Abstract
Purpose
In recent years, many psychological problems in patients with stomas have been addressed in a number of studies. But there are only a few studies that use objective measures to take into account self-appraisal by patients with permanent or temporary stomas. The aim of this study is to compare the psychological attitude of patients with permanent and temporary stomas and to determine the most appropriate psychological supportive care.
Methods
Sixty-five patients, who received a stoma between January 2009 and March 2012, were classified into two groups with either permanent or temporary stomas and were observed prospectively. We developed a questionnaire with the aid of a psychiatrist to analyze the grade of psychological attitude of self-appraisal of patients. The questionnaire was categorized into three parts; body image scale, self-esteem scale, and depression scale. Patients responded to the questionnaire 4 weeks after the operation and the answers of each group were compared.
Results
Out of 65 patients, 42 received temporary stomas and 23 received permanent stomas. There was no significant mean difference between permanent and temporary stoma patients in the body image scale, the self-esteem scale, and the depression scale. However, patients with a permanent stoma tended to have a worse body image and lower self-esteem on some specific items within the questionnaires.
Conclusion
Patients with stomas have negative attitudes toward themselves and some meaningful differences were found between different types of stoma applied. Surgeons should be concerned about postoperative psychological support for patients with stomas.
Keywords: Ostomy, Body image, Self esteem, Depression
INTRODUCTION
Stomas are generally known as an evacuation organ made with parts of the large or small intestine through the abdominal wall. It is needed to evacuate stool when it is difficult to maintain the continuity of the intestines due to congenital or acquired diseases and accidents. The psychological and emotional problems of patients with stomas, and its adverse effects on patients, have been discussed and reported for a long time [1-15]. Because stomas are known to adversely affect patients' quality of life (QoL), ways to reduce the necessity of stomas are constantly sought [1,2]. Nevertheless, it is still carried out in many patients due to the location of tumor, types of operations, complications and safety.
According to Ross et al. [1], patients with stomas express aspects of a more negative body image and dim future perspectives, lower social functioning, and a higher reported level of depression than in patients without stomas. Also, their QoL was found to worsen throughout the duration of the study. In addition, according to Gervaz et al. [2], patients with permanent stomas who had undergone abdominoperineal resection (APR) had their general QoL improved, but their body image and stoma-related problems were only slightly improved after 1 year. That is, even after physical problems like pain or fatigue disappeared due to the operation, the adverse effects of the stoma do not diminish with time. On the other hand, Tsunoda et al. [3] studied QoL of patients who underwent colectomy with temporary ileostomy. The article reported that patients with temporary ileostomy have declining physical functions and ability to perform regular activities, as well as worsening QoL. Thus, repairing the stoma was found to improve general QoL. Engel et al. [4] also reported declined emotional expression and ability to perform regular activities in patients with stomas, but these scales improved after repair of the stoma.
The consensus is clear about the adverse effect of stomas on patients. However, surgeons tend to think that a temporary stoma can be repaired relatively simply and, therefore, QoL or lifestyle of patients with stomas would recover easily. Therefore, surgeons perform their main operation plus a temporary stoma only for the purpose of 'prevention' of anastomotic leakage, and this tendency is relatively increasing while frequency of APR is decreasing in very low rectal cancer [1,2].
Some studies report that body image or QoL of patients with temporary stomas recover after repair of the stoma. The question is whether the QoL of patients with temporary stomas is better than that of patients with permanent stomas, primarily because of the expectation that the stoma can be easily repaired.
Previous studies have only focused on comparing patients with and without stomas, or before and after the stoma-repair. There has been no comparison study on temporary stomas that could be repaired, and permanent stomas that cannot be repaired. Therefore, this study presupposed that patients with temporary stomas would show better self-esteem appraisal than patients with permanent stomas. Patients with stomas were evaluated on the scales of body image, self-esteem, and depressive mood. Based on these results, proper support therapy was attempted to be determined according to the characteristics of each patient.
METHODS
Patients
Patients who received stomas in the Department of General Surgery from 2009 to 2012 were enrolled and informed consents were obtained. There were no restrictions on the diagnosis of patients, while patients with a previous psychological history and/or lacking the ability to comprehend to questionnaires were excluded.
Patients were classified into two groups as either permanent stoma group (PS group) or temporary stoma group (TS group).
Methods
Institutional Review Board
Prior to the study, we submitted our research plans, consent forms, and questionnaires to the institutional review board for deliberation and all received official approval.
Questionnaires
A psychiatrist at our institution was employed to digitize and measure the level of body image, self-esteem, and depressive mood, and to make the questionnaires form revised to suit Korean patients. Details of the questionnaires are as follows.
Body image scale: This questionnaire is a tool by which patients measure their own body image. There are a total of 15 questions, and each item measures two opposed ideas in 7-grades. The lowest score is 15 points and the highest is 105 points. Positive items like question 1, 2, 5, 6, 7, 11, 13 and 15, are calculated adversely, and question 9 is also calculated adversely in male patients. A higher total score means a more positive attitude to one's own body image (Supplementary material 1).
