Abstract
Since its initial description, a number of studies have described the use of microvolt T-wave alternans (MTWA) as a predictor of the primary or secondary occurrence of ventricular arrhythmic events. These studies, however, have been limited by small sample sizes and disparate patient populations. Studies of MTWA in post-myocardial infarction (MI) patients are few in number, but hold predictive value for risk of ventricular arrhythmias. We performed a study of MTWA in post-myocardial infarction patients to clarify the predictive accuracy and usefulness of MTWA compared to other invasive and non-invasive techniques. We enrolled 120 patients (74 men, 46 women, mean age 62.3 ± 15.2 years in men, and 64.2 ± 13.8 years in women) with a history of myocardial infarction but no prior sustained ventricular arrhythmias. Patients were assessed by echocardiography, Holter, signal averaged ECG, MTWA, and electrophysiology study. Mean follow-up was 14 months. The MTWA test had a good negative predictive value for arrhythmic events in post-MI patients and can be used for risk stratification. We consider that in patients with positive MTWA further invasive evaluation, respectively electrophysiology study, is necessary.
Keywords: risk stratification, sudden death, T-wave alternans, ventricular arrhythmias
Introduction
Microvolt-level electrical alternans of the T-wave (MTWA) was first reported in 1981 in a series of papers by Adam, Cohen and co-authors [1-6]. The papers reported the presence of microvolt-level alternation in T-wave amplitude during atrial pacing in animals following interventions that increased susceptibility to ventricular arrhythmias. In 1988, Smith et al. [6] reported on a Spectral Method for detecting microvolt-level alternans that is sensitive to any morphological pattern of alternation in the T-wave. Smith et al. used this technique to demonstrate a relationship between MTWA and ventricular fibrillation threshold in animal studies. Smith et al. also reported a statistically significant association of electrical alternans with inducibility of sustained ventricular tachycardia in 19 patients undergoing electrophysiology testing.
In 1994, in a study of 83 patients, Rosenbaum et al. [7] demonstrated a highly significant relationship between electrical alternans measured during atrial pacing, and inducibility of sustained ventricular tachycardia (VT) or ventricular fibrillation (VF). The same study also showed strong correlation between MTWA and 20-month arrhythmia-free survival.
In 1997, Hohnloser et al [8] demonstrated that MTWA can be reliably assessed during non-invasive exercise stress. The study showed 84% concordance of the presence of MTWA both during exercise and atrial pacing in 30 patients. Also in 1997, Klingenheben et al. [9] presented evidence relating MTWA and arrhythmia recurrence in 65 patients with an implantable cardioverter defibrillator (ICD). All patients underwent invasive electrophysiology study (EPS) and non-invasive risk stratification including microvolt T-wave alternans. T-wave alternans was a significant predictor of appropriate ICD firings with a sensitivity of 80% and positive predictive value of 50%. In this study, T-wave alternans was superior to EPS in predicting recurrent VT/VF. In a third study, Caref et al. [10] demonstrated that alternans is rare in normal control subjects, age-matched to typical VT/VF patients. Fewer than 2% of patients were MTWA positive with onset below 70% of maximum predicted heart rate in a group of 79 healthy controls.
In a multi-center clinical study consisting of 337 consecutive patients referred for electrophysiology (EP) study, microvolt T-wave alternans (MTWA) was measured during submaximal bicycle exercise. Actuarial arrhythmia-free survival of MTWA+ was 0.8117 and of MTWA- was 0.9828 (Risk Ratio 10.9; [p=0.002]). Actuarial arrhythmia-free survival of EP+ was 0.7643 and of EP- was 0.9667 (Risk Ratio 7.07; [p<0.001]) [11].
The ability of MTWA to predict the induction of sustained monomorphic VT during programmed stimulation was determined in a subset of 140 patients. MTWA predicted EP outcome with a sensitivity of 76% and specificity of 65% (p<0.0001).
Microvolt T-wave alternans testing is useful in the prediction of ventricular tachyarrhythmic events; however, there are significant limitations to its use. The predictive value of MTWA varies significantly depending on the disease substrate. The incremental prognostic value of MTWA when used with other methods of risk stratification is unclear [12].
