Abstract
Background:
Although intracranial Rosai–Dorfman disease is a principally benign lymphohistiocytosis, some patients run a relapsing or progressive course. However, reports about long-term follow-up are extremely rare.
Case Description:
In two patients, initial tumor resection was incomplete or followed by recurrences over 3 years, which finally subsided after application of chemotherapy, and patients remained tumor-free for more than 7 years thereafter.
Conclusion:
Up to now there is no agreement on how to treat complicated cases of intracranial Rosai–Dorfman disease; our good experience with adjuvant chemotherapy and long-term follow-up will contribute to treatment planning in complicated cases.
Keywords: Intracranial Rosai–Dorfman disease, incomplete resection, recurrence, chemotherapy, long-term follow-up
INTRODUCTION
Rosai–Dorfman disease (RDD) has been described as a benign lymphohistiocytosis presenting as a bilateral massive lymphoadenopathy with fever, neutrophilia, and an elevation of the sedimentation rate and gammaglobulins mainly affecting children and young adults. Histologically, the condition is characterized by large pale histiocytes containing engulfed erythro- and lymphocytes (“emperipolesis”). These so-called Rosai–Dorfman cells are CD68 and S-100 positive by immune-staining in the absence of Birbeck granules.[5] Extranodal manifestations occur in less than half of the cases affecting the skin, nasal cavity and sinuses, orbits, and salivary glands.
The central nervous system (CNS) – mainly the meninges – are involved in less than 5% of cases. Because the clinical and radiologic differentiation from meningiomas is difficult, surgery has been applied as first therapy and is considered to be essential for the diagnosis as well. After total removal, the outcome is usually good, but postoperative corticosteroids have been recommended, and some cases may need additional chemotherapy or radiation. However, because there is no standard treatment and reports about long-term results in difficult cases are rare,[1] our two case reports might contribute to treatment planning in complicated intracranial cases.
CASE REPORTS
Case 1
A 22-year-old male presented with progressive headache, focal convulsions, and monoparesis of his right arm and loss of vision of the right eye due to papillary congestion. In addition, he had noted a left supraclavicular swelling. Imaging showed a large extracranial space-occupying dura-based mass [Figure 1]. Lymph node and intracranial biopsy findings were compatible with RDD showing the emperipolesis phenomenon [Figure 2] and a positive S-100 reaction. On operation, the tumor could be removed completely. Nineteen months later, a right submaxillary lymph node was extirpated confirming the diagnosis. After further 10 months, a left temporo-basal and a parietal tumor and after another year, a left retrobulbar lesion appeared and was operated as well. Because of this relapsing course, the patient received chemotherapy consisting out of 8 cycles of cyclophosphamide (1 g), vincristine (2 mg), doxorubicin (50 mg), and prednisone (50 mg) for 5 days every 3 weeks according to a modified CHOP regimen.[4] Since then, no recurrences have been noted over a follow-up period of 7 years.
Figure 1.
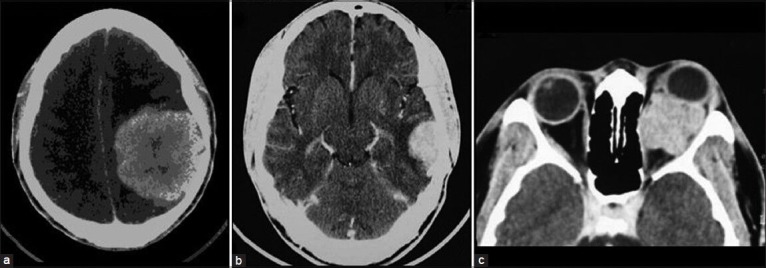
A 22-year-old male patient (case 1). (a) CT after injection of contrast medium shows an extra-axial left parietal tumor with strong enhancement, which was removed completely on first operation. (b) CT of left temporal tumor recurrence 29 months after first operation, which again was removed completely on second operation. (c) CT of intraorbital retrobulbar tumor recurrence 12 months after second operation
Figure 2.
