Abstract
The immune cell system is a critical component of host defense. Recruitment of immune cells to sites of infection, immune reaction, or injury is complex and involves coordinated adhesive interactions between the leukocyte and the endothelial cell monolayer that lines blood vessels. This article will review basic mechanisms in the recruitment of leukocytes to tissues, and then selectively review new concepts that are emerging based on advances in live cell imaging microscopy and mouse strains. These emerging concepts are altering the conventional paradigms of inflammatory leukocyte recruitment established in the early 1990’s. Indeed, recent publications have identified previously unrecognized contributions from pericytes and interstitial leukocytes and their secreted products that guide leukocytes to their targets. It is also notable that investigators have begun to design organs on a chip. Recent reports indicate that this avenue of research holds much promise.
Keywords: neutrophil, endothelial cell, pericytes, inflammation, monocyte
The conventional multistep adhesion cascade paradigm of leukocyte recruitment
The inflammatory response is the cornerstone of the body’s defense mechanism against bacterial and viral pathogens, as well as physical-, chemical- and environmental-mediated tissue and organ damage. Acute inflammation occurs within minutes to hours and the telltale signs are readily observed microscopically: the recruitment of blood leukocytes and an increase in vascular permeability (Robbins and Cotran: Pathologic Basis of Disease 2010). Successful leukocyte transmigration across postcapillary venules is the culmination of sequential and overlapping steps mediated by multiple classes of adhesion molecules expressed on the surface of endothelial cells and their interactions with cognate ligands expressed by leukocytes. Drs. von Andrian and Butcher were the first to describe a molecular model of leukocyte recruitment in vivo: a two-step model consisting of leukocyte rolling via L-selectin (formerly called LECAM-1) followed by firm adhesion via β2 integrins (von Andrian et al. 1991). As with most other molecules discovered later to play a role in leukocyte transmigration, the critical information was acquired using function blocking monoclonal antibodies to these adhesion molecules and direct visualization in real time of rabbit postcapillary venules by intravital microscopy (reviewed in (Butcher 1991)). Another paradigm shift in the field was the demonstration that the vascular endothelium plays an active and essential role in recruitment of circulating leukocytes. Upon tumor necrosis factor-(TNF)α or interleukin-1(IL-1)β cytokines or E. coli Gram negative lipopolysaccharide treatment, the normally non-adhesive and non-thrombogenic surface of endothelium becomes proadhesive or “activated” (Bevilacqua and Gimbrone, Jr. 1987). Reports by several labs in that time period revealed this transformation in endothelial cell phenotype was mediated by a transcriptionally regulated program involving the nuclear factor NF-kappa-B (NFκB) dependent pathway triggered by proinflammatory cytokines or bacterial endotoxins (reviewed in (Collins et al. 1995)).
The paradigm for neutrophil recruitment in postcapillary venules has since been further expanded by investigators based primarily on the study of neutrophils (Figure 1; reviewed in (Kolaczkowska and Kubes 2013), and one can broadly generalize that most leukocytes follow a similar multi-step cascade in the peripheral (non-lymphoid) vasculature with some exceptions. Accordingly, an updated adhesion cascade in postcapillary venules involves free-flowing leukocytes initial attachment or tethering and slow velocity rolling (step 1), stable adhesion (arrest) on endothelial cells (step 2), leukocyte flattening (step 3), and subsequent crawling on the vascular endothelium, transendothelial cell migration (TEM) between (paracellular route) or through (transcellular) the vascular endothelium (step 4), and uropod elongation to complete transmigration of postcapillary venules (step 5). The initial attachment and rolling steps are initiated by interactions of endothelial E- and P-selectins and their counterreceptors on leukocytes L-selectin, PSGL-1, CD44, CD43, and E-selectin ligand-(ESL)1. The rolling step is reversible, unless followed by endothelial-presented chemoattractants and/or chemokines that activate leukocyte α4β1 (also called VLA4) and two members of the β2 integrin family, LFA-1 and Mac-1, to cause leukocyte arrest by binding to their cognate ligands, VCAM-1 and ICAM-1, respectively. Neutrophils from patients with leukocyte adhesion deficiencies (LAD) that lack selectin ligands (LAD type II) are unable to roll on endothelium, whereas patients lacking β2 integrins or expressing mutant β2 integrins (LAD type I) are unable to arrest stably. LAD type 1 and 2 mutations are rare and result in defects in leukocyte recruitment and severe recurrent infections in these patients (reviewed in (van de Vijver et al. 2012)). Recently, leukocytes from patients that have mutations in kindlin-3 (FERMT3 gene), a cytosolic protein that binds to the cytoplasmic domains of β1, β2, and β3 integrins, fail to activate these 3 integrins and as a result emigrate poorly into tissues (Svensson et al. 2009). This disorder is called LAD type 3. Since kindlin-3 binds to αIIbβ3 integrin expressed in platelets, the fibrinogen receptor, LAD type 3 patients also have defects in platelet adhesion and coagulation, in addition to defects in leukocyte adhesion, and present with severe and recurrent infections and hemostasis defects (reviewed in (van de Vijver et al. 2012)). Once stably arrested on the endothelial surface, leukocytes flatten, probably to reduce their exposure to shear stress force of flowing blood and collisions with circulating blood cells, and crawl variable distances before initiating transendothelial migration. These events rely on leukocyte β1 and β2 integrins binding to their endothelial-expressed cognate ligands, ICAM-1 and VCAM-1, respectively. In particular, recent studies in neutrophils and monocytes indicate that the Mac-1 integrins (αMβ2) mediate the apical leukocyte crawling (Schenkel et al. 2004; Phillipson et al. 2006)
Figure 1. Steps of the conventional paradigm of leukocyte transmigration and ventral lamellipodia recovery of transmigration gaps.