We performed this study of MTWA in post-myocardial infarction patients to clarify the predictive accuracy and usefulness of MTWA compared to other invasive and non-invasive techniques.
Matherial and Methods
Patient population
This prospective study enrolled 120 patients (74 men, 46 women, mean age 62.3 ± 15.2 years in men, and 64.2 ± 13.8 years in women) with a history of myocardial infarction but no prior sustained ventricular arrhythmias.
Inclusion criteria were:
- Male or female, aged 18 years or more at inclusion;
- History of myocardial infarction (based on the clinical course, serum marker activity and on electrocardiogram) – at least one month ago;
- In sinus rhythm;
- In stable condition (for at least one month) with regards to symptoms (angina) and on appropriate and stable doses (for at least one month) of conventional cardiovascular medications.
Non-inclusion criteria were:
- Unlikely to cooperate in the study;
- Legal incapacity or limited legal incapacity;
- Class III-IV NYHA chronic heart failure;
- Patient unable to complete a stress test or with contraindication for atrial pacing.
Written informed consent was obtained from each patient at the screening visit; then each participant underwent a screening interview. Based on it, subjects were declared eligible to proceed if all inclusion criteria were fulfilled and no exclusion criteria were met. This study was approved by the Institutional Ethics Committee of Craiova Cardiology Center. It is also in agreement with Helsinki Declaration from 1975, which was revised in 1983.
Patient assessment
Echocardiography
Left ventricular ejection fraction (LVEF) was assessed by modified Simpson rule on echocardiography (HP Sonos 5500, 2.5-4 MHz transducer, with simultaneous ECG monitoring).
Holter
Ambulatory 24 hour ECG recordings were obtained using a commercial device (Zymed). We analyzed the presence of sustained or unsustained ventricular arrhythmia, and heart rate variability in the time domain (SDNN, SDANN5, RMSSD).
SAECG
Signal averaged ECGs were recorded with General Electric MAC 5500; target noise level was < 0.7 μV. Late ventricular potentials were considered to be present if filtered QRS duration > 114 ms, HFLA > 38 ms, and RMS40 < 20μV.
MTWA testing
Microvolt T wave alternans test was performed using a HearTwave II system (Cambrige Heart, Inc.) during bicycle exercise or during atrial pacing. In order to minimize the noise, skin preparation and high resolution electrodes were used. Electrocardiographic leads were placed at standard 12-lead positions and in orthogonal X, Y, Z configuration.
The MTWA test was interpreted as positive, negative or indeterminate:
- Positive: A test is positive if it has sustained alternans with an Onset Heart Rate ≤ 110 bpm (or has sustained alternans at the resting heart rate).
- Negative: A test is negative if it does not have sustained alternans with an Onset HR ≤ 110 bpm and the Maximum Negative HR is ≥ 105 bpm.
- Indeterminate: A test is indeterminate if it does not have an Onset HR ≤ 110 bpm or a Maximum Negative HR ≥ 105 bpm.
Sustained alternans is defined as alternans that is consistently present over a patient-specific heart rate threshold (except for gaps believed to be caused by obscuring factors such as ectopics, noise or HR dips).
- With at least 1 minute of Valt ≥ 1.9 μV and alternans ratio ≥ 3.
- In any of leads VM, X, Y, Z or in 2 adjacent precordial leads.
- With some period of artifact-free data (defined below and indicated on alternans trends by a black line on the time axis).
Electrophysiological study
After local anesthesia using lidocaine 1%, one electrode catheter was inserted percutaneously through the subclavian vein and advanced to the high lateral right atrium, across the tricuspid valve, and to the right apex in all patients.
Programmed ventricular stimulation was performed using stimulus duration of 2-ms at amplitude of two to three times the diastolic threshold, with up to three extrastimuli at basic drive cycle lengths, 600 ms and 400 ms respectively, starting at apex, then at outflow tract. Coupling intervals of extrastimuli were decreased in 10-ms interval until coupling interval of 180 ms was reached or refractoriness of all extrastimuli was reached.
