Abstract
The clinical efficacy of EGFR kinase inhibitors gefitinib and erlotinib is limited by the development of drug resistance. The most common mechanism of drug resistance is the secondary EGFR T790M mutation. Strategies to overcome EGFRT790M mediated drug resistance include the use of mutant selective EGFR inhibitors, including WZ4002, or by the use of high concentrations of irreversible quinazoline EGFR inhibitors such as PF299804. In the current study we develop drug resistant versions of the EGFR mutant PC9 cell line which reproducibly develops EGFRT790M as a mechanism of drug resistance to gefitinib. Neither PF299804 resistant (PFR) or WZ4002 resistant (WZR) clones of PC9 harbor EGFR T790M. Instead, they demonstrate activated IGF1R signaling as a result of loss of expression of IGFBP3and the IGF1R inhibitor, BMS 536924, restores EGFR inhibitor sensitivity. Intriguingly, prolonged exposure to either PF299804 or WZ4002 results in the emergence of a more drug resistant subclone which contains ERK activation. A MEK inhibitor, CI-1040, partially restores sensitivity to EGFR/IGF1R inhibitor combination. Moreover, an IGF1R or MEK inhibitor used in combination with either PF299804 or WZ4002 completely prevents the emergence of drug resistant clones in this model system. Our studies suggest that more effective means of inhibiting EGFR T790M will prevent the emergence of this common drug resistance mechanism in EGFR mutant NSCLC. However, multiple drug resistance mechanisms can still emerge. Preventing the emergence of drug resistance, by targeting pathways that become activated in resistant cancers, may be a more effective clinical strategy.
Keywords: Non -small cell lung carcinoma, kinase inhibitor, drug resistance
INTRODUCTION
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) gefitinib and erlotinib are clinically effective therapies for non-small cell lung cancer (NSCLC) patients with EGFR mutant cancers (1–6). However, therapy is universally limited by the development of acquired drug resistance (7). The most common mechanism of acquired drug resistance is the secondary EGFR T790M mutation and is detected in up to 60% of EGFR mutant NSCLC patients that develop acquired drug resistance to either gefitinib or erlotinib (8–10). The EGFR mutant PC9 cell line has been used as model of drug resistance and reproducibly develops EGFRT 790Mfollowing prolonged in vitro exposure to gefitinib or other reversible EGFR kinase inhibitors (11–13).
Irreversible second generation EGFR TKIs are undergoing clinical development to overcome EGFR T790M mediated drug resistance. The quinazoline-based irreversible TKIs, including neratinib (HKI-272), afatinib (BIBW2992), and dacomitinib (PF299804) have been shown to have potency against EGFR T790M bearing models at high concentrations in pre -clinical models (14–16). However, when used at low concentrations, those achievable in NSCLC patients being clinically treated with these agents, the resistance induced by these drugs in EGFR-mutant models, including in the PC9 cells, also occurs through the emergence of the T790M mutation (17, 18). In accordance with these pre-clinical data, neratinib and afatinib demonstrated only modest efficacy in EGFR-mutant NSCLC patients that had developed acquired resistance to gefitinib or erlotinib (19, 20). One potential reason why neratinib or afatinib have not been effective clinically is due to the inability to achieve sufficient drug concentrations to inhibit EGFR T790M in NSCLC patients. Dose escalation of irreversible quinazoline EGFR inhibitors is limited by on target inhibition of wild type (WT) EGFR which leads to dose limiting skin rash (21, 22). These clinical observations have prompted the development of alternative strategies to inhibit EGFR T790M. One strategy is to develop mutant selective EGFR inhibitors. In prior studies we identified a novel class of irreversible pyrimidine inhibitors, including WZ4002, which are significantly more potent against EGFR T790M compared to irreversible quinazoline based inhibitors (23). An alternative strategy is to use high, but intermittent, doses of current clinical agents including dacomitinib which may lead to sufficient drug concentrations to inhibit EGFR T790M as was observed in prior studies (11).
While the use of more effective therapeutic approaches against EGFR T790M may prevent the clinical emergence of this mechanism of drug resistance, such therapies are unlikely to cure advanced EGFR mutant NSCLC. Understanding these resistance mechanism(s) will allow the identification and subsequent prioritization of rationale treatment strategies and/or combination therapies. These combination strategies may ultimately lead to a more effective therapeutic cocktail against EGFR mutant NSCLC translating to improved patient outcome. To address and study mechanisms of resistance that may emerge instead of EGFR T790M, we generated models of drug resistance to the PC9 cells using2 structurally different EGFR TKIs, the quinazoline irreversible inhibitor PF00299804 and the pyrimidine irreversible inhibitor WZ4002.
MATERIAL AND METHODS
Generation of drug-resistant cell lines
PF299804 resistant (PFR) clones ofPC9 cells were generated by exposing cells to increasing concentrations (up to 1 μM) of PF299804 as previously described (11, 24). WZ4002 resistant (WZR) PC9 cells were generated in a 96-well plate, 200 cells/well, and exposed to 1 μM of WZ (17).
Individual clones from PFR cells or WZR cells were selected. Once cells had reached confluence, they were passed 5 more times in a medium with drug, then the drug was withdrawn and cells were confirmed to be drug-resistant using an MTS assay (11, 24).
Cell culture and reagents
The EGFR mutant NSCLC cell line PC9 has been previously characterized (25). PC9, PFR and WZR cells were cultured in RPMI supplemented with 10% FBS. Drug resistant cells were cultured with1 μM of PF299804 orWZ4002. PF299804 was obtained from Pfizer (La Jolla, CA, USA). Trichostatine A and CI -1040 were purchased from Calbiochem. BMS-536924 and OSI-906 were purchased from Selleck Chemicals (Houston, TX, USA). Recombinant human IGFBP3 was purchased from Sigma-Aldrich. WZ4002 was synthesized as previously described (23). The PC9 cells were obtained from Dr. Nishio and confirmed by fingerprinting using the Power Plex 1.2 system (Promega, Madison, WI) most recently on March 2012.
Cell proliferation and growth assays
Growth and inhibition of growth was assessed by MTS assay according to previously established methods (11, 24, 26). All experimental points were set up in six to twelve wells and all experiments were repeated at least three times. These data were graphically displayed using GraphPad Prism version 5.0 for Windows, (GraphPad Software; www.graphpad.com).
