Abstract
Objective To examine associations between parental history of pain and catastrophizing and their adolescent’s pain, somatic symptoms, catastrophizing, and disability. Methods Participants included 178 youths aged 11–14 years recruited through public schools. Adolescents completed measures assessing pain characteristics, somatic symptoms, and pain catastrophizing. Parents reported on their own pain, and catastrophizing about their adolescent’s pain. Results About one quarter of the adolescents and two thirds of parents reported having pain. Parent pain was associated with adolescent pain, somatic symptoms, and pain catastrophizing. Parent catastrophizing was a significant predictor of adolescent somatic symptoms and pain-related disability, beyond the contribution of parent pain. Adolescent catastrophizing mediated the association between parent catastrophizing and adolescent pain-related disability. Conclusions Parent history of pain and pain-related cognitions may contribute to adolescent risk for chronic pain.
Keywords: adolescence, childhood, pain, pain catastrophizing, parent factors
Introduction
Pain typically serves an adaptive function, and the experience of some pain is a normative part of child development. However, faulty beliefs about pain, such as pain catastrophizing, may contribute to development or maintenance of persistent pain and pain-related disability. Previous research has consistently shown pain catastrophizing (i.e., cognitions that magnify the threat value of pain; Quartana, Campbell, & Edwards, 2009) to be elevated among clinical populations of children and adults with chronic pain, and to be associated with higher levels of disability (e.g., Crombez et al., 2003; Sullivan, Lynch, & Clark, 2005). Pain catastrophizing is likely present in community samples, and may help distinguish individuals at risk to become disabled by pain from those who continue functioning well in the face of pain. Early adolescence is a developmental period during which pain experiences increase in the general population (e.g., Stanford, Chambers, Biesanz, & Chen, 2008), and thus, pain beliefs are particularly important to examine during this developmental period.
Children’s pain beliefs do not develop in isolation, and parent and family factors have been identified as important influences on children’s experience of pain and pain-related disability (Palermo & Chambers, 2005). These parent and family factors include the parents’ history of chronic pain, individual parent behaviors and cognitions (e.g., protectiveness, catastrophizing), and the overall family environment (Kunz, Rainville, & Lautenbacher, 2011; Palermo & Chambers, 2005). Parent pain is related to children’s experience of pain and somatic symptoms in both clinical pediatric pain samples and community samples (Campo et al., 2007; Goodman, McGrath, & Forward, 1997; Lester, Lefebvre, & Keefe, 1994; Piira & Pullukat, 2006; Stanford et al., 2008). From a social learning perspective, children do not need to experience high frequency or intensity pain themselves to develop pain catastrophizing beliefs, as parents provide salient models of pain behaviors, beliefs, and coping (Bandura, 1977).
Parental cognitions about their child’s pain, specifically worry and catastrophizing, are associated with children’s responses to pain (Goubert, Eccleston, Vervoort, Jordan, & Crombez, 2006). Previous research has shown that parental worry and catastrophizing about children’s pain is associated with higher pain complaints, pain intensity, and disability among children with chronic pain (Guite, Logan, McCue, Sherry, & Rose, 2009; Hechler et al., 2011; Lynch-Jordan, Kashikar-Zuck, Szabova, & Goldschneider, 2013). Parental catastrophizing may also increase parent attention to child pain behaviors, which may serve to inadvertently increase pain and disability (e.g., Caes, Vervoort, Trost, & Goubert, 2012).
There is increasing support for the indirect role of parental responses to their child’s pain. For instance, parental catastrophizing about their child’s pain has been shown to be associated with child cognitions about pain, which in turn are related to the child’s pain-related disability (e.g., Vowles, Cohen, McCracken, & Eccleston, 2010; Wilson, Lewandowski, & Palermo, 2011). The indirect effect of parent responses to children’s pain has been demonstrated longitudinally, with adolescent cognitions, specifically catastrophizing, mediating the effect of parent protectiveness on pain and disability over time (Welkom, Hwang, & Guite, 2013). Child catastrophizing has consistently been shown to be associated with the experience of pain in children and adolescents. Healthy children who report pain-related catastrophizing experience higher pain intensity (Lu, Tsao, Myers, Kim, & Zeltzer, 2007; Piira, Taplin, Goodenough, & von Baeyer, 2002). Among children with chronic pain conditions and healthy children, catastrophizing has been associated with higher levels of pain and somatic symptoms and higher pain-related disability (Lynch, Kashikar-Zuck, Goldschneider, & Jones, 2006; Vervoort, Eccleston, Goubert, Buysse, & Crombez, 2010; Vervoort, Goubert, Eccleston, Bijttebier, & Crombez, 2006).