The endpoint was the induction of sustained ventricular tachycardia (< 30 s in duration or associated with hemodynamic compromise requiring earlier intervention) or the completion of stimulation protocol. The induction of ventricular fibrillation was defined as an indeterminate result.
Follow-up
All patients were followed for an average of 14 months. Clinical follow-up was obtained as regular interval. Arrhythmic events during follow-up were defined as:
1. Sustained ventricular tachycardia or ventricular fibrillation;
2. Documented appropriate ICD therapy for ventricular tachyarrhythmia;
3. Sudden cardiac death.
Statistical analysis
Statistical analyses were performed by using SPSS 15.0 for Windows. Student's t test was used to analyze differences between mean values. A probability value of 0.05 or less was considered significant. For groups with fewer patients we chose t-repartition that requires a near-gaussian distribution of data and similar standard deviations in the compared groups. To verify the normality of data repartition we used Kolmogorov-Smirnov and Shapiro-Wilk tests; to verify the similarity of dispersions we used Levene test.
All results are expressed as mean ± standard deviation. Sensitivity, specificity, positive and negative predictive value, and the predictive accuracy of event-free prediction were evaluated.
Results
Microvolt T-wave alternans was determined during bicycle stress test in 71 patients (59%) and during atrial pacing in 34 patients (28%). In 15 patients (13%) we used both techniques, executed in consecutive days, in order to compare the results. In these 15 patients the results were similar. In 2 cases MTWA was indeterminate at bicycle test and positive at atrial pacing.
MTWA was positive in 34 patients (28%), negative in 70 patients (58%), and indeterminate in 22 patients (14%).
EPS was performed in 19 patients; it was positive in 5 patients, negative in 12 patients, and indeterminate in 2.
Predictors of EPS result were: male sex, echocardiography LVEF, 24 hour heart rate variability, late ventricular potentials, and MTWA (Table 1).
Table 1.
Predictors of EP study result
| EPS + (5 p) | EPS – (12 p) | p | |
| Age (years) | 59.2 ± 12.3 | 61.3 ± 11.7 | 0.3 |
| Male sex (%) | 80 | 70.5 | 0.04 |
| LVEF (%) | 38.2 ± 13.6 | 41.4 ± 12.8 | 0.003 |
| SDNN (ms) | 84 ± 18 | 112 ± 23 | 0.004 |
| SDANN5 (ms) | 91 ± 23 | 102 ± 27 | 0.05 |
| RMSSD | 32 ± 13 | 54 ± 21 | 0.05 |
| Holter NSVT (%) | 60 | 41 | 0.2 |
| LVP + (%) | 100 | 94 | 0.3 |
| MTWA + (%) | 60 | 0,9 | <0.0001 |
The positive predictive value of MTWA for inducible arrhythmia at EPS was 75%, negative predictive value was 88.8%, specificity – 94.1%, and sensitivity – 60%.
SAECG was less sensitive but more specific in predicting the result of EP study, suggesting that these tests could be used in combination. To verify this hypothesis we compared the results for each combination of results (Table 2). Patients with both test positive had the highest probability for inducible arrhythmia (hazard ratio = 6.2, p = 0.001). In patients with both tests negative sensitivity and NPV were low. Discordant combinations were less predictive.
Table 2.
Table 2
| Sensitivity | Specificity | PPV | NPV | RR | p | |
| MTWA | 60% | 94% | 75% | 88% | 5.2 | <0.001 |
| SAECG | 55% | 96% | 48% | 88% | 3.9 | <0.001 |
| MTWA+ SAECG+ | 51% | 97% | 77% | 91% | 6.2 | <0.001 |
| MTWA+ SAECG- | 29% | 75% | 24% | 79% | 1.5 | 0.4 |
| MTWA- SAECG+ | 8% | 85% | 13% | 78% | 0.4 | 0.6 |
| MTWA- SAECG- | 15% | 42% | 7% | 68% | 0.2 | <0.001 |
During follow-up in 11 patients (9.16%) arrhythmic events, as defined earlier, were recorded. Mortality was 4.16% (5 patients). End-point incidence was 11.66%, with an annual rate of 9.99%.
