Abstract
Sedation allows patients to tolerate unpleasant endoscopic procedures by relieving anxiety, discomfort, or pain. It also reduces a patient's risk of physical injury during endoscopic procedures, while providing the endoscopist with an adequate setting for a detailed examination. Sedation is therefore considered by many endoscopists to be an essential component of gastrointestinal endoscopy. Endoscopic sedation by nonanesthesiologists is a worldwide practice and has been proven effective and safe. Moderate sedation/analgesia is generally accepted as an appropriate target for sedation by nonanesthesiologists. This focused review describes the general principles of endoscopic sedation, the detailed pharmacology of sedatives and analgesics (focused on midazolam, propofol, meperidine, and fentanyl), and the multiple regimens available for use in actual practice.
Keywords: Sedation, Endoscopy, Analgesia, Endoscopic sedation
INTRODUCTION
Sedation, which can be defined as a drug-induced depression in the level of consciousness, is regarded by many endoscopists as an essential component of gastrointestinal endoscopy.1 Endoscopic procedures such as esophagogastroduod-enoscopy (EGD) and colonoscopy can be performed without sedation in some patients with certain characteristics, but these procedures are better tolerated when adequate sedation is administered. This is especially the case for more complex endoscopic procedures such as endoscopic retrograde cholangiopancreatography.2 Sedation allows patients to tolerate unpleasant procedures by relieving anxiety, discomfort, or pain, and it also reduces a patient's risk of physical injury during endoscopic procedures while providing the endoscopist with an adequate setting for a detailed examination.1
Expertise in the pharmacology, physiology, and clinical management of patients receiving sedation and analgesia is therefore very relevant to endoscopists.3 Endoscopic sedation by nonanesthesiologists is a worldwide practice that has been confirmed as effective and safe, especially when targeted to moderate sedation/analgesia.4,5,6,7,8 Propofol, as well as traditional agents (benzodiazepines and/or narcotics), can be safely titrated by endoscopists to provide adequate sedation.7 This focused review describes the basics of sedation, the pharmacology of sedatives and analgesics, and the multiple regimens available for use in actual practice.
SEDATION AND ANALGESIA FOR GASTROINTESTINAL ENDOSCOPY
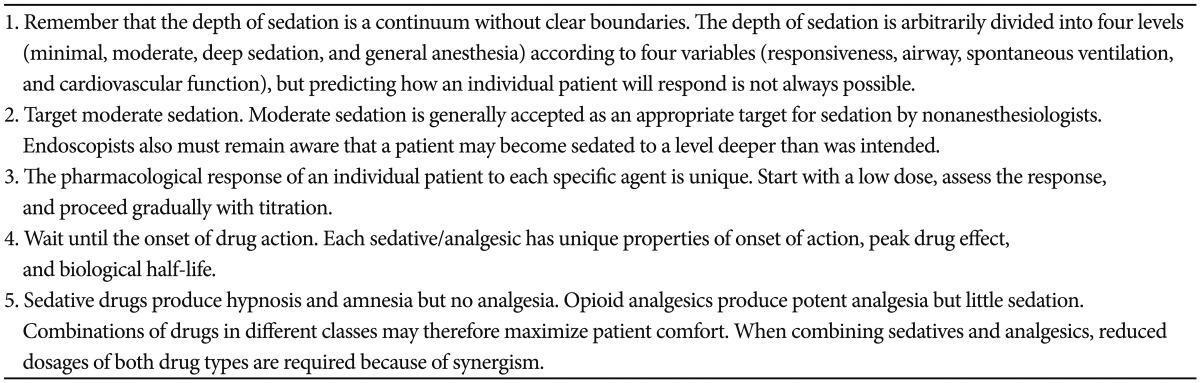
The aim of endoscopic sedation is to reduce patient discomfort, including anxiety and pain, while preserving a minimum rate of drug-related adverse events.1 Sedative drugs produce hypnosis and amnesia of discomfort but no analgesia, while opioid narcotics produce potent analgesia but little sedation.9 If analgesics are properly used, the amount of sedative required for satisfactory endoscopic sedation can be substantially reduced. Endoscopists should consider both patient and procedural factors for adequate and safe sedation. Patient factors include age, body mass, medical history, concurrent medications, preprocedural anxiety, previous responses to sedation, and pain tolerance.1,6,10 Procedural factors include the level of procedure-related discomfort, the need for the patient to lie relatively motionless, and the duration of examination.1,6,10 Optimal sedation by endoscopists is indicated in the sedation training curriculum for gastrointestinal endoscopy published by the gastroenterology and endoscopy societies, which includes concepts of sedation, preprocedural assessment, sedation pharmacology, patient monitoring, training in airway/rescue techniques, management of complications, and so forth.6,11 Table 1 summarizes the general principles of endoscopic sedation for nonanesthesiologists.3,6,8,9
Table 1.