For clonogenic assays, 2000 cells were plated in a 6-well plate, incubated overnight, then treated with indicated drug concentrations. Eight to 10 days later, wells were fixed with a 0.5% Crystal Violet solution. Number of colonies formed was estimated with the ImageJ software (http://rsbweb.nih.gov/ij/). All experimental points were set up in 3 wells and all experiments were repeated at least twice. These data were graphically displayed using GraphPad Prism version 5.0 for Windows.
Prevention of emergence of resistance
PC9 cells were plated (200 cells/well in 96-well format) and were either untreated or treated with one drug or combinations of drugs. The medium and drugs were regularly renewed for up to 3 months. Each confluent well was considered as one resistant colony.
Antibodies and western blotting
Cells grown under the previously specified conditions were lysed in a Lysis Buffer (Cell Signaling Technology). Western blot analyses were conducted after separation by SDS–PAGE electrophoresis and transfer to nitrocellulose membranes. Immunoblotting was performed according to the antibody manufacturer’s recommendations. Anti-phospho-Akt (Ser-473), anti-total-Akt, anti-phospho-IGF1R (pY1135), anti-total-IGF1R, and anti-EGFR antibodies were obtained from Cell Signaling Technology. The phospho-EGFR (pY1068), total-ERK1/2, phospho-ERK1/2 (pT185/pY187) antibodies were purchased from Invitrogen (Carlsbad, CA, USA). The anti-KDM5A and anti-DUSP6 antibodies were purchased from Abcam.
EGFR and IGF1R mutational and analysis
Total RNA was isolated from cell lines or tumors using Trizol (Invitrogen, Carlsbad, CA, USA) and purified using RNeasy minielute cleanup kit (Qiagen, Valencia, CA, USA). cDNA was transcribed with Superscript II Reverse Transcriptase (Invitrogen Life Technologies) and used as template for subsequent PCR based studies. The PCR primers and conditions are available upon request.
IGFBP3 methylation studies
Promoter methylation of IGFBP3 was evaluated using previously published methods and primers (27).
Gene Expression Analysis
Methods for Gene Expression Analysis have been described elsewhere (28). Synthesis of cRNA and hybridization to Human Expression Array U133 A2.0 chips were performed following Affymetrix protocols (Affymetrix, Inc. Santa Clara, CA, USA). Probe-level intensity data files in the CEL format were pre-processed using Robust Multichip Average program using the GenePattern software (genepattern.broadinstitute.org). Probes representing the same genes were collapsed into a single value, and standardized by taking the median value for each gene across sample set in the GenePattern software. The normalized data was subject to comparative maker selection module in GenePattern and genes differentially expressed in the samples that meet defined criteria (p<0.01, fold change (FC) >4) were selected. The expression values of the genes were log 2 converted and represented in a heat map using GENE-E. The expression data has been deposited to GEO (accession GSE38404).
RESULTS
Establishment of PC9-derived clones resistant to the irreversible EGFR inhibitors PF299804 and WZ4002
PF299804 resistant (PFR) cells were obtained by chronic exposure of PC9 cells to increasing doses of PF299804 up to 1μM using previously established methods (11, 24). All PFR clones had an IC50for PF299804 more than 100 fold that of parental PC9 cells (Fig. 1A). WZ4002 resistant (WZR) cells were obtained by exposing PC9 cells to 1μM of WZ4002 (17). WZR cells had an IC50about 10 fold that of parental PC9 cells (Fig. 1B). Within 4 to 6 months, more than 4 independent PF299804 resistant clones and 4 WZ4002 resistant clones were isolated. Resistance to PF299084 and WZ4002 was maintained overtime for PFR and WZR cells respectively, even after 20 passages in a medium with no drug (data not shown). The PFR and WZR cells were cross resistant to WZ4002 and PF299804, respectively as well as gefitinib (data not shown).
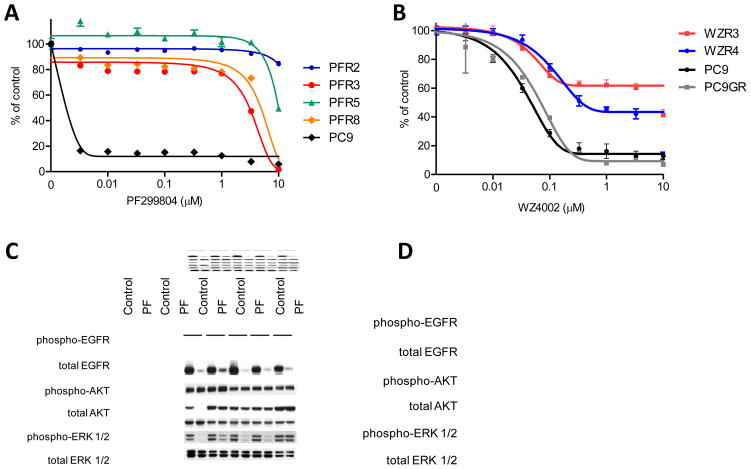
Figure 1. PF299084 and WZ4002 resistant cells maintain PI3K/AKT signaling following drug treatment.
A. PC9 (delE746_A750) and PF299804 resistant cells were treated at the indicated concentrations, and viable cells were measured after 72 hours of treatment and plotted relative to untreated controls B. PC9, PC9 GR4 (delET746_A750/T790M) and WZ4002 resistant cells were treated with WZ4002 as in A. C. PC9 and PFR cells were treated with PF299804 (1 μM) for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins. D. PC9 and WZR cells were treated with indicated concentrations of WZ4002 for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins.
PFR and WZR cells maintain AKT signaling in the presence of PF299804 or WZ4002 treatment
We next evaluated the effects of PF299804 and WZ4002 on phosphorylation of EGFR, A KT and ERK1/2 in the parental and PFR or WZR clones. In both the parental and drug resistant clones, PF299804 and WZ4002 effectively inhibited EGFR phosphorylation (Fig. 1C and D). Consistent with these observations, no secondary mutations in EGFR were detected in any of the PFR or WZR clones (data not shown). However, unlike in the parental PC9 cells, in both PFR and WZR clones, AKT phosphorylation was maintained following PF299804 and WZ4002 treatment respectively, compared to untreated cells (Figs. 1C and 1D). As PF299804 and WZ4002 still inhibited EGFR phosphorylation, unlike in the PC9 cells, EGFR is unlikely to be responsible for activation of AKT signaling in these drug resistant cells (Figure 1). In contrast to AKT, ERK1/2 phosphorylation was inhibited in all but one PFR clones (PFR 5) and in all of the WZR cells (Fig. 1C and D) suggesting that EGFR still controls ERK1/2 signaling in the majority of the drug resistant cells.
