Abstract
Background: The anxiety associated with unfamiliar surroundings, the disorientation and mental confusion, and the social isolation that accompanies dementia can often create increased stress for people living in long-term care settings. Such a response is thought to affect the autonomic nervous system and result in emotional and physical symptoms of distress that may be manifested as agitation. There is the potential for such distress to influence the physiological response and in particular Blood Pressure and Heart Rate. A relaxation intervention such as massage may influence the physiological stress response.
Methods: This randomized controlled trial aimed to compare the effect of foot massage (FM) versus a control activity (quiet presence, QP) on physiological stress response (i.e., blood pressure [BP] and heart rate [HR]) in people living with moderate-to-severe dementia in long-term-care settings.
Results: Fifty-three residents were randomized to intervention (10-minute FM) or control group (QP). While the FM group experienced a greater reduction in HR than the control group, these reductions were not significantly different between groups (p=0.83; see Table 1), or across time (p=0.46). Both groups experienced a reduction in systolic BP and diastolic BP, while the mean reduction in systolic BP was greater for those in the FM group.
Conclusions: While the findings do not provide strong support for FM, the finding that both conditions allowed the person with dementia to rest in the presence of another human being is of importance in the care of people with dementia. The close presence of another person may in fact promote relaxation and therefore improve BP and HR measures.
Introduction
Dementia is the term used to refer to a set of symptoms for a range of illnesses that are characterized by a progressive impairment of an individual's functioning.1 This includes a decline in mood and cognitive functioning and the emergence of behavioral problems such as sleep–wake and rest–activity pattern disturbance. The specific determinants of such disturbance remain unclear. Predisposing factors are related to internal features such as personality and functional and cognitive impairment, and external features including characteristics of the environment.2 The anxiety associated with unfamiliar surroundings, the disorientation and mental confusion, and the social isolation that accompanies dementia can often create increased stress for people living in long-term care (LTC) settings.3 Such a response is thought to affect the autonomic nervous system and result in emotional and physical symptoms of distress,4 and as a result the individual can experience a stress response.
According to Oken and colleagues,5 “physiologic responses to stress activate the hypothalamic-pituitary-adrenal and the locus coeruleus-norepinephrine-sympathetic nervous system pathways” (p. 191), and this is determined as a stress response. Most studies that explore the stress response focus on expected elevations of physiological response, such as elevated blood pressure (BP) and heart rate (HR). However, both elevated and blunted physiological responses have been documented in relation to a stress response.6–8 As either arousal or inhibition of the stress response as a result of stress is likely, it is therefore important to consider both high and low levels of physiological responses to stress.
Recent studies have demonstrated the influence of relaxation interventions on a reduction in BP and HR.9,10 There is, however, a paucity of literature related to the stress response in people with dementia. In people with late-stage dementia where communication is challenged, physiological measures may be one means of understanding the outcomes of interventions that target a relaxation response in people with dementia.8 This article offers a preliminary understanding of the physiological response of people with late-stage dementia to a foot massage (FM) intervention.
There is a growing body of literature suggesting that complementary and alternative therapies may be effective treatments for reducing stress and inducing comfort in people with dementia. 9–11 Massage is one such treatment that is thought to be beneficial (Brewer, S.G. 2001. Massage of feet: A pain control option. PhD diss., Indiana University). and has been used within a medical context since the 1800s.12 Massage has been found to promote a higher level of mental and emotional satisfaction (including alleviating anxiety and depression, improving relaxation) and to improve health and physical well-being (including reducing pain, BP, pulse rate, and improved sleep patterns). 13 In addition, a number of studies have found massage to be beneficial to the skeletal muscle, digestive, lymphatic, respiratory, nervous, and circulatory systems.14–17 This growing body of literature has reported positively on the effect of massage on stress.