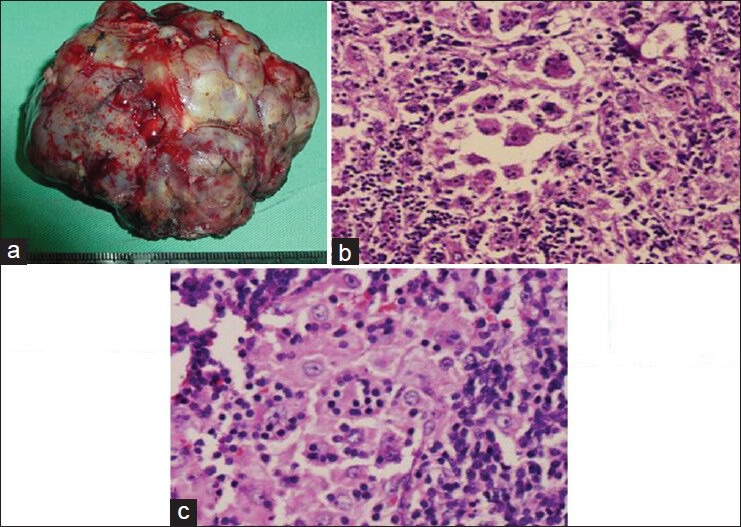
Same patient. Tumor after resection (a) and histology of this specimen (b) and of resected lymph node (c) histiocytes with large, pale nuclei and abundant cytoplasm containing several engulfed lymphocytes (emperipolesis). H and E, ×200 and ×400
Case 2
A 39-year-old male presenting with progressive headache since one year and a focal convulsion of the right side of his face on the day of admission. Computed tomography (CT) showed four space-occupying hyperdense lesions with prominent surrounding edema and enhancement in a left fronto-temporal, parietal/paramedian, occipital, and right central/periventricular localization [Figure 3]. The removal of the fronto-temporal mass was complicated by an extracranial cerebrospinal fluid (CSF)-containing cyst finally treated by duroplasty. Histology showed typical features of RDD. Two years later, because of persistence of the remaining lesions, the left parietal one was operated, and the others were treated successfully by chemotherapy following the CHOP regimen as in case 1. Since then, the patient has now been free from recurrences for 7 years.
Figure 3.
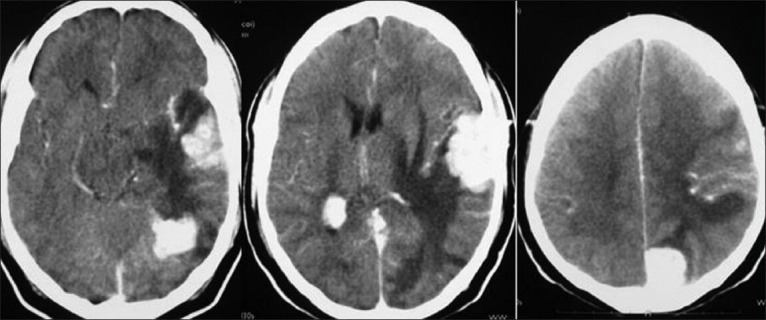
A 39-year-old male patient (case 2). CT after injection of contrast medium shows four enhancing lesions in a left fronto-temporal, parietal/paramedian, occipital, and right central/periventricular localization. On first operation, the fronto-temporal, and on second operation 2 years later, the parietal tumor was removed
DISCUSSION
In a first survey of 423 patients with RDD,[5] prognosis was found to correlate both with the number of nodal groups and systems affected. In an extensive review of 111 cases with involvement of the CNS published in 2010,[1] 15% of patients showed relapses, progression, or had died, but only 19 of them had been followed up for more than 3 years. Since then, further cases have been published mainly describing stable results after operation, sometimes together with application of corticosteroids or azathioprine. Partial resection followed by adjuvant chemotherapy has been recommended, especially in difficult localizations.[6] However, progression to blindness and deafness has been reported[7], as well as an “asymmetric response” – an enlargement of the intracranial lesion, but resolution of extracranial manifestations, following treatment with steroids.[9] In a recent retrospective study of 13 patients, 6 patients with involvement of the CNS, Zhu et al.[10] found stable conditions in only half of their cases. As the authors correctly stated, treatment is still controversial, mainly for relapsing cases or those with subresected lesions.