Early adolescence is a critical period for the emergence of chronic and recurrent pain, with studies showing increases in pain prevalence, particularly for girls, occurring between 12 and 14 years of age (Perquin et al., 2000). Estimates of weekly or more frequent pain range from 18% to 26% among 12–13 year-olds, with the most common locations including leg pain, headache, and abdominal pain (Larsson & Sund, 2007; Perquin et al., 2000; Stanford et al., 2008). Thus, the study of parent factors and their relationship to pain in early adolescence may be particularly important. Chronic pain in particular is a complex problem, which develops in the family and community setting well before presenting in the medical setting, and pediatric psychologists are uniquely posed to contribute to the development of prevention programs that might be targeted to reduce pain in high-risk youth.
Less is known about associations between parental catastrophizing, pain experiences, and disability among community samples of youth. One study found that parental catastrophizing was associated with pain in a community sample of youth but not with pain-related disability (Goubert et al., 2006). Understanding associations among parent pain, parental cognitions about pain, and child pain and disability in community samples may shed light on psychosocial mechanisms and systemic factors that may contribute to the development or maintenance of chronic pain problems in youth. Additionally, knowledge of these associations in community samples might inform the development of preventative interventions.
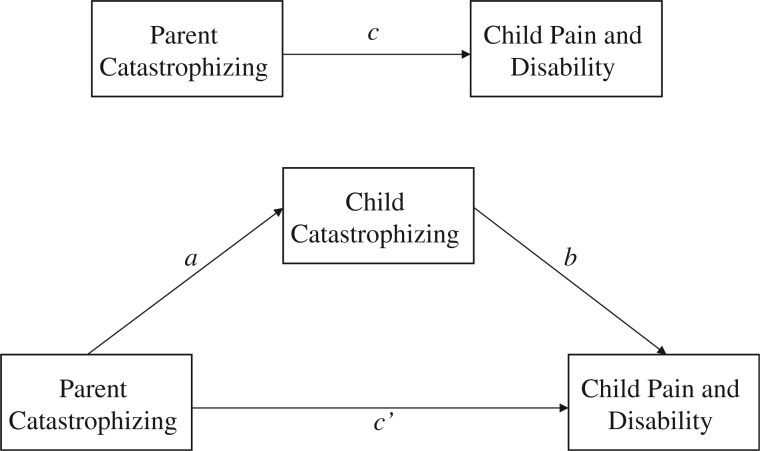
The current study is informed by a model of child pain outcomes that incorporates parent pain experiences, as well as parent and child psychological responses to pain (specifically catastrophizing). This model is adapted from an existing model of parent and family factors in pediatric chronic pain (Palermo & Chambers, 2005) and posits that parent catastrophizing about child pain will be directly associated with increased child pain, somatic symptoms, and pain-related disability. These parent and child factors occur in the context of parental pain, which is conceptualized as a parent factor associated with increased child pain and disability risk. The model also posits that parent responses to child pain contribute to child pain-related disability indirectly by influencing children’s own cognitions about pain, which will in turn be associated with disability (Figure 1).
Figure 1.
Theoretical model of the indirect association of parent catastrophizing with child pain and disability.
Therefore, study objectives were to (1) describe pain characteristics and pain catastrophizing in a community sample of early adolescents, (2) examine parental factors (parent pain, catastrophizing about the adolescent’s pain) that may be associated with higher levels of adolescent pain, somatic symptoms, and pain-related disability, and (3) examine the role of adolescent cognitions (pain catastrophizing) in pain-related disability and somatic symptoms. It was hypothesized that the presence of parent pain and higher parental catastrophizing would be associated with higher levels of adolescent pain and somatic symptoms, and with higher pain-related disability. It was also hypothesized that parental catastrophizing about adolescent pain would be indirectly associated with adolescent pain-related disability and somatic symptoms, such that adolescent catastrophizing mediates these associations.
Methods
Participants and Procedures
All study procedures were approved by the institutional review board at the first author’s home institution and by the participating schools’ district superintendents and principals. Youths (n = 178) aged 11–14 years (M = 12.36 years, 57.3% female) and their caregivers were recruited through two public middle schools, one suburban (School A, n = 123) and one rural (School B, n = 55). About 30% of students were classified as economically disadvantaged (defined by the State Department of Education as percentage of students receiving free school lunch at any point during the school year) at School A and 15.2% at School B. Children were recruited through sixth and seventh grade health, physical education, and/or home room classes, with the sample being composed of 102 sixth graders and 76 seventh graders. The majority of participating parents were mothers (90.1%), with the remainder being fathers. See Table I for additional school and participant characteristics.
Table I.
