Abstract
Usability testing is increasingly being recognized as a way to increase the usability and safety of health information technology (HIT). Medical simulation centers can serve as testing environments for HIT usability studies. We integrated the quality assurance version of our emergency department (ED) electronic health record (EHR) into our medical simulation center and piloted a clinical care scenario in which emergency medicine resident physicians evaluated a simulated ED patient and documented electronically using the ED EHR. Meticulous planning and close collaboration with expert simulation staff was important for designing test scenarios, pilot testing, and running the sessions. Similarly, working with information systems teams was important for integration of the EHR. Electronic tools are needed to facilitate entry of fictitious clinical results while the simulation scenario is unfolding. EHRs can be successfully integrated into existing simulation centers, which may provide realistic environments for usability testing, training, and evaluation of human–computer interactions.
Keywords: Electronic health records, Emergency Care Information Systems, Patient Simulation, Pilot Projects, User-computing interface
Introduction
Electronic health records (EHRs) are becoming increasingly common in hospitals and ambulatory practices.1 2 While most evaluation studies have demonstrated positive effects of health information technology (HIT),3 some studies have identified unintended consequences after the introduction of HIT (eg, increased time for antibiotic delivery after a hard stop during order entry, misreported data, and information loss).4–7 Healthcare providers have also expressed concerns that HIT is not easy to use and increases their workload.7–9 As a result, increased attention is being devoted to making HIT both safer and more usable.10 11
Usability evaluations performed by vendors/developers and researchers before, during, or after implementation can enhance the safety, efficiency, and user satisfaction of EHRs.12 To conduct HIT usability evaluations with users, researchers are increasingly using medical simulation to standardize clinical scenarios, simulate specific scenarios, and collect usability metrics, as these tasks are difficult if not impossible to perform in the clinical environment.13–22 Several research groups have created HIT usability laboratories to perform usability evaluations12 23; however, these dedicated facilities require large resource investments solely for HIT usability evaluation.
Over 130 US health care institutions have developed medical simulation centers to train and evaluate health professionals.24–27 Many of these centers have made large investments in physical space and expert staff. Some medical device manufacturers already use simulation centers as part of their product development processes, testing human factors, device features, and interaction with the clinical environment.28 Medical simulation centers can also be used as HIT usability laboratories, contributing to new product development, vendor content configuration, end user training, and evaluation.21 22
In order to study HIT usability and safety in medical simulation centers, EHRs must be integrated into them. However, previous reports have only described the use of virtual EHRs that have been specifically designed for the simulation environment.29 30 As part of a project to understand how emergency physicians use electronic documentation, we describe our approach and experience setting up, configuring, and using an actual emergency department (ED) EHR in a medical simulation center.
Case report
Setting
We partnered closely with our institution's multidisciplinary medical simulation center which is comprised of a variety of high-fidelity simulation suites, including two patient examination rooms, an operating room, conference and debriefing rooms, and virtual reality and technical skills laboratories. The simulation center is staffed by both simulation specialists and experts in simulation education. It is regularly used to train medical students, residents, and other hospital staff on resuscitation, critical care, team training, invasive procedures, and core content in a safe environment that replicates the clinical setting. The center is located on the hospital campus and is easily accessible by hospital staff. Our local institutional review board exempted this project from review.
Planning
We assembled an interdisciplinary team with expertise in clinical informatics, medical simulation, medical education, emergency medicine, and usability testing. Working closely with these experts in medical education and simulation, we designed a clinical scenario representative of a typical ED visit; the scenario was intentionally straightforward as the goal was to study emergency physician use of electronic documentation, not to assess medical knowledge or technical skills. The clinical scenario developed was that of a 55-year-old man with a history of atrial fibrillation on warfarin who presented to the ED with a headache after being hit in the head by a softball (see online supplementary appendix A). To increase the fidelity, we incorporated an interruption by a nurse requesting the participant to review an electrocardiogram for another ED patient, representing parallel processing that is typical in the ED.