Self-esteem scale: This tool measures the level of self-respect or self-approval. There are a total of 10 questions, five are related to positive self-esteem with the other five related to negative self-esteem. Each item is measured by a 4-grade method, the lowest score is 10 points and the highest is 40 points. The questions related with negative self-esteem, like question 3, 5, 8, 9, 10, are calculated adversely. A higher total score means higher self-esteem (Supplementary material 2).
Beck Depression inventory: This is based on clinical symptoms of depressive mood and checks the type or degree of depression. There are a total of 21 questions that can be categorized into emotional, cognitive, motivational, and physiological syndromes. It is scored by a 4-grade method, from 0 to 3, with the lowest score at 0 points and the highest at 63 points. The range from 0 to 9 points means a normal state, from 10 to 15 means a mild depressive mood, from 16 to 23 points means moderate, and from 24 to 63 means severe (Supplementary material 3).
Follow-up
Questionnaires were obtained from patients 4 weeks after the stoma operation. There were no differences in postoperative progress, course of routine examination, progress of diet and determination of discharge plan between patients who were enrolled in the study and those who were not. Patients who were discharged from hospital earlier than 4 weeks answered the questionnaire at the outpatient department after similar periods.
Statistical analysis
Statistical analysis was performed with PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA). Numerical data, such as age or scale score, were represented as 'mean ± standard deviation', and the data of patient characteristics were analyzed with chi-square test. A comparison of the average of the two groups (for example, permanent stoma and temporary stoma, male patients and female patients, benign disease group and malignant disease group) was performed using Student t-test. And a comparison of the average between more than three groups (for example, economic status, academic status, stage of malignant disease, etc.) was performed using one-way analysis of variance or Kruskal-Wallis nonparametric test. It was considered as statistically significant when P-value was less than 0.05.
RESULTS
A total of 65 patients were analyzed, 44 (67.7%) were male and 21 (32.3%) were female. Mean age was 57.5 ± 13.9 years old. Out of 65 patients, 23 had permanent stomas (35.4%), and 42 had temporary stomas (64.6%) (Table 1).
Table 1.
Demographic and social characteristics of patients in study
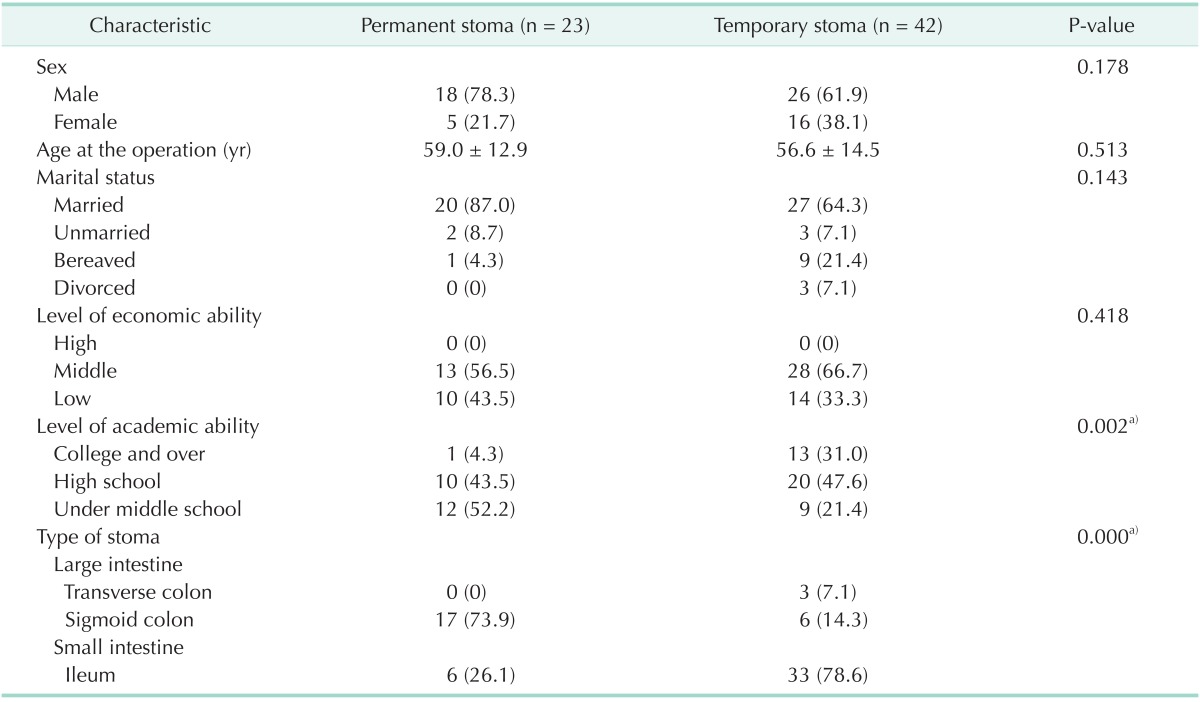
Values are presented as number (%) or mean ± standard deviation.
a)P < 0.05.