Studies to date suggest that massage may also have a positive effect on producing relaxation in older people with dementia16–19 and may reduce physically agitated behavior such as pacing, wandering, and resisting care, but not verbal agitation,18 and improve residents' appetite and reduce insomnia and communication problems.18 Physiological effects of massage such as a decrease in pulse and respiration and an increase in body temperature have also been demonstrated.20
Physiological models suggest that the sensation of massage has a calming and reassuring influence and the subsequent production of oxytocin reduces discomfort and agitation and improves mood, and this may have an influence on physiological measures such as BP and HR.13 Psychological models suggest that massage helps such individuals to retain a sense of meaningful and reassuring communication even when words fail and may help to activate memories.21 Importantly, no negative effects have been identified with massage.
Methods
The aim of this study was to compare the effect of FM versus a control activity (quiet presence, QP) on physiological stress response (i.e., BP and HR) in people living with moderate-to-severe dementia in LTC. It was hypothesized that participants in the FM condition would experience a greater decline in BP and HR compared to participants in the QP group.
Trial design
This study was originally designed and conducted as a randomized controlled trial with within-subjects, crossover design, so that participants could experience both the FM intervention and the QP control group. The trial was registered with the Australian and New Zealand Trials Registry (ACTRN 1262000658819) and was granted ethical approval by the University Human Research Ethics Committee.
Settings
Five LTC settings, located in South-East Queensland (Australia), were nominated by the partner aged-care organization as suitable research sites. The involvement of five facilities was necessary to overcome the difficulties in recruiting and retaining people with dementia as demonstrated in our pilot study.19 The chosen facilities are similar in respect to philosophy of care, staffing, and frailty of resident. All of the facilities provided low (assisted), high (nursing home), and respite care to both male and female residents.
Participants
A target sample of 60 residents was planned based on power of 0.95, effect size of 0.59, and α of 0.05, and allowing for 10% attrition. The two Clinical Coordinators and the Nurse Manager at the LTC facilities identified potential participants for the current study. Residents were eligible to participate if they had
1. An age of 65 or older
2. Permanent residence in one of the chosen facilities for at least 2 months
3. A diagnosis of dementia, or met the criteria for probable dementia of Alzheimer's type22
4. A Mini-Mental State Exam score <1823
5. A Pittsburgh Agitation Scale (PAS) score >3 during each day over a period of 1 week24
6. No specific medical-related contraindications
7. Two feet, excluding artificial legs
8. Informed consent (i.e., authority received from residents themselves and/or relatives and health attorney, to join the research).
Randomization and blinding
A member of the research team, blinded to the identity of eligible participants and not involved with data collection, used a computer program to undertake the permuted-block randomization process, with block size set at six. Participants were allocated to either the FM intervention or QP control group.
Interventions
The FM intervention and QP control sessions were administered to participants individually, in the resident's bedroom with a closed door displaying a “Do not disturb” sign. Staff members were also asked to refrain from attending participants' rooms during the session to maintain blinding, enhance privacy, and create a more conducive, therapeutic environment. Each session lasted for 10 minutes and the sessions were held five times a week, Monday to Friday, from 1:00 pm to 4:00 pm, for a period of 3 weeks. All participants had the opportunity to receive 15 sessions each for the FM intervention and the QP control.
The FM intervention research assistants (RAs), who were practicing massage therapists, received training in the implementation of the FM protocol. The QP RAs, who were nursing students, received training in the delivery of QP. Intervention RAs were also trained in how to communicate with people with dementia and in measurement of BP and HR. The training and the implementation of both conditions followed a standardized procedure manual. A Project Manager oversaw the study and monitored the delivery of the FM intervention at regular intervals. Spot checks on the massage techniques were also performed in the first 2 weeks of the intervention.
In each intervention session, the participant received a standardized 5-minute massage on each foot (10 minutes in total). The massage involved a light-pressure massage with long, gliding, rhythmical strokes and flexion, extension, and rotation of the toes, foot, and ankle. Unscented Sorbolene (8–10 mL, cetomacrogol aqueous cream) was applied as a lubricant for the massage.