PFR and WZR cells are sensitive to concurrent EGFR and IGF1R inhibition
In order to identify how AKT was activated in the PFR and WZR clones, we tested the sensitivity of these cells to drugs inhibiting PI3K/AKT (Fig S1A and B) signaling to determine if they would reverse drug resistance. The persistence of AKT phosphorylation but not ERK1/2 phosphorylation following drug exposure and reversal of resistance by the PI3K inhibitor PI-103 (Fig S1C and S1D) in the drug resistant cell lines, suggests that PI3K signaling may be activated by the insulin like growth factor receptor (IGF1R) (29). Furthermore, PI-103 and CI-1040 (MEK inhibitor) combination phenocopied the effects of PI-103 and PF299804 or WZ4002 (Fig. S1E and S1F). To more directly evaluate the role of IGF1R, we evaluated BMS536924, an IGF1R inhibitor alone or in combination with PF299804 or WZ4002 in the drug resistant cell lines (30). Although not effective when used as a single agent (Fig S2A), BMS536924, restored drug sensitivity in both PFR and WZR cells when used in combination with PF299804 or WZ 4002, respectively (Figs. 2A and 2B). The effects were similar in both short term (3 days (Figs. 2A and B)) and long term clonogenic (2 weeks (Figs. 2C and D)) assays. The only clone in which BMS536924 did not fully restore sensitivity to PF299804 was PFR5 which was also the only drug resistant clone to maintain ERK1/2 phosphorylation (Figs. 2A and 1C). However, in the clonogenic assay, there was some effect of BMS536924 and PF299804 in the PFR5 clone consistent with the modest effect observed in the MTS assay (Figs 2A and C). The IC50of PFR3 cells for PF299804 was more than 100 fold lower with the combination of BMS536924 and PF00299804 than with PF00299804 alone (Fig. 2A). Similar results were observed with OSI-906, a dual IGF1R/Insulin Receptor tyrosine kinase inhibitor, when combined with either PF299804 or WZ4002 (Fig. S3A and S3B) (31).
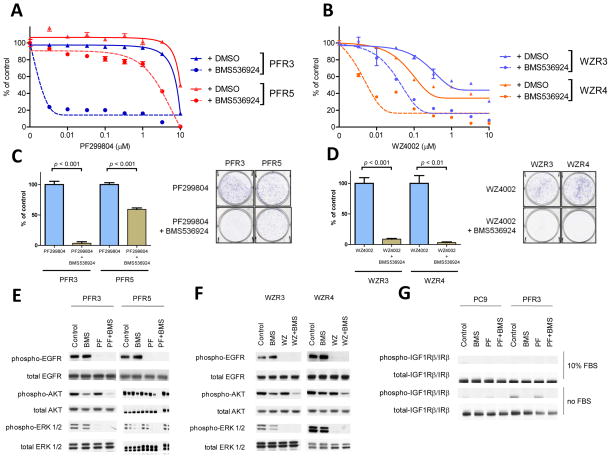
Figure 2. Inhibition of IGF1R restores sensitivity to EGFR TKIs in drug resistant cells.
A. PFR3 and PFR5 cells were treated with increasing concentrations of PF299804 alone or in the presence of BMS536924 (1 μM) at the indicated concentrations, and viable cells were measured after 72 hours of treatment and plotted relative to untreated controls. B. WZR3 and WZR4cells were treated as in A. C. Clonogenic assays of PFR3 and PFR5 cells. Cells were treated with PF299804 (1 μM) alone or in combination with BMS536924 (1 μM). D. Clonogenic assays of WZR3 and WZR4 cells. Cells were treated with WZ4002 (1 μM) alone or in combination with BMS536924 (1 μM). E. PFR3 and PFR5 cells were treated with PF299804 (1 μM) alone, BMS536924 (1 μM) alone or with the combination of both agents for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins. F. WZR3 and WZR4 cells were treated withWZ4002 (1 μM) alone, BMS536924 (1 μM) alone or with the combination of both agents for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins. G. PC9 or PFR3 cells were grown in the presence or absence of fetal bovine serum. Cells were treated with PF299804 (1 μM) alone or in combination with BMS536924 (1 μM) for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins.
The combined treatment with BMS536924 and PF299804 effectively inhibited A KT phosphorylation in the PFR3 but not PFR5 cells (Fig. 2E). Similar findings were observed when BMS536924 was combined with WZ4002 in the WZR cells (Fig. 2F). We noted that the levels of IGF1R phosphorylation were higher in PFR clones compared to parental PC9 cells, especially without serum in the culture medium (Fig. 2G). No mutation sin the tyrosine kinase of IGF1R were detected in either the PFR or the WZR clones (data not shown). Prior studies have identified drug-tolerant tumor cells showing transient resistance to gefitinib through activation of the IGF1R pathway and an altered chromatin state characterized by high levels of the histone demethylase RBP2/KDM5A/Jarid1A and sensitivity to histone deacetylase (HDAC) inhibition (32). However, the mechanism of drug resistance is different in the PFR and WZR cells. In addition, the PFR 3 cells had persistent resistance to PF299804 even while being cultured in the absence of drug (Fig. S4A) did not contain elevated KDM5A levels compared to parental PC9 cells (Fig. S4B) and were not sensitive to trichostatin A, an HDAC inhibitor (Fig. S4C) shown to reverse sensitivity in the drug tolerant cells (32).
IGFBP3 is down-regulated in PFR and WZR clones
In order to determine the mechanism leading to activation of the IGF1R pathway in PFR and WZR resistant clones, we performed gene expression analyses and compared the findings to the parental PC9 cells. Interestingly, we found that IGFBP3 was downregulated in the PF299804 resistantPFR3 cells, compared to parental PC9 cells (Fig. 3A). IGFBP3 is the main carrier protein for insulin-like growth factors and its downregulation has already been implicated as a mechanism of acquired resistance in the EGFR wild-type A431 cell line to gefitinib (29). We further validated the findings from the gene expression studies by Western blotting (Fig 3A). All of the resistant clones, including PFR5, demonstrated reduced levels of IGFBP3 compared to the parental PC9 cells. The decreased expression of IGFBP3 is as a result of promoter methylation as determined by methylation specific PCR (Fig. S5).