Seven patients had undergone the operation due to benign diseases, such as Crohn disease, ulcerative colitis, postoperative intestinal obstruction, and colon perforation. All of these 7 patients with benign disease showed resolution of disease. All the other participants were diagnosed with malignant diseases. Most of them were adenocarcinoma of the colon or rectum, one was mucinous carcinoma of the colon, two were ovarian cancer, and one was malignant lymphoma. Between PS group and TS group, frequency of malignant diseases was not statistically different (P = 0.474). Also, there was no difference in TNM stage (American Joint Committee on Cancer 7th edition) of colorectal adenocarcinoma between the two groups (P = 0.231). Among the patients with malignant disease, 20 patients showed progression of the disease, where 10 patients were in PS group while the other 10 patients were in TS group (Table 2).
Table 2.
Classification and follow-up results of diseases
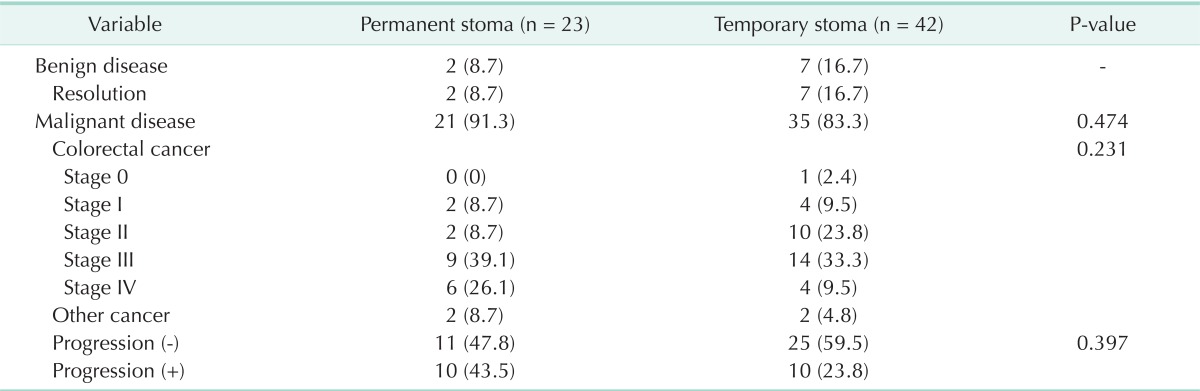
Values are presented as number (%).
Types of operations were significantly different between PS group and TS group (P = 0.000). About 65% of PS group had undergone APR, whereas about 60% of TS group had undergone lower anterior resection (LAR) with loop ileostomy, and about 10% had undergone Hartmann's operation. However, frequency of perioperative radiotherapy and chemotherapy was not statistically different (Table 3).
Table 3.
Types of treatments
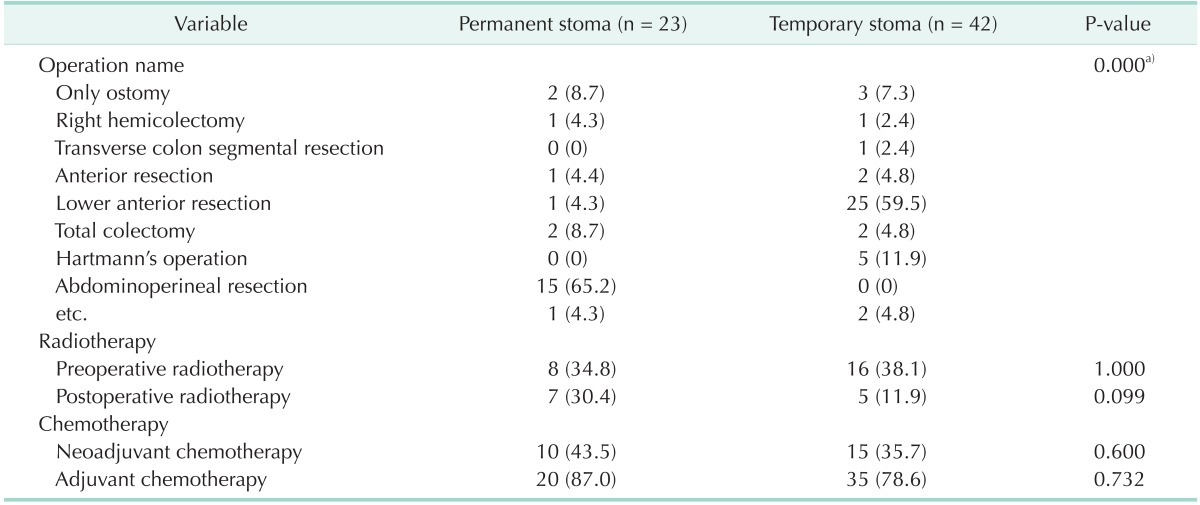
Values are presented as number (%).
a)P < 0.05.
There were a total of 8 cases of stoma-related complications, 2 cases were observed in PS group and 6 cases in TS group. There was no significant difference between the two groups (Table 4).
Table 4.
