 amino-acid EASGGPE linker, the gene encoding the deimmunized truncated PE38 with a DNA sequence encoding KDEL replacing the REDLK, followed by a NotI restriction site at the 3’ end of the DNA fusion sequence. This gene was then spliced into the pET21d bacterial expression vector containing an inducible isopropyl-b-D-thiogalactopyranoside (IPTG) T7 promoter and a carbenicillin selection gene. The DNA sequence was verified by DNA sequence analysis done at the University of Minnesota BioMedical Genomics Center [Minneapolis, MN].
Purification of dEpCAMCD133KDEL
Purification was performed as described previously (26). Briefly, the protein was expressed and purified from inclusion bodies using the Novagen pET expression system [Darmstadt, Germany]. Then a 2-step purification procedure was performed using an ion exchange fast protein liquid chromatography (Q sepharose Fast Flow, Sigma)[Saint Louis, MO] followed by size exclusion chromatography (Hiload Superdex 200, GE Life Sciences)[Uppsala, Sweden]. The purified protein was then analyzed by Bradford to determine the concentration and by SDS-PAGE stained with Coomassie Brilliant Blue to determine purity. The CD133 scFv from clone 7 and an anti-EpCAM Fc that was used to construct another bispecific TT described previously (20) were also produced and purified using this purification procedure and used in flow cytometric assays to determine the binding of dEpCAMCD133KDEL.
Cell lines and culturing techniques
UMSCC-11B is an HNSCC line that was derived from larynx tumor following chemotherapy (27). UMSCC11B-luc was transfected using a luciferase reporter construct, and maintained with 10 mg/mL of blastocidin. Cells were transfected using Invitrogen's Lipofectamine Reagent. NA-SCC is another HNSCC line isolated from a tongue tumor (28). Both lines were obtained from Dr. Frank Ondrey (University of Minnesota) who previously obtained them from their originator, Dr. Thomas E. Carey, Department of Otolaryngology-Head and Neck Surgery, University of Michigan in 2009. NA-SCC and UMSCC-11B cell lines were authenticated this year by STR testing done by the Fragment Analysis Facility, John Hopkins University. Caco-2 and HT-29 (colorectal carcinomas), BT-474 and SK-BR3 (breast carcinomas), Raji and Daudi (B-cell lymphomas), and U-87 (glioblastoma) were obtained from ATCC [Manassas, VA] and were positive for the appropriate markers. Only cells that were greater than 90% viable were used for experimentation. Mary-X is an inflammatory breast carcinoma spheroid line and was obtained from Dr. Sanford Barsky (University of Nevada).
Flow cytometry
EpCAM and CD133 expression was analyzed using a FACSCalibur at the University of Minnesota Flow Cytometry Core Facility. Antibodies and proteins used in flow cytometry were labeled with fluorescein isothiocyanate (FITC). Analysis of the results was performed using FLOWJO.
Bioassays to measure cellular proliferation
To measure the level of proliferation and the effect dEpCAMCD133KDEL was having on the carcinoma lines, 3H-thymidine (or 3H-leucine when cell lines did not take up thymidine) incorporation assays were used. Cells are plated in 96-well flat-bottomed plates and allowed to adhere overnight in appropriate media (leucine-free when 3H-leucine was used). The toxins were then added in triplicate at 10-fold dilutions to determine the IC50 values. Plates would then be incubated for an additional 48 hours. 3H-Thymidine or 3H-leucine would then be added for a final 18-hour incubation. Plates were then frozen to detach cells, and then thawed and harvested onto glass fiber filters, which were then washed, dried, and counted using standard scintillation methods. Trypan blue viability assays were also done to test the activity of dEpCAMCD133KDEL against the HNSCC lines. This was performed as described previously (14). Briefly, cells were plated in 24 well plates and toxin added daily. Cells were harvested using typsin and counted using trypan blue. For the Mary-X spheroid assay, Spheroids were plated into 24 well plates and counted to determine the starting number of spheroids per well. Then toxin was added daily and the number of spheroids counted on subsequent days. GraphPad Prism was used to analyze and graph all assay results. Data is reported as the percentage of control counts in the 3H-Thymidine or 3H-leucine assays and the Mary-X assay, and as cell number in the trypan blue viability assays. All assays were repeated at least three times to ensure reproducibility, and representative figures are shown.
Tumor treatment studies
For study one, six million UMSCC-11B/luc cells were injected into the right flank of 15 nude mice. Starting on day 7, tumors were treated with 20ug/mouse of dEpCAMCD133KDEL, 2219KDEL, or 100ul of saline. Mice were given four courses of injections where one course was 3 injections given every other day (MWF) for one week. Mice were weighed weekly and weights were recorded. Image could not be obtained for mouse 2 in the dEpCAMCD133KDEL group for day 48, but was visibly tumor free by caliper measurement.
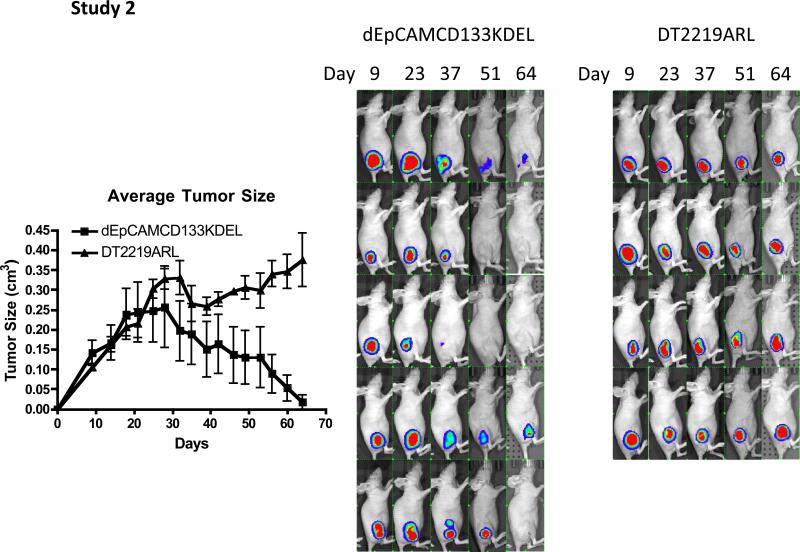
For study two, 3.5 million UMSCC-11B/luc cells were injected into the right flanks of 9 nude mice. Treatment began on day 12 and continued 4 times a week (MTWTh) for 7 weeks with 5 mice receiving 20ug of dEpCAMCD133KDEL and the remaining 4 mice receiving 10ug of DT2219ARL control, which is its MTD.