In the control sessions, the QP RAs sat silently near the participant's feet for 10 minutes without talking or making physical contact with the resident. The QP RAs were instructed that no deliberate conversation or touching was to occur during this time. The purpose of the QP condition was to isolate the effect of the FM from any potential, extraneous effects of additional attention or company provided by the RA.
Data collection
The intervention RAs measured each participant's systolic BP, diastolic BP, and HR immediately before and after each session. These physiological markers of stress were measured with a Digital Wrist Blood Pressure Monitor (model #6045) from American Diagnostic Corporation, America. This equipment was chosen because of its reliability of automatic BP measurement and was considered to be less intrusive when compared with an elbow brachial artery BP cuff.
Data analysis
Initial analyses indicated a significant carry-over effect across the washout period (p>0.05), so the data were analyzed as a parallel-groups randomized controlled trial.25 This meant that only the data from baseline and post-test 1 were analyzed. Thus, for the purpose of analysis, the study assumes a parallel-group, randomized controlled trial design.
Data were entered into SPSS Statistics Version 19.0 (SPSS Inc., Chicago, IL) for analysis. Basic frequency analyses were run on all demographics and outcome measures to inspect the initial spread of responses, check for outliers, and determine the extent of missing data. All outliers and missing data were checked against source data to ensure accuracy of the entries. An intention-to-treat analysis was applied, so that all randomized participants were included. Any missing values in the outcome variables were imputed with the respective series mean produced in SPSS. Physiological measures vary greatly among individuals and across time; thus, the series mean approach was used, as it is a more conservative estimate for the missing data. Analyses were performed on both the original dataset and the imputed dataset. Results were consistent across the two datasets, so the results from the imputed dataset are reported.
Change scores were calculated for systolic BP, diastolic BP, and HR across each of the 15 10-minute FM or QP sessions (i.e., post- minus pre-intervention). A negative change score indicates a reduction in the physiological measures, whereas a positive change score denotes an increase after intervention. Weekly mean change scores were then calculated for each of the 3 weeks by averaging across the five sessions (i.e., sum of change scores in a week divided by 5). Three mixed-design analyses of variance (ANOVAs) were undertaken to explore differences in the physiological effect of FM versus QP on participants' BP and HR across the 3 weeks. All statistical tests were considered significant at the level p<0.05.
Results
Sample characteristics
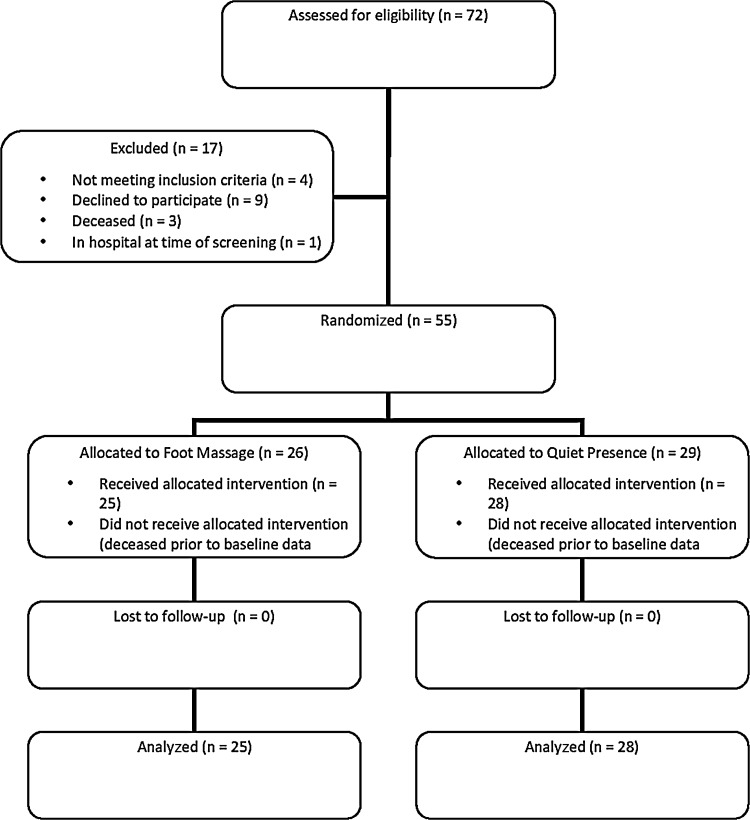
Seventy-two (72) people were screened and 55 were deemed eligible. Two (2) participants died prior to baseline data collection (Fig. 1). Data from the 53 residents (18 men, 35 women) randomized to intervention or control group were analyzed. Participants' ages ranged from 74 to 103 years, with a mean of 86.51 years (σ=7.13). Twenty-five (25) participants were assigned to the FM intervention, while 28 participants were in the QP condition. Post-hoc analyses showed that there were no significant differences between the FM and the QP group in terms of age (p=0.16) and gender (p=0.50). However, the FM group differed significantly on pre-intervention systolic BP (t (51)=2.60, p=0.01) when compared with the QP group. The use of change scores therefore eliminates the influence of the between-group difference. Overall, there was 0.6% missing data in the study, with seven individual sessions having incomplete data. Missing data occurred as a result of participants refusing to have their physiological measures taken.