Stoma-related complications
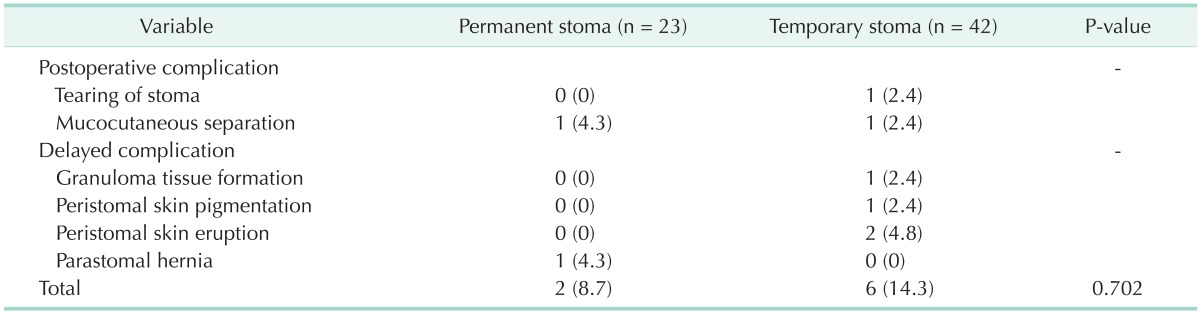
Values are presented as number (%).
Body image scale and self-esteem scale appeared to be lower in both groups than in control, and Beck Depression Inventory (BDI) showed that both groups had more depressive moods. However, there were no significant differences. The mean body image scale was 63.3 ± 15.5 points, and there was no significant difference in body image scale according to age, economic status, academic status, diagnosis, and type of operation. Mean of self-esteem scale was 28.7 ± 4.2 points, and patients without partner, for example, unmarried, divorced or bereaved, showed the tendency for a lower score but was not statistically significant. Lastly, the mean score of BDI was 13.7 ± 8.8 points and patients with stomas showed more depressive moods than the general population. It was found that the lower the economic status of the patients, the higher the BDI score was (P = 0.013) (Table 5).
Table 5.
Mean psychological scale scores to self-appraisal on various variables
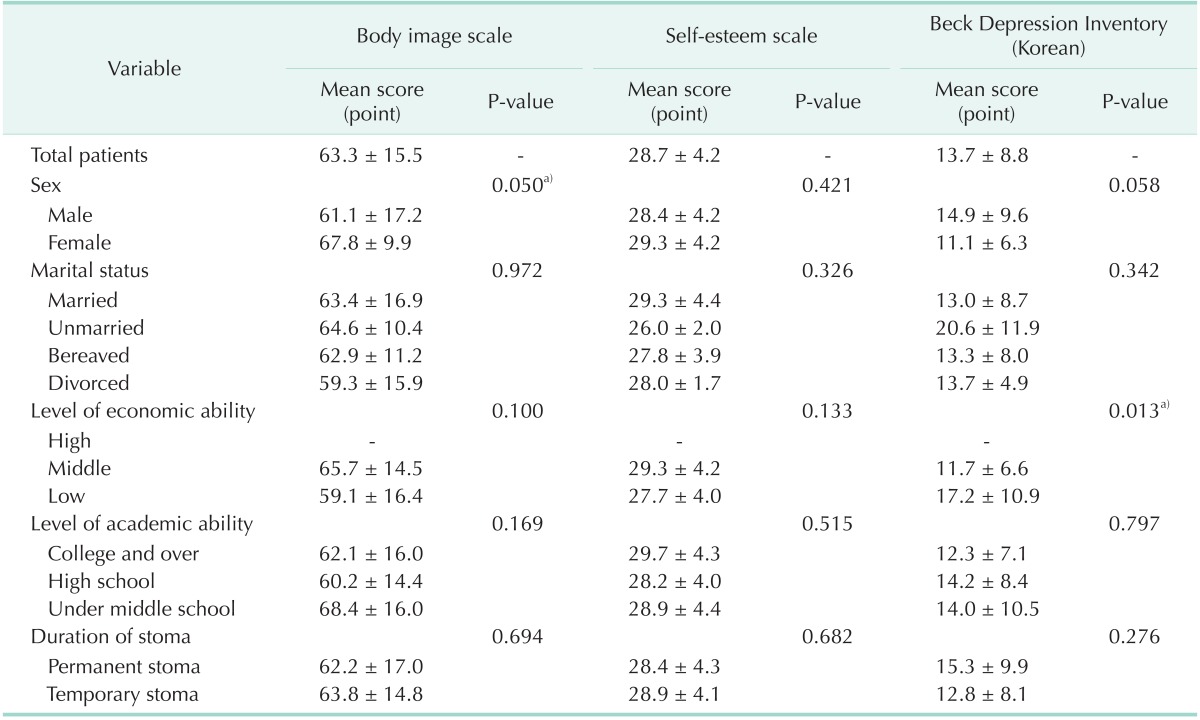
Values are presented as mean ± standard deviation.
a)P < 0.05.