Clinical Pearls for Adequate and Safe Endoscopic Sedation
PHARMACOLOGY OF SEDATIVES AND ANALGESICS
Endoscopists must understand the pharmacology, pharmacokinetics (time of onset, peak response, and duration of effect), pharmacodynamics, adverse effects, and drug-drug interactions of any sedative and analgesic that they use (Table 2). The most common agents used for endoscopic sedation are benzodiazepines (more specifically midazolam), opioids, and propofol.
Table 2.
Pharmacological Properties of Sedatives/Analgesics for Gastrointestinal Endoscopy
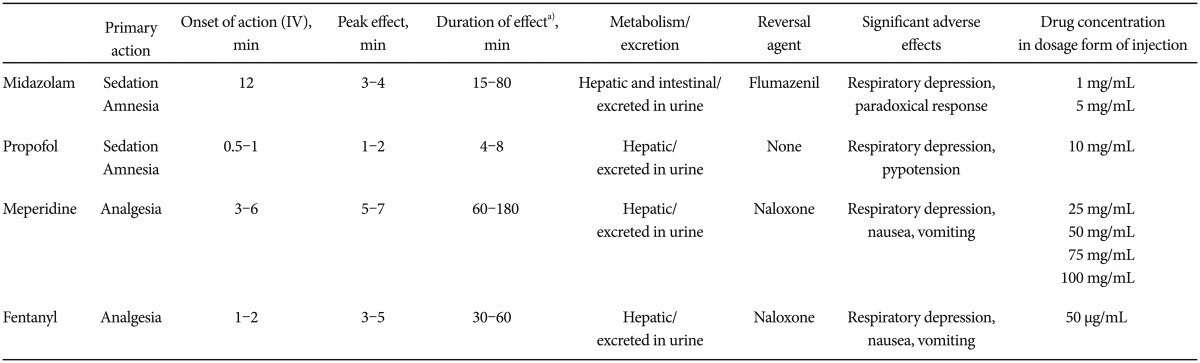
IV, intravenous.
a)The duration of drug effect may depend on the duration of administration.
Midazolam
Benzodiazepines have multiple pharmacologic effects that help facilitate sedation for endoscopy through interactions with the γ-aminobutyric acid (GABA) receptor. When benzodiazepines bind to the type A GABA (GABAA) receptor within the cerebrum and cerebellar cortex, they increase the binding affinity for GABA (inhibitory neurotransmitter) and promote its inhibitory action on the central nervous system.1,12 As a result, benzodiazepines have anxiolytic, euphoriant, sedative-hypnotic, amnestic (anterograde), anticonvulsant, and muscle-relaxing effects. The commonly used benzodiazepines for endoscopic sedation have been midazolam and diazepam, but midazolam is the benzodiazepine of choice due to the shorter duration of its effect and its better pharmacokinetic profile compared to diazepam.4,8,12 In addition, midazolam is 1.5 to 3.5 times more potent than diazepam.1
Midazolam is a water soluble benzodiazepine that is available parenterally and shows a pH-dependent solubility. In an acidic solution (pH <3-4), midazolam is water-soluble. After intravenous administration, midazolam undergoes an intramolecular reconfiguration at physiological pH (7.4) to yield the classic lipophilic benzodiazepine structure.1,12 The high lipophilicity of midazolam results in its rapid distribution across the blood-brain barrier to its site of action, i.e., the central nervous system. Midazolam is metabolized in the liver through oxidative and conjugative metabolism, and its metabolites are excreted by the kidney.
The onset of effect for midazolam is 1 to 2.5 minutes, the peak effect is at 3 to 4 minutes, and the duration of effect is 15 to 80 minutes. The duration of the effect of midazolam depends on the duration of its administration.4 Midazolam clearance is reduced in the elderly, the obese, and those with hepatic or renal impairment.1 The major adverse effects are respiratory depression, apnea, and hypotension. The respiratory depressant effect of benzodiazepines is dose dependent and results from depression of the central ventilator response to hypoxia and hypercapnia. Paradoxical reactions, including hyperactive or aggressive behavior, have been reported with benzodiazepines.4 The administration of flumazenil (a benzodiazepine antagonist) can reverse sedation, psychomotor impairment, memory loss, and respiratory depression.6 The onset of action for flumazenil is 1 to 2 minutes and the duration of its effect is 60 minutes.