FIG. 1.
Participant flow: Recruitment, allocation, and retention.
Outcome measures
Three two-way mixed-measures ANOVA were performed on the change scores for HR, systolic BP, and diastolic BP with time (i.e., week 1, 2, and 3) and group (i.e., FM and QP) as the independent variables.
Change scores in HR
While the FM group experienced a greater reduction in HR than the QP group, these reductions were not significantly different between groups (p=0.83; Table 1), or across time (p=0.46; Table 2).
Table 1.
Change Scores in Blood Pressure and Heart Rate in the Two Groups
| Mean change scores (σ) | Effect of group | ||||
|---|---|---|---|---|---|
| Dependent variable | Foot massage | Quiet presence | F-Value | Significance (p=) | Partial η2 |
| Heart rate | −0.89 (0.75) | −0.67 (0.71) | 0.05 | 0.83 | <0.01 |
| Systolic blood pressure | −9.34 (1.65) | −6.22 (1.55) | 1.90 | 0.17 | 0.034 |
| Diastolic blood pressure | −2.38 (1.14) | −3.38 (1.07) | 0.41 | 0.53 | 0.01 |
Total n=53; foot massage n=25; quiet presence n=28; σ=standard deviation. Change scores were calculated for blood pressure (systolic and diastolic) and heart rate for each of the 15 foot massage or quiet presence sessions (i.e., post- minus pre-intervention). An overall mean change score was then calculated for the foot massage and silent resting groups for each measure (i.e., sum of change scores divided by 15).
Table 2.
Change Scores in Blood Pressure and Heart Rate Across the Three-Week Intervention Period
| Mean change scores (σ) | Effect of group | |||||
|---|---|---|---|---|---|---|
| Dependent variable | Week 1 | Week 2 | Week 3 | F-Value | Significance (p=) | Partial η2 |
| Heart rate | −1.37 (0.75) | −1.33 (0.92) | 0.35 (1.36) | 0.78 | 0.46 | 0.02 |
| Systolic blood pressure | −14.24 (1.57) | −4.66 (2.42) | −6.54 (2.325) | 15.79 | <0.01* | 0.24 |
| Diastolic blood pressure | −1.32 (1.30) | −0.77 (1.47) | −6.56 (1.23) | 5.77 | 0.01 | 0.10 |
p<0.05; σ=standard deviation; change scores were calculated for blood pressure (systolic and diastolic) and heart rate for each of the 15 foot massage or quiet presence sessions (i.e., post- minus pre-intervention). A weekly mean change score was then calculated for the foot massage and silent resting groups across the three weeks of intervention (i.e., sum of change scores in a week divided by 5).
Change scores in BP
Mauchly's tests indicated that the assumption of sphericity was violated only in the analyses of diastolic BP; thus, degrees of freedom were corrected by using Huynh-Feldt estimates of sphericity (ξ=0.77).