The questionnaires for body image, self-esteem, and BDI were analyzed item by item, but no item showed significant difference. Every item of BDI was also analyzed and compared between PS group and TS group. PS group tended to feel 'guilty' (P = 0.017), and experienced a decrease in sexual interest (P = 0.010). Also, PS group answered more negatively to the statement 'I hate myself' than TS group, but there was no statistical meaning (P = 0.056) (Table 6).
Table 6.
Results of psychological scale scores to self-appraisal in permanent stoma group versus temporary stoma group
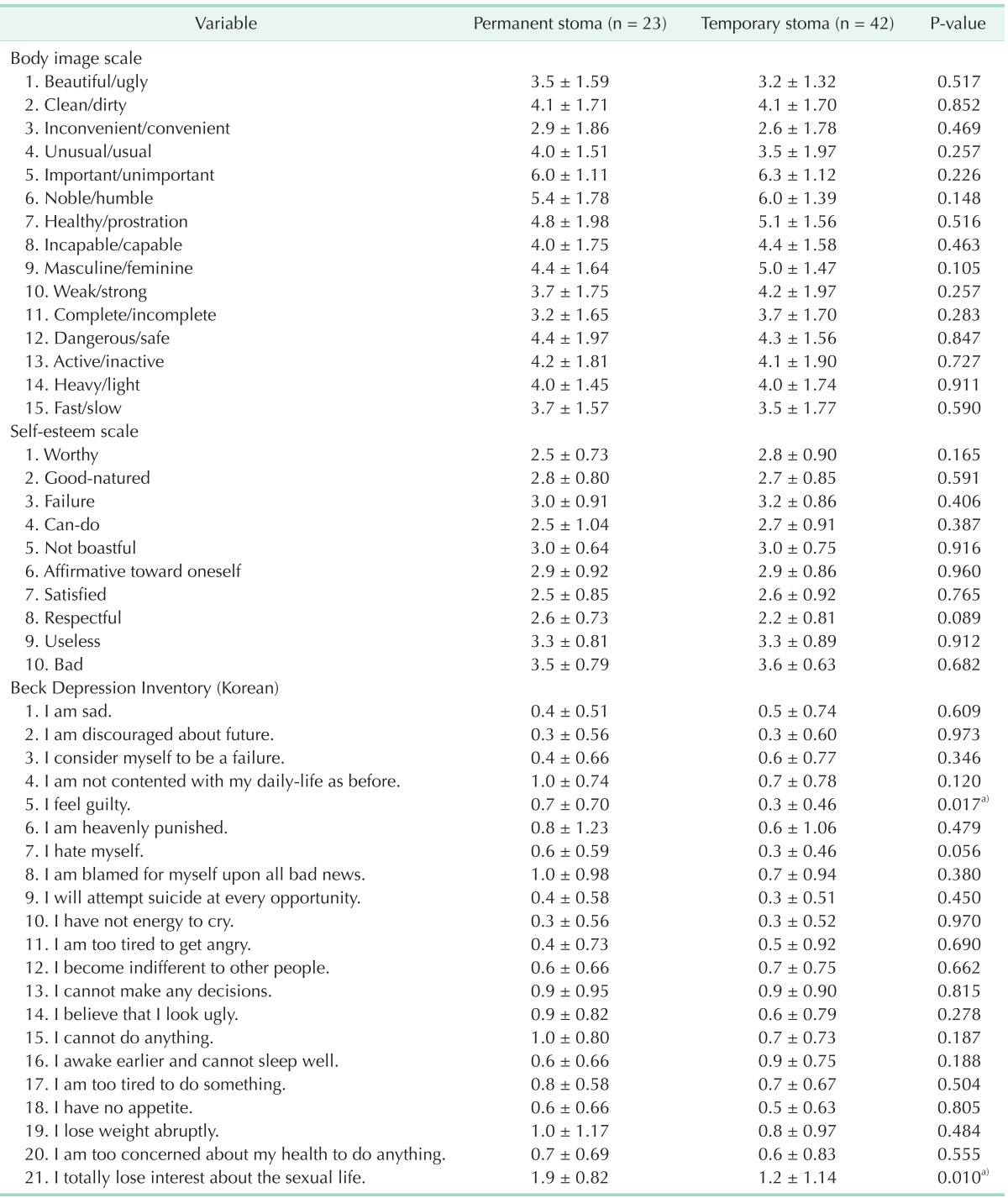
Values are presented as mean ± standard deviation.
a)P < 0.05.
Three scales were analyzed based on sex. In the results of the body image scale, males answered that they thought themselves unimportant (P = 0.006), humble (P = 0.016), incapable (P = 0.023), and less masculine (P=0.042). There was no difference between male and female in the results of the self-esteem scale. And in the results of the BDI, males answered that they felt themselves as a 'failure' (P = 0.000), being punished by Heaven (P = 0.016) could not feel satisfied with daily-life (P = 0.002), and also could not sleep well (P = 0.042) (Table 7).
Table 7.