For both studies, mice were imaged every other week using the Xenogen Ivis 100 imaging system and analyzed with Living Image 2.5 software [Xenogen Corporation, Cranbury, New Jersey]. Mice were injected with 3 mg of luciferin substrate 10 minutes before imaging and anesthetized via isoflurane gas inhalation. Two-minute exposures were performed to capture tumor fluorescence. Units for the regions of interest are expressed as photons/sec/cm2/sr.
Results
dEpCAMCD133KDEL binds selectively
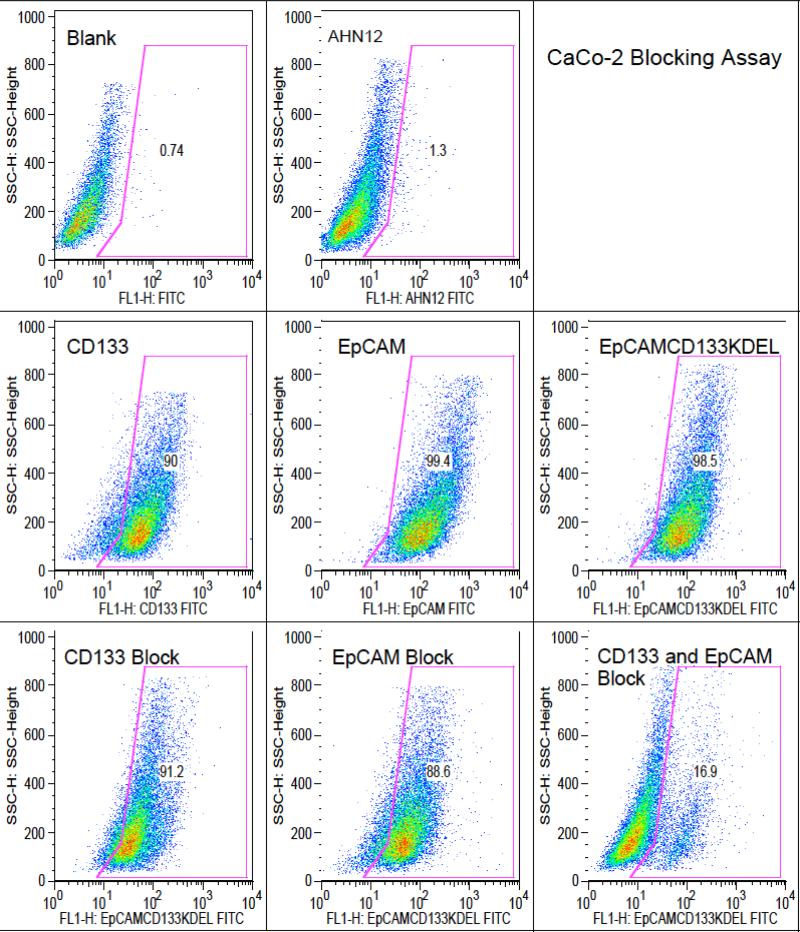
To determine whether both scFv portions of dEpCAMCD133KDEL were functional and bound their respective receptors, flow cytometry was performed on Caco-2 cells, a colon carcinoma. Caco-2 highly expresses both EpCAM and CD133. As can be seen from Figure 1, FITC labeled CD133 scFv from clone 7 and a humanized EpCAM Fc bound and were 90% and 99.4% positive respectively, while dEpCAMCD133KDEL bound with high affinity as well. When dEpCAMCD133KDEL was blocked with either unlabeled CD133scFv or unlabeled EpCAM separately, the bispecific was still able to bind via its other ligand. But when unlabeled CD133 and EpCAM were both added the binding of dEpCAMCD133KDEL was blocked.
Figure 1.
Flow cytometry was performed on Caco-2 cells to test the binding ability of FITC labeled dEpCAMCD133KDEL. When either CD133 scFv or EpCAM scFv were added separately with dEpCAM133KDEL-FITC to the cells they did not block the binding of the bispecific drug. In contrast, when both were added in combination, the binding of dEpCAMCD133KDEL was significantly reduced indicating that both binding domains of dEpCAMCD133KDEL are functional. When one receptor is blocked, the other is still free to bind. However, when both are simultaneously blocked, binding cannot occur.
Another colon carcinoma, HT-29, was tested for its level of EpCAM and CD133 expression and determine whether it might be a suitable target for dEpCAMCD133KDEL. As seen in Table 1, HT-29 was 98.8% EpCAM positive and 2.61% CD133 positive. The table also shows two HNSCCs (UMSCC-11B and NA-SCC) and two breast carcinomas (BT-474 and SKBR3) which all showed low levels of CD133 expression and very high levels of EpCAM expression. Two negative control cell lines, U87 and Raji, were also tested on flow cytometry and also expressed low levels of CD133, but both had negligible EpCAM expression.
Table 1.
Flow cytometry was performed on a number of cancer lines to determine the level EpCAM and CD133 positivity. As shown here, colon carcinoma, HNSCC, and breast carcinoma lines were highly positive for EpCAM, and had a subpopulation of CD133+ cells. Caco-2 was the only line tested that was highly positive for both EpCAM and CD133. U87, a glioblastoma, was mostly negative for EpCAM, but still had a small subpopulation of CD133+ cells. A CD45 antibody, AHN-12, was used as a negative control for all the cell lines except Raji, a B cell lymphoma, where it acted as the positive control.