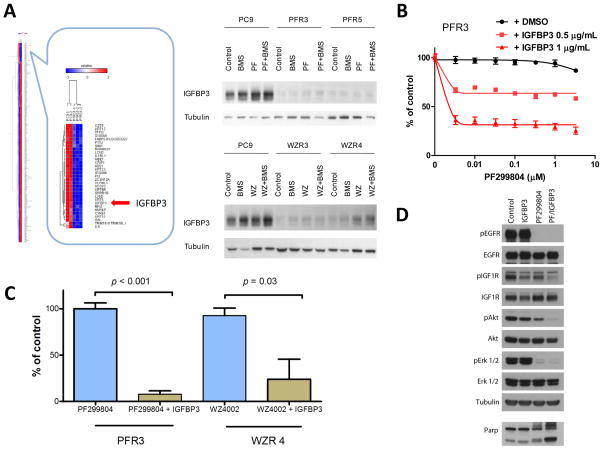
Figure 3. IGFBP3 is downregulated in PFR and WZR cells.
A. (Left) Comparison of expression profiles of PC9 and PFR3 cells (left panel). Hierarchical clustering of the differentially expressed genes (p<0.0025, fold change (FC) >3.9) was performed using GENE-E. (Right) The indicated cell lines were treated with either PF299804 (1 μM) alone, WZ4002 alone (1 μM) or in combination with BMS536924 (1 μM) for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins. B. PFR3 cells were treated with increasing concentrations of PF299804 alone or in combination with IGFBP3. Viable cells were measured after 72 hours of treatment and plotted relative to untreated controls. C. PFR3or WZR4 cells were treated with PF299804 (1 μM) alone or in combination with IGBP3 (1 μg/mL). Colonies were counted after 14 days of treatment. D. PFR3 cells were treated with PF299804 (1 μM) alone, IGFBP3 alone (1 μg/mL) or with both agents for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins.
We next tested whether re -expression of IGFBP3 alone could sensitize the PFR3 cells to PF299804. Treatment of PFR3 cells with recombinant IGFBP3 restored sensitivity to PF299804 in a dose-dependent manner (Fig 3B). There was no effect of IGFBP3 by itself (Fig. S2B). We observed similar findings using a clonogenic assay (Fig 3C). The addition of IGFBP3 also restored the ability of PF299804 to downregulate Akt phosphorylation in the PFR3 cells in accordance with the observations in the growth assays (Figs. 3D). Our studies suggest that in the drug resistant cell lines, downregulation of IGFBP3 leads to activation of IGF1R signaling, which activates PI3K/AKT signaling resulting in resistance to either PF299804 or WZ4002.
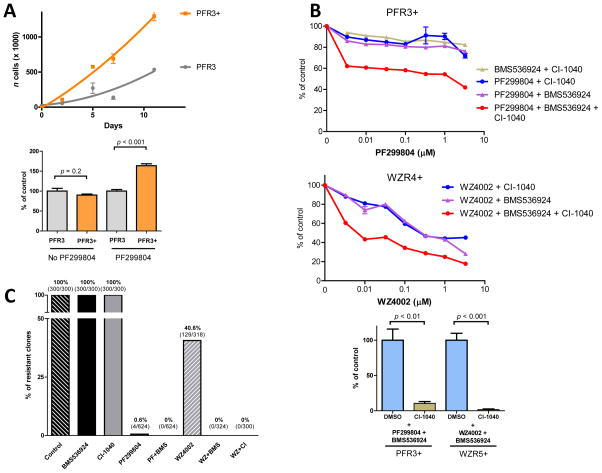
Prolonged exposure of PFR or WZR cells to PF299804 or WZ4002 leads to a more resistant phenotype
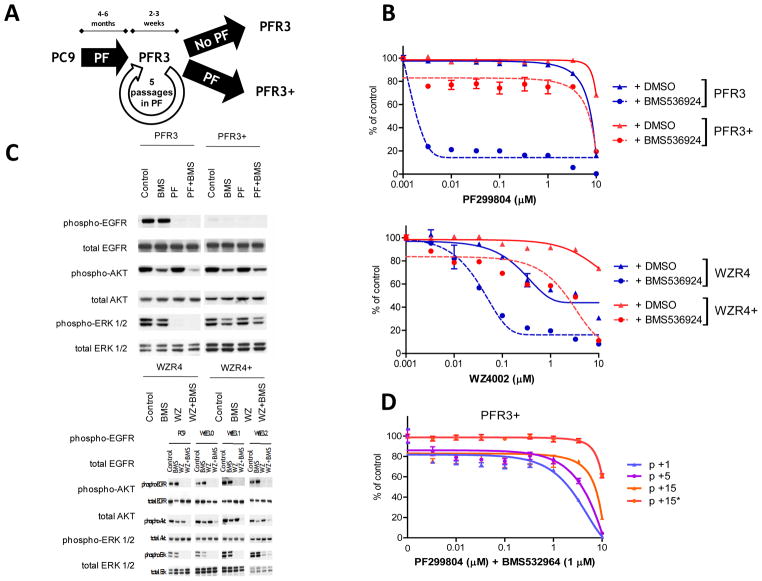
Following the generation of PFR and WZR cells by prolonged exposure to PF299804 and WZ4002 respectively we cultured the cells in drug free media for > 20 passages. These cells retained their resistant phenotype, mediated by IGF1R signaling, despite being cultured in the absence of either PF299804 or WZ4002. In parallel, we also continued to culture the cells in the presence of either PF299804 or WZ4002. As EGFR kinase inhibitors are sometimes clinically administered to patients despite the development of drug resistance as defined by standard radiographic criteria, we wanted to explore, using these cell line models, whether additional mechanisms of resistance might emerge using this approach (Fig 4A). These resistant cells are called PFR3+ and WZR4 + to reflect persistent drug exposure (Fig. 4A). Surprisingly, we observed that both the PFR3+ or WZR4+ cells had a different phenotype from their PFR3 and WZR4 counterparts. Unlike PFR3 and WZR4, the PFR3+ and WZR4+ cells were no longer sensitive to the combination of BMS536924 and either PF299804 or WZ4002 (Fig 4B). There were no differences in pIGF1R in PFR3 + and WZR4+ cells compared to their parental counterparts (Fig. S6). Furthermore, in the PFR3+ and WZR4+ cells, neither PF299804 nor WZ4002 inhibited ERK1/2 phosphorylation unlike in the PFR3 or WZR4 cells (Fig 4C). These observations are similar to those in the PFR5 cells (Figs. 1C and 2A). No secondary mutations in NRAS, KRAS, HRAS, BRAF, MEK1, MEK2, MAPK1or MAPK3were detected in these cells (data not shown). We also generated PFR5+ cells by continued exposure of the PFR5 cells to PF299804. The PFR5+and PFR5 and cells were similar in their growth characteristics, following drug treatment (Fig S7). The removal of PF299804 from the culture media did not change the resistance phenotype in the PFR3+ cells (Fig. 4D).
