Abstract
Purpose
Current management for patients with differentiated thyroid cancer includes near total thyroidectomy and radioactive iodine therapy followed by administration of supraphysiological doses of levothyroxine (L-T4). Although hyperthyroidism is a well known risk factor for osteoporosis, the effects of L-T4 treatment on bone mineral density (BMD) in patients with thyroid cancer do not appear to be as significant as with endogenous hyperthyroidism. In this study, we evaluated the impact of long-term suppressive therapy with L-T4 on BMD and bone turn over markers in Korean female patients receiving L-T4 suppressive therapy.
Methods
We enrolled 94 female subjects (mean age, 50.84 ± 11.43 years) receiving L-T4 after total or near total thyroidectomy and radioactive iodine therapy for thyroid cancer (mean follow-up period, 12.17 ± 4.27 years). The subjects were divided into three groups by thyroid stimulating hormone (TSH) level (group 1 with TSH level ≤0.001 µIU/mL, group 2 with TSH level between 0.001 and 0.17 µIU/mL, group 3 with TSH level >0.17 µIU/mL) and four groups by quartile of free T4 level. L-T4 dosage, BMD (examined by dual-energy x-ray absorptiometry), and bone turnover markers were evaluated according to TSH and free T4 levels.
Results
No significant decrease was detected in BMD or bone turnover markers according to TSH level or free T4 level. Also, the prevalence of osteoporosis and osteopenia was not different among groups.
Conclusion
Long-term L-T4 suppressive therapy after thyroid cancer management did not affect bone density or increase the prevalence of osteoporosis even though TSH levels were supraphysiologically suppressed.
Keywords: Thyroid neplasms, Levothyroxine, Bone mineral density, Osteoporosis, Osteopenia
INTRODUCTION
Current management for patients with differentiated thyroid cancer includes near total thyroidectomy and radioactive iodine therapy followed by administration of supraphysiological doses of levothyroxine (L-T4). Because hyperthyroidism accelerates bone turnover and shortens the normal bone remodeling cycle [1,2], it was expected that suppressive L-T4 therapy for differentiated thyroid cancer might influence bone mineral density (BMD). Although longitudinal studies in patients with suppressive L-T4 therapy for differentiated thyroid cancer have reported conflicting data [3-12], the majority of investigators have concluded that recommended dose of L-T4 for postoperative therapy does not have negative effects on bone density [13]. However, the effects of suppressive L-T4 therapy on bone density in the Korean population have not been well defined. The aim of our study is to evaluate the impact of long-term suppressive therapy with L-T4 on BMD and bone turnover markers in Korean female patients who have undergone suppressive therapy for more than 10 years.
METHODS
Subjects
This cross-sectional study was conducted at a single center, Yonsei University Wonju College of Medicine, Korea. Ninety-four female subjects (range, 35-79 years) who underwent total or near total thyroidectomy and radioactive iodine therapy due to thyroid-differentiated carcinoma were enrolled in the study. We enrolled subjects from October 2009 to October 2010. Mean follow-up period was 12.17 ± 4.27 years (median, 12.00 years; range, 5-22 years) and 60.4% of enrolled subjects had been receiving L-thyroxine for more than 10 years. The mean dosage of L-thyroxine during the follow-up period was 160 µg (range, 25-200 µg/day). The percentage of subjects who were premenopausal was 66.7%. Patients with a history of vertebral or femoral fracture that were treated with agents that could interfere with bone metabolism, such as steroids and bisphosphonates, were excluded. To examine the effects of L-T4 on skeletal tissue, we analyzed BMD, bone turnover markers, and biochemical parameters from all subjects, who were divided into three groups by thyroid stimulating hormone (TSH) level (group 1 with TSH level ≤0.001 µIU/mL; group 2 with TSH level between 0.001 and 0.17 µIU/mL; group 3 with TSH level >0.17 µIU/mL) and four groups by quartile of free T4 level. Because most patient TSH levels were suppressed below 0.01 µIU/mL (61.4% of subjects), TSH level could not be grouped into tertiles. Instead, patients with TSH level above 0.01 µIU/mL were divided into two groups-upper 50% and lower 50%.