| Cell Line | EpCAM+ | CD133+ | AHN12 |
|---|---|---|---|
| Caco-2 | 99.4 | 90.0 | 1.3 |
| HT-29 | 98.8 | 2.61 | 2.18 |
| UMSCC-11B | 98.3 | 5.90 | 0.50 |
| NA-SCC | 97.9 | 5.88 | 0.65 |
| BT-474 | 97.2 | 4.09 | 0.47 |
| SK-BR3 | 96.7 | 4.40 | 0.98 |
| U87 | 1.33 | 2.38 | 0.46 |
| Raji | 0.27 | 2.27 | 91.2 |
Bioassays show dEpCAMCD133KDEL activity
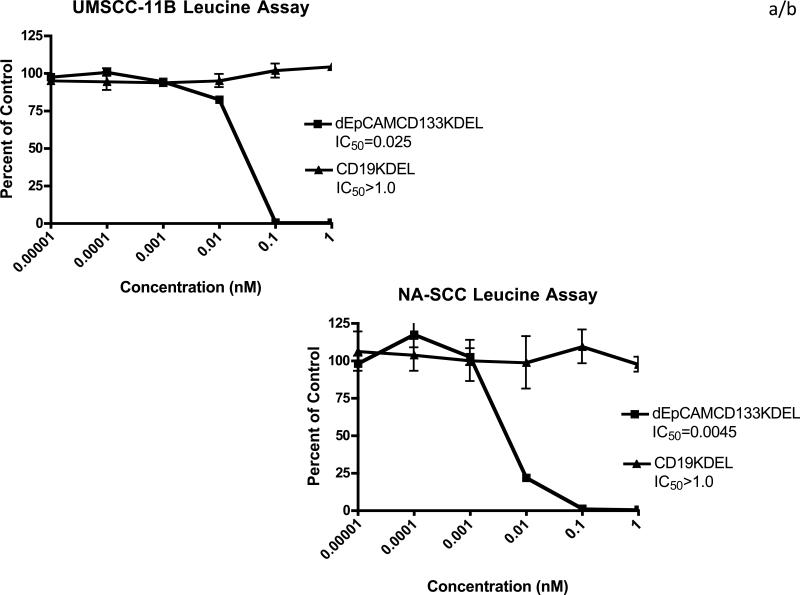
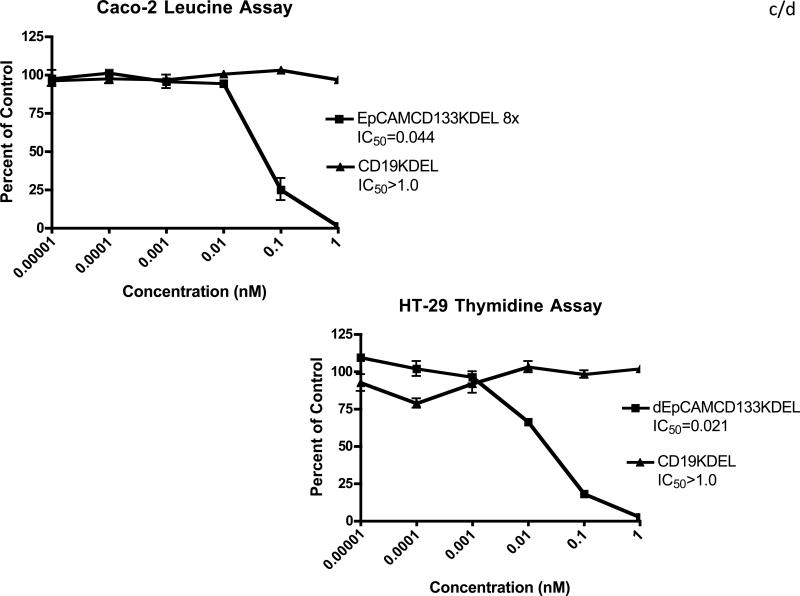
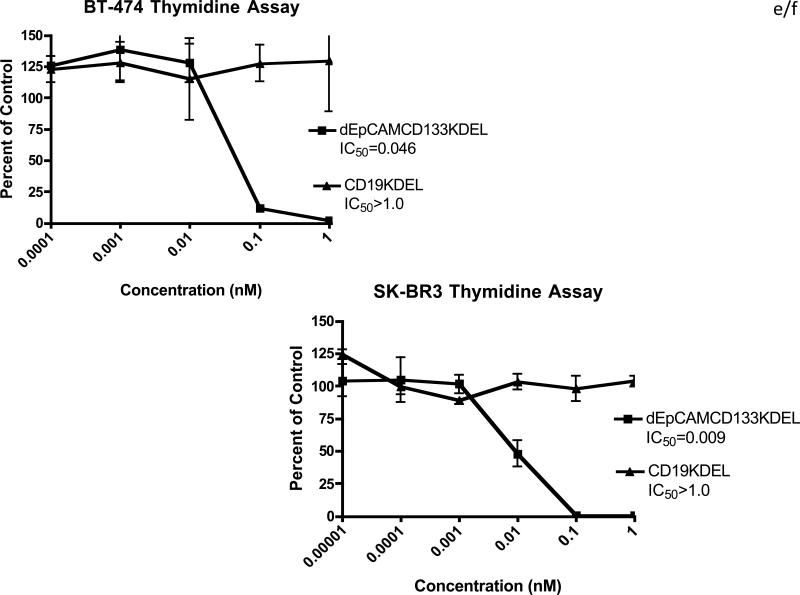
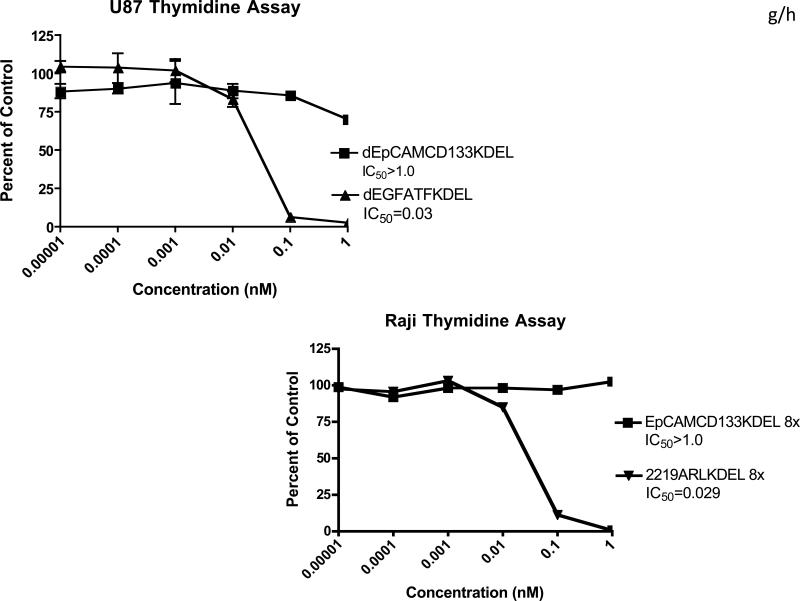
To test the efficacy of dEpCAMCD133KDEL, the HNSCC lines were tested in 3H-Leucine incorporation assays to determine the level of protein translation inhibition. As seen in Figure 2a and b, dEpCAMCD133KDEL inhibited both UMSCC-11B and NA-SCC with IC50 values of 0.025nM and 0.0045nM respectively. Similar IC50 values were obtained when the two colon carcinoma lines were tested. Furthermore, dEpCAMCD133KDEL showed subnanomolar activity against the two breast carcinomas shown in Figure 2e and 2f as well. However, as seen in Figure 2g and 2h, the two EpCAM negative cell lines were not affected by dEpCAMCD133KDEL at the concentrations tested, while positive controls potently inhibited proliferation.