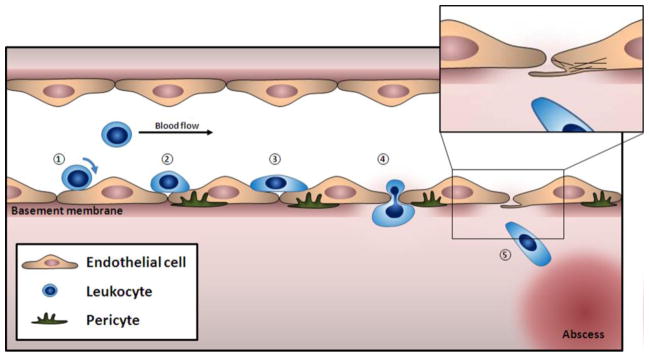
Inflammation from an abscess activates the endothelium to express adhesion molecules E-selectin, ICAM-1 and VCAM-1, and chemokines that mediate the multistep adhesion cascade. 1) Rolling of leukocytes via expression of selectin ligands (PSGL-1, L-selectin). 2) Arrest and firm adhesion is induced when β2 integrins on the leukocyte (LFA-1) bind to ICAM-1 on the activated endothelium under laminar shear flow conditions. Further integrin-mediated adhesion strengthening and 3) spreading is LFA-1 - ICAM-1 dependent; VCAM-1 is also involved in monocytes, T cells, basophils and eosinophils adhesion. 4) Transmigration occurs primarily by the paracellular pathway, as shown here, and in some cases by a transcellular transendothelial route (reviewd in (Alcaide et al. 2009)). The leukocyte crosses the basement membrane preferentially at areas of lower collagen and laminin densities and 5) migrates towards the inflammatory focus. Schematic model of transmigration pore closure with ventral lamellipodia is shown in the enlarged window (upper right). Loss of tension in the endothelial cell actin filaments (black lines in the cell) is proposed as one trigger initiating ventral lamellipodia formation.
Dissecting molecular mechanisms of transendothelial migration: contributions of both endothelium and leukocytes are necessary
Recent studies suggest that crawling T lymphocytes probe the apical surface for sites to transmigrate by generating membrane protrusions, called podoprints or filopodia, into the endothelial surface, however, whether neutrophils or other leukocyte types produce these membrane protrusions is as yet unknown (Carman et al. 2007; Shulman et al. 2009). Colocalizing with the T cell membrane protrusions are clusters of endothelial molecules including ICAM-1; VCAM-1 did not appear to exhibit this behavior (Shulman et al. 2009). The adhesion of many leukocyte types to ICAM-1, E-selectin, VCAM-1, CD47, PECAM-1 has been documented to trigger multiple intracellular signals in the endothelium that precede leukocyte transendothelial migration (TEM) (reviewed in (Alcaide et al. 2009; van Buul and Hordijk 2009)). The proximal signaling events detected include transient intracellular Ca2+ mobilization, activation of multiple tyrosine kinases including Src and Pyk-2, phosphotyrosine phosphatases, and subsequent association of many of these adhesion molecules to the cytoskeleton through binding to cytoskeletal adaptor molecules such as cortactin, α-actinin, and filamin. Intracellular vesicles, termed lateral border recycling compartment (LBRC) contain leukocyte adhesion molecules that are essential for leukocyte TEM. LBRC are actively transported to locations at cell-cell borders where transmigration of leukocytes occurs (see next section for details on the LBRC). In addition, VCAM-1, ICAM-1, and E-selectin have been shown to interact with one another and are organized in the plasma membrane into endothelial adhesion platforms, or EAPs by tetraspanins. EAPs are envisioned to facilitate leukocyte attachment and signaling during transmigration (Barreiro et al. 2008) as well as contributing to the activation of small GTPases that initiate cytoskeletal reorganization. Ultimately the signals generated by adherent leukocytes trigger gaps to form in the protein complexes that form the adherens junctions at endothelial cell-cell borders. The major complex includes the vascular endothelial (VE)-cadherin and its associated cytosolic binding partners α-, β-, γ- and p120-catenins and vascular endothelial-receptor protein tyrosine phosphatase (VE-PTP) (Alcaide et al. 2009; Vestweber 2012). The mechanisms underlying dissociation of VE-cadherin-catenin-VE-PTP and the gap formation has not been completely elucidated, but it appears to involve tyrosine phosphorylation of the cytoplasmic tail of VE-cadherin that destabilizes or dissociates VE-cadherin from catenins and VE-PTP, thus enabling VE-cadherin to be either endocytosed or transiently moved aside (reviewed in (Alcaide et al. 2009; Vestweber 2012). A recent report found that VCAM-1 induced Rac1, ROS and Pyk2 signaling plays a key role triggering dissociation of VE-PTP - VE-cadherin complex via a surprising requirement for binding of a substrate for the VE-PTP (Vockel and Vestweber 2013). It is unclear whether this is a universal mechanism since not all leukocytes have express the ligand VLA-4, which binds to VCAM-1, suggesting that other molecule(s) are needed to initiate this process.
The lateral border recycling compartment (LBRC)
A certain amount of membrane movement has been described to occur at endothelial cell borders during leukocyte transendothelial migration, with membrane constitutively being internalized and recycled in what has been termed the lateral border recycling compartment (LBRC) by Muller and colleagues (Muller 2011). Homophilic interactions between PECAM-1 (also called CD31) on leukocytes and PECAM-1 at the endothelial border trigger targeted recycling of PECAM-1 containing membrane vesicles from the LBRC that is located beneath actively transmigrating leukocytes at the lateral borders (Mamdouh et al. 2003; Mamdouh et al. 2008). Although the LBRC contains other junctional molecules involved in transmigration including CD99, JAM-A, and poliovirus receptor (CD155), interestingly VE-cadherin is not included. As mentioned above, during transmigration VE-cadherin moves out of the way, forming characteristic gaps in the otherwise linear VE-cadherin complex (Shaw et al. 2001; Allport et al. 2000b). The LBRC membrane surrounds the transmigrating leukocyte and is transported along microtubules to the site of diapedesis by kinesin motors (Mamdouh et al. 2008). Indeed, blocking PECAM-1 or depolymerizing microtubules or blocking kinesin function all inhibit transmigration without affecting leukocyte adhesion and without being additive, indicating a role in the same pathway. The authors conclude that the LBRC integrates the molecules necessary for leukocyte passage into a “transmigration complex”, with a high number of unligated adhesion molecules available to interact, while at the same time opening or loosening junctions by excluding VE-cadherin. Recently, the Muller lab also found that CD155 or Poliovirus receptor PVR, which is involved in transmigration through interactions with its cognate ligand DNAM-1 (CD266) expressed on monocytes, can also be found in the LBRC (Reymond et al. 2004; Sullivan et al. 2013). Adhesion of monocytes to endothelial cell CD155 activates a src-kinase dependent recruitment of the tyrosine-protein phosphatase non-receptor type 11 (also called Shp-2). The authors, therefore, suggest that the localization of adhesion/signaling molecules to the lateral border recycling compartment and the recruitment ofhpHP-2 may be common mechanisms for the regulation of TEM. There are some key aspects of the LBRC that remain unanswered. How the dynamics of the LBRC vesicular compartment synchronize with the VE-cadherin - VE-PTP - catenin complex to create the portal for leukocyte transmigration, and by extension, how does the LBRC play a role in recovery of the VE-cadherin-VE-PTP-catenin complex at cell-cell borders. Each of these processes is also very relevant to control of vascular permeability.
