Abstract
Most ingested foreign bodies often pass through the gastrointestinal tract uneventfully; however, complications such as perforation do occur. Most cases of perforation are caused by thin, pointed objects such as needles, toothpicks, or fish and chicken bones. Herein, we report an unusual case of duodenal perforation caused by a lollipop stick with blunt ends. A 23-year-old woman was admitted to the emergency department complaining of epigastric and right upper quadrant pain for the last 2 days. Abdominal computed tomography scans confirmed the presence of a foreign body in the duodenum, with signs of duodenal perforation and inflammation. The patient was not aware of ingesting the foreign body. Endoscopy revealed the presence of a lollipop stick in the duodenum, which was removed with forceps. The duodenal perforation was successfully managed by using hemoclips and a detachable snare.
Keywords: Foreign bodies, Perforation, Endoscopy
INTRODUCTION
Ingestion of a foreign body is a relatively common clinical problem. Most of these ingested foreign bodies pass through the gastrointestinal tract uneventfully; however, a small proportion (<1%) cause complications such as perforation.1 Diagnosis of bowel perforation is often challenging because patients are frequently unaware of ingesting a foreign body; clinical manifestations vary from nonspecific findings of abdominal pain, nausea, vomiting, or fever to even no symptoms at all,1,2 and abdominal radiographs or computed tomography (CT) scans have limited reliability.3,4 While these perforations have been treated surgically in the past, the development of endoscopic procedures has made less invasive management possible. We herein report an unusual case of duodenal perforation caused by a lollipop stick with blunt ends, managed successfully by using endoscopic hemoclips and a detachable snare.
CASE REPORT
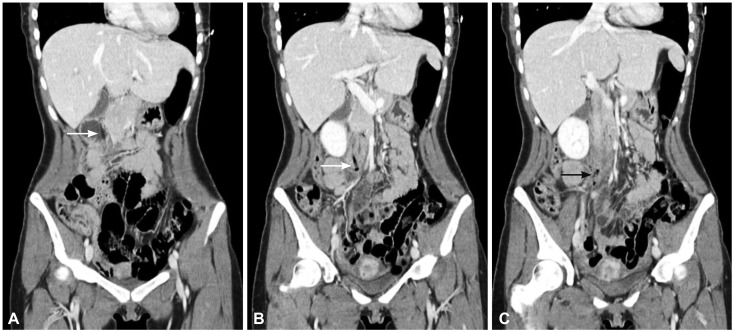
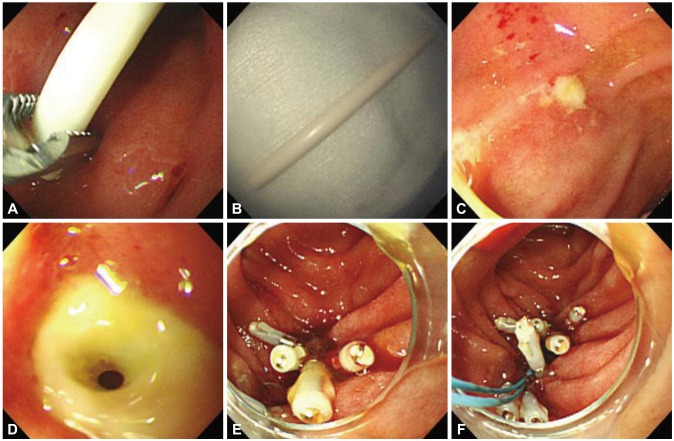
A 23-year-old woman presented to the emergency department of our hospital with epigastric and right upper quadrant pain that started 2 days ago. She had no significant medical history and not taking any medicine. Physical examination revealed epigastric and right upper quadrant tenderness, with rebound tenderness in the right upper quadrant. Her vital signs were as follows: blood pressure, 130/90 mm Hg; heart rate, 78 beats per minute; body temperature, 36.6℃; and respiratory rate, 18 breaths per minute. Plain radiographs of the abdomen did not reveal any abnormal findings. Laboratory tests revealed a white blood cell count of 12,800/mm3 (neutrophil, 81.7%); hemoglobin level of 11.4 g/dL; platelet count of 175,000/mm3; and C-reactive protein level of 10.7 mg/dL (reference limit, 0.1 to 1 mg/dL). Liver function tests, renal function tests, and electrolytes were all within the reference limits. An abdominal CT scan revealed a 7-cm-long, stick-like foreign body situated vertically from the duodenal bulb to the third portion of the duodenum. Mottled air density and blurred periduodenal fat planes with streaky soft tissue stranding were also observed around the third portion of the duodenum; however, no pneumoperitoneum was observed (Fig. 1). The patient was unaware of ingesting the foreign body. Emergency esophagogastroduodenoscopy was performed to identify the foreign body. A surgical team was contacted to ascertain whether emergency surgery could be carried out immediately if bowel perforation is detected during esophagogastroduodenoscopy or if the abdominal pain becomes worse. A lollipop stick was found in the duodenum, with a shallow ulcer in the proximal third portion of the duodenum, and it was endoscopically removed with rat-tooth