Figure 2.
Leucine and thymidine incorporation assays show the ability of dEpCAMCD133KDEL to inhibit the proliferation of carcinoma lines. UMSCC-11B (A) and NA-SCC (B) cells were incubated with dEpCAMCD133KDEL and the 50% inhibitory concentration (IC50) was determined to be 0.025nM and 0.0045nM respectively. Two colon carcinoma lines Caco-2 (C) and HT-29 (D) also were potently inhibited by dEpCAMCD133KDEL with IC50 values of 0.044nM and 0.02nM1 respectively. dEpCAMCD133KDEL was also tested against BT-474 (E) and SK-BR3 (F) two breast carcinomas and subnanomolar IC50 values were 0.046nM and 0.009nM respectively. Finally, two negative control lines were tested to test the specificity of dEpCAMCD133KDEL. U87 is a glioblastoma line that is EpCAM negative and has little CD133 expression. dEpCAMCD133KDEL had no effect, while the positive control targeted toxin, dEGFATFKDEL had an IC50 of 0.03nM. Likewise dEpCAMCD133KDEL had no effect on Raji, a B cell lymphoma, but the positive control targeted toxin d2219ARLKDEL inhibited with an IC50 value of 0.029nM.
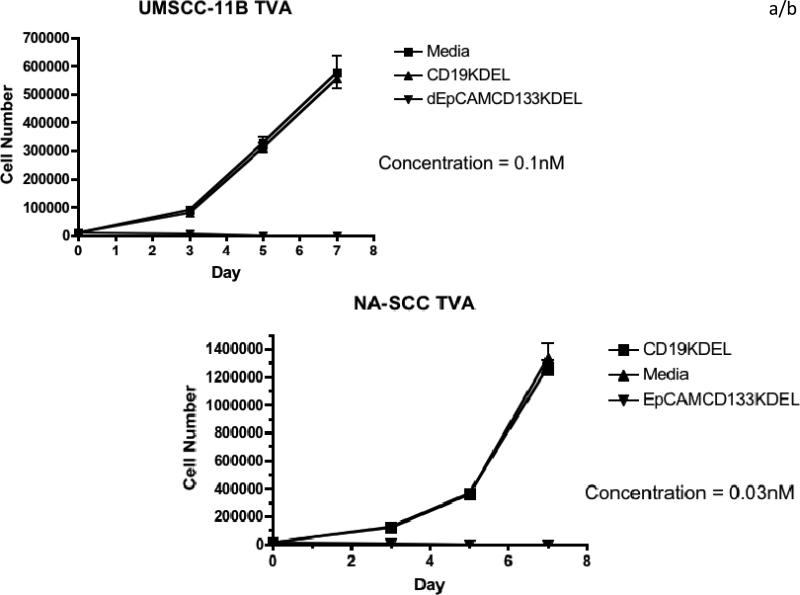
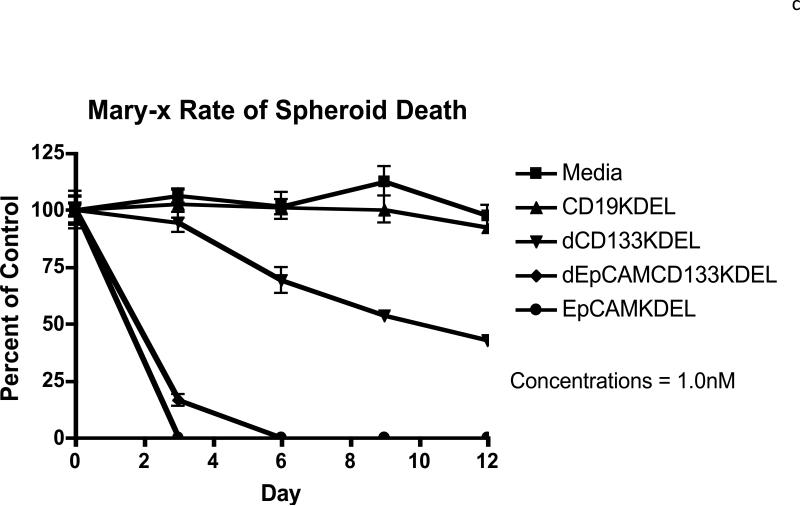
To determine whether the inhibition of protein translation was causing cell death in the cancer lines, time course viability assays were performed. As seen in Figure 3a, dEpCAMCD133KDEL killed all UMSCC-11B carcinoma cells while a negative control TT, CD19KDEL, did not. NA-SCC cells were killed in the same manner in Figure 3b. Furthermore, when inflammatory breast carcinoma Mary-X spheroids were tested in a time course spheroid assay in Figure 3c, dEpCAMCD133KDEL eliminated the spheroids while the negative control had no effect. The monospecific targeted toxins were also tested in this assay and both were also able to eliminate tumor spheroids over time.
Figure 3.