New insights into molecules that regulate leukocyte integrin affinity
Integrins are a family of αβ heterodimeric adhesion receptors that mediate attachment between cells and other cells or to basement membrane, and transmit via signal transduction information about the environmental status into cells, and as such are vital players in leukocyte recruitment. The β2 integrin family is exclusively expressed in leukocytes and as mentioned earlier is essential for leukocyte arrest on the endothelium and for migration across the endothelium (Ley et al. 2007). Integrin activation is required for these adhesive functions. An important aspect of integrin biology is their dual role of sensing and interacting with the surrounding environment through outside-in and inside-out signaling (Hynes 2002). Integrins exist in various states of activation, which are in equilibrium with one another and depend on the activation status of the cell. In unstimulated leukocytes integrins are usually in a conformation with low binding affinity, until they receive stimulating signals from other receptors, such as chemokine receptors and the T cell receptor complex, or in conjunction with ligands including ICAM-1. Upon activation, there is a dramatic shift in conformation of the molecule from a bent, compact shape to an extended, open one, thereby displaying high-affinity for ligands (Luo et al. 2007). Ligand binding appears necessary to stabilize the high affinity conformations. Monoclonal antibodies recognizing these conformations have been described for β2 integrins (Schurpf and Springer 2011). In the presence of lateral shear forces from flowing blood, integrin switching to a higher affinity conformation is faster because the transmembrane subunits are pushed slightly apart, facilitating the full extended conformation (Kim et al. 2003). This allows for rapid and tight binding to ICAM-1 (Zhu et al. 2008). Dysregulation of integrin affinity can occur through mutations in integrins or cytosolic binding molecules. It is therefore not surprising that integrins are also highly regulated molecules.
CD47 regulates the affinity of LFA-1 and VLA-4 in T cells
Recently our laboratory has identified CD47 as an important transmembrane protein that regulates the expression of high affinity conformations of leukocyte VLA-4 and LFA-1 and their adhesive functions (Azcutia et al. 2013; Azcutia et al. 2012; Stefanidakis et al. 2008; Martinelli et al. 2013b). CD47 is a broadly expressed 50 kDa transmembrane glycoprotein (Brown et al. 1990). CD47 interacts in “trans” with signal regulatory protein (SIRP), SIRPα and SIRPγ, and thrombospondin-1. CD47 has also been called Integrin Associated Protein (IAP) because of its ability to interact “in cis” with multiple integrins including αVβ3, α2β1, and αvβ3 in non-leukocyte cell types (reviewed in (Brown and Frazier 2001; Oldenborg 2013). CD47 is expressed on both endothelium and leukocytes, where our lab has shown that it plays a role in both cell types during leukocyte transmigration in in vivo and in in vitro models of inflammation (Azcutia et al. 2013; Stefanidakis et al. 2008; Martinelli et al. 2013b; Azcutia et al. 2012). In the endothelium, CD47 engagement by anti-CD47 antibody crosslinking promotes src-kinase activation, actin stress fiber formation and VE-cadherin tyrosine phosphorylation (Martinelli et al. 2013b; Stefanidakis et al. 2008), however, its ability to interact “in cis” and regulate endothelial cell integrins has not been reported. Murine T helper type 1 (Th1) cells from CD47−/− mice exhibited defects in tethering to TNF-α activated endothelium in the cremaster muscle microcirculation, and showed impaired arrest and transmigration of TNF-α activated murine heart endothelium in an in vitro flow chamber assay. More recently, CD47 has been shown to associate with human leukocyte β2 integrins, primarily LFA-1, “in cis” by fluorescence lifetime imaging microscopy and Förster resonance energy transfer (FLIM-FRET). Using reporter monoclonal antibodies that recognize high affinity forms of human β1 and β2 integrins revealed that loss of CD47 impaired their ability to express the high affinity “extended and open” conformation. These results support the concept that CD47 associates “in cis” with Th1 cell LFA-1 and VLA-4 integrins, and that CD47 is necessary to induce high affinity conformations of these integrins to bind to their endothelial cell ligands ICAM-1 and VCAM-1, and support leukocyte adhesion and transendothelial migration (Azcutia et al. 2013).
Preservation of barrier function during transmigration
The endothelium, although an obstacle that transmigrating leukocytes have to overcome, is a thin monolayer of cells attached to a basement membrane by integrins in focal adhesion complexes and to each other by gap, tight, and adherens junctions (Bazzoni and Dejana 2004). The endothelium is well adapted to respond to biomechanical forces mediated by blood flow and blood pressure (Gimbrone, Jr. et al. 2000). Transmigrating leukocytes pose a problem to endothelial barrier function by disrupting cell-cell and cell-matrix junctions and disrupting VE-cadherin connections as just mentioned. Transmigrating leukocytes induce micrometer-scale disruptions in endothelial layer integrity through F-actin protrusions such as pseudopodia and invasive podosomes (reviewed in (Ley et al. 2007)). Although inflammatory cytokines and neutrophil secreted substances (reactive oxygen species (ROS), proteases, and other secreted products (DiStasi and Ley 2009) can cause significant barrier loss accompanying transmigration, little loss in barrier function or significant plasma leakage is observed during transmigration per se, because the formed VE-cadherin gaps disappear quickly and the transmigration pores are rapidly resealed behind the leukocyte so that endothelial integrity is restored, revealing the strong self-restorative capacity of the endothelium (Shaw et al. 2001; Carman and Springer 2004; Sage and Carman 2009; He 2010). In this respect, the recent report by Martinelli et al. describes a Rac1-, arp2/3- and ROS-dependent actin remodeling mechanism in endothelium to monitor local barrier disruptions and to effectively close these micro-wounds (Martinelli et al. 2013a). In the case of transcellular pores, these studies reveal the existence of an asymmetric actin-mediated wound closure mechanism related to membrane protrusions. Total internal reflective (TIRF) microscopy revealed that such actin structures were ventrally located, thus coining the term “ventral lamellipodia”. These authors also describe that ventral lamellipodia formation depended on alpha3 and alpha5 integrin association with the basolateral extracellular matrix. Similarly, leukocyte paracellular transmigration pores were rapidly closed by ventral lamellipodia travelling peripherally to fill the gaps and re-establish cell-cell contacts. Using live-cell imaging, VE-cadherin was shown to regain its linear pattern and adherens junctions were reconstituted within 5 minutes of gap closure (see Figure 1), which agrees nicely with previous reports that described VE-cadherin gap formation and closure during leukocyte transmigration (Shaw et al. 2001; Allport et al. 2000a). Martinelli et al found that these ventral lamellipodia are initiated by tension loss (after adhesion rupture, for example) that occurred in wounding or was transmitted through the monolayer, which induces local signaling for repair that is initiated from preexisting actin filaments. These lamellipodia propagate beneath cells, which is a type of actin remodeling different from known lamellipodia or dorsal ruffles (Chhabra and Higgs 2007). It is likely that these ventral lamellipodia, which were also observed in epithelia, represent a more general mechanism of closing pores and gaps as well as cell migration, thus maintaining barrier integrity during leukocyte transmigration or during recovery from stimuli that promote vascular leakage (thrombin, histamine, VEGF). It will be of interest to determine whether the transmigration induced dynamics of the LBRC and the VE-cadherin-VE-PTP-catenin complex are mechanistically linked to the formation of endothelial ventral lamellipodia.