Propofol
Propofol (2,6-diisopropofol) is a sedative-hypnotic drug with an amnestic effect, but a minimal analgesic effect. Its hypnotic effect results from potentiating GABA through the GABAA receptor in a manner similar to that of benzodiazepines.12 The depth of sedation increases in a dose-dependent manner. Serum levels of propofol should be greater than 1 µg/mL to produce sleep.12 The current formulation of propofol contains 1% propofol (10 mg/mL), 10% soybean oil, 2.25% glycerol, and 1.2% purified egg phosphatide. Propofol has the benefits of a very rapid onset of action and a short recovery time.
Propofol is highly lipophilic and rapidly crosses the blood-brain barrier. It is metabolized rapidly in the liver via hydroxylation and conjugation with glucuronide and sulfate, and its metabolites are excreted by the kidney. The onset of effect for propofol is 0.5 to 1 minutes and the duration of effect is 4 to 8 minutes. The pharmacokinetic parameters of propofol vary with patient factors such as weight, sex, age, and concomitant disease. Because elderly patients have a decreased volume of distribution and total body clearance for propofol, they are more sensitive to propofol.12 Chronic kidney disease or liver cirrhosis does not significantly alter propofol pharmacokinetics.1,12
Major adverse effects are respiratory depression, hypotension, and pain on injection.1 Hypotension results from the cardiovascular effects of propofol including decreased cardiac output and systemic vascular resistance. With overdosing, respiratory depression generally precedes clinically significant hypotension.8 Pain on injection is reported by up to 30% of patients, especially when receiving an intravenous bolus of propofol. That there is no existing pharmacologic antagonist is a disadvantage of propofol, although hypotension and respiratory depression typically responds rapidly to a dose reduction or interruption of drug infusion.
Opioids
The opioid class of drugs has potent analgesic with some sedative effects. Opioid analgesics mainly inhibit neurotransmission of pain by binding to specific opioid receptors that are present in the central nervous system and peripheral tissues. Properties of opioid analgesics include rapid onset, ease of titration, and no ceiling effect. Among the opioid analgesics (morphine, meperidine, fentanyl, remifentanil, and so forth), meperidine and fentanyl are the most commonly used for endoscopic sedation. The equianalgesic dose refers to the relative potency of two opioids to produce the same analgesic effect.12 The standard comparison dose is 10 mg parenteral morphine, which is equivalent to 75 mg of meperidine and 0.1 mg of fentanyl.
Meperidine is a full opioid agonist with effects similar to those of morphine. The onset of action for meperidine is 3 to 6 minutes when intravenously administered and 10 to 15 minutes when administered intramuscularly.1,12 The duration of effect is 60 to 180 minutes. Meperidine is metabolized in the liver and excreted in the urine. All opioids increase biliary tract pressure, but meperidine has a lesser effect.12
Fentanyl, a synthetic full opioid agonist, is highly lipid-soluble and 80 to 100 times as potent as morphine. The onset of action for fentanyl is 1 to 2 minutes and its duration of effect is 30 to 60 minutes. Fentanyl is metabolized in the liver and excreted in the urine.
Common adverse effects of opioids include constipation, respiratory depression, miosis, nausea and vomiting, urinary retention, and myoclonus.12 Respiratory depression occurs in a dose-dependent manner, and the concomitant use of a benzodiazepine with an opioid has a synergistic effect on the risk of respiratory depression. Opioid analgesics usually produce only mild hemodynamic depression.12 Among the opioids, fentanyl has relatively little effect on the cardiovascular system.1 Nausea and vomiting resulting from stimulation of the medullary chemoreceptor trigger zone occurs in a dose-independent manner.1 Naxloxone is a pure antagonist for opioid receptors and is used to reverse the effects of the opioid narcotics. The onset of action for naloxone is 1 to 2 minutes and the duration of its effect is 30 to 45 minutes.
SEDATION REGIMENS FOR ENDOSCOPISTS IN ACTUAL PRACTICE
Implementation of an evidence-based sedation regimen may improve the quality of sedation practice and reduce the incidence of sedation-related adverse events.1 However, a fine line may exist between over- and under-sedation in actual practice.12 Experience combined with knowledge is required for safe and effective administration of sedatives/analgesics for the purpose of induction and maintenance of moderate sedation. Table 3 describes the detailed sedation regimens for endoscopists. When deep sedation or general anesthesia is required for extended periods in complex endoscopic procedures, anesthesiologist-assisted sedation may play an important role.13
Table 3.