BMD and laboratory assays
BMD was measured at the lumbar spine (levels L2-4), femur neck, and trochanter by dual-energy radiographic absorptiometry (LUNAR prodigy, GE Healthcare, Little Chalfont, UK). T-score was defined as the number of standard deviations (SDs) between measured values and the mean for a control group from the general population matched for gender at 25-45 years of age. T-score ≤-2.5 SD at the lumbar spine, femur neck, or femur trochanter was defined as osteoporosis; T-score between -2.5 and -1.0 SD was defined as osteopenia; T-score ≥ -1.0 was defined as normal. A serum sample was taken from each participant without overnight fasting. We measured free T4 and TSH using the Centaur system (Siemens, Munich, Germany). For bone turnover markers, osteocalcin representative bone formation marker and C-telopeptides of type I collagen (CTX, Modular E170, Hoffmann-La Roche, Basel, Switzerland) representative bone resorption marker were measured.
Statistical analysis
Data were expressed as the mean ± SD. A one-way analysis of variance was used for the comparison of various anthropometric parameters, biochemical parameters, and BMD. The associations between the prevalence of osteoporosis or osteopenia and TSH and FT4 stratified groups were assessed using a chisquare test. The odds ratios were analyzed using logistic regression. All analyses were done using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) and SAS ver. 9.2 (SAS Institute, Cary, NC, USA). A P-value <0.05 was considered significant.
RESULTS
The clinical characteristics of the subjects are summarized in Table 1. Mean duration of LT4 treatment was 15.0 ± 5.7 years, and mean L-T4 dose was 125.27 ± 38.81 µg/day (range, 25-200 µg/day). Because most patient TSH levels were suppressed below 0.01 µU/mL, the subjects of group 1 defined by TSH ≤0.001 µIU/mL represented 61.17% of participants. The subjects of group 2 defined by TSH >0.001 to ≤0.17 µIU/mL and group 3 defined by TSH >0.17 µIU/mL accounted for 17% and 21% of patients, respectively. Mean BMD contents and T-scores for each group divided by TSH level did not differ significantly among groups (Table 2). Also, bone turnover markers and prevalence of osteoporosis and osteopenia were not different among groups (Table 2). For grouping by FT4 level, all subjects were divided into FT4 quartiles. The subjects of Q1, Q2, Q3, and Q4 were defined by FT4 ≤1.44 ng/dL, FT4 >1.44 through ≤1.63 ng/dL, FT4 >1.63 through ≤1.86 ng/dL, and FT4 >1.86 ng/dL, respectively. The relationship between BMD and prevalence of osteoporosis and osteopenia also did not show any differences among the four FT4 groups (Table 3). No differences existed between BMD and bone turnover markers among groups according to FT4 and TSH levels when subgroup analysis was performed according to state of menopause (data not shown). The odds ratios for risk of osteoporosis and osteopenia in groups 2 and 3 were not significant when compared to the reference group (group 1) (Table 4). The odds ratios for risk of osteoporosis and osteopenia in Q2, Q3, and Q4 by FT4 were not significantly larger than the reference group (Q 1) (Table 4). Also, the prevalence of osteoporosis and osteopenia was not different among groups (Table 4).
Table 1.