forceps. Two small ulcers, one proximal with exudates and the other distal with air bubbles, were also seen in the third portion of the duodenum. Successful closure was performed by placing 3 hemoclips (HX-610-135; Olympus, Tokyo, Japan) to the proximal ulcer. Five hemoclips were placed circumferentially around the perimeter of the perforation edge of the distal ulcer. A detachable snare (SD 6L-1; Olympus) was placed around the perimeter base of the clips. The snare was then tightened, successfully bringing all the edges of the wound together (Fig. 2). The patient recalled having slept drunk with a lollipop in her mouth 2 weeks previously. The next day, abdominal CT was repeated to observe the hemoclips in the duodenum and the periduodenal inflammation; however, no pneumoperitoneum was yet observed. An intravenous proton-pump inhibitor and antibiotic treatments, including metronidazole and a third-generation cephalosporin, were used, and she was placed on a nothing-per-oral status with nasogastric tube drainage for 5 days. From the sixth day of hospitalization, feeding was gradually advanced from water to a liquid diet, and then to a soft diet. She refused to undergo follow-up endoscopy and was discharged on the ninth day of hospitalization. She remained asymptomatic at the subsequent follow-up 2 weeks after discharge.
Fig. 1.
(A-C) Computed tomography findings. A stick-like foreign body was observed in the duodenum (white arrow). Mottled air density was observed around the third portion of the duodenum (black arrow).
Fig. 2.
Endoscopic findings. (A, B) A lollipop stick was removed by using rat-tooth forceps. (C) A proximal small ulcer with exudates was observed in the third portion of the duodenum. (D) A distal ulcer with air bubble was observed in the third portion of the duodenum. (E) Five hemoclips were applied to the margin of the duodenal perforation. (F) A detachable snare was used to approximate the ends of the perforation.
DISCUSSION
Treatment of foreign body ingestion is a relatively common clinical practice. The patient's medical history is the primary basis for the diagnosis of foreign body ingestion. However, as patients are often unaware of ingesting a foreign body and the clinical manifestations vary widely, diagnosing a case of foreign body ingestion is challenging.1 Plain radiographs or abdominal CT scans may help in detecting foreign bodies or associated complications.4 In the present case, the patient was not aware of ingesting the foreign body. Abdominal CT was performed to evaluate the abdominal pain, which revealed the object in the duodenum but failed to identify its nature. Endoscopy confirmed the presence of a lollipop stick, and it was only after the foreign body was retrieved did she recall possibly having swallowed the object.
While coins and toy parts are the most commonly swallowed objects by children,5 fish bones and dentures represent the most often accidentally ingested objects by adults.4 Most ingested foreign bodies pass through the gastrointestinal tract without any complications, and gastrointestinal tract perforation is rare (<1%).1 Most cases of perforation are caused by ingestion of thin, pointed objects such as needles, toothpick, or fish and chicken bones,1 as well as batteries causing direct pressure necrosis, local electrical currents, and alkali leakage.6 However, in the present case, the object causing duodenal perforation was a lollipop stick with blunt ends, which is a very rare cause of perforation. The inability of the foreign body to pass the duodenum because of its length (7 cm) and the long-standing pressure leading to necrosis of the mucosa might have been the possible mechanisms of duodenal perforation in this case.