Both groups experienced a reduction in systolic BP and diastolic BP, while the mean reduction in systolic BP was greater for those in the FM group (Table 1). However, no significant difference was found between the two groups (p=0.17 for systolic BP, and p=0.53 for diastolic BP).
There was a significant difference across time regardless of groups for both systolic BP (F (2, 102)=15.79, p<0.01, partial η2=0.24), and diastolic BP (F (1.62, 82.46)=15.79, p=0.01, partial η2=0.10). For systolic BP, post hoc comparisons showed that the average reduction in week 1 was significantly higher than the other 2 weeks (p<0.01). For diastolic BP, significantly higher mean reduction was observed at week 3 (p=0.02; Table 2).
Weekly pre- and post-intervention raw scores for BP
Despite there being no significant difference between the groups in the change scores for systolic BP and diastolic BP, there was a distinct reduction in both systolic BP and diastolic BP. To investigate these reductions, the mean pre- and postintervention scores were computed for systolic and diastolic BP by averaging the scores for each group across the 3 weeks. This resulted in a mean pre- and post-intervention systolic and diastolic BP for each group. Two paired t-tests were then performed to compare the respective pre- and post-intervention scores. Results indicated that the post-intervention systolic and diastolic BP was significantly lower in comparison to preintervention scores (p<0.01 in both groups; Table 3).
Table 3.
Average Total Pre- and Post-Intervention Scores for Systolic Blood Pressure and Diastolic Blood Pressure
| Average total scores (σ) | Effect of group | |||
|---|---|---|---|---|
| Dependent variable | Pre-intervention | Post-intervention | t-Value | Significance (p=) |
| Systolic blood pressure | 125.16 (16.77) | 117.46 (17.47) | 6.75 | <0.01* |
| Diastolic blood pressure | 69.94 (11.88) | 67.03 (11.45) | 3.75 | <0.01* |
p<0.05; σ=standard deviation; average total scores for systolic blood pressure and diastolic blood pressure were computed by averaging the pre- and post-intervention raw scores, respectively, across 15 sessions (3 weeks) and the two intervention groups (foot massage and quiet presence).
Safety
FM and QP were well tolerated apart from some individual variations. Some residents objected to having the BP cuff placed on and off their wrist and this may have increased rather than decreased their physiological stress measures. While the majority of participants felt comforted by the FM as indicated by their positive comments about it, or appeared relaxed by it, indicated by their falling asleep, these effects in some participants were not evident on the post-test measures when analyzed at the group level.
Discussion
In this randomized controlled trial of FM and QP, FM did not significantly reduce physiological stress when compared with the control group. Rather, the two groups, FM and QP, demonstrated a significant reduction in post-intervention BP scores in comparison to pre-intervention scores. While these findings pose more questions than answers, they should stimulate researchers to further investigate the use of physiological stress measurement as an outcome of interventions with this population.
We were mindful of recent research that has demonstrated autonomic dysfunction can be considerable, in particular, the severity of cardiovascular autonomic dysfunction in people with Lewy bodies and Parkinson's disease dementia.26 However, due to the number of participants in this study, we were unable to undertake subanalysis of different types of dementia. Because participants' BP and HR were taken while they were sitting or lying in the same position, there was no likelihood of orthostatic hypotension influencing the findings.