Characteristics of participants (n = 94)
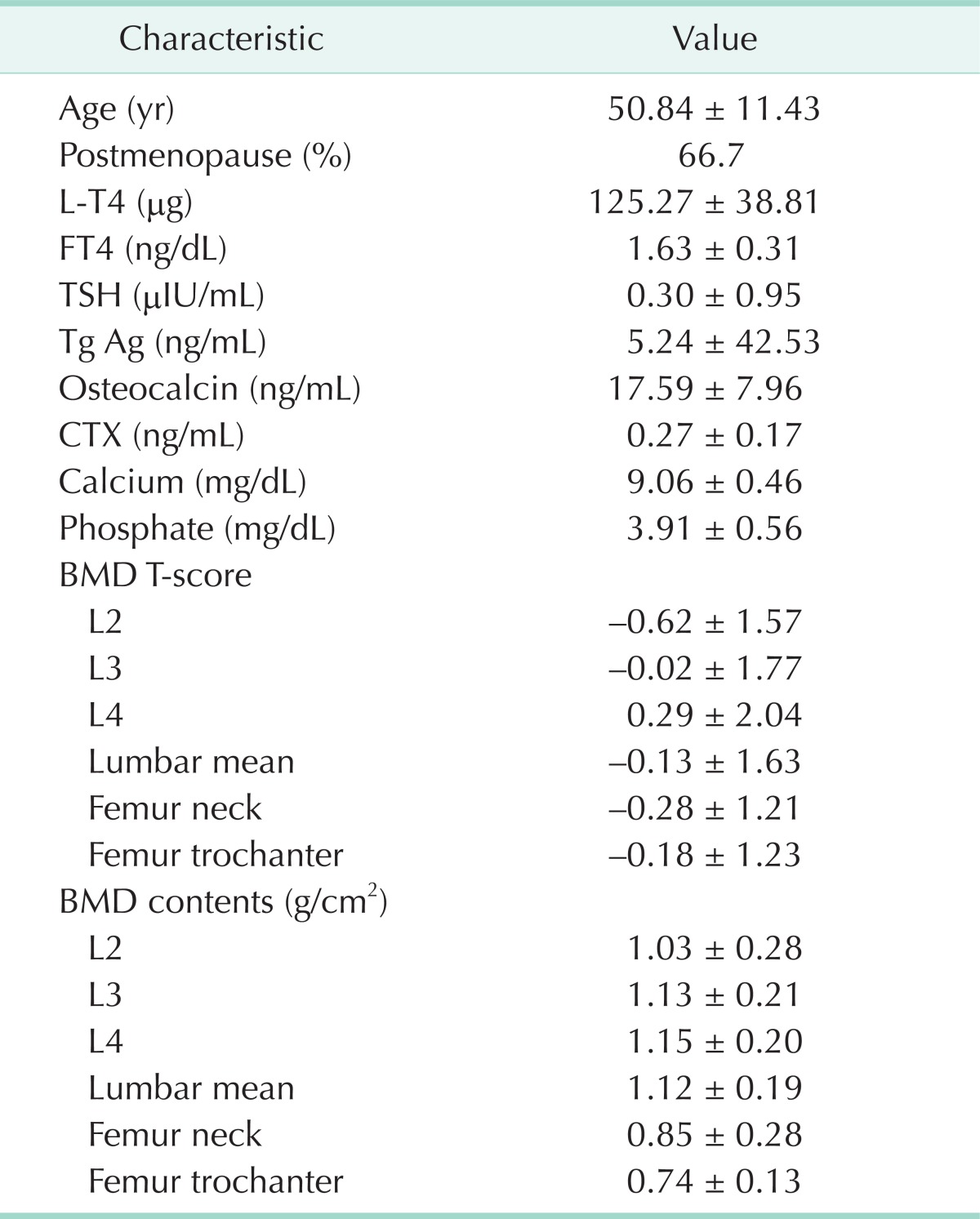
Values are presented as mean ± standard deviaion.
L-T4, levothyroxine; FT4, free T4; TSH, thyroid stimulating hormone; Tg Ag, thyroglobulin antigen; CTX, C-telopeptides of type I collagen; BMD, bone mineral density.
Table 2.