Time course viability assays were performed for the two HNSCC lines, UMSCC-11B (A) and NA-SCC (B). In both assays, dEpCAMCD133KDEL killed all cells as determined by viability staining using trypan blue. (C) dEpCAMCD133KDEL also eliminated Mary-X spheroids completely by day 5 in a time course spheroid assay. The monospecifics, EpCAMKDEL and dCD133KDEL, also were effective at eliminating tumor spheroids compared to the negative control targeted toxin, CD19KDEL, and the media control.
dEpCAMCD133KDEL effective in HNSCC mouse studies
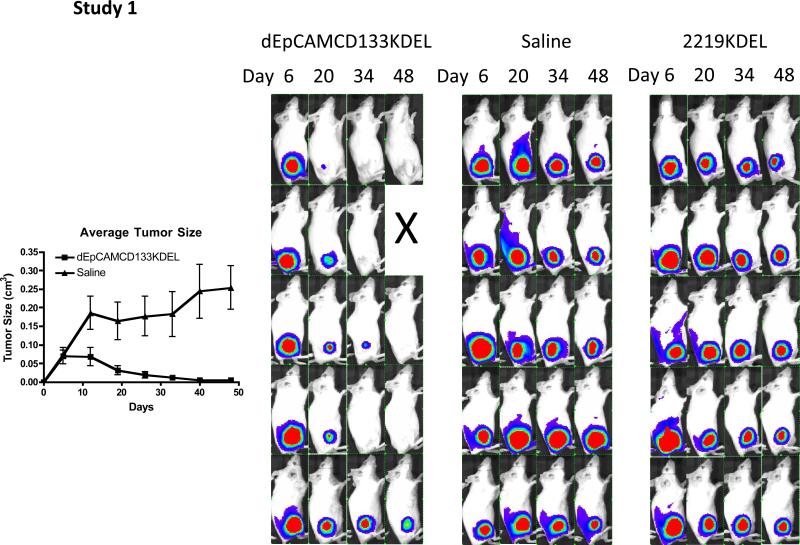
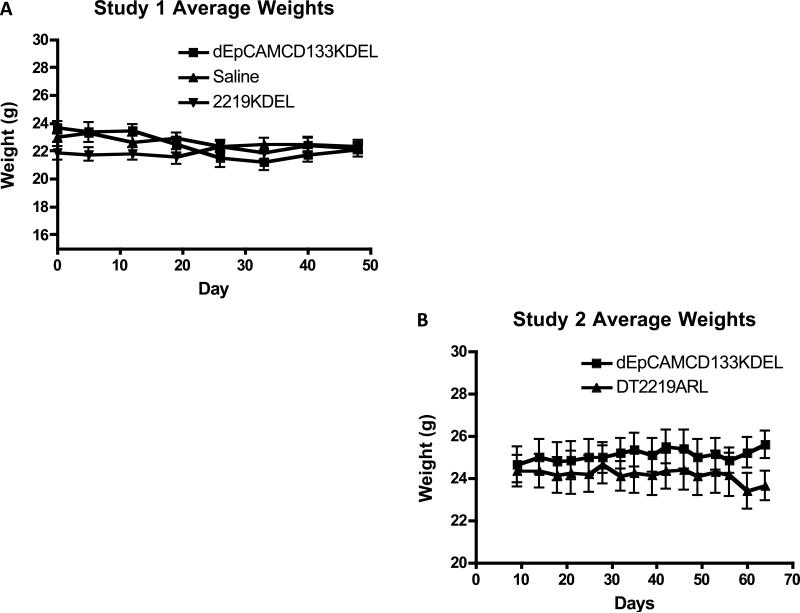
To determine the ability of dEpCAMCD133KDEL to cause tumor regression in vivo, nude mice were injected with UMSCC-11B/luc cells into their right flanks. In the first study (Figure 4), 3 groups of mice (5 mice/group) were treated intratumorally starting on day 7. Thus, these were smaller tumors at the time that therapy was initiated. Treatment was discontinued on day 40. All 5 dEpCAMCD133KDEL treated tumors regressed, with 4 mice achieving tumor-free status. Caliper data reflected the imaging results. In the second study shown in Figure 5, tumors were permitted to grow larger and become more established before therapy was begun. Mice were treated intratumorally starting on day 12 instead of day 7. One group of 5 mice were treated with dEpCAMCD133KDEL and another group treated with the negative control DT2219ARL since there are no B cell markers on UMSCC-11B. Treatment was discontinued on day 63. Figure 5 shows that all tumors responded to dEpCAMCD133KDEL therapy and three of the tumors completely regressed. The negative control tumors were unaffected. The drop in tumor size in the DT2219ARL group on day 32 occurred because 2 of the 4 tumors ulcerated causing a temporary decrease in tumor size. Interestingly, regressions did take place slowly overtime in keeping with our hypothesis that destruction of CSC prevented self-renewal. We did not see any significant weight loss in either study, which would have been indicative of toxicity. As seen in Figure 6, the average weights remained steady throughout each study.
Figure 4.
In experiment 1, UMSCC-11B/luc cells were injected into the right flanks of nude mice and treatment began on day 7. dEpCAMCD133KDEL caused tumor regression in all treated animals, with 4 of 5 being tumor free on day 48. The average tumor measurement by caliper measurement corresponds to the imaging data showing tumor regression in the dEpCAMCD133KDEL treated mice.
Figure 5.
In experiment 2, UMSCC-11B/luc cells were injected into the right flanks of nude mice and allowed to grow until day 12 when treatment began. The starting average tumor size was almost twice the starting size of the tumors in experiment 1. Imaging and caliper data show tumor regression in all 5 dEpCAMCD133KDEL treated mice, while the negative control, DT2219ARL, had no effect. 3 out of 5 mice were tumor free when the study was discontinued on day 64.
Figure 6.
Average group weights from mouse experiment 1 (A) and experiment 2 (B) are shown. No toxic side effects were visually observed in the mice. Additionally, no significant weight loss occurred despite the high multiple dosing indicating the absence of significant off target effects by dEpCAMCD133KDEL.
In order to evaluate whether the monospecific drugs were as effective as the bispecific drug, in experiment 2, a third group of mice were treated with monospecific anti-CD133 targeted toxin (not shown). In this case, responses were noted, but not all of the animals completely responded as they did for the bispecific drug. Thus, in vivo findings correlated with the in vitro Mary-X data shown in Figure 3c in that the dEpCAM133KDEL was more effective than monospecific dCD133KDEL. Also, it was not possible to assess monospecific EpCAMKDEL at this dose since it exceeded the MTD and was toxic to the mice.
Discussion
A common problem in carcinoma therapy is drug refractory relapse. CSC's have been widely implicated as the particular cells responsible for the development of this tumor chemoresistance (8,29-32). Therefore, it is imperative that adjunct therapies are developed that can target this subpopulation of cells. We have developed and tested the first known bispecific TT specifically designed to simultaneously bind two independent markers on CSC's.