Results of psychological scale scores to self-appraisal in male versus female
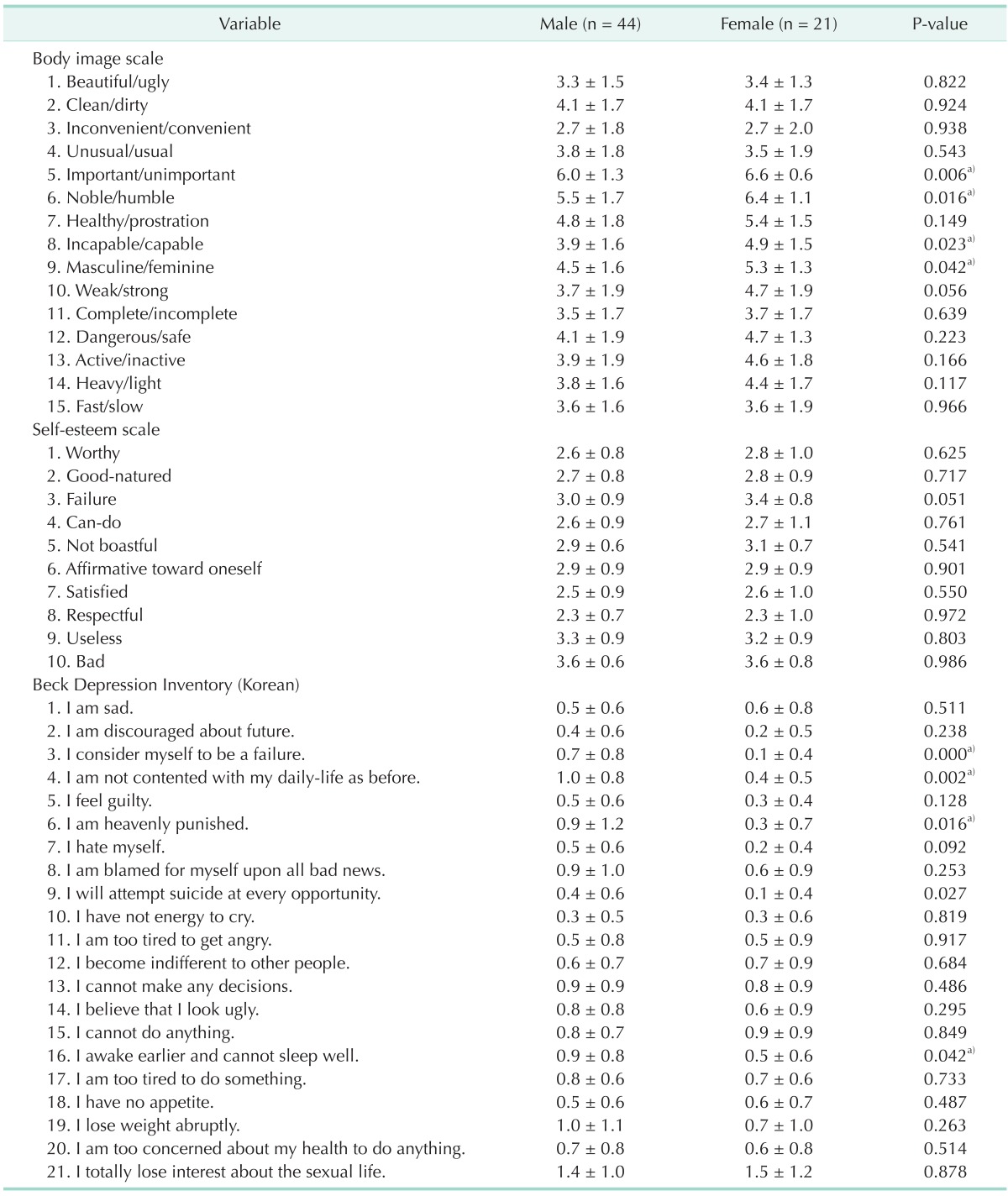
Values are presented as mean ± standard deviation.
a)P < 0.05.
DISCUSSION
Stomas have negative effects on psychological or emotional conditions of patients. In this study, patients with stomas present a lower level of body image scale and self-esteem scale (63.3 ± 15.5, 28.7 ± 4.2) and a higher level of depressive moods. Although the results are not statistically significant, patients without partners, such as unmarried, divorced or bereaved patients, have a tendency to show worse self-esteem. Patients with stomas have a mean BDI of 13.7 ± 8.8, which could be interpreted as having a 'mild' depressive mood. Also, the lower the socioeconomic level, the higher the level of depressive mood (P = 0.013) (Table 5). Psychological and emotional conditions of patients were affected by not only the presence of the stoma, but also the 'social status' or 'economic level.'
Analyzing each item according to sex, male patients feel themselves unimportant, humble, and less masculine. As well, they are not satisfy with their daily-life, cannot sleep well or wake up early. They even think of themselves as failures or being punished by a higher power (P < 0.05) (Table 7). Therefore, these results favor the idea that compliance of stomas is lower in males than females.