BMD and prevalence of osteoporosis or osteopenia grouped by TSH level
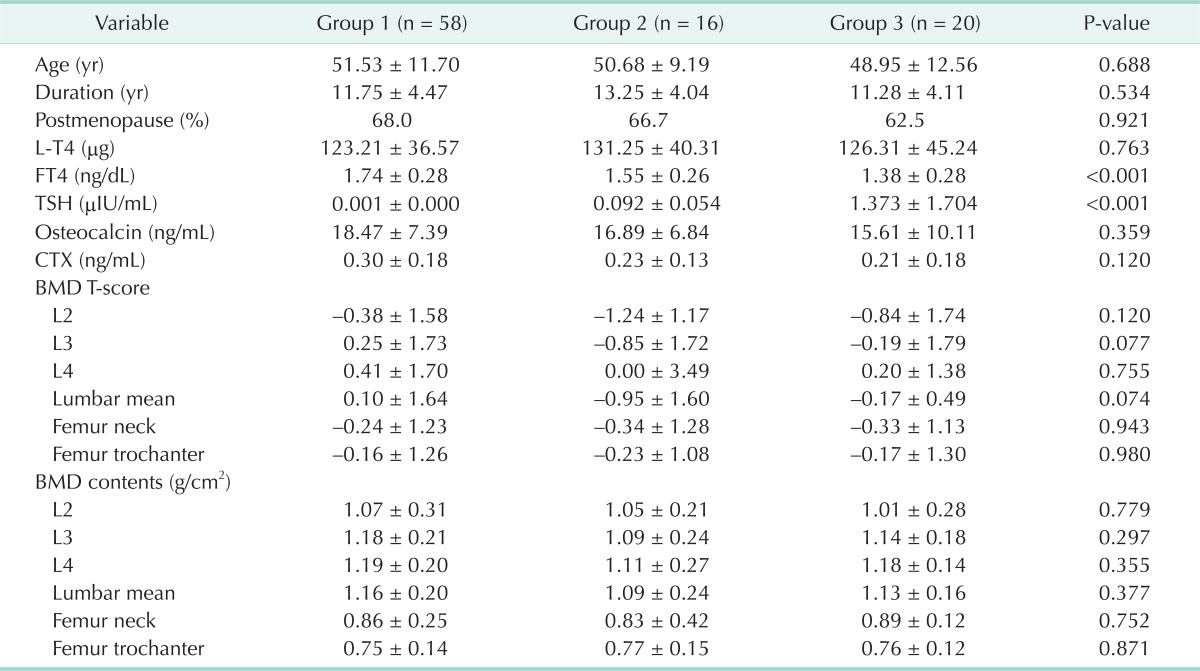
Values are presented as mean ± standard deviaion.
BMD, bone mineral density; TSH, thyroid stimulating hormone; L-T4, levothyroxine; FT4, free T4; Tg Ag, thyroglobulin antigen; CTX, C-telopeptides of type I collagen.
Table 3.
BMD and prevalence of osteoporosis or osteopenia grouped by FT4 quartile
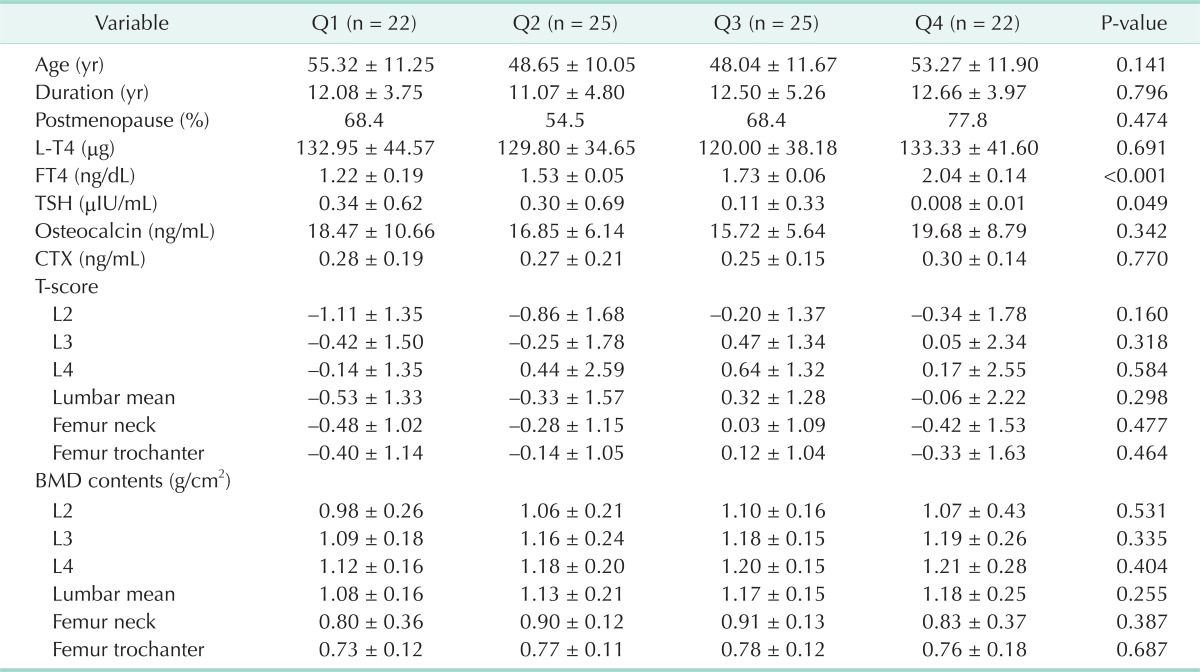
Values are presented as mean ± standard deviaion.