These findings are supportive of the hypothesis that being in close contact with others might in fact be comforting. This is reflected in the reductions on physiological stress measures seen in the QP group. Losses in social functioning associated with dementia can result in the person with dementia feeling alone and furthermore, when living in a LTC facility, their connection with others may be influenced by the environment, limited staffing and visitors,2–4 as well as by the stigmatization of their disease.27 Social connections are important28 and can improve psychological well-being.29 Recent research suggests the importance of positive people work whereby the person with dementia is acknowledged, listened to, and given direct eye contact.30 In both the intervention and control groups, the RAs were trained to enter the room and introduce themselves to the resident, providing direct eye contact and then to ask each participant if they were willing for the RA to either sit with them (QP) or have their feet massaged (intervention). While the conversation and connection was only of short duration, it may have been enough to reduce (if the person was feeling lonely or isolated) or increase (if the person was uncomfortable with strangers) the person's anxiety.31 The RA was taught to approach the participant with a person-oriented rather than a task-oriented approach, and this may also have helped the participant to cooperate and thereby reduce their anxiety and distress, and promote comfort.30,31
Although this study aimed to explore the effect of 10-minute FM on physiological measurement, the findings also suggest that this intervention may be useful in reducing hypertension, which is acknowledged to have an influence on the progression of dementia.32
There are several limitations of this study. We were unable to alter medication use in this sample. A future study might review medication and its influence on physiological measures. A second limitation relates to the potential for measurement error. There was the potential for BP and HR to be lowered or raised as a result of the participant's arm being placed at an angle lower than was recommended by the equipment manufacturer. However, this limitation was reduced through well-trained RAs and regular checking of the equipment. The third limitation relates to missing data when participants refused to have their physiological measures taken. Although the equipment chosen was deemed to be the least intrusive, the pressure from the inflated BP cuff had the potential to be uncomfortable, and this may have influenced physiological response.
Conclusions
The findings support the positive impact of the opportunity for the person with dementia to rest in the presence of another human being. The close presence of another person may in fact reduce anxiety and promote comfort, thereby improving BP and HR measures. Furthermore, the findings raise further questions and provide support for future research.
Acknowledgments
The authors acknowledge the funding for the conduct of the study that came from the National Health and Medical Research Council (NHMRC Project grant: 597415). The authors thank Dr. Mavourneen Casey who contributed to the initial analysis; Churches of Christ Care, Queensland, who supported the study in five of their facilities; and the residents who participated and the managers, care staff, and families for their support. Furthermore, the RAs who worked on this project are acknowledged for their contribution to the integrity of the research. Trial registration: ACTRN12612000658819.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Australian Institute of Health and Welfare. Residential Aged Care in Australia, 2002–2003: A statistical overview. Canberra: AIHW, Cat. no. AGE 38, 2004 [Google Scholar]
- 2.Cohen-Mansfield J, Marx MS, Rosenthal AS. Dementia and agitation in nursing home residents: How are they related? Psychology Aging 1990;5:3–8 [DOI] [PubMed] [Google Scholar]
- 3.Moyle W, Venturato L, Griffiths S, et al. Factors influencing quality of life for people with dementia: A qualitative perspective. Aging Mentl Hlth 2011;15:970–977 [DOI] [PubMed] [Google Scholar]
- 4.Cohen-Mansfield J. Nonpharmacologic interventions for inappropriate behaviours in dementia: A review, summary and critique. Am J Geriatr Psych 2001;9:361–381 [PubMed] [Google Scholar]