Conservative treatment is justified in most cases of foreign body ingestion, as most swallowed objects pass through the gastrointestinal tract easily. This is the treatment of choice if the foreign body is blunt, short (<6 cm), and narrow (<2.5 cm in diameter), and when it has passed through the pylorus. Spontaneous passage occur within 4 to 6 days.7 However, impacted objects in the esophagus require immediate removal, and objects within the stomach are often recommended to be removed early, especially when sharp objects and batteries are involved.8,9 Surgical intervention is required in <1% of cases.10
The traditional treatment of gastrointestinal perforation has been surgical repair. However, a nonsurgical strategy can be successful in certain cases. A successful conservative treatment in a case of a duodenal perforation, identified several days after the ingestion of a toothpick by a 15-year-old boy, has been reported.11 Since Binmoeller et al.12 reported a case of endoscopic closure of an iatrogenic gastric perforation by using metallic clips in 1993, attempts on managing bowel perforation nonsurgically have been successful. Furthermore, after a detachable snare was used for the first time in 1989 by Hachisu13 for hemostasis after the removal of large polyps, multiple case reports have been published on the successful management of bowel perforation by using endoscopy. In one case of esophageal perforation caused by a fishbone that had been ingested 1 day earlier, endoscopic clipping and antibiotic treatment were successful.14 In another case report of an esophageal perforation due to a dog bone, mediastinitis was found to be present and endoscopic treatment was performed 4 days after the foreign body ingestion, and the patient recovered without any other complications.15 In cases of esophageal perforations, indications for nonsurgical treatment include instrumental perforation, small perforations after therapeutic endoscopy, or minimal symptoms when perforations are diagnosed several days after the injury.16 Similar indications are applicable for the nonsurgical treatment of duodenal perforations. Kaneko et al.17 suggested some conditions for the endoscopic treatment of bowel perforations, such as adequate diameter and size of the perforation and an excellent visual field. In case of duodenal perforation due to foreign bodies, localized inflammation and absence of peritoneal irritation sign or sepsis should be considered in addition to these conditions because bacterial contamination is more common in this situation than iatrogenic perforation during endoscopic submucosal dissection or endoscopic retrograde cholangiopancreatography in fasting patients. Boškoski et al.18 reported a case of endoscopic closure of a duodenal wall perforation caused by a 12-cm teaspoon without peritoneal irritation signs, by using clips and fibrin glue. Delayed duodenal perforation caused by a biliary plastic stent in a patient with gallbladder cancer that was successfully managed by endoscopic closure with clips and a detachable snare has also been reported.19 In the present case, the patient did not have any toxic signs, abdominal CT revealed localized mottled air density around the duodenum, and the size of the perforation was small enough to be closed by using endoscopy, which are similar to the findings in previously published case series. Although the duodenal perforation was small, both hemoclips and a detachable snare were used in the present case because using clips alone often fails to achieve tight closure, owing to the relatively stiff wall of the duodenum compared with that of the stomach or the esophagus. In the past, we have experienced a few cases of dehiscence of duodenal perforation closed by using only clips, resulting in leakage of enteric fluid and peritonitis.
If the perforation is treated with endoclips, the patient should receive intravenous antibiotic therapy and a proton-pump inhibitor when the perforation site was the upper gastrointestinal tract. If an abdominal radiograph taken 24 hours after the intervention is negative for free air in the abdomen, and laboratory tests are normal, feeding can be advanced to liquid or solid diets after several days.20 In the present case, the patient received broad-spectrum antibiotics and a proton-pump inhibitor. After a few days of bowel rest without any complications, feeding was advanced and she was subsequently discharged 8 days after the procedure.