Modification of the “conventional” multistep paradigm for organs (Liver, Lung and Kidney)
Intravital microscopy of postcapillary venules in the cremaster muscle, mesentery and hamster cheek pouch microcirculation in combination with either fluorescently labeled leukocytes or the recent novel mouse strains expressing leukocyte-specific fluorescent reporter molecules have been the most commonly studied tissues to visualize behavior of leukocyte subsets and to gain insight into the mechanisms that mediate their recruitment. This “conventional” multistep paradigm was discussed earlier (Figure 1). Reports using new methodologies for in vivo imaging including two photon-intravital microscopy (TP-IVM) and Spinning Disk Confocal Microscopy-IVM suggest that leukocyte-endothelial interactions in certain organs do not conform to the multi-step model paradigm observed in postcapillary venules. In particular, the liver, lung, and kidney also are prone to inflammatory diseases (e.g., hepatitis, acute respiratory distress syndrome, glomerulonephritis), and recent studies have made progress in deciphering the steps and molecules involved in leukocyte-endothelial interactions in these organs. It is obvious that these organs are structurally different from one another, and hence are characterized by unique functional specializations reflected in their microvasculature. In these organs blood leukocytes interact with capillaries (lung), sinusoids (liver), and glomerulus capillary plexus (kidney), rather than postcapillary and collecting venules. Here we briefly review recent reports in models of inflammation in these organs.
The liver lobule microvasculature receives an arterial and venous supply and is composed of sinusoid capillaries lined with fenestrated endothelium that drain into post sinusoidal central veins. The endothelium is separated from hepatocytes by a discontinuous basement membrane and a space called space of Disse, which contains microvilli of the hepatocytes and Kupffer cells, the resident liver macrophages. Liver sinusoid endothelium express a different leukocyte adhesion molecule profile than peripheral tissue postcapillary venules, with little E- and P-selectin or VCAM-1 expression, while exhibiting constitutively high expression of ICAM-1 and Vascular Adhesion Protein (VAP)-1 (McNab et al. 1996). While leukocytes do adhere to sinusoidal endothelium, rolling interactions have not been reported. In the post sinusoidal central veins in liver, leukocyte rolling does occur (reviewed in (Jenne and Kubes 2013)). In knockout mouse models, leukocyte transmigration was shown to be independent of selectin expression but dependent on ICAM-1 (Wong et al. 1997). Also, in a model of neutrophil recruitment induced by LPS, adhesive interactions were found to be mediated by the endothelial cell expressed glycosaminoglycan hyaluronan acid (HA) that binds serum derived HA-binding protein, which interacts with its ligand CD44 expressed by neutrophils (McDonald et al. 2008). Other leukocyte types are present in the liver, including invariant natural killer T cells (iNKT cells) and Kupffer cells. See the review by Jenne and Kubes for a detailed discussion of the dynamics of both of these cells in various models (Jenne and Kubes 2013).
The lung vasculature is composed of capillaries that are extremely thin to facilitate gas exchange. The capillaries form a complex interconnecting network of short vessels that are continuous and not fenestrated. Previous reports found leukocyte recruitment occurred at capillaries, and did not use the conventional multistep cascade and did not rely on either the β2 integrins or selectins (Wang et al. 2004). Using TP-IVM, a recent study reported significant numbers of extravascular neutrophils in the lung of mechanically ventilated LysM-GFP transgenic mice at baseline (Kreisel et al. 2010). These neutrophils appeared weakly motile (~2–3 μm/min). Within minutes of L. monocytogenes bacterial challenge, however, rapid and significant influx of neutrophils occurred. Their motility speed increased 3.5-fold (~10 μm/min), and they formed clusters containing ~20 cells. In a model of ischemia-reperfusion induced as a result of WT lung transplanted in LysM-GFP recipients, blood monocytes were also imaged because of their fortuitous uptake of 655-nm Q-dots. Using this approach, monocytes were infrequently found arrested or extravasated in lung capillaries. In this model significant neutrophil extravasation was noted and the cells showed high velocity crawling, forming dynamic clusters similar to those seen after bacterial challenge. Monocytes were required for this behavior because clodronate liposome injection to deplete monocytes markedly reduced extravascular neutrophils and cluster formation. The authors speculated that monocytes secreted chemoattractants that caused the neutrophil clustering behavior in both the bacterial and lung transplantation models. One could also speculate that a chemotaxis relay system also is at work in this lung model. For example, chemotaxing “leader” interstitial neutrophils following the initial monocyte derived chemoattractant(s) may be stimulated to produce their own chemoattractant, perhaps LTB4, to amplify locally the initial monocyte product to recruit additional neutrophils (see below, the swarming of neutrophils).
Leukocyte interactions with the vascular wall in the kidney glomerulus has been reported recently under resting and after induction of acute inflammation by multiphoton-IVM (immune complex deposition) (Devi et al. 2013). Again, contrary to the “conventional” paradigm discussed earlier, leukocyte interactions with the glomerulus microvessels of the kidney are distinctly different. Under resting conditions in the kidney both neutrophils and monocytes interacted with the apical endothelial surface of glomerular capillaries for >30 seconds to periods as long as a few minutes, which the authors termed “dwell time”. These adherent and crawling leukocytes were localized to the lumen and characterized as performing patrolling activities with migration velocities of ~11 μm/min. Conceptually, intravascular patrolling has also been observed in the liver and lung, and is thought to confer intravascular immune surveillance in organs. These investigators envision that such localization enables rapid responses by these leukocytes to infectious and sterile inflammatory stimuli. In the kidney study, that is exactly what occurs. Upon initiating inflammation in the kidney (i.e., glomerulonephritis) by immune complex deposition in the glomerulus basement membrane, leukocyte dwell time in vessel lumen increased dramatically, and was greater than 20 minutes. Many adherent and crawling leukocytes produced toxic reactive oxygen species that may damage the endothelium and lead to proteinuria in these mice. These types of studies revealed novel concepts for glomerular homeostasis and a more clear understanding of the molecular mechanisms of leukocyte trafficking—instead of undergoing transendothelial migration after adhesion, the leukocytes increase their intravascular retention time and under pro-inflammatory conditions, produce ROS and other pro-inflammatory mediators that can damage tissues and organs.