Practical Sedation Regimens for Gastrointestinal Endoscopy
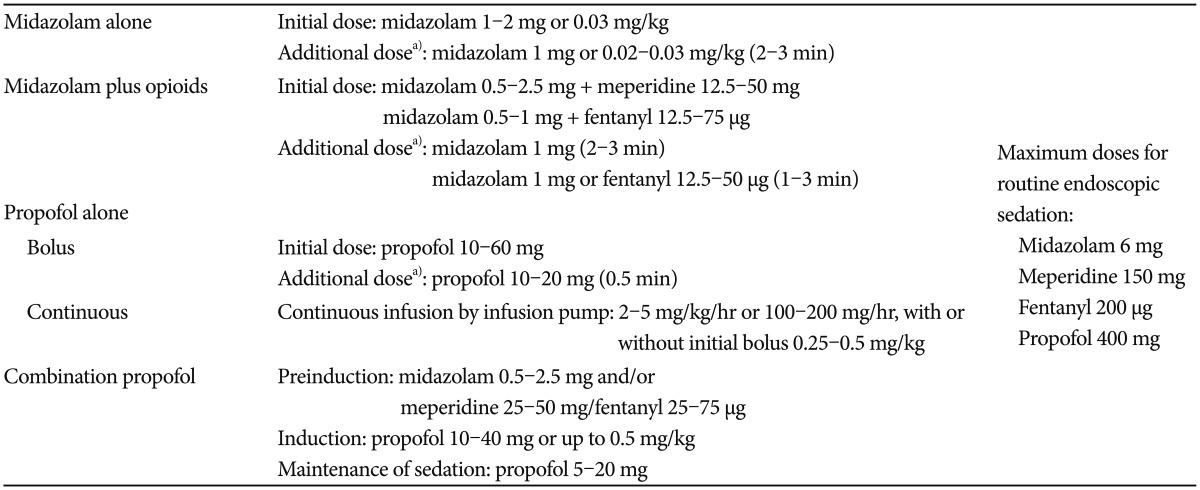
a)Minimal interval of administration.
Midazolam alone
The choice of traditional sedatives/analgesics generally consists of a benzodiazepine used either alone or in combination with an opiate.10 Midazolam is the most widely used benzodiazepine drug because it has a more rapid onset of action and a shorter duration than the other benzodiazepines. The initial intravenous dose for endoscopic sedation in healthy adults younger than 60 years of age is 1 to 2 mg (or no more than 0.03 mg/kg body weight) injected over 1 to 2 minutes.1,6 Additional doses of 1 mg (or 0.02 to 0.03 mg/kg) may be administered at 2-minute intervals until adequate sedation is achieved. The usual total dose is 2.5 to 5 mg.14 A maximal dosage of midazolam for routine endoscopic procedure is 6 to 7.5 mg.6,15 A reduction in the midazolam dosage (20% or more) is required for patients older than 60 years of age and for those with American Society of Anesthesiologists physical status III or greater.
Midazolam plus opioids
When midazolam is used in combination with an opioid analgesic, a reduction in the dosage of midazolam/opioids may be indicated due to a synergistic interaction.1 The initial doses are 0.5 to 1 mg midazolam plus 12.5 to 50 mg meperidine or 12.5 to 75 µg fentanyl.16,17,18,19 Additional medication is titrated at 1 to 3 minutes intervals to achieve or maintain the desired level of sedation. The time of titration can be decreased by using an initial dose of 2.5 mg midazolam and 25 to 50 mg meperidine with an additional dose of midazolam.15
Propofol alone
The clinical advantages of propofol include rapid onset and off-set of sedation with quick recovery times. A meta-analysis showed that propofol allows a more rapid initiation of sedation (2 vs. 6 to 8.5 minutes) and a shorter recovery time (15 vs. 50 to 55 minutes) when compared with midazolam-based regimens.20 Many patients who receive propofol alone may require deep sedation because propofol provides no analgesic effect.1
The published protocols for propofol recommend an initial bolus of propofol ranging from 10 to 60 mg, followed by additional boluses of 10 to 20 mg administered with a minimum of 20 to 30 seconds between doses.1 The short duration of action of propofol may require frequent and somewhat technically demanding propofol administration to maintain sedation levels.