School and Participant Characteristics
| Characteristic | School A | School B | Study participantsb |
|---|---|---|---|
| Locale codesa | Town, fringe (suburban) | Rural, fringe (rural) | |
| Total enrollment | 468 | 356 | 173 |
| Grades | 6–8 | 5–8 | 6–7 |
| Students classified as economically disadvantaged, defined as receiving free lunch at any point during the school year | 29.7% | 15.2% | |
| Student body race/ethnicity | |||
| African American | 0.6% | 0.3% | 0.6% |
| American Indian | 0.4% | 0.0% | 0.0% |
| Asian American | 0.4% | 0.8% | 1.1% |
| Caucasian | 61.7% | 89.9% | 73.0% |
| Hispanic | 35.4% | 5.6% | 21.9% |
| Other/Unknown | 1.5% | 0.4% | 14.6% |
Note. aAs per National Center for Education Statistics guidelines: http://nces.ed.gov/ccd/rural_locales.asp#defs. Both schools on fringe of a large city (population > 500,000).
bChild race and/or ethnicity was not reported by 9.6% of participating parents.
A 10–15-min presentation about the study purpose and procedures was made to students, who were then provided with an informational flyer and informed consent and assent forms to take home and review with their parent(s) or caregiver(s). Children were not eligible to participate if they had a serious medical condition or chronic disease (e.g., cancer, arthritis) or were not English speaking. Parents were asked to report on whether their child had a serious medical condition when returning consent forms. Three youths were not eligible to participate due to the presence of a serious medical condition, and were not enrolled in the study. Adolescents and their parents completed questionnaire measures, and were provided with written and verbal instructions to complete the measures independently. Questionnaires were made available for participants to take home from school, and were returned to school 1 week later. Questionnaires were returned in person to a research assistant who checked each packet for overall completeness, and any parent or adolescent packets missing a page or more of responses were returned to the adolescent for completion. Measures assessing somatic symptoms, activity limitations, and catastrophizing were considered complete and included in analyses if ≥75% of the items were completed. Scores were calculated as the mean response multiplied by the number of items completed for each measure. Families received gift cards valued at $25.00 from local stores for their participation. Of the 178 enrolled families, five returned parent-report but not adolescent-report questionnaires. These five adolescents were not included in analyses for a final sample size of 173.
Measures
Sociodemographics
Parents completed a demographic and socioeconomic information form, including ethnicity, family income, and parental marital status.
Adolescent Pain Characteristics
Adolescent pain frequency in the past 3 months was assessed using a Likert-type scale with six response options, “not at all” to “daily.” Adolescent usual pain intensity was measured using an 11-point Numeric Rating Scale (NRS; 0–10), which has good evidence for reliability and validity (von Baeyer et al., 2009). Adolescents used a body map to indicate pain location(s). Psychometric data on these pain perception variables are available and indicate satisfactory validity (Peterson & Palermo, 2004).
Adolescent Somatic Symptoms
Somatic symptoms were assessed using the Children’s Somatization Inventory-24 (CSI-24; Walker, Beck, Garber, & Lambert, 2009). The CSI-24 assesses the presence of somatic symptoms including aches, pains, and other physical complaints. The CSI-24 has demonstrated excellent psychometric properties (Walker et al., 2009), and coefficient alpha in the current sample was .89.
Adolescent Disability
Adolescent report of pain-related disability was assessed using the Child Activity Limitations Interview-21 (CALI-21), a self-report version of the original interview measure (Palermo, Lewandowski, Long, & Burant, 2008). This 21-item questionnaire assesses difficulty participating in a variety of activities because of pain. Respondents rate difficulty using a Likert-type 5-point scale ranging from 0 (“not at all difficult”) to 4 (“extremely difficult”). The total scale was used, with higher scores indicating higher levels of pain-related disability. The CALI-21 has shown excellent reliability, and coefficient alpha in the current sample was .91.
Adolescent Pain Catastrophizing
Adolescent pain catastrophizing was assessed using the 13-item Pain Catastrophizing Scale-Child Version or PCS-C (Crombez et al., 2003). Items assessing catastrophic thoughts and feelings about pain use a Likert-type 5-point scale (0 = “not at all” to 4 = “extremely”). The PCS-C yields three subscale scores for rumination, magnification, and helplessness, as well as a total score ranging from 0 to 52. The total score was used in analyses in the current study, and coefficient alpha was .91 in the current sample.
Parent Pain Characteristics
Parents reported on their own current pain problems via a pain problem checklist, which was selected based on commonly endorsed pain problems in the general population. Parents were asked to indicate whether they currently experience the following (Yes = 1 or No = 0): back pain, headache, pain in limbs or joints, abdominal pain. Number of problems endorsed was also summed to create a 0–4 score indicating number of pain locations. Similar pain checklists and scoring systems have been used in previous research examining family pain history (e.g., Kashikar-Zuck et al., 2008; Laurell, Larsson, & Eeg-Olofsson, 2005).