In these studies, we determined the efficacy of dEpCAMCD133KDEL against head and neck, breast, and colon carcinoma and found it potently inhibited proliferation. We also showed the ability of dEpCAMCD133KDEL to kill tumor spheroids in an in vitro assay using the transplantable human inflammatory breast carcinoma, MARY-X (33). This is significant because tumor spheroids are enriched with cancer stem cells and show enhanced tumorigenicity and clonogenic and differentiation potential (34). Furthermore, we have shown the ability of this bispecific TT to cause tumor regression of small tumors and more established tumors using an in vivo model of HNSCC. This drug is unique because not only does dEpCAMCD133KDEL target the cancer stem cell population within carcinomas via CD133, but it also can bind EpCAM, a commonly overexpressed marker in many carcinomas. EpCAM has recently been recognized as a CSC marker (5,35,36). Furthermore, high EpCAM expression correlates with increased tumorigenicity while little or no EpCAM expression does not. (5,6).
There are potential benefits to simultaneously targeting two independent markers expressed on CSCs. First, not all carcinomas express the same CSC markers (8,37). Furthermore, CSC biomarkers are imperfect in that there is a dynamic continuum where certain markers are expressed for varying amounts of time and can be reexpressed from more differentiated non-CSC populations due to back differentiation (38). For instance, markers such as CD133 that are known to be expressed on many CSC populations undergo a high rate of plasticity, a phenomenon in which CD133 expression can arise from the more differentiated CD133 negative cell population (39). Thus, using two CSC reactive ligands would target a broader population of CSCs. Targeting a marker such as EpCAM that has more widespread expression would not only target independent populations of CSCs, but also inhibit populations of cancer cells from which CSCs may arise.
The monospecific targeted toxins, EpCAMKDEL and dCD133KDEL, were tested in the in vitro Mary-X spheroid assay to determine their efficacy compared with the bispecific drug. While, EpCAMKDEL was as potent as the bispecific drug in vitro, it was much more toxic than the bispecific TT in vivo. This prevented EpCAMKDEL from being tested at the same dose as dEpCAM133KDEL. Also, the monospecific drugs are smaller than the bispecific TT and may be more readily filtered into the liver and/or kidney causing these non-target toxicities. Taken together, these data show that dEpCAMCD133KDEL was more effective compared with dCD133KDEL, dEpCAMCD133KDEL was more effective in vitro and in vivo.
A Major limitation of past TT's has been the development of neutralizing antibodies following prolonged treatment. We have addressed this issue by deimmunizing the truncated version of pseudomonas exotoxin by mutating key immunogenic epitopes on the surface of the molecule. This lowers the immunogenicity of this toxin and significantly reduces the amount of anti-toxin antibodies produced (14,40). This deimmunized toxin has been used and tested for a number of targeted toxins we have developed (14,17,19).
Past studies have shown that current chemotherapy in combination with a TT is more effective than using either therapy alone (41,42). It will be interesting to test whether this principle is also true when using a CSC targeted therapy in combination with classical chemotherapy. The hypothesis would be that the chemotherapy would target the rapidly dividing bulk of the tumor, while the CSC targeted therapy would eliminate the subpopulation of cells responsible for the development of chemoresistance. This dual approach may be necessary in order to achieve tumor regression and prevent drug refractory relapse.
We chose our animal model based on the fact that intratumoral injection is an accepted model for testing drug efficacy in head and neck cancer. There are many examples of head and neck cancer clinical trials whereby drugs are administered directly to the tumor site (21,43). Undoubtedly, this related to the accessibility of the primary tumor nodule. Still, it will be important to understand the activity of the drug when given systemically. Thus, future studies are planned to optimize the dose and dose schedules using intravenous or interperitoneal injections in other models of carcinoma.
In summary, we have developed a novel deimmunized bispecific TT that selectively binds both EpCAM and CD133 CSC markers. Targeting these drug resistant CSC offers a potential solution to our most challenging problem in cancer therapy, drug refractory relapse. dEpCAMCD133KDEL potently inhibited cellular proliferation in three different types of carcinoma. Furthermore, it caused tumor regression in in vivo studies using a HNSCC mouse model. This work represents the first known bispecific CSC TT and we believe dEpCAMCD133KDEL warrants further study as a potential therapy for use in human carcinoma.
Acknowledgements
This work was supported in part by the US Public Health Service Grant R01-CA36725 awarded by the NCI and the NIAID, DHHS, the Randy Shaver Foundation, the Atwater Cancer Drug Development Award, and a CETI translational award from the University of Minnesota Masonic Cancer Center.