Four research staff helped run the simulation scenario. A physician-actor played the role of the patient using a standardized script (see online supplementary appendix A). One research analyst facilitated and moderated the session. A second research analyst took notes during the encounter and played the role of nurse interrupter. A simulation center technician assisted with session setup and audiovisual recording.
Physical space
We configured the physical space of the simulation center to represent a typical ED examination room and used portable room dividers to delineate space inside and outside the patient room. Study staff monitored the session from a control room, separated from the examination room by one-way glass (figure 1).
Figure 1.

Adjacent simulation center control room allows research analysts to observe clinical simulation and collect data with usability software.
Computers
Our clinicians often use workstations on wheels (WOWs) in the ED. We used a similar WOW running the same software—Microsoft Windows XP and Microsoft Internet Explorer 8 (Microsoft, Redmond, Washington, USA) for the web-based ED EHR (figure 2). At their discretion, participants could freely move the WOW into the examination room for documenting at the patient bedside or leave the WOW outside while they performed their history and physical examinations.
Figure 2.

Participant gathering patient history and entering electronic clinical documentation using a workstation on wheels during a simulated patient encounter.
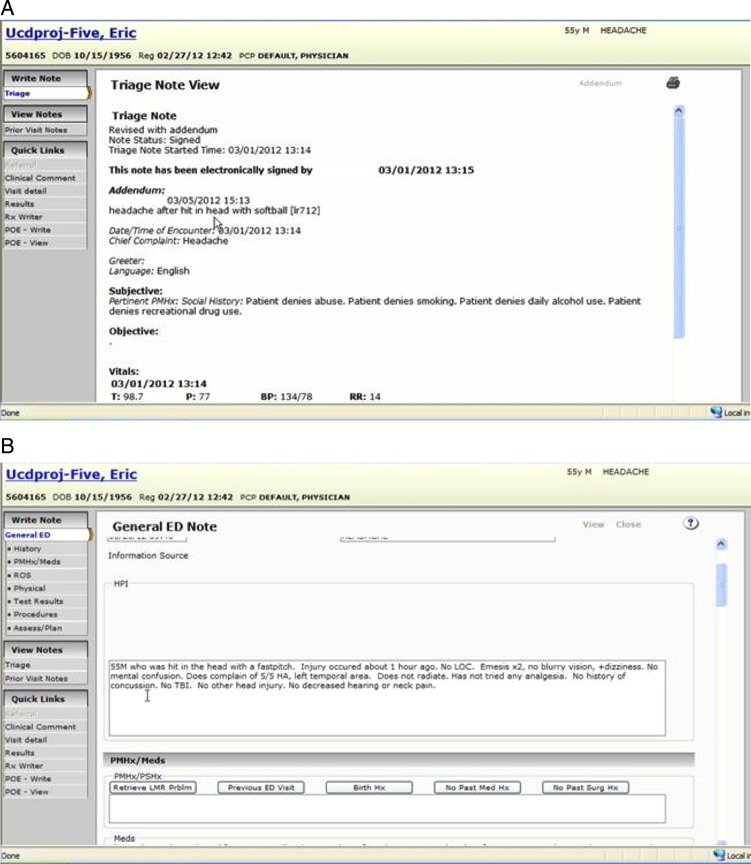
Electronic health record
We integrated the custom-developed, web-based ED EHR used in one of our EDs into the simulation scenario, focusing on the patient tracking and electronic physician documentation features. We used the quality assurance (QA) environment of the ED EHR, a fully functional version of the production system but without real patient data, that is primarily used by the information systems (IS) team to test new releases. Given this existing EHR testing environment, minimal IS resources were required to configure the QA EHR in the simulation setting. While there were no direct IS costs to our project, we needed to coordinate with IS to ensure concurrent use of the QA environment would not interfere with development activities and that the functionality would be the same as the current production system. The IS team also granted temporary access to the QA environment to research analysts and simulation session participants. The research analysts then created fictitious test patients with chief complaint and triage data specific to the scenario (see online supplementary appendix A) in the ED EHR (figure 3A).
Figure 3.