Parent Catastrophizing
Parental catastrophizing about their adolescent’s pain was measured using the Pain Catastrophizing Scale-Parent Version (PCS-P; Goubert et al., 2006). The PCS-P includes 13 items concerning the different thoughts and feelings parents may have when their child experiences pain. Items assessing catastrophic thoughts and feelings about their child’s pain use a Likert-type 5-point scale (0 = “not at all” to 4 = “extremely”). The PCS-P yields three subscale scores for rumination, magnification, and helplessness, as well as a total score ranging from 0 to 52. The total score was used in analyses in the current study, and coefficient alpha for the PCS-P was .92 in the current sample.
Analyses
All analyses were conducted with SPSS v 21.0. Descriptive statistics were calculated for all study variables, and bivariate and Spearman correlations were conducted to examine associations between key study variables. Independent t-tests and Chi-square were used to test for differences in study variables by child sex. To test the direct effects of parent pain and parent catastrophizing, multiple linear regression models were conducted predicting pain frequency, usual pain intensity, somatic symptoms, and pain-related disability. Child sex was controlled for in Step 1, parent pain locations were entered in Step 2 and parental catastrophizing was entered in Step 3 of these models. To test the mediation model in which adolescent catastrophizing mediates the association between parental catastrophizing and adolescent pain-related disability, the Sobel test was used to test indirect effects (as per Preacher & Hayes, 2004). An alternative mediation model in which parental catastrophizing mediates the association between adolescent catastrophizing and pain-related disability was also tested.
Results
Descriptives of Adolescent Sample
About one quarter of the adolescents in the sample (26.6%) endorsed pain at least once a week, 23.1% reported pain 1–3 times per month, 25.4% reported pain <1 time per month, and 24.9% reported no pain in the past 3 months. Most frequently reported pain locations were as follows: leg (45.7%), back (28.3%), abdomen (19.1%), and head (15.0%). About one third of youth (30.0%) reported pain in more than one location. Usual pain intensity was low-moderate (M = 3.14/0–10 NRS, SD = 2.23), and somatic symptoms were low overall (CSI-24: M = 11.69, SD = 10.07), as was pain-related disability (CALI-21: M = 7.37, SD = 8.41). Pain catastrophizing was somewhat lower in this sample (PCS-C: M = 9.35, SD = 9.13) than in the sample of school children aged 8–16 years used in measure development (M score = 16.79; Crombez et al., 2003), and than a separate sample of 9–13-year-old school children (M score = 13.27; Vervoort et al., 2006) (Table II).
Table II.
Adolescent Pain Characteristics, Somatic Symptoms, Disability, and Catastrophizing
| Males | Females | Total | ||
|---|---|---|---|---|
| n = 74 | n = 99 | n = 173 | ||
| Variable | Observed range | M (SD)/N(%) | M (SD)/N(%) | M (SD)/N(%) |
| Pain frequency in past 3 months | ||||
| Not at all | 20 (27.0%) | 23 (23.2%) | 43 (24.9%) | |
| <1 time per month | 16 (21.6%) | 28 (28.3%) | 44 (25.4%) | |
| 1–3 times per month | 21 (28.4%) | 19 (19.2%) | 40 (23.1%) | |
| 1 time per week or morea | 17 (23.0%) | 29 (29.3%) | 36 (26.6%) | |
| Usual pain intensity (range: 0–10, NRS) | 0–8 | 3.04 (2.28) | 3.21 (2.20) | 3.14 (2.23) |
| Somatic symptoms (CSI-24, range 0–96) | 0–65 | 11.21 (8.69) | 12.10 (11.20) | 11.69 (10.06) |
| Pain-related disability (CALI-21, range 0–84) | 0–53 | 7.11 (9.12) | 7.58 (7.83) | 7.37 (8.41) |
| Adolescent pain catastrophizing (PCS-C, range 0–52) | 0–41 | 8.55 (7.98) | 10.93 (9.16) | 9.35 (9.13) |
| Parent pain catastrophizing (PCS-P, range 0–52)b | 0–42 | 7.44 (7.09) | 11.06 (10.36)* | 9.36 (9.13) |
Note. aCollapsed category includes responses of “once per week,” “2–3 times per week,” “4–6 times per week,” and “Daily.”
bParent report of catastrophizing about their adolescent’s pain.
*Females significantly higher than males, p = .02.
Descriptives of Parent Sample
Parents reported experiencing current pain problems at the following rates by location: back pain (41.8%), headache (37.0%), limb or joint pain (29.9%), and stomach pain (18.5%). Regarding the number of pain locations, 30.8% of parents reported no pain in these common locations, 30.8% reported one location, and 38.4% reported pain in two or more of these locations. The number of parent pain locations was correlated with higher parental catastrophizing about adolescent pain (Spearman’s rho = .40, p < .001), and with higher adolescent pain catastrophizing (Spearman’s rho = .24, p < .01). Parents also reported significantly higher levels of catastrophizing about adolescent pain for their female adolescent children compared with their male children (PCS-P for females M = 11.06, for males M = 7.44, p < .05). Overall, parental catastrophizing in this sample was somewhat lower than was reported in the sample of parents of school children aged 9–16 years used in development of the measure (M score = 15.67; Goubert et al., 2006).