BMD, bone mineral density; FT4, free T4; L-T4, levothyroxine; TSH, thyroid stimulating hormone; Tg Ag, thyroglobulin antigen; CTX, C-telopeptides of type I collagen.
Table 4.
Odds ratios of osteoporosis and osteopenia by regression analysis according to FT4 and TSH groups
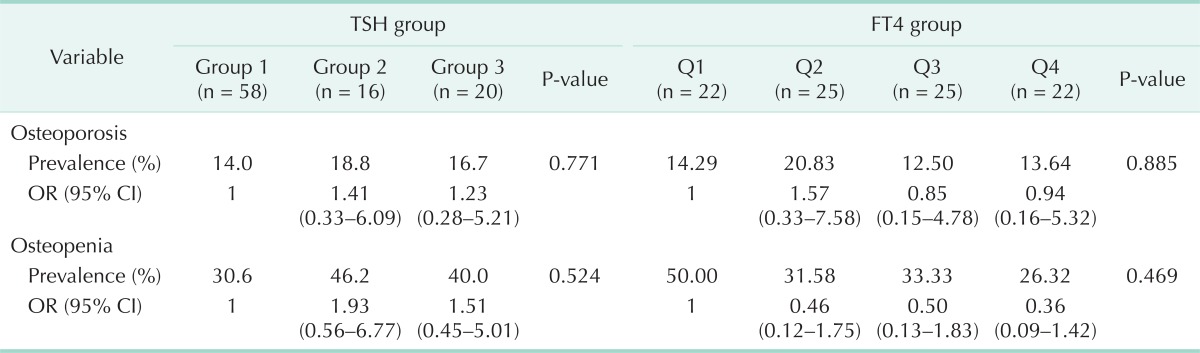
FT4, free T4; TSH, thyroid stimulating hormone; OR, odds ratio; CI, confidence interval.
DISCUSSION
Although overt endogenous hyperthyroidism is known to be an important risk factor of osteoporosis, osteopenia, and osteoporotic fracture [14-17], the clinical outcome of patients with subclinical hyperthyroidism, mild thyrotoxicosis associated with treatment of levothyroxine for hypothyroidism, or suppression therapy after thyroid cancer remains unclear [3-8,18,19].
Abe et al. [20] reported that the TSH receptor is expressed in osteoblasts and osteoclasts. Also, TSH treatment could suppress bone turnover and prevent bone loss [20,21]. Two other in vitro studies reported that increased thyroid hormone-not decreased TSH level-induced bone loss [22,23]. Subsequently, although composited results also exist [24], the roles of thyroid hormone and TSH on BMD have been emphasized by clinicians.
Patients with differentiated thyroid cancer have been treated with a supraphysiological dose of levothyroxine for inhibition of tumor recurrence and metastasis after total or near total thyroidectomy. Clinical studies regarding the relationship between levothyroxine treatment and bone turnover markers or BMD do not show consistent results. Thus, the effect of high dose levothyroxine on bone metabolism remains controversial.
There have been no data about levothyroxine or BMD reported from patients with differentiated thyroid cancer in Korea. In our data, the prevalence of osteoporosis and osteopenia were not different between patients with different TSH suppression and different levels of FT4. Also, BMD and bone turnover markers were not different among the patient groups. However, the prevalence of osteoporosis and osteopenia did not show consistent change according to increase of TSH or decrease of FT4 level. Although we expected that the prevalence of osteoporosis and osteopenia would decrease incrementally according to TSH level, the results were contrary to our expectation. This may be due to the number of subjects: because a large number of patients were treated with levothyroxine up to TSH level < 0.003 µIU/mL, the number of subjects with high TSH level and low FT4 level was relatively small. Therefore, the prevalence of osteoporosis and osteopenia among subjects with high TSH level and low FT4 level may seem improbably high. Because the purpose of TSH suppression is prevention of tumor recurrence, we attempted to suppress the TSH level below the undetectable level. But, for patients with old age, comorbid condition, or reduced adherence to medication due to thyrotoxic symptoms, we suppressed the TSH level to 0.1-2.0 µIU/mL. So, the majority of the subjects showed TSH levels of <0.003 µIU/mL.