The table below presents the predictors of ventricular arrhythmia and sudden cardiac death.
Table 3.
Arrhythmia and SCD predictors
| + (16 p) | – (104 p) | p | |
| Age (years) | 62.4 ± 14.1 | 63.7 ± 12.7 | 0.07 |
| Male sex (%) | 81.25 | 58.65 | 0.03 |
| LVEF (%) | 39.3 ± 11.6 | 43.8 ± 12.4 | 0.003 |
| SDNN (ms) | 82 ± 22 | 119 ± 25 | 0.001 |
| SDANN5 (ms) | 85 ± 31 | 110 ± 26 | 0.04 |
| RMSSD | 36 ± 18 | 58 ± 26 | 0.05 |
| Holter NSVT (%) | 18.75 | 7.69 | 0.05 |
| LVP + (%) | 37.5 | 29.8 | 0.3 |
| MTWA + (%) | 87.5 | 19.23 | <0.0001 |
| EPS + (%) | 25 | 0.96 | <0.0001 |
To identify the independent predictors for clinical events, we performed a multivariate analysis. The composite end-point was ventricular arrhythmia and sudden cardiac death.
Left ventricular ejection fraction (hazard ratio = 3.5, p = 0.002), MTWA (hazard ratio = 11.2) and EPS (hazard ratio = 3.1) – X2 = 19.6 (p < 0.0001) were predictors of ventricular arrhythmia and sudden cardiac death. A Cox regression analysis that included only non-invasive tests showed that MTWA was the only independent predictor (hazard ratio = 10.2, X2= 15.5, p < 0.0001).
Discussions
Our study demonstrates that microvolt TWA can be used for arrhythmia risk stratification after myocardial infarction, having a good negative predictive value.
The positive predictive value of MTWA could be improved when the test is combined with other noninvasive markers, specifically ventricular late potentials. We consider that in patients with positive MTWA further evaluation, including electrophysiological study with programmed ventricular stimulation is needed.
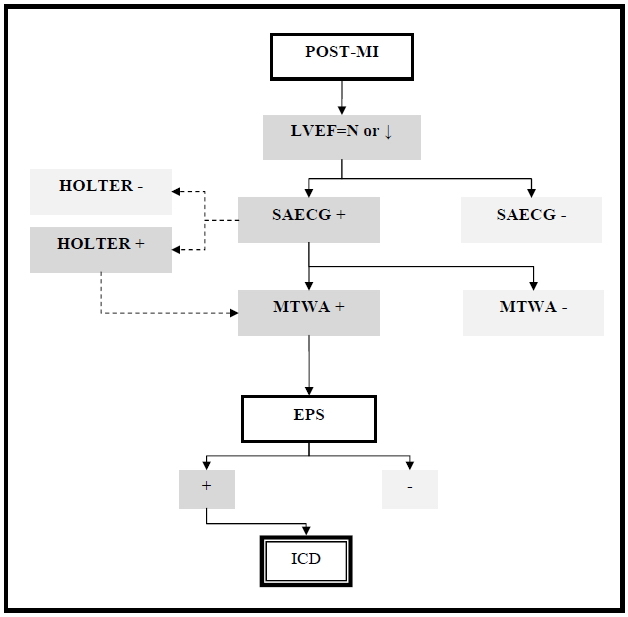
We propose the following algorithm for post-myocardial infarction arrhythmia risk stratification (Fig.1).
Fig.1.
Conclusions
The MTWA test has a good negative predictive value for arrhythmic events in post-MI patients and can be used for risk stratification. We consider that in patients with positive MTWA further invasive evaluation, respectively electrophysiology study, is necessary.