Multiple Linear Regression Models Predicting Adolescent Outcomes
Separate multiple linear regression models were used to test the direct effects of parent pain and catastrophizing in the prediction of four adolescent outcomes: pain frequency, usual pain intensity, somatic symptoms, and pain-related disability (Table III). Adolescent sex was controlled for in Step 1, parent pain locations were entered in Step 2 (coded as 0 or 1 for presence of pain in each location), and parental catastrophizing was entered in Step 3. After controlling for child sex, the presence of parent back pain contributed significantly to adolescent pain frequency (β = .23, 95% CI .04–.35, p < .01,), pain intensity (β = .24, 95% CI .04–.35, p < .01), and somatic symptoms (β = .22, 95% CI .04–.35, p < .05). The presence of parent headache was also positively associated with adolescent pain frequency (β = .17, p < .05). No single parent pain location emerged as significant in the prediction of adolescent pain-related disability, although the presence of parent pain overall (i.e., across locations) contributed to pain-related disability. Parent catastrophizing was not associated with adolescent pain intensity or frequency, but made additional contributions beyond parent pain locations to adolescent somatic symptoms (β = .19, p < .05), and to pain-related disability (β = .24 p < .01). Overall, the amount of variance explained by parent pain and parental catastrophizing was low, with all R square change values being <.10. Observed power for the regression models ranged from 91.9 to 94.7%.
Table III.
Multiple Linear Regressions Predicting Adolescent Pain, Somatic Symptoms, and Disability
| Pain frequency |
Pain intensity |
Somatic symptoms (CSI-24) |
Pain-related disability (CALI-21) |
|||||
|---|---|---|---|---|---|---|---|---|
| Independent variables | Δ R2 | β at final | Δ R2 | β at final | Δ R2 | β at final | Δ R2 | β at final |
| Step 1: Sexa | .00 | −.04 | .00 | .03 | .00 | .01 | .00 | −.03 |
| Step 2: Parent pain | .10** | .10** | .07* | .06* | ||||
| Back pain | .23** | .24** | .22* | .05 | ||||
| Headache | .17* | .15 | .04 | .12 | ||||
| Abdominal pain | −.11 | .02 | −.07 | .00 | ||||
| Limb/joint pain | −.04 | .07 | .04 | .12 | ||||
| Step 3: Parental catastrophizing | .01 | .02 | .00 | −.03 | .03* | .19* | .05** | .24** |
Note. Values are standardized beta coefficients.
aCoded 0 = male, 1 = female.
*p < .05; **p < .01.
Testing Adolescent Pain Catastrophizing As a Mediator
Support was found for adolescent pain catastrophizing as a mediator of the association between parental catastrophizing and adolescent-report of pain-related disability. The initial significant association between parent catastrophizing and pain-related disability (β = .50, p < .001) was nonsignificant (β = .24, p = .11) after accounting for adolescent pain catastrophizing (β = .37, p < .05). This indirect effect (β = .26, 95% CI .14–.36) was significant (Sobel test, z = 2.01, p < .05), providing support for the hypothesis that parental catastrophizing about adolescent pain is associated with adolescent pain-related disability indirectly, through adolescent pain catastrophizing. The alternative model, testing parental catastrophizing as a mediator of the association between adolescent catastrophizing was not supported, with the indirect effect (β = .04, 95% CI −.01 to .36) being nonsignificant (Sobel test, z = 1.66, p = .10).
Contrary to hypotheses, no support was found for adolescent pain catastrophizing as a mediator of the association between parental catastrophizing and adolescent-report of somatic symptoms. The initial small but significant association between parent catastrophizing and pain-related disability was still significant after accounting for adolescent pain catastrophizing, with no significant indirect effect observed (β = .00, 95% CI −.002 to .004; Sobel test, z = 0.57, p = .57).
Discussion
Consistent with prior research, our results suggest that pain is a common experience among early adolescents, with 27% of the youth in our community sample reporting pain on a weekly or more frequent basis, and another 25% reporting pain several times per month. As compared with clinical samples, pain intensity and somatic complaints were relatively low; however, about one third of early adolescents reported pain in multiple locations. This comports with emerging evidence that early adolescence is a period of increasing risk for the emergence of chronic and recurrent pain. Leg pain was the most commonly experienced pain location, with nearly half the sample endorsing pain in that site. This finding is consistent with other research in healthy or community samples and likely represents “growing pains,” muscle soreness, minor injuries, or overuse (Kaspiris & Zafiropoulou, 2009). Other common pain locations parallel proportions seen in epidemiological samples with back, abdomen, and head pain representing the most commonly endorsed bodily locations.