Our two cases of a predominantly intracranial localization of RDD showed a complicated course after surgical removal as the only treatment, but have been free of any further recurrences after application of chemotherapy now for 7 years. To our knowledge, this is the longest follow-up time reported in intracranial recurrences of this condition. Long-term observation is needed for two reasons: First, because there is no standard therapeutic concept as shown earlier and second, because recurrences may occur after several years as we can see from reports of progressions or recurrences after a latency of several years. A stable intraorbital lesion treated by immune-suppressive therapy progressed after 5 years,[3] a new intraspinal lesion developed 5 years after the operation of an intracranial one,[8] and in two patients with extracranial localization (cervical lymph nodes), the disease relapsed even after a course of 10 years.[2]
CONCLUSION
In intracranial RDD, the usual first approach is a surgical one because preoperative differentiation from meningiomas on imaging criteria alone is extremely difficult, and debulking of a space-occupying tumor is indicated. In difficult localizations, however, or in systemic involvement, biopsy may be the first option. Histology will then show the correct diagnosis, and the further course can be followed. However, according to our experience with two complicated cases, we recommend additional chemotherapy if there are signs of tumor persistence or recurrence. Another secondary treatment option might be stereotactic radiation of local recurrences or partially resected tumors, although experiences in this field are yet limited. Thereafter, long-term follow-up for several years is strongly recommended.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/1/30/128003
Contributor Information
Diones Rivera, Email: dionesrivera@gmail.com.
Miguelina Pérez-Castillo, Email: miguelinaperez@codetel.net.do.
Belkis Fernández, Email: belkis.fernandez@hotmail.com.
Peter Stoeter, Email: peter.stoeter@gmx.de.
REFERENCES
- 1.Adeleye AO, Amir G, Fraifeld S, Shoshan Y, Umansky F, Spektor S. Diagnosis and management of Rosai-Dorfman disease involving the central nervous system. Neurol Res. 2010;32:572–8. doi: 10.1179/016164109X12608733393836. [DOI] [PubMed] [Google Scholar]
- 2.Ben Turkia H, Ben Romdhane M, Azzouz H, Ben Chehida A, Abdelmoula MS, Ben Abdelaziz R, et al. Rosai -Dorfman disease: A two cases report. Tunis Med. 2011;89:497–501. [PubMed] [Google Scholar]
- 3.De Silva D, Joshi N. Rosai-Dorfman disease recurrence with bilateral orbital masses following immunosuppressant therapy. Orbit. 2005;24:51–3. doi: 10.1080/01676830590897209. [DOI] [PubMed] [Google Scholar]
- 4.Fisher RI, Gaynor ER, Dahlberg S, Oken MM, Grogan TM, Mize EM, et al. Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin's lymphoma. N Engl J Med. 2005;328:1002–6. doi: 10.1056/NEJM199304083281404. [DOI] [PubMed] [Google Scholar]
- 5.Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): Review of the entity. Semin Diagn Pathol. 1990;7:19–73. [PubMed] [Google Scholar]
- 6.Le Guenno G, Galicier L, Uro-Coste E, Petitcolin V, Rieu V, Ruivard M. Successful treatment with azathioprine of relapsing Rosai-Dorfman disease of the central nervous system. J Neurosurg. 2012;117:486–9. doi: 10.3171/2012.5.JNS12148. [DOI] [PubMed] [Google Scholar]
- 7.Nalini A, Jitender S, Anantaram G, Santosh V. Rosai Dorfman disease: Case with extensive dural involvement and cerebrospinal fluid pleocytosis. J Neurol Sci. 2012;314:152–4. doi: 10.1016/j.jns.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Seyednejad F, Tubbs RS, Shoja MM, Daghigi MH, Oakes WJ. Presumed recurrence of intracranial Rosai-Dorfman disease as a cervical spine tumor. Acta Neurochir (Wien) 2007;149:425–7. doi: 10.1007/s00701-007-1125-1. [DOI] [PubMed] [Google Scholar]
- 9.Walker RN, Nickles TP, Lountzis NI, Jacobs DL, Nawaz NK. Rosai-Dorfman disease with massive intracranial involvement: Asymmetric response to conservative therapy. J Neuroimaging. 2011;21:194–6. doi: 10.1111/j.1552-6569.2009.00404.x. [DOI] [PubMed] [Google Scholar]
- 10.Zhu F, Zhang JT, Xing XW, Wang DJ, Zhu RY, Zhang Q, et al. Rosai-Dorfman disease: A retrospective analysis of 13 cases. Am J Med Sci. 2013;345:200–10. doi: 10.1097/MAJ.0b013e3182553e2d. [DOI] [PubMed] [Google Scholar]