Mechanisms of post-diapedesis leukocyte migration: Pass through the basement membrane and “turn right” onto pericytes “Avenues” for guidance to interstitial targets
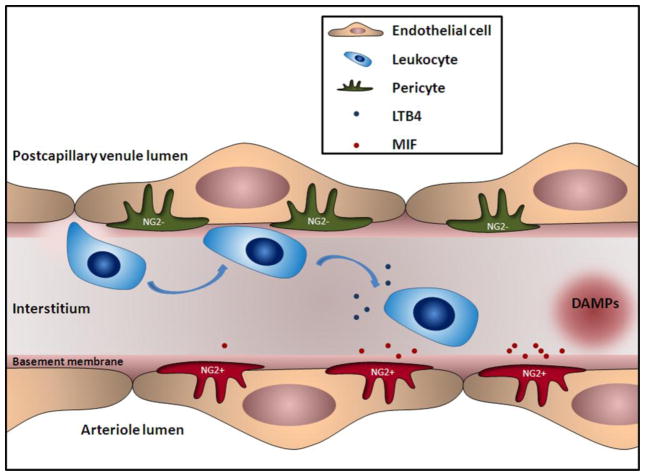
Leukocytes that have successfully transmigrated across the vascular endothelium in most tissues encounter the basement membrane, and in many tissues, pericytes, which discontinuously wrap around arterioles, capillaries, and postcapillary and collecting venules (Figure 2 and reviewed in (Armulik et al. 2005)). With the improving characterization of pericytes, their importance in leukocyte migration has recently come into sharp focus. Recent studies have reported that neutrophils and monocytes preferentially migrate through specific areas in the basement membrane where matrix proteins collagen type IV and laminin 10 are expressed at a lower density (Wang et al. 2006; Voisin et al. 2009). A recent study has reported that emigrated interstitial neutrophils interact extensively with neuron-glial 2 positive (NG2+) pericytes after migrating across the vascular endothelium in a murine model of sterile TNF-α induced inflammation (Proebstl et al. 2012). Another recent studies revealed that pericytes express ICAM-1 and secrete chemoattractants as well (Stark et al. 2013). Notably, two different populations of pericytes were described that associated with distinct blood vessel types: NG2+ and α-smooth muscle actin positive (α-SMC+) pericytes are located along arterioles and capillaries whereas NG2 negative (NG2−) and α-SMC+ are located along postcapillary venules in a dermal mouse model. Emigrated neutrophils and monocytes first encounter the NG2− population on postcapillary venules and crawl along these, and then become attracted to the NG2+ pericytes. This is because NG2+ pericytes become stimulated by tissue derived damage and pathogen associated molecular pattern DAMPS and PAMPs to produce the chemokine macrophage migration-inhibitory factor (MIF) and other chemokines, which attract these just transmigrated neutrophils. These studies provide a broader picture of mechanisms that mediate innate cell recruitment and strong evidence that the endothelium, the basement membrane and pericytes are active participants in the innate immune response. These reports beg the question of whether other interstitial cells or physiological systems are involved in regulating and guiding leukocytes to sites of inflammation? A recent report sheds light on this question (Lammermann et al. 2013).
Figure 2. Transmigration and interactions of neutrophils after transendothelial migration.
Neutrophils cross the basement membrane of a postcapillary venule (top endothelial layer) at a region of lower concentrations of collagen IV and laminin 10 densities and are guided in the interstitium by interactions with pericytes. Neutrophils first crawl along the NG2− pericytes (green) outside of postcapillary venules. MIF secretion from activated pericytes on arterioles (red) further guides cells towards the inflammatory focus. We speculate that in neutrophils attract further influx of neutrophils by secreting LTB4 or other chemoattractants that trigger a swarming behavior of neutrophils around a wound. DAMP, damage-associated molecular pattern.
Interstitial neutrophil dance ballad called “The Swarming of Neutrophils”
A deeper understanding of migration of neutrophils in the interstitial space has been detected in a model of laser-induced sterile skin injury using TP-IVM (Lammermann et al. 2013). In contrast to the conventional multistep model of neutrophil extravasation, they uncovered an integrin independent, molecular relay mechanism that occurs in conjunction with coordinated chemotaxis and cluster formation of neutrophils in the extravascular space of damaged dermal tissue. This type of behavior is also known as swarming. It is temporally coordinated and is characterized by initial chemotaxis of the neutrophils closest to the damaged tissue, followed by a strong influx of cells from more distant sites, and finally neutrophil clustering as reported earlier (Ng et al. 2011). Neutrophils immediately swarm the wound as demonstrated by highly directional chemotaxis at high speeds whereas chemokine receptor CXCR3+ monocytes migrate at a later time and at slower speeds, and do not enter the developing cluster of neutrophils. This phase is followed by a second phase of neutrophil influx from more distant sites, which is catalyzed by the death of only a small number of neutrophils. Studying neutrophils lacking different G-protein coupled receptors (GPCR) and then narrowing down the respective receptors, the authors were able to identify the receptor for leukotriene B4 (LTB4R1) as crucial and the neutrophil secreted LTB4 chemoattractant as the relaying signal among neutrophils over larger distances. It is this relaying signal that amplifies cell death signals, thus broadening the radius of chemotactic signal. Indeed, neutrophils lacking the LTB4 receptor, Ltb4r1−/− still migrated towards the wound, but the second phase of the neutrophil response was missing. The clustering step, however, was found to be integrin mediated. The authors suggest these events trigger a self-organized neutrophil influx that forms a wound seal ending with the later monocyte recruitment that isolates the injured from the viable tissue (Lammermann et al. 2013).