A major aim of the present study was to examine the role of parental factors as contributors to child pain characteristics, somatic symptoms, and disability. Notably, location of parental pain appeared to contribute to youth’s pain experience. Children of parents who endorsed experiencing back pain were more likely to report increased frequency and intensity of pain, as well as more somatic symptoms. Likewise, children of parents with headache also endorsed greater pain frequency. The presence of parent pain overall also contributed significantly to adolescent pain-related disability and pain catastrophizing, although no one parent pain location emerged as significant in these analyses. Consistent with previous research, these findings provide additional evidence for parental pain history as being associated with children’s experience of pain and somatic symptoms, as well as with pain impact (e.g., Levy et al., 2004). Parental psychological responses to their adolescent’s pain, particularly parent pain catastrophizing, were significantly associated with adolescent pain-related disability and catastrophizing after controlling for parent pain locations. This is in contrast to one previous study that did not show an association between parental pain catastrophizing and pain-related disability in a community sample (Goubert et al., 2006), but consistent with prior findings in clinical pain samples (Guite et al., 2009; Vowles et al., 2010). It should be noted that the contribution of parent pain and catastrophizing, though significant, was fairly small.
Integral to the current study was the role of pain catastrophizing as a potential mechanism explaining the link between parental pain catastrophizing and adolescent disability. Catastrophizing about adolescent pain appears to be more likely among parents who experience pain themselves, and is related to adolescent outcomes. We found that parental catastrophizing about their adolescent’s pain uniquely explained a substantial proportion of variance in adolescent-reported frequency of pain, as well as somatic complaints and pain-related disability, even after controlling for the presence of parental pain. This is consistent with recent findings in clinical samples of youth, which have suggested that parental beliefs about pain contribute to pain perceptions and impact (Vowles et al., 2010). To further explicate the relationship between parental cognitions and adolescent disability, we tested a model wherein parental pain catastrophizing operated indirectly on adolescent pain-related disability, through the adolescent’s own pain-related beliefs. Our results provide support for this indirect model, and highlight the role of adolescent pain catastrophizing as a potential mechanism explaining the association between parental catastrophizing about adolescent pain and pain-related disability. Importantly, an alternative mediation model where parent catastrophizing mediated the association between adolescent catastrophizing and pain-related disability was not supported, thus affirming support for the hypothesized mediation model. Parental catastrophizing about their adolescent’s pain may increase the likelihood that adolescents will catastrophize themselves, which in turn is associated with increased disability.
The current study has several implications for the design of preventative interventions. First, the examination of parental factors and adolescent catastrophizing in a community sample may inform the identification of youth at increased risk for developing chronic pain and related disability. Results from the current study suggest that a portion of youth and their parents evidence levels of catastrophizing that are similar to that seen in clinical populations (e.g., Lynch-Jordan et al., 2013), and might benefit from preventative interventions. The results suggest that parents would need to be involved in prevention programs, and that pain catastrophizing would potentially be a good target for a cognitive intervention with high-risk youth and their parents. Examination of parental pain catastrophizing and other parent psychological responses to their adolescent’s pain (e.g., worry, pain-related fear) in community samples will help increase our understanding of psychosocial mechanisms of pain across the developmental period of adolescence and may identify additional potential targets for preventive interventions. Future work might also examine these associations over time, and with approaches such as structural equation modeling, which might be used to confirm theoretical models of parent factors and pain beliefs in large community samples.
Study Limitations
This study provides a useful starting point in our understanding of parental pain catastrophizing and its impact on adolescent pain characteristics and related disability in a community sample of youth. The following limitations can help inform directions for future research. First, the present study relied exclusively on parent and adolescent self-report. Although this is a useful initial step when investigating a construct like pain catastrophizing, which is primarily cognitive in nature, future research would benefit from the inclusion of behavioral observations and/or an experimental paradigm to help clarify ways in which parental catastrophizing is communicated to adolescents. Such an approach would allow for exploration of potential behavioral mechanisms (i.e., modeling, attention to pain, activity avoidance) that might further explain the link between parental pain catastrophizing and adolescent outcomes. The present study also measured a restricted age-range at one point in time. While the present findings clearly highlight the importance of the early adolescent period, extending the age range to include older adolescents or investigating these processes longitudinally may lead to a better understanding of how parental and adolescent catastrophizing impacts the pain experience over time. Given the school-based survey method, it is also possible that parents and children did not complete measures independently, despite instructions to do so. Results may also not generalize to adolescents in other communities, as the sample was primarily Caucasian. Finally, the current study used a restricted measure of parent pain; future research would benefit from inclusion of a more thorough and multidimensional assessment of parental pain history, including pain impact and disability.