Glossary
| Abbreviation | Expansion |
|---|---|
| EP | electrophysiological |
| EPS | electrophysiology study |
| HFLA | high frequency low amplitude |
| HR | heart rate |
| ICD | implantable cardioverter/defibrillator |
| LVEF | left ventricular ejection fraction |
| LVP | late ventricular potentials |
| MI | myocardial infarction |
| MTWA | microvolt T-wave alternans |
| NPV | negative predictive value |
| NSVT | unsustained ventricular tachycardia |
| PPV | positive predictive value |
| RMS40 | root mean square of the terminal 40 ms of the filtered QRS |
| RMSSD | square root of the mean squared differences of successive NN intervals |
| SDNN | standard deviation of the NN interval |
| SDANN5 | standard deviation of the average NN interval calculated over 5 minutes |
| SAECG | signal averaged electrocardiography |
| SCD | sudden cardiac death |
| Valt | voltage alternans |
| VT | ventricular tachycardia |
| VF | ventricular fibrillation |
References
- 1.Adam DR, Akselrod S, Cohen RJ. Estimation of ventricular vulnerability to fibrillation through T-wave time series analysis. Comp in Card. 1981;8:307–310. [Google Scholar]
- 2.Adam DR, Powell AO, Gordon H, et al. Ventricular fibrillation and fluctuations in the magnitude of the repolarization vector. Comp in Card. 1982;9:241–244. [Google Scholar]
- 3.Adam DR, Smith JM, Akselrod S, et al. Fluctuations in T-wave morphology and susceptibility to ventricular fibrillation. J Electrocard. 1984;17(3):209–218. doi: 10.1016/s0022-0736(84)80057-6. [DOI] [PubMed] [Google Scholar]
- 4.Ritzenberg AL, Adam DR, Cohen RJ. Period multiplying-evidence for nonlinear behaviour of the canine heart. Nature. 1984;307:159–161. doi: 10.1038/307159a0. [DOI] [PubMed] [Google Scholar]
- 5.Smith JM, Blue B, Clancy EA, et al. Subtle alternating electrocardiographic morphology as an indicator of decreased cardiac electrical stability. Comp in Card. 1985;12:109–113. [PubMed] [Google Scholar]
- 6.Smith JM, Clancy EA, Valeri CR, et al. Electrical alternans and cardiac electrical instability. Circulation. 1988;77:110–121. doi: 10.1161/01.cir.77.1.110. [DOI] [PubMed] [Google Scholar]
- 7.Rosenbaum DS, Jackson LE, Smith JM, et al. Electrical alternans and vulnerability to ventricular arrhythmias. NEJM. 1994;330:235–241. doi: 10.1056/NEJM199401273300402. [DOI] [PubMed] [Google Scholar]
- 8.Hohnloser SH, Klingenheben T, Zabel M, et al. T-wave alternans during exercise and atrial pacing in humans. J Cardiov Electroph. 1997;8(9):987–993. doi: 10.1111/j.1540-8167.1997.tb00621.x. [DOI] [PubMed] [Google Scholar]
- 9.Klingenheben T, Zabel M, Peetermans J, et al. Assessment of T-wave alternans for prediction of recurrent ventricular tachycardia/fibrillation in patients with an implantable cardioverter/defibrillator. American Heart Association. 1997 Abstract #4010. [Google Scholar]
- 10.Caref EB, Stoyanovsky V, Cohen RJ, et al. Incidence of T-wave alternans in normal subjects, and effect of heart rate on onset. American Heart Association. 1997 Abstract #3256. [Google Scholar]
- 11.Zabel M, Siedow A, Klingenheben T, et al. Noninvasive Risk Stratification in Patients with Congestive Heart Failure: Comparison of Traditional Risk Markers and T Wave Alternans. J Am Coll Cardio. 1997;29(2):1091–1098. [Google Scholar]
- 12.Gehi AK, Stein RH, Metz LD, et al. Microvolt T-Wave Alternans for the Risk Stratification of Ventricular Tachyarrhythmic Events. A Meta-Analysis. J Am Coll Cardiol. 2005;46:75–82. doi: 10.1016/j.jacc.2005.03.059. [DOI] [PubMed] [Google Scholar]