Neutrophil extracellular traps: their role in host defense and in disease
The ability of neutrophils to swarm, phagocytose, and/or neutralize foreign materials, necrotic tissues, and bacteria is unparalleled in nature. Moreover, as neutrophils are performing their “cleanup” job or once their cleanup is complete, they keep on giving of themselves through formation of neutrophil extracellular traps, or NETs (Brinkmann et al. 2004). During an inflammatory response, neutrophils can be stimulated by physiological agonist and bacterial endotoxins to release NETs, a cloud-like mixture of highly negatively charged strands of DNA and its associated proteins and granule enzymes. NETs are envisioned to enhance the cell’s ability to trap and inactivate virulence factors, and have been demonstrated to kill Gram-positive (Staphylococcus aureus) and Gram-negative (Salmonella typimurium) pathogenic bacteria (Brinkmann and Zychlinsky 2012; Brinkmann et al. 2004). Subsequent studies have corroborated these findings and provided the stepwise pathway for generation and release of NETS by neutrophils. Other granulocyte leukocytes including mast cells and basophils have been demonstrated to release NETs (Kolaczkowska and Kubes 2013). It is also of interest that NETs appear to have a dark side. Recent reports have shown that NETs contribute to thrombus formation in an experimental deep vein thrombosis model (Brinkmann and Zychlinsky 2012; Fuchs et al. 2010). Once again, Mother Nature has provided yet another layer of defense in the immune system that was unexpected.
A few words about Organs on a Chip
The advent of microdevices has provided new approaches to model and study different aspects of organ function. Organs on chips are a class of microengineered tissue models that could be an appropriate conduit to transition from basic single cell in vitro models to in vivo experimental disease models (van der Meer and van den Berg 2012). Although beyond the scope of this review, recent reports from the Ingber laboratory and other laboratories have advanced this field by providing a fertile environment in which cell biologists and bioengineers work collaboratively to develop microfluidic devices. These devices use living cells in well-controlled environmental conditions that induce cells to express and maintain tissue specific differentiated properties that mimic organs including physiological relevant 3 dimension structural units of living organs such as kidney, liver, brain, heart, intestine, and lung (Huh et al. 2013). Spatiotemporal chemical gradients or mechanical forces such as breathing movements, fluid flow or gut peristalsis can be mimicked creating a more physiologically cell culture model, upgrading the classical in vitro experiments and thus representing a possible low-cost alternative to animal models. In such devices, inflammation can be successfully mimicked and studied. The future task is how to best utilize these organs on chips and integrate these technologies, and to determine whether their “added value” will hold up to the expectations and help to gain an in depth understanding of how leukocyte enter and exit during normal and pathological settings and where and when to intervene successfully.
Concluding remarks
Recent studies have highlighted the role of inflammation in obesity, diabetes, hypertension, autoimmune disease, and cardiovascular diseases including stroke and atherosclerosis. A common approach to develop innovative and effective anti-inflammatory therapeutics is to understand basic mechanisms regulating leukocyte entry and exit from tissues and organs, and then translate these observations into a physiological model that mimics human disease. Going forward, important discussion point are how to harness our knowledge of these key events to build a rational therapeutic with minimal off targets effects? Will organ on a chip become the intermediate step from basic single cell in vitro assays to murine models? Will these new imaging modalities enable researchers to put all the data together for faster drug discoveries?
Acknowledgments
Supported by funding from the NHLBI, NIH (HL-36028) and American Heart Association Postdoctoral Fellowship (11POST7730055). The project was also supported by the National Research Fund, Luxembourg, and co-funded under the Marie Curie Actions of the European Commission (FP7-COFUND).
Reference List
- Alcaide P, Auerbach S, Luscinskas FW. Neutrophil recruitment under shear flow: it’s all about endothelial cell rings and gaps. Microcirculation. 2009;16:43–57. doi: 10.1080/10739680802273892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allport JR, Muller WA, Luscinskas FW. Monocytes induce reversible focal changes in vascular endothelial cadherin complex during transendothelial migration under flow. J Cell Biol. 2000a;148:203–216. doi: 10.1083/jcb.148.1.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allport JR, Muller WA, Luscinskas FW. Monocytes induce reversible focal changes in vascular endothelial cadherin complex during transendothelial migration under flow. J Cell Biol. 2000b;148:203–216. doi: 10.1083/jcb.148.1.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armulik A, Abramsson A, Betsholtz C. Endothelial/pericyte interactions. Circ Res. 2005;97:512–523. doi: 10.1161/01.RES.0000182903.16652.d7. [DOI] [PubMed] [Google Scholar]
- Azcutia V, Routledge M, Williams MR, Newton G, Frazier WA, Manica A, Croce K, Parkos CA, Schmider AB, Turman MV, Soberman RJ, Luscinskas FW. CD47 plays a critical role in T cell recruitment by regulation of LFA-1 and VLA-4 integrin adhesive functions. Mol Biol Cell. 2013 Sep 4; doi: 10.1091/mbc.E13-01-0063. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azcutia V, Stefanidakis M, Tsuboi N, Mayadas T, Croce KJ, Fukuda D, Aikawa M, Newton G, Luscinskas FW. Endothelial CD47 promotes vascular endothelial-cadherin tyrosine phosphorylation and participates in T cell recruitment at sites of inflammation in vivo. J Immunol. 2012;189:2553–2562. doi: 10.4049/jimmunol.1103606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreiro O, Zamai M, Yanez-Mo M, Tejera E, Lopez-Romero P, Monk PN, Gratton E, Caiolfa VR, Sanchez-Madrid F. Endothelial adhesion receptors are recruited to adherent leukocytes by inclusion in preformed tetraspanin nanoplatforms. J Cell Biol. 2008;183:527–542. doi: 10.1083/jcb.200805076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzoni G, Dejana E. Endothelial cell-to-cell junctions: molecular organization and role in vascular homeostasis. Physiol Rev. 2004;84:869–901. doi: 10.1152/physrev.00035.2003. [DOI] [PubMed] [Google Scholar]