Continuous infusion of propofol by pumps may theoretically be associated with a reduced need for nurse intervention and a more stable maintenance of a consistent level of sedation. The published protocols for continuous propofol infusion states are 2 to 5 mg/kg/hr (or 100 to 200 mg/hr), sometimes with an initial 0.25 to 0.5 mg/kg bolus.9,21,22,23 Although continuous infusion of propofol by a pump is widely used in anesthesia practice and the pumps are easily programmed, most nonanesthesiologists prefer the flexibility of the bolus approach.9,21
Balanced propofol sedation (combination propofol)
Balanced propofol sedation is analogous to balanced anesthesia, which is a well-established pharmacologic concept in the practice of general anesthesia. Balanced anesthesia involves the administration of a mixture of small amounts of several neuronal depressants to maximize the therapeutic actions while minimizing the likelihood of a dose-related adverse reaction from any of the individual drugs.1 In endoscopic practice, balanced propofol sedation describes the use of an opioid and/or benzodiazepine, where each is given as a single dose, followed by small incremental doses of propofol administered to achieve a target level of sedation (preferably moderate sedation).5,6 Balanced propofol sedation can provide the benefits of propofol-mediated sedation while reducing the risk of rapid, irreversible oversedation.1 However, recovery time from balanced propofol sedation might be longer than recovery from propofol only.
The published protocols for balanced propofol sedation dictate a pre-induction dose of either an opioid (fentanyl, 25 to 75 µg; meperidine, 25 to 50 mg), midazolam (0.5 to 2.5 mg), or both.1,24,25 An initial bolus of propofol (10 to 40 mg, or up to 0.5 mg/kg) is then administered, followed by additional boluses of 5 to 20 mg titrated to achieve the target level of sedation.6,24,25 Maintenance of sedation is achieved with repeated doses of 5 to 20 mg propofol. The average cumulative doses of propofol in balanced propofol sedation are 65 to 100 mg for colonoscopy and 35 to 70 mg during EGD.1
CONCLUSIONS
Various sedation regimens using a single agent or mixture of sedatives and analgesics are now used for gastrointestinal endoscopy. Because endoscopic sedation by nonanesthesiologists is a worldwide practice, it is important for endoscopists to be fully aware of the general principles of sedation and the pharmacology of any sedative and analgesic that they use. Experience combined with knowledge will promote optimal administration of sedatives/analgesics for the purpose of induction and maintenance of moderate sedation. Sedation regimens for adequate and safe sedation continue to evolve.
Footnotes
The author has no financial conflicts of interest.
References
- 1.Cohen LB, Delegge MH, Aisenberg J, et al. AGA Institute review of endoscopic sedation. Gastroenterology. 2007;133:675–701. doi: 10.1053/j.gastro.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Dumonceau JM, Riphaus A, Aparicio JR, et al. European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and the European Society of Anaesthesiology Guideline: non-anesthesiologist administration of propofol for GI endoscopy. Endoscopy. 2010;42:960–974. doi: 10.1055/s-0030-1255728. [DOI] [PubMed] [Google Scholar]
- 3.American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004–1017. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 4.Triantafillidis JK, Merikas E, Nikolakis D, Papalois AE. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013;19:463–481. doi: 10.3748/wjg.v19.i4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vargo JJ, Cohen LB, Rex DK, Kwo PY. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc. 2009;70:1053–1059. doi: 10.1016/j.gie.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 6.American Association for Study of Liver Diseases; American College of Gastroenterology; American Gastroenterological Association Institute et al. Multisociety sedation curriculum for gastrointestinal endoscopy. Gastrointest Endosc. 2012;76:e1–e25. doi: 10.1016/j.gie.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Rex DK, Deenadayalu VP, Eid E, et al. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009;137:1229–1237. doi: 10.1053/j.gastro.2009.06.042. [DOI] [PubMed] [Google Scholar]