Conclusions
Results indicate that parental pain status and cognitions are associated with adolescent pain perceptions, somatic symptoms, and pain-related disability in a community sample of early adolescents. These findings parallel emerging evidence in clinical samples of youth with chronic pain and their parents, and highlight the importance of incorporating parents in future prevention and intervention efforts. Although a growing body of research suggests that parental factors play a key role in the pain experience of children and adolescents, additional research is needed to clarify potential mechanisms through which such factors lead to increased pain for adolescents (e.g., modeling, communication about pain cognitions). Parent pain experiences and parent cognitions may help identify adolescents at risk for developing chronic pain problems who may benefit from preventive interventions.
Funding
NIH/NICHD K23HD064705 (PI: A.C.W.). Oregon Clinical and Translational Research Institute (OCTRI), (UL1TR000128) from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH).
Conflicts of interest: None declared.
References
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- Caes L, Vervoort T, Trost Z, Goubert L. Impact of parental catastrophizing and contextual threat on parents' emotional and behavioral responses to their child's pain. Pain. 2012;153:687–695. doi: 10.1016/j.pain.2011.12.007. [DOI] [PubMed] [Google Scholar]
- Campo J V, Bridge J, Lucas A, Savorelli S, Walker L, Di Lorenzo C, Iyengar S, Brent D A. Physical and emotional health of mothers of youth with functional abdominal pain. Archives of Pediatrics and Adolescent Medicine. 2007;161:131–137. doi: 10.1001/archpedi.161.2.131. [DOI] [PubMed] [Google Scholar]
- Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K. The child version of the Pain Catastrophizing Scale (PCS-C): A preliminary validation. Pain. 2003;104:639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- Goodman J E, McGrath P J, Forward S P. Aggregation of pain complaints and pain-related disability and handicap in a community sample of families. In: Jensen T S, Turner J A, Wiesenfeld Z, editors. Proceedings of the World Congress in Pain, Progress in Pain and Pain Research. Seattle, WA: IASP Press; 1997. pp. 673–682. [Google Scholar]
- Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G. Parental catastrophizing about their child's pain. The parent version of the Pain Catastrophizing Scale (PCS-P): A preliminary validation. Pain. 2006;123:254–263. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- Guite J W, Logan D E, McCue R, Sherry D D, Rose J B. Parental beliefs and worries regarding adolescent chronic pain. The Clinical Journal of Pain. 2009;25:223–232. doi: 10.1097/AJP.0b013e31818a7467. doi:1097/AJP.1090b1013e31818a37467. [DOI] [PubMed] [Google Scholar]
- Hechler T, Vervoort T, Hamann M, Tietze AL, Vocks S, Goubert L, Hermann C, Wager J, Blankenburg M, Schroeder S, Zernikow B. Parental catastrophizing about their child's chronic pain: Are mothers and fathers different? European Journal of Pain. 2011;15:515.e1–59. doi: 10.1016/j.ejpain.2010.09.015. [DOI] [PubMed] [Google Scholar]
- Kashikar-Zuck S, Lynch A M, Slater S, Graham T B, Swain N F, Noll R B. Family factors, emotional functioning, and functional impairment in juvenile fibromyalgia syndrome. Arthritis and Rheumatism. 2008;59:1392–1398. doi: 10.1002/art.24099. [DOI] [PubMed] [Google Scholar]
- Kaspiris A, Zafiropoulou C. Growing pains in children: Epidemiological analysis in a Mediterranean population. Joint Bone Spine. 2009;76:486–490. doi: 10.1016/j.jbspin.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Kunz M, Rainville P, Lautenbacher S. Operant conditioning of facial displays of pain. Psychosomatic Medicine. 2011;73:422–431. doi: 10.1097/PSY.0b013e318218db3e. [DOI] [PubMed] [Google Scholar]
- Larsson B, Sund A M. Emotional/behavioural, social correlates and one-year predictors of frequent pains among early adolescents: Influences of pain characteristics. European Journal of Pain. 2007;11:57–65. doi: 10.1016/j.ejpain.2005.12.014. [DOI] [PubMed] [Google Scholar]
- Laurell K, Larsson B, Eeg-Olofsson O. Headache in schoolchildren: Association with other pain, family history and psychosocial factors. Pain. 2005;119:150–158. doi: 10.1016/j.pain.2005.09.030. [DOI] [PubMed] [Google Scholar]
- Lester N, Lefebvre J C, Keefe F J. Pain in young adults: I. Relationship to gender and family pain history. The Clinical Journal of Pain. 1994;10:282–289. doi: 10.1097/00002508-199412000-00007. [DOI] [PubMed] [Google Scholar]
- Levy R L, Whitehead W E, Walker L S, Von Korff M, Feld A D, Garner M, Christie D. Increased somatic complaints and health-care utilization in children: Effects of parent IBS status and parent response to gastrointestinal symptoms. The American Journal of Gastroenterology. 2004;99:2442–2451. doi: 10.1111/j.1572-0241.2004.40478.x. [DOI] [PubMed] [Google Scholar]