Figure 4. Prolonged drug exposure leads to emergence of a more drug resistant subclone.
A. Schema for prolonged culture. The PF R3+ cells were obtained by prolonged culture to PF299804 while PFR3 cells were cultured in the absence of drug. Similar strategy was used for WZR cells B. PFR3+ and WZR4+ cells are resistant to combination of PF299804 or WZ4002 and BMS536924. The indicated cell lines were treated with increasing concentrations of PF299804 alone, WZ4002 alone or in combination with BMS536924 (1 μM) and viable cells were measured after 72 hours of treatment and plotted relative to untreated controls. C. The indicated cell lines were treated with PF299804 (1 μM) alone, WZ4002 (1 μM) alone, BMS536924 (1 μM) alone or with the combination of both agents for 6 hours. Cell extracts were immunoblotted to detect the indicated proteins. D. Resistance in PFR3+ cells to the combination of BMS536924 and PF299804 is maintained after 15 passages in a medium with PF299804 (p15) and after10 more passages in a medium with no PF299804 (p15*).
In order to understand why PFR+ cells emerged so rapidly with continued drug exposure we analyzed the proliferation rates of PFR3 and PFR3+ cells in culture. Compared to the PFR3 cells, the PFR3+ cells had a faster rate of proliferation (Fig. 5A). In addition, the PFR3+ cells formed greater numbers of colonies in a clonogenic assay in the presence, but not in the absence, of PF299804 (Fig 5A). These differences may be due to ability of PF299804 to still inhibitERK1/2 signaling, a known mediator of cell proliferation, in the PFR3 but not in the PFR3+ cells (Figs. 1C and 4C) thus allowing the latter cell population to emerge even in the presence of drug.
Figure 5. PFR+ and WZR+ cells exhibit ERK activation and are sensitive to the addition of a MEK inhibitor.
A. PFR3+ cells grow faster than their drug sensitive (PFR3) counterparts. Growth curves for PFR3 and PFR3+ cells were obtained by counting the number of viable cells at the indicated time points in the presence of PF299804 (1 μM). Colonies were counted after 15 days of treatment with or without PF299804 (1 μM). B. Addition of CI -1040 (1 μM) partly restores sensitivity of PFR3+ and WZR4+ cells toPF299804 and WZ4002 respectively in combination with BMS536924 in both short term (top) and clonogenic (bottom) assays C. Addition of BMS536924 or CI-1040 suppresses emergence of resistant clones induced by prolonged exposure of parental PC9 cells to PF299804 or WZ4002. Cells were plated in a96 -well plates and cultured up to 3 months in the presence of indicated drugs (1 μM).
To understand why the PFR3+ cells had a faster rate of proliferation (Fig. 5A) and persistent ERK1/2 signaling in the presence of PF299804 (Fig. 4C), we performed gene expression analyses comparing the PFR3 and PFR3+ cells. These studies revealed that several phosphatases, including members of the dual specific phosphatase (DUSP) family, that normally inhibit ERK1/2 signaling, were dowregulated in the PFR3+ compared with the PFR3 cells. DUSP6 demonstrated the greatest degree of downregulation (7 fold) between the PFR3+ and PFR cells (Fig. S8A). By western blotting, we observed decreased levels of DUSP6 in both in the PFR3+ and PFR5 cells compared to PC9 and PFR3 cells (Fig S8B). We further confirmed that DUSP6 expression was dependent on ERK1/2 signaling in various lung cancer cell lines, including PC9 and PFR3 cells (Fig. S8B and S8C). However, in PFR+ cells, levels of DUSP6 remained low, despite high levels of ERK1/2 phosphorylation, suggesting a disconnection in the negative feedback (Fig. S8B). We expressed DUSP6 in the PFR3+ cells to determine whether re-expression could restore the sensitivity of the PFR3+ cells to PF29904/BMS536924. However, despite adequate expression of DUSP6, the cells remained resistant to the drug combination (data not shown).
Given the high levels of ERK1/2 phosphorylation, and the gene expression studies demonstrating downregulation of multiple phosphatases that may regulate ERK1/2 signaling, we evaluated whether pharmacologic inhibition of ERK1/2 signaling using CI-1040 could restore sensitivity to PF299804/BMS536924. In short term assays, the addition of the MEK inhibitor CI-1040 partially restored sensitivity to PF299804/BMS536924 or WZ4002/BMS536924 in the PFR3+ and WZR4+ cells, respectively. The effects of CI-1040 were more dramatic in clonogenic assays where significant and almost complete inhibition of colony formation was observed (Fig. 5B). However, despite inhibition of ERK 1/2 signaling in the PFR3+ cells, this did not result in apoptosis and only minimally so in WZR 4+ cells (Fig. S9A and S9B).
Our studies suggest that resistance to irreversible EGFR inhibitors can be mediated by IGF1R signaling. This however appears to be a transient process as additional drug exposure leads to activation of ERK1/2 signaling. An alternative therapeutic strategy to treating drug resistance is to prevent it from emerging especially if multiple different drug resistant clones are present (such as PFR3 and PFR5) or emerge as a result of persistent drug treatment (PFR3 and PFR3+). Given that the role of IGF1R and ERK1/2 signaling in this process we wished to determine whether their inhibition could delay or prevent the emergence of drug resistant clones. We thus treated the parental EGFR TKI sensitive PC9 cells with either irreversible EGFR TKIs alone, BMS536924 alone, CI-1040 alone or with drug combinations (Fig. 5C). Although resistant colonies emerged following 3 month exposure to Irreversible EGFR TKIs alone, BMS536924 alone, CI-1040 alone we were unable to isolate any clones from the combination of PF299804/BMS536924, WZ4002/BMS536924 or WZ4002/CI-1040 (Fig. 5C).