(A) Participant reviews simulated patient's nursing triage note in the emergency department (ED) electronic health record (EHR) (captured using Morae Recorder). (B) Participant enters history of present illness in the ED EHR (captured using Morae Recorder).
Computerized provider order entry (CPOE), electronic result review, and clinical document review are also available in our ED EHR, but handled by separate enterprise applications. Making these applications available for the simulated patients required additional coordination with enterprise application teams. Since our primary objective was to understand how emergency physicians used electronic documentation, we did not invest the additional resources to enable CPOE and results review features for the simulation encounter. Participants were therefore instructed to verbalize all orders (medications, laboratory, and imaging), the standard practice during simulation training in our facility. Further, there was no method for simulation staff to enter laboratory or imaging results into the EHR during the session. Consistent with current simulation center practice, Microsoft PowerPoint slides with laboratory and imaging results were displayed on a liquid crystal display monitor in the simulation room for participants to review.
Participants
We recruited participants from our emergency medicine residency program, offering a US$50 incentive payment. Participation was voluntary and did not impact performance evaluations or employment. All participating resident physicians had substantial experience with the ED EHR (residents use this EHR in their clinical practice) as well as the simulation environment (residents participate in biweekly simulation training as part of their residency training).25
Simulation scenario
Participants received a short, scripted orientation from research analysts explaining the logistics of the session and were then given 20 min to perform a complete ED visit, including history taking, physical examination, diagnostic testing, and disposition, as well as electronic documentation. All documentation was completed on the ED EHR system running on the WOW. Participants were permitted to proceed with patient evaluation as they deemed appropriate. The session was terminated when the participant completed clinical documentation or after 20 min, whichever endpoint was reached first.
Data collection
We collected multifaceted data on the participants’ use of the ED EHR during this session. The medical simulation environment enabled the research analysts to observe each simulation session from the control room, taking notes on the participant actions, workflow, and challenges using the ED EHR. We installed Morae Recorder (TechSmith, Okemos, Michigan, USA) onto the WOW to capture participant screen actions and interactive behavior in real time (figure 3B). Morae Observer was installed on a control room workstation, which allowed our trained research staff to monitor the participant's actions on the WOW and to record key interactions with the EHR interface.
Since simulation scenarios often need to be recorded for later debriefing, our medical simulation center is equipped with a state-of-the-art audiovisual system. We used existing wireless microphones and multiple cameras to record audio and video of the sessions for subsequent review.
Pilot testing
We performed a dry run with our project team and then pilot tested the entire simulated scenario, including the EHR and audiovisual equipment, with a physician participant. These pilot tests, well-established simulation best practices,31 32 identified issues with displaying laboratory and imaging results and WOW network connectivity that were resolved before additional physicians participated.
Results
Resident physicians successfully completed this simulation scenario and ED EHR electronic documentation. Each session generated quantitative and qualitative data on the participant's workflow and use of the ED EHR that will be analyzed to understand and improve ED EHR electronic documentation features.
We summarize the key tasks and resources needed to set up and use an EHR in a medical simulation center clinical scenario in table 1. We also held study team debriefings after every participant session, collecting feedback on operations and fidelity. We compiled cumulative lessons learned into a pre-simulation checklist (box 1) that was used before each simulation session to help ensure all systems were operational and previous missteps were not replicated.
Table 1.