Footnotes
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Trzpis M, McLaughlin PM, de Leij LM, Harmsen MC. Epithelial cell adhesion molecule: More than a carcinoma marker and adhesion molecule. Am J Pathol. 2007;171:386–395. doi: 10.2353/ajpath.2007.070152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Munz M, Baeuerie AP, Gires O. The emerging role of EpCAM in stem cell signaling. Cancer Res. 2009;69:5627. doi: 10.1158/0008-5472.CAN-09-0654. [DOI] [PubMed] [Google Scholar]
- 3.Takahashi-Yanaga F, Kahn M. Targeting Wnt signaling: Can we safely eradicate cancer stem cells? Clin Cancer Res. 2010;16:3153–3162. doi: 10.1158/1078-0432.CCR-09-2943. [DOI] [PubMed] [Google Scholar]
- 4.Moncharmont C, Levy A, Gilormini M, Bertrand G, Chargari C, Alphonse G, Ardail D, Rodriguez-Lafrasse C, Magne N. Targeting a cornerstone of radiation resistance. Cancer stem cell Cancer Lett. 2012;322:139–147. doi: 10.1016/j.canlet.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Van der Gun BT, Melchers LJ, Ruiters MH, de Leij LF, McLaughlin PM, Rots MG. EpCAM in carcinogenesis: the good, the bad or the ugly. Carcinogenesis. 2010;31:1913–1921. doi: 10.1093/carcin/bgq187. [DOI] [PubMed] [Google Scholar]
- 6.Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8:755–768. doi: 10.1038/nrc2499. [DOI] [PubMed] [Google Scholar]
- 7.Yin AH, Miraglia S, Zanjani ED, Almeida-Porada G, Ogawa M, Leary AG, Olweus J, Kearney J, Buck DW. AC133, A novel marker for human hematopoietic stem and progenitor cells. Blood. 1997;90:5002–12. [PubMed] [Google Scholar]
- 8.Boman BM, Wicha MS. Cancer stem cells: a step toward the cure. J Clin Oncol. 2008;26:2795–9. doi: 10.1200/JCO.2008.17.7436. [DOI] [PubMed] [Google Scholar]
- 9.Ferrandina G, Petrillo M, Bonanno G, Scambia G. Targeting CD133 antigen in cancer. Expert Opin Ther Targets. 2009;13:823–837. doi: 10.1517/14728220903005616. [DOI] [PubMed] [Google Scholar]
- 10.Rappa G, Fodstad O, Lorico A. The stem cell-associated antigen CD133 (Prominin-1) is a molecular therapeutic target for metastatic melanoma. Stem Cells. 2008;26:3008–3017. doi: 10.1634/stemcells.2008-0601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mak AB, Nixon AM, Kittanakom S, Stewart JM, Chen GI, Curak J, Gingras AC, Mazitschek R, Neel BG, Stagljar I, Moffat J. Regulation of CD133 by HDAC6 Promotes β-Catenin Signaling to Suppress Cancer Cell Differentiation. Cell Rep. 2012;2:951–963. doi: 10.1016/j.celrep.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takenobu H, Shimozato O, Nakamura T, Ochiai H, Yamaguchi Y, Ohira M, Nakagawara A, Kamijo T. CD133 suppresses neuroblastoma cell differentiation via signal pathway modification. Oncogene. 2011;30:97–105. doi: 10.1038/onc.2010.383. [DOI] [PubMed] [Google Scholar]
- 13.Swaminathan SK, Niu L, Waldron NN, Kalscheuer S, Zellmer D, Olin MR, Ohlfest JR, Vallera DA, Panyam J. Identification and characterization of a novel scFv recognizing human and mouse CD133. Drug Deliv and Transl Res. 2013 doi: 10.1007/s13346-012-0099-6. doi 10.1007/s13346-012-0099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waldron NN, Kaufman DS, Oh S, Inde Z, Hexum MK, Ohlfest JR, Vallera DA. Targeting tumor-initiating cancer cells with dCD133KDEL shows impressive tumor reductions in a xenotransplant model of human head and neck cancer. Mol Cancer Ther. 2011;10:1829–1838. doi: 10.1158/1535-7163.MCT-11-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohlfest JR, Zellmer D, Panyam J, Swaminathan SK, Oh S, Waldron NN, Toma S, Vallera DA. Immunotoxin targeting CD133+ breast carcinoma cells. Drug Deliv Transl Res. 2012 doi: 10.1007/s13346-012-0066-2. doi 10.1007/s13346-012-0066-2. [DOI] [PubMed] [Google Scholar]
- 16.Skubitz APN, Taras EP, Boylan KLM, Waldron NN, Oh S, Panoskaltsis-Mortari A, Vallera DA. Targeting CD133 in an in vivo ovarian cancer model reduces ovarian cancer progression. Gynecologic Oncology. 2013 doi: 10.1016/j.ygyno.2013.05.027. Submitted for publication 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stish BJ, Oh S, Chen H, Dudek AZ, Kratzke RA, Vallera DA. Design and modification of EGF4KDEL 7mut, a novel bispecific ligand-directed toxin, with decreased immunogenicity and potent anti-mesothelioma activity. Br J Cancer. 2009;101:1114–23. doi: 10.1038/sj.bjc.6605297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsai AK, Oh S, Chen H, Shu Y, Ohlfest JR, Vallera DA. A novel bispecific ligand-directed toxin designed to simultaneously target EGFR on human glioblastoma cells and uPAR on tumor neovasculature. J Neurooncol. 2011;103:255–66. doi: 10.1007/s11060-010-0392-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vallera DA, Oh S, Chen H, Shu Y, Frankel AE. Bioengineering a unique deimmunized bispecific targeted toxin that simultaneously recognizes human CD22 and CD19 receptors in a mouse model of B-cell metastases. Mol Cancer Ther. 2010;9:1872–83. doi: 10.1158/1535-7163.MCT-10-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stish BJ, Chen H, Shu Y, Panoskaltsis-Mortari A, Vallera DA. Increasing anticarcinoma activity of an anti-erbB2 recombinant immunotoxin by the addition of an anti-EpCAM sFv. Clin Cancer Res. 2007;13:3058–3067. doi: 10.1158/1078-0432.CCR-06-2454. [DOI] [PubMed] [Google Scholar]
- 21.MacDonald GC, Rasamoelisolo M, Entwistle J, Cizeau J, Bosc D, Cuthbert W, Kowalski M, Spearman M, Glover N. A phase I clinical study of VB4-845: Weekly intratumoral administration of an anti-EpCAM recombinant fusion protein in patients with squamous cell carcinoma of the head and neck. Drug Des Devel Ther. 2009;2:105–114. doi: 10.2147/dddt.s3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kowalski M, Entwistle J, Cizeau J, Niforos D, Loewen S, Chapman W, MacDonald GC. A Phase I study of an intravesically administered immunotoxin targeting EpCAM for the treatment of nonmuscle-invasive bladder cancer in BCG-refractory and BCG-intolerant patients. Drug Des Devel Ther. 2010;4:313–320. doi: 10.2147/DDDT.S14071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kowalski M, Guindon J, Brazas L, Moore C, Entwistle J, Cizeau J, Jewett MA, MacDonald GC. A Phase II Study of Oportuzumab Monatox: An Immunotoxin Therapy for Patients with Noninvasive Urothelial Carcinoma In Situ Previously Treated with Bacillus Calmette-Guérin. J Urol. 2012;188:1712–1718. doi: 10.1016/j.juro.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 24.Fitzgerald D, Pastan I. Targeted toxin therapy for the treatment of cancer. J Natl Cancer Inst. 1989;81:1455–63. doi: 10.1093/jnci/81.19.1455. [DOI] [PubMed] [Google Scholar]