- 8.Rex DK. Review article: moderate sedation for endoscopy: sedation regimens for non-anaesthesiologists. Aliment Pharmacol Ther. 2006;24:163–171. doi: 10.1111/j.1365-2036.2006.02986.x. [DOI] [PubMed] [Google Scholar]
- 9.Karan SB, Bailey PL. Update and review of moderate and deep sedation. Gastrointest Endosc Clin N Am. 2004;14:289–312. doi: 10.1016/j.giec.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. Lichtenstein DR, Jagannath S, et al. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008;68:815–826. doi: 10.1016/j.gie.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 11.Dumonceau JM, Riphaus A, Beilenhoff U, et al. European curriculum for sedation training in gastrointestinal endoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA) Endoscopy. 2013;45:496–504. doi: 10.1055/s-0033-1344142. [DOI] [PubMed] [Google Scholar]
- 12.Horn E, Nesbit SA. Pharmacology and pharmacokinetics of sedatives and analgesics. Gastrointest Endosc Clin N Am. 2004;14:247–268. doi: 10.1016/j.giec.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Vargo JJ. Anesthesia-mediated sedation for advanced endoscopic procedures and cardiopulmonary complications: of mountains and molehills. Clin Gastroenterol Hepatol. 2010;8:103–104. doi: 10.1016/j.cgh.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Waring JP, Baron TH, Hirota WK, et al. Guidelines for conscious sedation and monitoring during gastrointestinal endoscopy. Gastrointest Endosc. 2003;58:317–322. doi: 10.1067/s0016-5107(03)00001-4. [DOI] [PubMed] [Google Scholar]
- 15.Riphaus A, Gstettenbauer T, Frenz MB, Wehrmann T. Quality of psychomotor recovery after propofol sedation for routine endoscopy: a randomized and controlled study. Endoscopy. 2006;38:677–683. doi: 10.1055/s-2006-925244. [DOI] [PubMed] [Google Scholar]
- 16.Laluna L, Allen ML, Dimarino AJ., Jr The comparison of midazolam and topical lidocaine spray versus the combination of midazolam, meperidine, and topical lidocaine spray to sedate patients for upper endoscopy. Gastrointest Endosc. 2001;53:289–293. doi: 10.1016/s0016-5107(01)70400-2. [DOI] [PubMed] [Google Scholar]
- 17.Zakko SF, Seifert HA, Gross JB. A comparison of midazolam and diazepam for conscious sedation during colonoscopy in a prospective double-blind study. Gastrointest Endosc. 1999;49:684–689. doi: 10.1016/s0016-5107(99)70282-8. [DOI] [PubMed] [Google Scholar]
- 18.Sipe BW, Rex DK, Latinovich D, et al. Propofol versus midazolam/meperidine for outpatient colonoscopy: administration by nurses supervised by endoscopists. Gastrointest Endosc. 2002;55:815–825. doi: 10.1067/mge.2002.124636. [DOI] [PubMed] [Google Scholar]
- 19.Ulmer BJ, Hansen JJ, Overley CA, et al. Propofol versus midazolam/fentanyl for outpatient colonoscopy: administration by nurses supervised by endoscopists. Clin Gastroenterol Hepatol. 2003;1:425–432. doi: 10.1016/s1542-3565(03)00226-x. [DOI] [PubMed] [Google Scholar]
- 20.McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008;67:910–923. doi: 10.1016/j.gie.2007.12.046. [DOI] [PubMed] [Google Scholar]
- 21.Byrne MF, Chiba N, Singh H, Sadowski DC Clinical Affairs Committee of the Canadian Association of Gastroenterology. Propofol use for sedation during endoscopy in adults: a Canadian Association of Gastroenterology position statement. Can J Gastroenterol. 2008;22:457–459. doi: 10.1155/2008/268320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chun SY, Kim KO, Park DS, et al. Safety and efficacy of deep sedation with propofol alone or combined with midazolam administrated by nonanesthesiologist for gastric endoscopic submucosal dissection. Gut Liver. 2012;6:464–470. doi: 10.5009/gnl.2012.6.4.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riphaus A, Geist C, Schrader K, Martchenko K, Wehrmann T. Intermittent manually controlled versus continuous infusion of propofol for deep sedation during interventional endoscopy: a prospective randomized trial. Scand J Gastroenterol. 2012;47:1078–1085. doi: 10.3109/00365521.2012.685758. [DOI] [PubMed] [Google Scholar]
- 24.Lee CK, Lee SH, Chung IK, et al. Balanced propofol sedation for therapeutic GI endoscopic procedures: a prospective, randomized study. Gastrointest Endosc. 2011;73:206–214. doi: 10.1016/j.gie.2010.09.035. [DOI] [PubMed] [Google Scholar]
- 25.Lee TH, Lee CK, Park SH, et al. Balanced propofol sedation versus propofol monosedation in therapeutic pancreaticobiliary endoscopic procedures. Dig Dis Sci. 2012;57:2113–2121. doi: 10.1007/s10620-012-2234-0. [DOI] [PubMed] [Google Scholar]