- Bevilacqua MP, Gimbrone MA., Jr Inducible endothelial functions in inflammation and coagulation. Semin Thromb Hemost. 1987;13:425–433. doi: 10.1055/s-2007-1003519. [DOI] [PubMed] [Google Scholar]
- Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, Weinrauch Y, Zychlinsky A. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- Brinkmann V, Zychlinsky A. Neutrophil extracellular traps: is immunity the second function of chromatin? J Cell Biol. 2012;198:773–783. doi: 10.1083/jcb.201203170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown E, Hooper L, Ho T, Gresham H. Integrin-associated protein: a 50-kD plasma membrane antigen physically and functionally associated with integrins. J Cell Biol. 1990;111:2785–2794. doi: 10.1083/jcb.111.6.2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown EJ, Frazier WA. Integrin-associated protein (CD47) and its ligands. Trends Cell Biol. 2001;11:130–135. doi: 10.1016/s0962-8924(00)01906-1. [DOI] [PubMed] [Google Scholar]
- Butcher EC. Leukocyte-endothelial cell recognition: three (or more) steps to specificity and diversity. Cell. 1991;67:1033–1036. doi: 10.1016/0092-8674(91)90279-8. [DOI] [PubMed] [Google Scholar]
- Carman CV, Sage PT, Sciuto TE, de la Fuente MA, Geha RS, Ochs HD, Dvorak HF, Dvorak AM, Springer TA. Transcellular diapedesis is initiated by invasive podosomes. Immunity. 2007;26:784–797. doi: 10.1016/j.immuni.2007.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carman CV, Springer TA. A transmigratory cup in leukocyte diapedesis both through individual vascular endothelial cells and between them. J Cell Biol. 2004;167:377–388. doi: 10.1083/jcb.200404129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chhabra ES, Higgs HN. The many faces of actin: matching assembly factors with cellular structures. Nat Cell Biol. 2007;9:1110–1121. doi: 10.1038/ncb1007-1110. [DOI] [PubMed] [Google Scholar]
- Collins T, Read MA, Neish AS, Whitley MZ, Thanos D, Maniatis T. Transcriptional regulation of endothelial cell adhesion molecules: NF-kappa B and cytokine-inducible enhancers. FASEB J. 1995;9:899–909. [PubMed] [Google Scholar]
- Devi S, Li A, Westhorpe CL, Lo CY, Abeynaike LD, Snelgrove SL, Hall P, Ooi JD, Sobey CG, Kitching AR, Hickey MJ. Multiphoton imaging reveals a new leukocyte recruitment paradigm in the glomerulus. Nat Med. 2013;19:107–112. doi: 10.1038/nm.3024. [DOI] [PubMed] [Google Scholar]
- DiStasi MR, Ley K. Opening the flood-gates: how neutrophil-endothelial interactions regulate permeability. Trends Immunol. 2009;30:547–556. doi: 10.1016/j.it.2009.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs TA, Brill A, Duerschmied D, Schatzberg D, Monestier M, Myers DD, Jr, Wrobleski SK, Wakefield TW, Hartwig JH, Wagner DD. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci U S A. 2010;107:15880–15885. doi: 10.1073/pnas.1005743107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gimbrone MA, Jr, Topper JN, Nagel T, Anderson KR, Garcia-Cardena G. Endothelial dysfunction, hemodynamic forces, and atherogenesis. Ann N Y Acad Sci. 2000;902:230–239. doi: 10.1111/j.1749-6632.2000.tb06318.x. [DOI] [PubMed] [Google Scholar]
- He P. Leucocyte/endothelium interactions and microvessel permeability: coupled or uncoupled? Cardiovasc Res. 2010;87:281–290. doi: 10.1093/cvr/cvq140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh D, Kim HJ, Fraser JP, Shea DE, Khan M, Bahinski A, Hamilton GA, Ingber DE. Microfabrication of human organs-on-chips. Nat Protoc. 2013;8:2135–2157. doi: 10.1038/nprot.2013.137. [DOI] [PubMed] [Google Scholar]
- Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110:673–687. doi: 10.1016/s0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- Jenne CN, Kubes P. Immune surveillance by the liver. Nat Immunol. 2013;14:996–1006. doi: 10.1038/ni.2691. [DOI] [PubMed] [Google Scholar]
- Kim M, Carman CV, Springer TA. Bidirectional transmembrane signaling by cytoplasmic domain separation in integrins. Science. 2003;301:1720–1725. doi: 10.1126/science.1084174. [DOI] [PubMed] [Google Scholar]
- Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13:159–175. doi: 10.1038/nri3399. [DOI] [PubMed] [Google Scholar]
- Kreisel D, Nava RG, Li W, Zinselmeyer BH, Wang B, Lai J, Pless R, Gelman AE, Krupnick AS, Miller MJ. In vivo two-photon imaging reveals monocyte-dependent neutrophil extravasation during pulmonary inflammation. Proc Natl Acad Sci U S A. 2010;107:18073–18078. doi: 10.1073/pnas.1008737107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar V, Abbas AK, Fausto N, Aster J. Robbins and Cotran: Pathologic Basis of Disease. 8. Elsevier; Philadelphia: 2010. [Google Scholar]
- Lammermann T, Afonso PV, Angermann BR, Wang JM, Kastenmuller W, Parent CA, Germain RN. Neutrophil swarms require LTB4 and integrins at sites of cell death in vivo. Nature. 2013;498:371–375. doi: 10.1038/nature12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley K, Laudanna C, Cybulsky MI, Nourshargh S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7:678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- Luo BH, Carman CV, Springer TA. Structural basis of integrin regulation and signaling. Annu Rev Immunol. 2007;25:619–647. doi: 10.1146/annurev.immunol.25.022106.141618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamdouh Z, Chen X, Pierini LM, Maxfield FR, Muller WA. Targeted recycling of PECAM from endothelial surface-connected compartments during diapedesis. Nature. 2003;421:748–753. doi: 10.1038/nature01300. [DOI] [PubMed] [Google Scholar]
- Mamdouh Z, Kreitzer GE, Muller WA. Leukocyte transmigration requires kinesin-mediated microtubule-dependent membrane trafficking from the lateral border recycling compartment. J Exp Med. 2008;205:951–966. doi: 10.1084/jem.20072328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinelli R, Kamei M, Sage PT, Massol R, Varghese L, Sciuto T, Toporsian M, Dvorak AM, Kirchhausen T, Springer TA, Carman CV. Release of cellular tension signals self-restorative ventral lamellipodia to heal barrier micro-wounds. J Cell Biol. 2013a;201:449–465. doi: 10.1083/jcb.201209077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinelli R, Newton G, Carman CV, Greenwood J, Luscinskas FW. Novel Role of CD47 in Rat Microvascular Endothelium: Signaling and Regulation of T-Cell Transendothelial Migration. Arterioscler Thromb Vasc Biol. 2013b;33:2566–2576. doi: 10.1161/ATVBAHA.113.301903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald B, McAvoy EF, Lam F, Gill V, de la MC, Savani RC, Kubes P. Interaction of CD44 and hyaluronan is the dominant mechanism for neutrophil sequestration in inflamed liver sinusoids. J Exp Med. 2008;205:915–927. doi: 10.1084/jem.20071765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNab G, Reeves JL, Salmi M, Hubscher S, Jalkanen S, Adams DH. Vascular adhesion protein 1 mediates binding of T cells to human hepatic endothelium. Gastroenterology. 1996;110:522–528. doi: 10.1053/gast.1996.v110.pm8566600. [DOI] [PubMed] [Google Scholar]