- 25.Kreitman RJ, Pastan I. Importance of the glutamate residue of KDEL in increasing the cytotoxicity of Pseudomonas exotoxin derivatives and for increased binding to the KDEL receptor. Biochem J. 1995;307:697, 29–37. doi: 10.1042/bj3070029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vallera DA, Chen H, Sicheneder AR, Panoskaltsis-Mortari A, Taras EP. Genetic alteration of a bispecific ligand directed toxin targeting human CD19 and CD22 receptors resulting in improved efficacy against systemic. Leuk Res. 2009;33:1233–42. doi: 10.1016/j.leukres.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Worsham MJ, Chen KM, Meduri V, Nygren AO, Errami A, Schouten JP, Benninger MS. Epigenetic events of disease progression in head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg. 2006;132:668–77. doi: 10.1001/archotol.132.6.668. [DOI] [PubMed] [Google Scholar]
- 28.Abu-Ali S, Fotovati A, Shirasuna K. Tyrosine-kinase inhibition results in EGFR clustering at focal adhesions and consequent exocytosis in uPAR down-regulated cells of head and neck cancers. Mol Cancer. 2008;7:47. doi: 10.1186/1476-4598-7-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eyler CE, Rich JN. Survival of the fittest: cancer stem cells in therapeutic resistance and angiogenesis. J Clin Onc. 2008;26:2839–45. doi: 10.1200/JCO.2007.15.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fabrizi E, di Martino S, Pelacchi F, Ricci-Vitiani L. Therapeutic implications of colon cancer stem cells. World J Gastroenterol. 2010;16:3871–7. doi: 10.3748/wjg.v16.i31.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dylla SJ, Beviglia L, Park IK, Chartier C, Raval J, Ngan L, Pickell K, Aguilar J, Lazetic S, Smith-Berdan S, Clarke MF, Hoey T, Lewicki J, Gurney AL. Colorectal cancer stem cells are enriched in xenogeneic tumors following chemotherapy. PLoS One. 2008;3:e2428. doi: 10.1371/journal.pone.0002428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dallas NA, Xia L, Fan F, Gray MJ, Gaur P, van Buren G, 2nd, Samuel S, Kim MP, Lim SJ, Ellis LM. Chemoresistant colorectal cancer cells, the cancer stem cell phenotype, and increased sensitivity to insulin-like growth factor-I receptor inhibition. Cancer Res. 2009;69:1951–7. doi: 10.1158/0008-5472.CAN-08-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alpaugh ML, Tomlinson JS, Shao ZM, Barsky SH. A novel human xenograft model of inflammatory breast cancer. Cancer Res. 1999;59:5079–5084. [PubMed] [Google Scholar]
- 34.Hirschhaeuser F, Menne H, Dittfeld C, West J, Mueller-Klieser W, Kunz-Schughart LA. Multicellular tumor spheroids: An underestimated tool is catching up again. Journal of Biotechnology. 2010;148:3–15. doi: 10.1016/j.jbiotec.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 35.Imrich S, Hachmeister M, Gires O. EpCAM and its potential role in tumor-initiating cells. Cell Adh Migr. 2012;6:30–38. doi: 10.4161/cam.18953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yamashita T, Ji J, Budhu A, Forgues M, Yang W, Wang HY, Jia H, Ye Q, Qin L, Wauthier E, Reid LM, Minato H, Honda M, Kaneko S, Tang ZY, Wang XW. EpCAM-positive hepatocellular carcinoma cells are tumor-initiating cells with stem/progenitor cell features. Gastroenterology. 2009;136:1012–1024. doi: 10.1053/j.gastro.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rutella S, Bonanno G, Marone M, De Ritis D, Mariotti A, Voso MT, Scambia G, Mancuso S, Leone G, Pierelli L. Identification of a novel subpopulation of human cord blood CD34- CD133- CD7- CD45þ lineage-cells capable of lymphoid/NK cell differentiation after in vitro exposure to IL-15. J Immunol. 2003;171:2977–88. doi: 10.4049/jimmunol.171.6.2977. [DOI] [PubMed] [Google Scholar]
- 38.Floor S, van Staveren W C, Larsimont D, Dumont J E, Maenhaut C. Cancer cells in epithelial-to-mesenchymal transition and tumor-propagating-cancer stem cells: distinct, overlapping or same populations. Oncogene. 2011;30:4609–4621. doi: 10.1038/onc.2011.184. [DOI] [PubMed] [Google Scholar]
- 39.Suuronen EJ, Wong S, Kapila V, Waghray G, Whitman SC, Mesana TG, Ruel M. Generation of CD133+ cells from CD133- peripheral blood mononuclear cells and their properties. Cardiovasc Res. 2006;70:126–135. doi: 10.1016/j.cardiores.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 40.Onda M, Beers R, Xiang L, Nagata S, Wang QC, Pastan I. An immunotoxin with greatly reduced immunogenicity by identification and removal of B-cell epitopes. Proc Natl Acad Sci U S A. 2008;105:701, 11311–6. doi: 10.1073/pnas.0804851105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hassan R, Broaddus VC, Wilson S, Liewehr DJ, Zhang J. Anti-mesothelin immunotoxin SS1P in combination with Gemcitabine results in increased activity against mesothelin-expressing tumor xenografts. Clin Cancer Res. 2007;13:7166–71. doi: 10.1158/1078-0432.CCR-07-1592. [DOI] [PubMed] [Google Scholar]
- 42.Pearson JW, Sivam G, Manger R, Wiltrout RH, Morgan AC, Jr, Longo DL. Enhanced therapeutic efficacy of an immunotoxin in combination with chemotherapy against an intraperitoneal human tumor xenograft in athymic mice. Cancer Res. 1989;49:4990–5. [PubMed] [Google Scholar]
- 43.Fujiwara S, Wada H, Miyata H, Kawada J, Kawabata R, Nishikawa H, Gnjatic S, Sedrak C, Sato E, Nakamura Y, Sakakibara M, Kanto T, Shimosegawa E, Hatazawa J, Takahashi T, Kurokawa Y, Yamasaki M, Nakajima K, Takiguchi S, Nakayama E, Mori M, Doki Y. Clinical trial of the intratumoral administration of labeled DC combined with systemic chemotherapy for esophageal cancer. J Immunother. Jul. 2012;35(6):513–21. doi: 10.1097/CJI.0b013e3182619cb4. [DOI] [PubMed] [Google Scholar]