Gastrointestinal perforation by an ingested foreign body is rare but potentially life threatening. Sharp objects or batteries are the most common foreign bodies that cause perforation. However, blunt but long and stiff materials may fail to pass through the duodenum, also resulting in bowel perforation, as shown in this case. Although surgery has been the treatment of choice for intestinal perforation, reports on successful closure of perforation have been increasing with the progress of endoscopic techniques. Further studies to develop clinical guidelines for endoscopic treatment of gastrointestinal perforation are required.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg. 1996;20:1001–1005. doi: 10.1007/s002689900152. [DOI] [PubMed] [Google Scholar]
- 2.Goh BK, Chow PK, Quah HM, et al. Perforation of the gastrointestinal tract secondary to ingestion of foreign bodies. World J Surg. 2006;30:372–377. doi: 10.1007/s00268-005-0490-2. [DOI] [PubMed] [Google Scholar]
- 3.Coulier B, Tancredi MH, Ramboux A. Spiral CT and multidetectorrow CT diagnosis of perforation of the small intestine caused by ingested foreign bodies. Eur Radiol. 2004;14:1918–1925. doi: 10.1007/s00330-004-2430-1. [DOI] [PubMed] [Google Scholar]
- 4.Chiu YH, Hou SK, Chen SC, et al. Diagnosis and endoscopic management of upper gastrointestinal foreign bodies. Am J Med Sci. 2012;343:192–195. doi: 10.1097/MAJ.0b013e3182263035. [DOI] [PubMed] [Google Scholar]
- 5.Cheng W, Tam PK. Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg. 1999;34:1472–1476. doi: 10.1016/s0022-3468(99)90106-9. [DOI] [PubMed] [Google Scholar]
- 6.Marom T, Goldfarb A, Russo E, Roth Y. Battery ingestion in children. Int J Pediatr Otorhinolaryngol. 2010;74:849–854. doi: 10.1016/j.ijporl.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 7.Ambe P, Weber SA, Schauer M, Knoefel WT. Swallowed foreign bodies in adults. Dtsch Arztebl Int. 2012;109:869–875. doi: 10.3238/arztebl.2012.0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith MT, Wong RK. Foreign bodies. Gastrointest Endosc Clin N Am. 2007;17:361–382. doi: 10.1016/j.giec.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 9.ASGE Standards of Practice Committee. Ikenberry SO, Jue TL, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085–1091. doi: 10.1016/j.gie.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41:39–51. doi: 10.1016/s0016-5107(95)70274-1. [DOI] [PubMed] [Google Scholar]
- 11.Ragazzi M, Delcò F, Rodoni-Cassis P, Brenna M, Lavanchy L, Bianchetti MG. Toothpick ingestion causing duodenal perforation. Pediatr Emerg Care. 2010;26:506–507. doi: 10.1097/PEC.0b013e3181e5bf85. [DOI] [PubMed] [Google Scholar]
- 12.Binmoeller KF, Grimm H, Soehendra N. Endoscopic closure of a perforation using metallic clips after snare excision of a gastric leiomyoma. Gastrointest Endosc. 1993;39:172–174. doi: 10.1016/s0016-5107(93)70060-7. [DOI] [PubMed] [Google Scholar]
- 13.Hachisu T. A new detachable snare for hemostasis in the removal of large polyps or other elevated lesions. Surg Endosc. 1991;5:70–74. doi: 10.1007/BF00316840. [DOI] [PubMed] [Google Scholar]
- 14.Leem JM, Han JH, Ko BS, et al. A case of fishbone-induced esophageal perforation closed by endoscopic clipping. Korean J Gastrointest Endosc. 2010;41:151–154. [Google Scholar]
- 15.Han WS, Park JJ, Lee BJ, et al. A case of foreign body induced esophageal perforation repaired by endoscopic clipping. Korean J Gastrointest Endosc. 2007;35:28–32. [Google Scholar]
- 16.Jones WG, 2nd, Ginsberg RJ. Esophageal perforation: a continuing challenge. Ann Thorac Surg. 1992;53:534–543. doi: 10.1016/0003-4975(92)90294-e. [DOI] [PubMed] [Google Scholar]
- 17.Kaneko T, Akamatsu T, Shimodaira K, et al. Nonsurgical treatment of duodenal perforation by endoscopic repair using a clipping device. Gastrointest Endosc. 1999;50:410–413. doi: 10.1053/ge.1999.v50.97235. [DOI] [PubMed] [Google Scholar]
- 18.Boškoski I, Tringali A, Landi R, et al. Endoscopic retrieval of a duodenal perforating teaspoon. World J Gastrointest Endosc. 2013;5:186–188. doi: 10.4253/wjge.v5.i4.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nam HS, Kim GH, Kim DU, et al. A case of duodenal perforation caused by biliary plastic stent treated with approximation using endoclip and detachable snare. Korean J Gastroenterol. 2011;57:129–133. doi: 10.4166/kjg.2011.57.2.129. [DOI] [PubMed] [Google Scholar]
- 20.Mangiavillano B, Viaggi P, Masci E. Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis. 2010;11:12–18. doi: 10.1111/j.1751-2980.2009.00414.x. [DOI] [PubMed] [Google Scholar]