Timeline with key resources for using an electronic health record in a medical simulation center clinical scenario
| Project stage | Task | Key required resources* (people and equipment) |
|---|---|---|
| Planning | Formulate operational or research question | |
| Establish partnership with simulation center and IS teams | Simulation leadership, IS leadership | |
| Understand available simulation center resources (ie, facilities, technicians) | Simulation staff | |
| Understand available IS resources (ie, EHR test environments) | IS analysts | |
| Simulation configuration | Design the clinical simulation scenario, including standardized test script and participant instructions | Clinical education experts, simulation staff |
| Identify staff required to run the scenario, including actors, project staff, and simulation center technicians | Simulation staff | |
| Identify simulation center physical space and props needed for scenario | Simulation staff | |
| Plan for how tests will be ordered and results viewed, within the scenario | Simulation staff, medical education experts | |
| If audio/video recording is needed, consider using simulation center resources (if available) | Simulation staff | |
| Information systems configuration | Plan for computer hardware in the simulation center (use existing or add new) | Simulation staff, computer workstation |
| Identify and coordinate use of an EHR test environment | IS analysts, EHR test environment | |
| Obtain access to the EHR test environment for study staff and participants | IS analysts | |
| Configure EHR for scenario, if needed | ||
| Consider installation of specialized software to capture all participant interactions with the EHR | Usability testing software | |
| Test configuration and operation of computers, EHR, and usability testing software in simulation center | ||
| Pilot testing | Dry run with project team | Simulation staff |
| Pilot test | Simulation staff, patient actor, participant | |
| Execute session | Recruit participants | Participants |
| Consent participants | ||
| Train participants on simulation setting and EHR, as needed | ||
| Perform pre-simulation session checklist (box 1) to verify EHR, AV equipment, and scenario are ready | Simulation staff | |
| Execute scenario | Simulation staff, patient actor, participant |
*Key resources also include one to two research analysts who will participate in all tasks.
AV, audiovisual; EHR, electronic health record; IS, information systems.
Box 1. Pre-simulation session checklist.
- Prepare and test emergency department (ED) electronic health record (EHR) in simulation center
- Boot workstation on wheels
- Login
- Open ED EHR application (verifies successful network connection)
- Select and confirm patient in ED EHR tracking board to be used for scenario
- Prepare and test audiovisuals
- Portable microphones for participant and interviewer
- Preset camera views/angles
- Test and queue PowerPoint presentation with laboratory and imaging results to project into simulation room after ordered by participant
- Set up Morae Recording environment
- Install Morae Recorder module on participant workstations
- Install Morae Observer module on control room workstation
- Connect Morae Observer and Recorder via network
- Confirm connection and live recording
- Prepare simulation
- Moulage standardized patient with hat and make-up to simulate head injury from softball game
- Ensure roles are known by standardized patient and nurse confederate
- Assemble necessary props (eg, stethoscope, otoscope, penlight, etc)
- Prepare paper electrocardiogram for interruption
- Position room dividers
Discussion
We successfully integrated an actual ED EHR into our medical simulation center, creating an EHR usability laboratory. Our methods and experiences serve as a model for others seeking to integrate real EHRs into their simulation centers and sessions. Meticulous planning, using existing facilities and infrastructure, and strong partnerships with clinical educators, medical simulation experts, and IS will facilitate integration of the EHR into the simulation setting. Once established, simulation centers with EHR capabilities have numerous applications, including workflow analysis, testing and evaluating clinical systems, and training clinical staff on IS.
Using our QA environment allowed us to rapidly integrate the EHR clinicians use in clinical practice into the medical simulation center. A similar approach can be taken by other simulation centers looking to add to their facilities’ EHR regardless of system type (home-grown, vendor, modular, or enterprise). IS routinely creates and maintains different versions or environments of their system such as development, testing/QA, training, and production. Working with the institution's IS team, simulation centers can create independent, dedicated simulation EHR environments or use an existing application environment, as we did.
Limitations
This simulation was not a formal evaluation or validation of the EHR in the simulation environment. In this case report, we did not analyze workflow or usability data on the participants’ use of the EHR during the simulated scenario. Participants had considerable experience with both the EHR and simulation environment. Alternative approaches, such as additional training time, may be needed if participants are unfamiliar with simulation or the system being tested. While we used a custom-developed ED EHR system, the general principles we described for integrating an EHR into a simulation scenario apply to any EHR system. Additional resources may also be required for more complex simulation scenarios and for institutions without comprehensive medical simulation centers and robust EHR testing environments. Finally, an important challenge is the inability of simulation scenario facilitators to electronically enter results in the simulated patients’ electronic records. Tools are needed to allow manual entry (or predefined automatic entry) of fictitious clinical results (such as laboratory and imaging results) to the patient record in real time while the simulation scenario is unfolding.