- Lu Q, Tsao J C, Myers C D, Kim S C, Zeltzer L K. Coping predictors of children's laboratory-induced pain tolerance, intensity, and unpleasantness. The Journal of Pain. 2007;8:708–717. doi: 10.1016/j.jpain.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Lynch A M, Kashikar-Zuck S, Goldschneider K R, Jones B A. Psychosocial risks for disability in children with chronic back pain. The Journal of Pain. 2006;7:244–251. doi: 10.1016/j.jpain.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Lynch-Jordan A M, Kashikar-Zuck S, Szabova A, Goldschneider K R. The interplay of parent and adolescent catastrophizing and its impact on adolescents' pain, functioning, and pain behavior. The Clinical Journal of Pain. 2013;29:681–688. doi: 10.1097/AJP.0b013e3182757720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T M, Chambers C T. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain. 2005;119:1–4. doi: 10.1016/j.pain.2005.10.027. [DOI] [PubMed] [Google Scholar]
- Palermo T M, Lewandowski A S, Long A C, Burant C J. Validation of a self-report questionnaire version of the child activity limitations interview (CALI): The CALI-21. Pain. 2008;139:644–652. doi: 10.1016/j.pain.2008.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perquin C W, Hazebroek-Kampschreur A A, Hunfeld J A, Bohnen A M, van Suijlekom-Smit L W, Passchier J, van der Wouden J C. Pain in children and adolescents: A common experience. Pain. 2000;87:51–58. doi: 10.1016/S0304-3959(00)00269-4. [DOI] [PubMed] [Google Scholar]
- Peterson CC, Palermo TM. Parental reinforcement of recurrent pain: The moderating impact of child depression and anxiety on functional disability. The Journal of Pain. 2004;29:331–341. doi: 10.1093/jpepsy/jsh037. [DOI] [PubMed] [Google Scholar]
- Piira T, Pullukat R. Are the children of chronic pain patients more likely to develop pain? Enfance. 2006;58:20–25. [Google Scholar]
- Piira T, Taplin J E, Goodenough B, von Baeyer C L. Cognitive-behavioural predictors of children's tolerance of laboratory-induced pain: Implications for clinical assessment and future directions. Behaviour Research and Therapy. 2002;40:571–584. doi: 10.1016/s0005-7967(01)00073-0. [DOI] [PubMed] [Google Scholar]
- Preacher K J, Hayes A F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Quartana P J, Campbell C M, Edwards R R. Pain catastrophizing: A critical review. Expert Review of Neurotherapeutics. 2009;9:745–758. doi: 10.1586/ERN.09.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford E A, Chambers C T, Biesanz J C, Chen E. The frequency, trajectories and predictors of adolescent recurrent pain: A population-based approach. Pain. 2008;138:11–21. doi: 10.1016/j.pain.2007.10.032. [DOI] [PubMed] [Google Scholar]
- Sullivan M J, Lynch M E, Clark A J. Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain. 2005;113:310–315. doi: 10.1016/j.pain.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Vervoort T, Eccleston C, Goubert L, Buysse A, Crombez G. Children's catastrophic thinking about their pain predicts pain and disability 6 months later. European Journal of Pain. 2010;14:90–96. doi: 10.1016/j.ejpain.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Vervoort T, Goubert L, Eccleston C, Bijttebier P, Crombez G. Catastrophic thinking about pain is independently associated with pain severity, disability, and somatic complaints in school children and children with chronic pain. Journal of Pediatric Psychology. 2006;31:674–683. doi: 10.1093/jpepsy/jsj059. [DOI] [PubMed] [Google Scholar]
- von Baeyer C L, Spagrud L J, McCormick J C, Choo E, Neville K, Connelly M A. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children's self-reports of pain intensity. Pain. 2009;143:223–227. doi: 10.1016/j.pain.2009.03.002. [DOI] [PubMed] [Google Scholar]
- Vowles K E, Cohen L L, McCracken L M, Eccleston C. Disentangling the complex relations among caregiver and adolescent responses to adolescent chronic pain. Pain. 2010;151:680–686. doi: 10.1016/j.pain.2010.08.031. [DOI] [PubMed] [Google Scholar]
- Walker L S, Beck J E, Garber J, Lambert W. Children's somatization inventory: Psychometric properties of the revised form (CSI-24) Journal of Pediatric Psychology. 2009;34:430–440. doi: 10.1093/jpepsy/jsn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welkom J S, Hwang W T, Guite J W. Adolescent pain catastrophizing mediates the relationship between protective parental responses to pain and disability over time. Journal of Pediatric Psychology. 2013;38:541–550. doi: 10.1093/jpepsy/jst011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson A, Lewandowski A, Palermo T M. Fear-avoidance beliefs and parental responses to pain in adolescents with chronic pain. Pain Research and Management. 2011;16:178–182. doi: 10.1155/2011/296298. [DOI] [PMC free article] [PubMed] [Google Scholar]