DISCUSSION
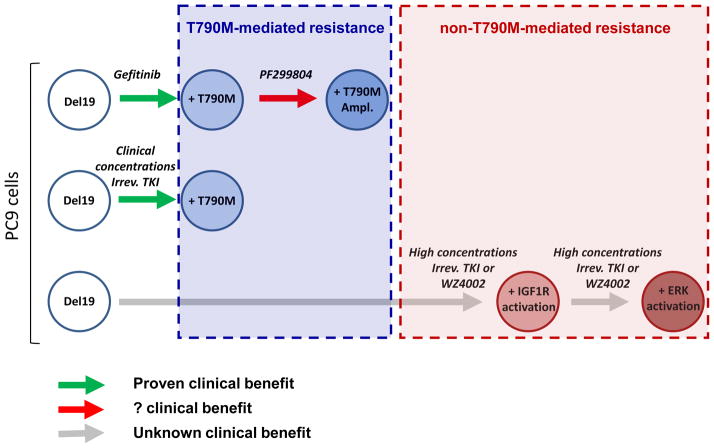
Current strategies to overcome EGFR T790M, the most common mechanism of acquired resistance to gefitinib and erlotinib, have been relatively ineffective in EGFR mutant NSCLC patients (19, 20). In the present study we used two independent methods to inhibit EGFR T790M in model systems. These include a mutant selective EGFR kinase inhibitor, WZ4002, and high concentrations of a clinical irreversible EGFR kinase inhibitor PF299804. With both agents, we have previously demonstrated that they can inhibit the growth of cancers harboring an established EGFR T790M mutation (11, 23). UsingPF299804, inhibition of EGFR T790M occurs only at high concentrations (> 1 μM) which may not be achieved in patients using current continuous dosing regimens (11, 22). However, alternative dosing strategies, such as intermittent pulsatile dosing, may achieve sufficient PF299804 concentrations to inhibit T790M (11). Importantly, using both WZ4002 and high concentrations of PF299804 we prevent the emergence of EGFR T790M in the PC9 cells which multiple investigators have reproducibly demonstrated to develop EGFR T790M following exposure to gefitinib, erlotinib or to clinical concentrations of irreversible EGFR inhibitors (12, 13, 17, 18). This observation suggests that, if applied clinically, lung cancer patients may achieve a longer progression free survival than is currently possible with gefitinib or erlotinib.
A critical goal of our studies was to understand how cancers develop drug resistance if we are able to fully inhibit EGFR T790M. Intriguingly none of our drug resistant clones harbored a secondary mutation in EGFR. Previous studies have demonstrated that mutations in the site of covalent binding (C797) can confer resistance to irreversible EGFR TKIs including WZ4002 (17, 23). Why we do not observe this mutation using our drug exposure model of resistance remains to be determined.
We found that PC9 cells resistant to eitherPF299804 orWZ4002 maintain PI3K/AKT signaling, through activation of IGF1R signaling which is in turn mediated by downregulation of IGFBP3 (Figs. 1–3). This mechanism of acquired resistance has previously been reported for models of gefitinib sensitive EGFR wild type cancers (using A431 cells) (29). Moreover, Sharma and colleagues observed that PC9 cells could acquire transient resistance to gefitinib through a chromatin change that is reversible with IGF1R inhibitors (32). Our resistant cells do not harbor this resistance mechanism (Fig S4). IGF1R signaling as a mechanism of drug resistance in EGFR mutant cancer has not been previously reported with reversible or irreversible EGFR inhibitors. One potential reason for these observations is, until recently, the lack of efficacious therapeutic strategies against EGFR T790M. Several studies suggest that EGFR T790M pre-exists in treatment naïve cancers and undergoes a selection process following drug exposure (33) (34). When EGFR T790M is present in just a few rare clones, such as the PC9 cells, PF299804 effectively prevents its emergence when used at high concentrations (Fig. 6). In contrast, when EGFR T790M is already present, inhibition is only transient followed by selection for EGFR T790M amplified PF299804 resistant cells (Fig. 6) (11). Thus outgrowth of an EGFR T790M containing clone may be an easier or faster means for an EGFR mutant cancer to develop drug resistance than activating additional signaling pathways. This hypothesis is supported by recent clinical studies that demonstrated no increase in progression free survival by the addition of the IGFIR antibody R1507 to erlotinib compared to erlotinib alone (35).
Figure 6. Mechanisms of resistance to EGFR TKIs in PC9 cells.
Treatment of PC9 cells with reversible quinazoline-based TKIs (upper line) or clinical concentrations of irreversible TKI (middle line) leads to emergence of the EGFR T790M mutation as a mechanism of resistance. Treatment with a T790M -potent EGFR TKI (bottom line) prevents emergence of the EGFR T790M mutation and results in a sequential acquisition of non-T790M resistance mechanisms involving IGF1R and MAPK pathways.
Models of drug resistance to EGFR TKIs have typically identified a single molecular event including EGFR T790M and MET amplification (12, 24) Here, we find that the resistance to PF299804 and WZ4002 occurs through a more dynamic and multistep process which could be more reflective of clinical drug resistance. These processes can also occur rapidly as highlighted by the PFR5 cells (Fig 1C) which are similar to the PFR3+ cells but different from the PFR3 cells. Our data suggest that the first step is required for the second step to occur, since we found that PFR3+ emerged from prolonged exposure of PFR3 cells to PF299804 and inhibition of IGF1R prevented emergence of PFR3+ cells from PC9 cells (Fig. 5B). Resistance acquired at each step was maintained overtime, suggesting that these mechanisms are permanent, in contrast to the mechanism in the drug -tolerant tumor cells that have been previously described (32). However, with additional drug exposure, in the second step, EGFR could no longer inhibit MAPK signaling and this pathway becomes activated through an EGFR independent mechanism (Figs. 1C, 1D and 4C). These cells had a proliferative advantage over the “first-step”-resistant ones, which likely contributed to their emergence upon continued therapeutic pressure (Fig 5A). Our findings further imply that although activation of the PI3K/AKT pathway is required for resistance to EGFR TKI, activation of the MAPK pathway may also offer a proliferative advantage to these cells. However, the resistance is more complex, as despite inhibiting EGFR and downstream pathways, the PFR3+ cells do not die (Fig. S9A and S9B). Thus the phenotype may involve more than one process including the inability to undergo apoptosis; a mechanism recently reported for crizotinib resistance (36). These findings highlight the potential clinical challenges in developing therapeutic strategies against just one mechanism of drug resistance.