Conclusion
Medical simulation centers can be used as EHR usability laboratories. We described one approach to integrating clinical IS into a medical simulation center using the QA environment of our EHR and working closely with our IS and simulation center teams. With greater interest in EHR usability and simulation, challenges with real-time simulation results entry and review are likely to be overcome. With the integration of real EHR systems, medical simulation centers can become usability laboratories to facilitate analysis of clinician workflow, test and evaluate IS, and train clinical staff on IS.
Supplementary Material
Acknowledgments
The authors wish to thank the resident physicians who participated in the study, as well as Camille Ducharme and Andrew Reisner, MD, from the Massachusetts General Hospital for their support.
Footnotes
This work was presented as a poster at the American Medical Informatics Association Annual Symposium in Chicago, IL, in November 2012.
Contributors: ABL, CNP, and EGP conceived the project; ABL, PN, JH, ASR, CNP, GS, and EGP developed the simulation case; ABL, LR, PN, and SP facilitated the simulations; ABL, LR, and PN drafted the manuscript and all authors contributed substantially to its revision. ABL had full access to all of the data in the case report and takes responsibility for the paper as a whole.
Funding: This work was supported by the Brigham and Women's Hospital Department of Emergency Medicine Esther B. Kahn Fund Young Investigator Award and the Brigham and Women's Hospital Neil and Elise Wallace STRATUS Center for Medical Simulation.
Competing interests: ABL received grant funding from the Brigham and Women's Hospital. SP is now principal of Simulation Consulting, a firm he started after the completion of this research but prior to manuscript preparation and publication. No other authors have competing interests to declare.
Ethics approval: The Partners Human Research Committee approved this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Desroches CM, Charles D, Furukawa MF, et al. Adoption of electronic health records grows rapidly, but fewer than half of US hospitals had at least a basic system in 2012. Health Aff (Millwood) 2013;32:1478–85 [DOI] [PubMed] [Google Scholar]
- 2.Hsiao CJ, Jha AK, King J, et al. Office-based physicians are responding to incentives and assistance by adopting and using electronic health records. Health Aff (Millwood) 2013;32:1470–7 [DOI] [PubMed] [Google Scholar]
- 3.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011;30:464–71 [DOI] [PubMed] [Google Scholar]
- 4.Strom BL, Schinnar R, Aberra F, et al. Unintended effects of a computerized physician order entry nearly hard-stop alert to prevent a drug interaction: a randomized controlled trial. Arch Intern Med 2010;170:1578–83 [DOI] [PubMed] [Google Scholar]
- 5.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005;293:1197–203 [DOI] [PubMed] [Google Scholar]
- 6.Horsky J, Kuperman GJ, Patel VL. Comprehensive analysis of a medication dosing error related to CPOE. J Am Med Inform Assoc 2005;12:377–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel VL, Kushniruk AW, Yang S, et al. Impact of a computer-based patient record system on data collection, knowledge organization, and reasoning. J Am Med Inform Assoc 2000;7:569–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kellermann AL, Jones SS. What it will take to achieve the as-yet-unfulfilled promises of health information technology. Health Aff (Millwood) 2013;32:63–8 [DOI] [PubMed] [Google Scholar]
- 9.Campbell EM, Sittig DF, Ash JS, et al. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2006;13:547–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schumacher R, Lowry S. NIST guide to the processes approach for improving the usability of electronic health records. November 2010
- 11.Armijo D, McDonnell C, Werner K. Electronic health record usability: interface design considerations. Agency for Healthcare Research and Quality, 2009 [Google Scholar]