- 5.Oken BS, Fonareva I, Wahbeh H. Stress-related cognitive dysfunction in dementia caregivers. J Geriatr Psych Neuro 2011;24:191–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biondi M, Picardi A. Psychological stress and neuroendocrine function in humans; the last two decades of research. Psychother Psychosom 1999;68:114–150 [DOI] [PubMed] [Google Scholar]
- 7.Black PH, Garbutt LD. Stress, inflammation and cardiovascular disease. J Psychosom Res 2002;52:1–23 [DOI] [PubMed] [Google Scholar]
- 8.Suter PM, Maire R, Holtz D, Vetter W. Relationship between self–perceived stress and blood pressure. J Hum Hypertens 1997;11:171–176 [DOI] [PubMed] [Google Scholar]
- 9.Burns JL, Labbe E, Arke B, et al. The effects of different types of music on perceived and physiological measures of stress. J Music Ther 2002;39:101–116 [DOI] [PubMed] [Google Scholar]
- 10.Han L, Li JP, Sit JW, et al. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: A randomised controlled trial. J Clin Nurs 2010;19:978–987 [DOI] [PubMed] [Google Scholar]
- 11.Brett H. Complementary Therapies in the Care of Older People. London: Whurr Publishers Ltd., 2002 [Google Scholar]
- 12.Goldstone LA. Massage as an orthodox medical treatment past and future. Complement Ther Nurs Midwifery 2000;6:169–175 [DOI] [PubMed] [Google Scholar]
- 13.Uvnäs-Moberg K. The Oxytocin Factor: Tapping the Hormone of Calm, Love, and Healing. Cambridge, MA: Da Capo Press, 2004 [Google Scholar]
- 14.Sansome P, Schmitt L. Providing tender touch massage to elderly nursing home residents: A demonstration project. Geriatr Nurs 2000;21:286–331 [DOI] [PubMed] [Google Scholar]
- 15.Tuchtan V. The evidence for massage therapy. In: Tutchan C, Tutchan V, Stelfox D. Foundations of Massage, 2nd ed. Sydney: Churchill Livingstone, 2004, Chapter 4 [Google Scholar]
- 16.Nelson D. The power of human touch in Alzheimer's care. Massage Ther J 2004;43:82–92 [Google Scholar]
- 17.Remington R. Calming music and hand massage with agitated elderly. Nurs Res 2002;51:317–323 [DOI] [PubMed] [Google Scholar]
- 18.Rowe M, Alfred D. The effectiveness of slow-stroke massage in diffusing agitated behaviours in individuals with Alzheimer's disease. J Gerontol Nurs 1999;25:22–34 [DOI] [PubMed] [Google Scholar]
- 19.Moyle W, Johnston A, O'Dwyer S. Exploring the effect of foot massage on agitated behaviours in older people with dementia: A pilot study. Aust J Ageing 2011;30:159–161 [DOI] [PubMed] [Google Scholar]
- 20.Wang HL, Keck JF. Foot and hand massage as an intervention for postoperative pain. Pain Manag Nurs 2004;5:59–65 [DOI] [PubMed] [Google Scholar]
- 21.Bush E. The use of human touch to improve the well-being of older adults: A holistic nursing interventon. J Holistic Nurs 2011;19:256–270 [DOI] [PubMed] [Google Scholar]
- 22.Amercian Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). Washington: Author, 2000 [Google Scholar]
- 23.Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psych Res 1975;12:189–98 [DOI] [PubMed] [Google Scholar]
- 24.Rosen J, Burgio L, Kollar M, et al. The Pittsburgh Agitation Scale: A user-friendly instrument for rating agitation in dementia patients. Am J Geriatr Psych 1994;2:52–59 [DOI] [PubMed] [Google Scholar]
- 25.Wellek S, Blettner M. On the proper use of the crossover design in clinical trials. Deutsches Arztebllatt Intern 2012;109:276–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allan LM, Ballard CG, Allen J, et al. Autonomic dysfunction in dementia. J Neurol Neurosurg Psychiatry 2007;78:671–677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen Y, Ryden M, Feldt K, et al. The relationship between social interaction and characteristics of aggressive, cognitively impaired nursing home residents. Am J Alzh Dis 2000;15:10–17 [Google Scholar]
- 28.Bowlby J. Attachment and Loss. Vol 3 New York: Basic Books, 1980 [Google Scholar]
- 29.Philipson C. Social relationships in later life: A review of the research literature. Int J Geriatric Psych 1997;12:501–512 [DOI] [PubMed] [Google Scholar]
- 30.Sabat S, Lee JM. Relatedness among people diagnosed with dementia: Social cognition and the possibility of friendship. Dementia 2012;11:315–327 [Google Scholar]
- 31.Cheston R, Thorne K, Whitby P, et al. Stimulated presence therapy and separation amongst people with dementia. Dementia 2007;6:442–449 [Google Scholar]
- 32.Williams RG, King E, Smith AD, et al. Blood pressure, dementia and Alzheimer's disease: The OPTIMA longitudinal study. Dement Geriatr Cogn Disord 2009;28:70–74 [DOI] [PubMed] [Google Scholar]