An alternative clinical strategy is to identify the spectrum of potential mechanisms of acquired drug resistance and to inhibit them before they emerge in combination with EGFR inhibitors (37). By combining an effective strategy to inhibit EGFR T790M with either an IGF1R or MEK inhibitor we prevented the emergence of drug resistant clones using this model system. Either one or both of these may be an effective clinical approach, lead to prolonged progression free survival for EGFR mutant NSCLC patients, and should be tested in future clinical trials.
Supplementary Material
Acknowledgments
This study is supported by grants from the National Institutes of Health RO1CA114465 (P.A.J.), R01CA135257 (P.A.J.), the National Cancer Institute Lung SPORE P50CA090578 (P.A.J. and K.-K.W.), the College des Enseignants de Pneumologie (A.B.C.) and the Fondation de France (A.B.C.).
Footnotes
On behalf of all authors on this manuscript, following conflicts of interest that need to be disclosed. All authors have completed separate conflict of interest forms.
P.A. Jänne –
Consultant/Advisory Board
(Minor $10,000 or less)
Astra Zeneca, Boehringer Ingelheim, Pfizer, Roche, Genentech, Sanofi
(Major $10,000 or more)
Lab Corp
Inventor on Dana Farber Cancer Institute owned patent on WZ4002 (Minor $10,000 or less)
J.G. Christensen -
Employee of Pfizer and receives stock from Pfizer
(Major $10,000 or more)
N.S. Gray -
Inventor on Dana Farber Cancer Institute owned patent on WZ4002 (Minor $10,000 or less)
A.B. Cortot, C.E. Repellin, T. Shimamura, M. Capelletti, K. Zejnullahu, D. Ercan, and K.-K. Wong
No conflicts of interest
References
- 1.Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 2.Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–39. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 3.Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A. 2004;101:13306–11. doi: 10.1073/pnas.0405220101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–57. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 5.Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12:735–42. doi: 10.1016/S1470-2045(11)70184-X. [DOI] [PubMed] [Google Scholar]
- 6.Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012 doi: 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- 7.Engelman JA, Janne PA. Mechanisms of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small cell lung cancer. Clin Cancer Res. 2008;14:2895–9. doi: 10.1158/1078-0432.CCR-07-2248. [DOI] [PubMed] [Google Scholar]
- 8.Oxnard GR, Arcila ME, Sima CS, Riely GJ, Chmielecki J, Kris MG, et al. Acquired resistance to EGFR tyrosine kinase inhibitors in EGFR-mutant lung cancer: distinct natural history of patients with tumors harboring the T790M mutation. Clin Cancer Res. 2011;17:1616–22. doi: 10.1158/1078-0432.CCR-10-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3:75ra26. doi: 10.1126/scitranslmed.3002003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arcila ME, Oxnard GR, Nafa K, Riely GJ, Solomon SB, Zakowski MF, et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin Cancer Res. 2011;17:1169–80. doi: 10.1158/1078-0432.CCR-10-2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ercan D, Zejnullahu K, Yonesaka K, Xiao Y, Capelletti M, Rogers A, et al. Amplification of EGFR T790M causes resistance to an irreversible EGFR inhibitor. Oncogene. 2010;29:2346–56. doi: 10.1038/onc.2009.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogino A, Kitao H, Hirano S, Uchida A, Ishiai M, Kozuki T, et al. Emergence of epidermal growth factor receptor T790M mutation during chronic exposure to gefitinib in a non small cell lung cancer cell line. Cancer Res. 2007;67:7807–14. doi: 10.1158/0008-5472.CAN-07-0681. [DOI] [PubMed] [Google Scholar]
- 13.Ichihara E, Ohashi K, Takigawa N, Osawa M, Ogino A, Tanimoto M, et al. Effects of vandetanib on lung adenocarcinoma cells harboring epidermal growth factor receptor T790M mutation in vivo. Cancer Res. 2009;69:5091–8. doi: 10.1158/0008-5472.CAN-08-4204. [DOI] [PubMed] [Google Scholar]
- 14.Kwak EL, Sordella R, Bell DW, Godin-Heymann N, Okimoto RA, Brannigan BW, et al. Irreversible inhibitors of the EGF receptor may circumvent acquired resistance to gefitinib. Proc Natl Acad Sci U S A. 2005;102:7665–70. doi: 10.1073/pnas.0502860102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li D, Ambrogio L, Shimamura T, Kubo S, Takahashi M, Chirieac LR, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene. 2008 doi: 10.1038/onc.2008.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engelman JA, Zejnullahu K, Gale CM, Lifshits E, Gonzales AJ, Shimamura T, et al. PF00299804, an irreversible pan-ERBB inhibitor, is effective in lung cancer models with EGFR and ERBB2 mutations that are resistant to gefitinib. Cancer Res. 2007;67:11924–32. doi: 10.1158/0008-5472.CAN-07-1885. [DOI] [PubMed] [Google Scholar]
- 17.Godin-Heymann N, Ulkus L, Brannigan BW, McDermott U, Lamb J, Maheswaran S, et al. The T790M “gatekeeper” mutation in EGFR mediates resistance to low concentrations of an irreversible EGFR inhibitor. Mol Cancer Ther. 2008;7:874–9. doi: 10.1158/1535-7163.MCT-07-2387. [DOI] [PubMed] [Google Scholar]
- 18.Chmielecki J, Foo J, Oxnard GR, Hutchinson K, Ohashi K, Somwar R, et al. Optimization of Dosing for EGFR-Mutant Non-Small Cell Lung Cancer with Evolutionary Cancer Modeling. Sci Transl Med. 2011;3:90ra59. doi: 10.1126/scitranslmed.3002356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sequist LV, Besse B, Lynch TJ, Miller VA, Wong KK, Gitlitz B, et al. Neratinib, an irreversible pan-ErbB receptor tyrosine kinase inhibitor: results of a phase II trial in patients with advanced non-small-cell lung cancer. J Clin Oncol. 2010;28:3076–83. doi: 10.1200/JCO.2009.27.9414. [DOI] [PubMed] [Google Scholar]