- 12.Russ AL, Weiner M, Russell SA, et al. Design and implementation of a hospital-based usability laboratory: insights from a Department of Veterans Affairs laboratory for health information technology. Jt Comm J Qual Patient Saf 2012;38:531–40 [DOI] [PubMed] [Google Scholar]
- 13.Saleem JJ, Patterson ES, Militello L, et al. Impact of clinical reminder redesign on learnability, efficiency, usability, and workload for ambulatory clinic nurses. J Am Med Inform Assoc 2007;14:632–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saleem JJ, Patterson ES, Militello L, et al. Using human factors methods to design a new interface for an electronic medical record. AMIA Annu Symp Proc 2007:640–4 [PMC free article] [PubMed] [Google Scholar]
- 15.Agutter J, Drews F, Syroid N, et al. Evaluation of graphic cardiovascular display in a high-fidelity simulator. Anesth Analg 2003;97:1403–13 [DOI] [PubMed] [Google Scholar]
- 16.Borycki EM, Kushniruk AW, Kuwata S, et al. Use of simulation in the study of clinician workflow. AMIA Annu Symp Proc 2006:61–5 [PMC free article] [PubMed] [Google Scholar]
- 17.Kushniruk AW, Patel VL. Cognitive and usability engineering methods for the evaluation of clinical information systems. J Biomed Inform 2004;37:56–76 [DOI] [PubMed] [Google Scholar]
- 18.Kushniruk AW, Santos SL, Pourakis G, et al. Cognitive analysis of a medication reconciliation tool: applying laboratory and naturalistic approaches to system evaluation. Stud Health Technol Inform 2011;164:203–7 [PubMed] [Google Scholar]
- 19.Ammenwerth E, Hackl WO, Binzer K, et al. Simulation studies for the evaluation of health information technologies: experiences and results. HIM J 2012;41:14–21 [DOI] [PubMed] [Google Scholar]
- 20.Lawton K, Binzer K, Skjoet P, et al. Lessons learnt from conducting a high fidelity simulation test in health IT. Stud Health Technol Inform 2011;166:217–26 [PubMed] [Google Scholar]
- 21.Haugen H. Advantages of simulation training. How to improve EMR adoption. Health Manag Technol 2012;33:10–11 [PubMed] [Google Scholar]
- 22.Pennathur PR, Cao D, Sui Z, et al. Development of a simulation environment to study emergency department information technology. Simul Healthc 2010;5:103–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elkin PL, Sorensen B, De Palo D, et al. Optimization of a research web environment for academic internal medicine faculty. J Am Med Inform Assoc 2002;9:472–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okuda Y, Bryson EO, DeMaria S, et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med 2009;76:330–43 [DOI] [PubMed] [Google Scholar]
- 25.Binstadt ES, Walls RM, White BA, et al. A comprehensive medical simulation education curriculum for emergency medicine residents. Ann Emerg Med 2007;49:495–504, 504.e491–411 [DOI] [PubMed] [Google Scholar]
- 26.Gordon JA, Shaffer DW, Raemer DB, et al. A randomized controlled trial of simulation-based teaching versus traditional instruction in medicine: a pilot study among clinical medical students. Adv Health Sci Educ Theory Pract 2006;11:33–9 [DOI] [PubMed] [Google Scholar]
- 27.Society for Simulation in Healthcare. Simcenter US: Sim Centers in the US. http://ssih.org/directory-of-sim-centers-2/simcenter-us (accessed 8 Jul 2013)
- 28.Wiklund ME, Kendler J, Strochlic AY. Usability testing for medical devices. New York: CRC Press, 2011 [Google Scholar]
- 29.Tworek J, Topps D. Simulated electronic medical record (EMR) training using virtual patient software. Simulation Healthc 2011;6:499 [Google Scholar]
- 30.Giguiere T, Adams R, Leveille D, et al. Simulating information technology: an electronic medical record as an enhancement in medical simulation. Simulation Healthc 2011;6:456 [Google Scholar]
- 31.Ziewacz JE, Arriaga AF, Bader AM, et al. Crisis checklists for the operating room: development and pilot testing. J Am Coll Surg 2011; 213:212–17e210 [DOI] [PubMed] [Google Scholar]
- 32.Ishman SL, Brown DJ, Boss EF, et al. Development and pilot testing of an operative competency assessment tool for pediatric direct laryngoscopy and rigid bronchoscopy. Laryngoscope 2010;120:2294–300 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.