Previous studies have reported that chemotherapy or radiotherapy might have numerous influences on the QoL of patients with stomas, symptoms presenting maximally within 1 year after operation [2]. But in this study, conducting chemotherapy or radiotherapy in patients diagnosed with malignant diseases is not related with psychological or emotional conditions. Nevertheless, diagnosis of patients, benign or malignant, progression of disease, also does not affect the results of questionnaires.
However, because of the possibility of stoma repair, it is predicted that the reluctance of patients with stomas must be different dependent on the type of stoma, permanent or temporary. So, each item, body image, self-esteem, and BDI in the questionnaire, is analyzed according to the type of stoma.
QoL of patients with stomas has been studied for a long time. Gervaz et al. [2] have reported that body image, sexual dysfunction and many problems related to stoma in patients who underwent APR, do not improve even after 1 year. In this study, patients with a permanent stoma, for example, patients who underwent APR, also represent lower scores in body image scale and self-esteem scale (62.2 ± 17.0 points, 28.4 ± 4.3 points), and 'moderate' depressive mood in BDI, 15.3 ± 9.9 points (Table 5).
Furthermore, patients with permanent stomas tend to feel more guilty and be less interested in sex than patients with temporary stomas (P < 0.05). Actually, the frequency of APR in PS group is more than 65%, and the decrease in interest in sex could be considered as a complication of APR [1,2]. Likewise, there is no significant difference in total score of body image, self-esteem, and BDI between PS group and TS group (Table 5), though there is a significant difference in each item between the two groups (Table 6).
For the last 20 years, there has been a trend in operation of very low rectal cancer due to the development of techniques and instruments of operations, that frequency of APR operation is decreasing relative to that of LAR, which is increasing in frequency; thus QoL of patients is also being improved [5,6]. However, this fact brings about the result that frequency of LAR with loop ileostomy is rather increased [7-9].
Temporary stoma is performed as a preliminary operation as an emergency measure of anastomotic leakage after colorectal surgery, for the patency of the lumen, and for depression of intestines. Surgeons tend to consider that repairing temporary stomas is a simple technique, thus they readily perform the stoma operation for prevention of anastomotic leakage or severe peritonitis, as recommended in LAR with loop ileostomy initially [6,8,9].
As with the results of other studies that use research on patients with temporary stoma [3,10], in this study, patients with temporary stomas represent lower levels of body image scale and self-esteem scale; 63.8 ± 14.8 points and 28.9 ± 4.1 points, and show 'mild' depressive mood, 12.8 ± 8.1 points.
Temporary stomas can be recovered within 1 year, except in special cases. So, the negative influence of the stoma could be predicted to decrease due to the expectation of stoma repair. But in this research, the results of patients with and without stomas does not indicate significant differences. These results imply how the psychological stress of stomas is great and severe. Even if the patient knows that a repair of the stoma is possible, the stoma itself affects negatively on body image, self-esteem, and mood.
Comparing before and after stoma repair, one study reported that the ability of physical function and role function became worse despite general QoL improvement [3]. Other research showed that items of body image or activity were improved but general QoL had not changed, and even gastrointestinal problems were found to have been increased [10].
Therefore, patients with stomas, even for short durations, need to be educated accurately about the many problems related with stomas. It is necessary to support the patients with not only permanent stomas but also temporary stomas through psychiatric consultations.
As mentioned above, male patients have worse compliance toward stomas than female patients (Table 7). So, intensity of psychiatric influence of stomas varies according to sex or type of stoma; patient-customized counsel needs to be implemented.
According to one study, the cases in which stoma operation was performed additionally after main operation due to complications have more problems than the cases where stoma operation and main operation were performed at same time [1]. However, there are no significant differences between chronological order of stoma operation and main operation on the body image scale or self-esteem scale, or BDI. Thus, it is not desirable to perform a stoma operation initially with the main operation for prevention of anastomotic leakage.
Above all, surgeons should have good judgment when conducting the stoma operation. Although repair of stoma is considered as a relatively simple procedure to surgeons, the stoma itself could be a huge stress to patients physically or emotionally, even over short durations. Thus, surgeons must perform the stoma operation selectively on a limited number of patients when determined to be absolutely necessary.
Meanwhile, there are some limitations in this study. First, the number of enrolled patients was insufficient. There was likely to be bias involved because the number of patients was small in each group. But there were no differences between the two groups in demographic characteristics, diagnosis, stoma-related complications, and so on. Therefore, we believe that the results of this study represent much to surgeons when deciding to perform stoma surgery. Second, the biggest disadvantage of this study was that diagnosis of patients was not controlled. Most of the enrolled patients were diagnosed with malignant diseases and have suffered from pain of cancer, depressive mood, chemotherapy and radiotherapy. Their QoL has also already declined, although there were no significant differences between PS group and TS group. In other words, the presence of malignant disease, having had perioperative chemotherapy or radiotherapy, and having different prognosis might change the psychiatric or emotional conditions of patients. Third, according to the type of operation, parts or length of residual bowel and resected organs differed, as well as the postoperative pain and bowel habit that might change the QoL of patients. Fourth, types of stoma were not controlled. As a result, most patients of PS group had colostomy, especially sigmoid colostomy, and most patients of TS group had ileostomy. Although there was no statistical difference, stoma-related complications, which affected patients with ileostomy more, like parastomal skin eruption, showed more often in TS group. The results did not pan out as expected by its design. Therefore, further evaluation with a greater number of patients with controlled diagnosis and operations is needed.