- 20.Miller VA, Hirsh V, Cadranel J, Chen Y-M, Park K, Kim S-W, et al. Phase IIB/III Double-Blind Randomized Trial of Afatinib (BIBW2992, an Irreversible Inhibitor of EGFR/HER1 and HER2) + Best Supportive Care (BSC) Versus Placebo + BSC in Patients with NSCLC Failing 1–2 Lines of Chemotherapy and Erlotinib or Gefitinib (LUX-LUNG 1) Annals of Oncology. 2010;21:LBA1. [Google Scholar]
- 21.Eskens FA, Mom CH, Planting AS, Gietema JA, Amelsberg A, Huisman H, et al. A phase I dose escalation study of BIBW 2992, an irreversible dual inhibitor of epidermal growth factor receptor 1 (EGFR) and 2(HER2) tyrosine kinase in a 2 -week on, 2-week off schedule in patients with advanced solid tumours. Br J Cancer. 2008;98:80–5. doi: 10.1038/sj.bjc.6604108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Janne PA, Boss DS, Camidge DR, Britten CD, Engelman JA, Garon EB, et al. Phase I dose-escalation study of the pan-HER inhibitor, PF299804, in patients with advanced malignant solid tumors. Clin Cancer Res. 2011;17:1131–9. doi: 10.1158/1078-0432.CCR-10-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou W, Ercan D, Chen L, Yun CH, Li D, Capelletti M, et al. Novel mutant-selective EGFR kinase inhibitors against EGFR T790M. Nature. 2009;462:1070–4. doi: 10.1038/nature08622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–43. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 25.Ono M, Hirata A, Kometani T, Miyagawa M, Ueda S, Kinoshita H, et al. Sensitivity to gefitinib (Iressa, ZD1839) in non-small cell lung cancer cell lines correlates with dependence on the epidermal growth factor (EGF) receptor/extracellular signal-regulated kinase 1/2 and EGF receptor/Akt pathway for proliferation. Mol Cancer Ther. 2004;3:465–72. [PubMed] [Google Scholar]
- 26.Tracy S, Mukohara T, Hansen M, Meyerson M, Johnson BE, Janne PA. Gefitinib induces apoptosis in the EGFRL858R non-small-cell lung cancer cell line H3255. Cancer Res. 2004;64:7241–4. doi: 10.1158/0008-5472.CAN-04-1905. [DOI] [PubMed] [Google Scholar]
- 27.Tomii K, Tsukuda K, Toyooka S, Dote H, Hanafusa T, Asano H, et al. Aberrant promoter methylation of insulin-like growth factor binding protein-3 gene in human cancers. Int J Cancer. 2007;120:566–73. doi: 10.1002/ijc.22341. [DOI] [PubMed] [Google Scholar]
- 28.Carretero J, Shimamura T, Rikova K, Jackson AL, Wilkerson MD, Borgman CL, et al. Integrative genomic and proteomic analyses identify targets for Lkb1-deficient metastatic lung tumors. Cancer Cell. 2010;17:547–59. doi: 10.1016/j.ccr.2010.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guix M, Faber AC, Wang SE, Olivares MG, Song Y, Qu S, et al. Acquired resistance to EGFR tyrosine kinase inhibitors in cancer cells is mediated by loss of IGF-binding proteins. J Clin Invest. 2008;118:2609–19. doi: 10.1172/JCI34588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wittman M, Carboni J, Attar R, Balasubramanian B, Balimane P, Brassil P, et al. Discovery of a (1H-benzoimidazol-2-yl)-1H-pyridin-2-one (BMS-536924) inhibitor of insulin-like growth factor I receptor kinase with in vivo antitumor activity. J Med Chem. 2005;48:5639–43. doi: 10.1021/jm050392q. [DOI] [PubMed] [Google Scholar]
- 31.Ji Q-s, Mulvihill MJ, Rosenfeld-Franklin M, Cooke A, Feng L, Mak G, et al. A novel, potent, and selective insulin-like growth factor-I receptor kinase inhibitor blocks insulin-like growth factor-I receptor signaling in vitro and inhibits insulin-like growth factor-I receptor–dependent tumor growth in vivo. Molecular Cancer Therapeutics. 2007;6:2158–67. doi: 10.1158/1535-7163.MCT-07-0070. [DOI] [PubMed] [Google Scholar]
- 32.Sharma SV, Lee DY, Li B, Quinlan MP, Takahashi F, Maheswaran S, et al. A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell. 2010;141:69–80. doi: 10.1016/j.cell.2010.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maheswaran S, Sequist LV, Nagrath S, Ulkus L, Brannigan B, Collura CV, et al. Detection of mutations in EGFR in circulating lung-cancer cells. N Engl J Med. 2008;359:366–77. doi: 10.1056/NEJMoa0800668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Su KY, Chen HY, Li KC, Kuo ML, Yang JC, Chan WK, et al. Pretreatment epidermal growth factor receptor (EGFR) T790M mutation predicts shorter EGFR tyrosine kinase inhibitor response duration in patients with non-small-cell lung cancer. J Clin Oncol. 2012;30:433–40. doi: 10.1200/JCO.2011.38.3224. [DOI] [PubMed] [Google Scholar]
- 35.Ramalingam SS, Spigel DR, Chen D, Steins MB, Engelman JA, Schneider CP, et al. Randomized phase II study of erlotinib in combination with placebo or R1507, a monoclonal antibody to insulin-like growth factor-1 receptor, for advanced-stage non-small-cell lung cancer. J Clin Oncol. 2011;29:4574–80. doi: 10.1200/JCO.2011.36.6799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Katayama R, Shaw AT, Khan TM, Mino-Kenudson M, Solomon BJ, Halmos B, et al. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung Cancers. Sci Transl Med. 2012;4:120ra17. doi: 10.1126/scitranslmed.3003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mumenthaler SM, Foo J, Leder K, Choi NC, Agus DB, Pao W, et al. Evolutionary Modeling of Combination Treatment Strategies To Overcome Resistance to Tyrosine Kinase Inhibitors in Non-Small Cell Lung Cancer. Mol Pharm. 2011 doi: 10.1021/mp200270v. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.