The limitations of our study include small sample size and the fact that all participants were enrolled at a single center. Also, we could not analyze daily calcium intake or exercise-both known to be influencing factors for osteoporosis and osteopenia. Finally, because we performed a cross-sectional study, we could not obtain the initial BMD and other markers that was the another limitation of our study. So, further prospective studies are needed.
In conclusion, we suggest that the degree of TSH suppression in thyroid cancer patients is not directly related to bone health, and long-term treatment with levothyroxine can be safely used in patients with total or subtotal thyroidectomy after thyroid cancer.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Eriksen EF. Normal and pathological remodeling of human trabecular bone: three dimensional reconstruction of the remodeling sequence in normals and in metabolic bone disease. Endocr Rev. 1986;7:379–408. doi: 10.1210/edrv-7-4-379. [DOI] [PubMed] [Google Scholar]
- 2.Mosekilde L, Eriksen EF, Charles P. Effects of thyroid hormones on bone and mineral metabolism. Endocrinol Metab Clin North Am. 1990;19:35–63. [PubMed] [Google Scholar]
- 3.Diamond T, Nery L, Hales I. A therapeutic dilemma: suppressive doses of thyroxine significantly reduce bone mineral measurements in both premenopausal and postmenopausal women with thyroid carcinoma. J Clin Endocrinol Metab. 1991;72:1184–1188. doi: 10.1210/jcem-72-6-1184. [DOI] [PubMed] [Google Scholar]
- 4.Florkowski CM, Brownlie BE, Elliot JR, Ayling EM, Turner JG. Bone mineral density in patients receiving suppressive doses of thyroxine for thyroid carcinoma. N Z Med J. 1993;106:443–444. [PubMed] [Google Scholar]
- 5.Franklyn JA, Betteridge J, Daykin J, Holder R, Oates GD, Parle JV, et al. Long-term thyroxine treatment and bone mineral density. Lancet. 1992;340:9–13. doi: 10.1016/0140-6736(92)92423-d. [DOI] [PubMed] [Google Scholar]
- 6.Hawkins F, Rigopoulou D, Papapietro K, Lopez MB. Spinal bone mass after long-term treatment with L-thyroxine in postmenopausal women with thyroid cancer and chronic lymphocytic thyroiditis. Calcif Tissue Int. 1994;54:16–19. doi: 10.1007/BF00316283. [DOI] [PubMed] [Google Scholar]
- 7.Pioli G, Pedrazzoni M, Palummeri E, Sianesi M, Del Frate R, Vescovi PP, et al. Longitudinal study of bone loss after thyroidectomy and suppressive thyroxine therapy in premenopausal women. Acta Endocrinol (Copenh) 1992;126:238–242. doi: 10.1530/acta.0.1260238. [DOI] [PubMed] [Google Scholar]
- 8.Rosen HN, Moses AC, Garber J, Ross DS, Lee SL, Ferguson L, et al. Randomized trial of pamidronate in patients with thyroid cancer: bone density is not reduced by suppressive doses of thyroxine, but is increased by cyclic intravenous pamidronate. J Clin Endocrinol Metab. 1998;83:2324–2330. doi: 10.1210/jcem.83.7.4782. [DOI] [PubMed] [Google Scholar]
- 9.Heijckmann AC, Huijberts MS, Geusens P, de Vries J, Menheere PP, Wolffenbuttel BH. Hip bone mineral density, bone turnover and risk of fracture in patients on long-term suppressive L-thyroxine therapy for differentiated thyroid carcinoma. Eur J Endocrinol. 2005;153:23–29. doi: 10.1530/eje.1.01933. [DOI] [PubMed] [Google Scholar]
- 10.Mikosch P, Jauk B, Gallowitsch HJ, Pipam W, Kresnik E, Lind P. Suppressive levothyroxine therapy has no significant influence on bone degradation in women with thyroid carcinoma: a comparison with other disorders affecting bone metabolism. Thyroid. 2001;11:257–263. doi: 10.1089/105072501750159679. [DOI] [PubMed] [Google Scholar]