Unlike the initial presumption, body image scale, self-esteem scale and BDI did not show significant differences between PS group and TS group. Therefore, in deciding the method of operation, surgeons should conduct circumspection in performing temporary stomas. Patients who have temporary stomas that can be repaired within 6 months or 1 year should take counseling related with psychiatric or emotional problems. Also, surgeons must be conscious of this fact and be concerned with stoma patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
This paper was presented at the 13th Korea-Japan-China Colorectal Cancer Symposium, September 8th-9th, 2012.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via http://thesurgery.or.kr/src/sm/astr-86-152-s001.pdf.
Body image scale
Self-esteem scale
Beck Depression Inventory (Korean version)
References
- 1.Ross L, Abild-Nielsen AG, Thomsen BL, Karlsen RV, Boesen EH, Johansen C. Quality of life of Danish colorectal cancer patients with and without a stoma. Support Care Cancer. 2007;15:505–513. doi: 10.1007/s00520-006-0177-8. [DOI] [PubMed] [Google Scholar]
- 2.Gervaz P, Bucher P, Konrad B, Morel P, Beyeler S, Lataillade L, et al. A prospective longitudinal evaluation of quality of life after abdominoperineal resection. J Surg Oncol. 2008;97:14–19. doi: 10.1002/jso.20910. [DOI] [PubMed] [Google Scholar]
- 3.Tsunoda A, Tsunoda Y, Narita K, Watanabe M, Nakao K, Kusano M. Quality of life after low anterior resection and temporary loop ileostomy. Dis Colon Rectum. 2008;51:218–222. doi: 10.1007/s10350-007-9101-7. [DOI] [PubMed] [Google Scholar]
- 4.Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Holzel D. Quality of life in rectal cancer patients: a four-year prospective study. Ann Surg. 2003;238:203–213. doi: 10.1097/01.sla.0000080823.38569.b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Audisio RA, Filiberti A, Geraghty JG, Andreoni B. Personalized surgery for rectal tumours: the patient's opinion counts. Support Care Cancer. 1997;5:17–21. doi: 10.1007/BF01681957. [DOI] [PubMed] [Google Scholar]
- 6.Nicholls RJ, Hall C. Treatment of non-disseminated cancer of the lower rectum. Br J Surg. 1996;83:15–18. doi: 10.1002/bjs.1800830105. [DOI] [PubMed] [Google Scholar]
- 7.Karanjia ND, Corder AP, Holdsworth PJ, Heald RJ. Risk of peritonitis and fatal septicaemia and the need to defunction the low anastomosis. Br J Surg. 1991;78:196–198. doi: 10.1002/bjs.1800780221. [DOI] [PubMed] [Google Scholar]
- 8.Marusch F, Koch A, Schmidt U, Geibetaler S, Dralle H, Saeger HD, et al. Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum. 2002;45:1164–1171. doi: 10.1007/s10350-004-6384-9. [DOI] [PubMed] [Google Scholar]
- 9.Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H, et al. Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg. 2005;92:1137–1142. doi: 10.1002/bjs.5045. [DOI] [PubMed] [Google Scholar]
- 10.Siassi M, Hohenberger W, Losel F, Weiss M. Quality of life and patient's expectations after closure of a temporary stoma. Int J Colorectal Dis. 2008;23:1207–1212. doi: 10.1007/s00384-008-0549-2. [DOI] [PubMed] [Google Scholar]
- 11.Jess P, Christiansen J, Bech P. Quality of life after anterior resection versus abdominoperineal extirpation for rectal cancer. Scand J Gastroenterol. 2002;37:1201–1204. doi: 10.1080/003655202760373425. [DOI] [PubMed] [Google Scholar]
- 12.Pachler J, Wille-Jorgensen P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev. 2005;(2):CD004323. doi: 10.1002/14651858.CD004323.pub3. [DOI] [PubMed] [Google Scholar]
- 13.Camilleri-Brennan J, Steele RJ. Objective assessment of morbidity and quality of life after surgery for low rectal cancer. Colorectal Dis. 2002;4:61–66. doi: 10.1046/j.1463-1318.2002.00300.x. [DOI] [PubMed] [Google Scholar]
- 14.Camilleri-Brennan J, Steele RJ. Prospective analysis of quality of life after reversal of a defunctioning loop ileostomy. Colorectal Dis. 2002;4:167–171. doi: 10.1046/j.1463-1318.2002.00352.x. [DOI] [PubMed] [Google Scholar]
- 15.Lee GG, Chang HW, Kim JH, Chung KS. Complications of Colostomy. J Korean Surg Soc. 1997;53:670–675. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Body image scale
Self-esteem scale
Beck Depression Inventory (Korean version)