- 11.Reverter JL, Colome E, Holgado S, Aguilera E, Soldevila B, Mateo L, et al. Bone mineral density and bone fracture in male patients receiving long-term suppressive levothyroxine treatment for differentiated thyroid carcinoma. Endocrine. 2010;37:467–472. doi: 10.1007/s12020-010-9339-z. [DOI] [PubMed] [Google Scholar]
- 12.Sugitani I, Fujimoto Y. Effect of postoperative thyrotropin suppressive therapy on bone mineral density in patients with papillary thyroid carcinoma: a prospective controlled study. Surgery. 2011;150:1250–1257. doi: 10.1016/j.surg.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Quan ML, Pasieka JL, Rorstad O. Bone mineral density in well-differentiated thyroid cancer patients treated with suppressive thyroxine: a systematic overview of the literature. J Surg Oncol. 2002;79:62–69. doi: 10.1002/jso.10043. [DOI] [PubMed] [Google Scholar]
- 14.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, et al. Study of Osteoporotic Fractures Research Group. Risk factors for hip fracture in white women. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 15.Nicholls JJ, Brassill MJ, Williams GR, Bassett JH. The skeletal consequences of thyrotoxicosis. J Endocrinol. 2012;213:209–221. doi: 10.1530/JOE-12-0059. [DOI] [PubMed] [Google Scholar]
- 16.Vestergaard P, Mosekilde L. Hyperthyroidism, bone mineral, and fracture risk: a meta-analysis. Thyroid. 2003;13:585–593. doi: 10.1089/105072503322238854. [DOI] [PubMed] [Google Scholar]
- 17.Svare A, Nilsen TI, Bjoro T, Forsmo S, Schei B, Langhammer A. Hyperthyroid levels of TSH correlate with low bone mineral density: the HUNT 2 study. Eur J Endocrinol. 2009;161:779–786. doi: 10.1530/EJE-09-0139. [DOI] [PubMed] [Google Scholar]
- 18.Leese GP, Jung RT, Guthrie C, Waugh N, Browning MC. Morbidity in patients on L-thyroxine: a comparison of those with a normal TSH to those with a suppressed TSH. Clin Endocrinol (Oxf) 1992;37:500–503. doi: 10.1111/j.1365-2265.1992.tb01480.x. [DOI] [PubMed] [Google Scholar]
- 19.Melton LJ, 3rd, Ardila E, Crowson CS, O'Fallon WM, Khosla S. Fractures following thyroidectomy in women: a population-based cohort study. Bone. 2000;27:695–700. doi: 10.1016/s8756-3282(00)00379-3. [DOI] [PubMed] [Google Scholar]
- 20.Abe E, Marians RC, Yu W, Wu XB, Ando T, Li Y, et al. TSH is a negative regulator of skeletal remodeling. Cell. 2003;115:151–162. doi: 10.1016/s0092-8674(03)00771-2. [DOI] [PubMed] [Google Scholar]
- 21.Sampath TK, Simic P, Sendak R, Draca N, Bowe AE, O'Brien S, et al. Thyroid-stimulating hormone restores bone volume, microarchitecture, and strength in aged ovariectomized rats. J Bone Miner Res. 2007;22:849–859. doi: 10.1359/jbmr.070302. [DOI] [PubMed] [Google Scholar]
- 22.Bassett JH, O'Shea PJ, Sriskantharajah S, Rabier B, Boyde A, Howell PG, et al. Thyroid hormone excess rather than thyrotropin deficiency induces osteoporosis in hyperthyroidism. Mol Endocrinol. 2007;21:1095–1107. doi: 10.1210/me.2007-0033. [DOI] [PubMed] [Google Scholar]
- 23.Bassett JH, Williams AJ, Murphy E, Boyde A, Howell PG, Swinhoe R, et al. A lack of thyroid hormones rather than excess thyrotropin causes abnormal skeletal development in hypothyroidism. Mol Endocrinol. 2008;22:501–512. doi: 10.1210/me.2007-0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsai JA, Janson A, Bucht E, Kindmark H, Marcus C, Stark A, et al. Weak evidence of thyrotropin receptors in primary cultures of human osteoblast-like cells. Calcif Tissue Int. 2004;74:486–491. doi: 10.1007/s00223-003-0108-3. [DOI] [PubMed] [Google Scholar]