- Muller WA. Mechanisms of leukocyte transendothelial migration. Annu Rev Pathol. 2011;6:323–344. doi: 10.1146/annurev-pathol-011110-130224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng LG, Qin JS, Roediger B, Wang Y, Jain R, Cavanagh LL, Smith AL, Jones CA, de Veer M, Grimbaldeston MA, Meeusen EN, Weninger W. Visualizing the neutrophil response to sterile tissue injury in mouse dermis reveals a three-phase cascade of events. J Invest Dermatol. 2011;131:2058–2068. doi: 10.1038/jid.2011.179. [DOI] [PubMed] [Google Scholar]
- Oldenborg PA. CD47: A Cell Surface Glycoprotein Which Regulates Multiple Functions of Hematopoietic Cells in Health and Disease. ISRN Hematol. 2013;2013:614619. doi: 10.1155/2013/614619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipson M, Heit B, Colarusso P, Liu L, Ballantyne CM, Kubes P. Intraluminal crawling of neutrophils to emigration sites: a molecularly distinct process from adhesion in the recruitment cascade. J Exp Med. 2006;203:2569–2575. doi: 10.1084/jem.20060925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proebstl D, Voisin MB, Woodfin A, Whiteford J, D’Acquisto F, Jones GE, Rowe D, Nourshargh S. Pericytes support neutrophil subendothelial cell crawling and breaching of venular walls in vivo. J Exp Med. 2012;209:1219–1234. doi: 10.1084/jem.20111622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reymond N, Imbert AM, Devilard E, Fabre S, Chabannon C, Xerri L, Farnarier C, Cantoni C, Bottino C, Moretta A, Dubreuil P, Lopez M. DNAM-1 and PVR regulate monocyte migration through endothelial junctions. J Exp Med. 2004;199:1331–1341. doi: 10.1084/jem.20032206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sage PT, Carman CV. Settings and mechanisms for trans-cellular diapedesis. Front Biosci (Landmark Ed) 2009;14:5066–5083. doi: 10.2741/3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenkel AR, Mamdouh Z, Muller WA. Locomotion of monocytes on endothelium is a critical step during extravasation. Nat Immunol. 2004;5:393–400. doi: 10.1038/ni1051. [DOI] [PubMed] [Google Scholar]
- Schurpf T, Springer TA. Regulation of integrin affinity on cell surfaces. EMBO J. 2011;30:4712–4727. doi: 10.1038/emboj.2011.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw SK, Bamba PS, Perkins BN, Luscinskas FW. Real-time imaging of vascular endothelial-cadherin during leukocyte transmigration across endothelium. J Immunol. 2001;167:2323–2330. doi: 10.4049/jimmunol.167.4.2323. [DOI] [PubMed] [Google Scholar]
- Shulman Z, Shinder V, Klein E, Grabovsky V, Yeger O, Geron E, Montresor A, Bolomini-Vittori M, Feigelson SW, Kirchhausen T, Laudanna C, Shakhar G, Alon R. Lymphocyte crawling and transendothelial migration require chemokine triggering of high-affinity LFA-1 integrin. Immunity. 2009;30:384–396. doi: 10.1016/j.immuni.2008.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark K, Eckart A, Haidari S, Tirniceriu A, Lorenz M, von Bruhl ML, Gartner F, Khandoga AG, Legate KR, Pless R, Hepper I, Lauber K, Walzog B, Massberg S. Capillary and arteriolar pericytes attract innate leukocytes exiting through venules and ‘instruct’ them with pattern-recognition and motility programs. Nat Immunol. 2013;14:41–51. doi: 10.1038/ni.2477. [DOI] [PubMed] [Google Scholar]
- Stefanidakis M, Newton G, Lee WY, Parkos CA, Luscinskas FW. Endothelial CD47 interaction with SIRPgamma is required for human T-cell transendothelial migration under shear flow conditions in vitro. Blood. 2008;112:1280–1289. doi: 10.1182/blood-2008-01-134429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan DP, Seidman MA, Muller WA. Poliovirus receptor (CD155) regulates a step in transendothelial migration between PECAM and CD99. Am J Pathol. 2013;182:1031–1042. doi: 10.1016/j.ajpath.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svensson L, Howarth K, McDowall A, Patzak I, Evans R, Ussar S, Moser M, Metin A, Fried M, Tomlinson I, Hogg N. Leukocyte adhesion deficiency-III is caused by mutations in KINDLIN3 affecting integrin activation. Nat Med. 2009;15:306–312. doi: 10.1038/nm.1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buul JD, Hordijk PL. Endothelial adapter proteins in leukocyte transmigration. Thromb Haemost. 2009;101:649–655. [PubMed] [Google Scholar]
- van de Vijver E, Maddalena A, Sanal O, Holland SM, Uzel G, Madkaikar M, de Boer M, van Leeuwen K, Koker MY, Parvaneh N, Fischer A, Law SK, Klein N, Tezcan FI, Unal E, Patiroglu T, Belohradsky BH, Schwartz K, Somech R, Kuijpers TW, Roos D. Hematologically important mutations: leukocyte adhesion deficiency (first update) Blood Cells Mol Dis. 2012;48:53–61. doi: 10.1016/j.bcmd.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Meer AD, van den Berg A. Organs-on-chips: breaking the in vitro impasse. Integr Biol (Camb) 2012;4:461–470. doi: 10.1039/c2ib00176d. [DOI] [PubMed] [Google Scholar]
- Vestweber D. Novel insights into leukocyte extravasation. Curr Opin Hematol. 2012;19:212–217. doi: 10.1097/MOH.0b013e3283523e78. [DOI] [PubMed] [Google Scholar]
- Vockel M, Vestweber D. How T cells trigger the dissociation of the endothelial receptor phosphatase VE-PTP from VE-cadherin. Blood. 2013;122:2512–2522. doi: 10.1182/blood-2013-04-499228. [DOI] [PubMed] [Google Scholar]
- Voisin MB, Woodfin A, Nourshargh S. Monocytes and neutrophils exhibit both distinct and common mechanisms in penetrating the vascular basement membrane in vivo. Arterioscler Thromb Vasc Biol. 2009;29:1193–1199. doi: 10.1161/ATVBAHA.109.187450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Andrian UH, Chambers JD, McEvoy LM, Bargatze RF, Arfors KE, Butcher EC. Two-step model of leukocyte-endothelial cell interaction in inflammation: distinct roles for LECAM-1 and the leukocyte beta 2 integrins in vivo. Proc Natl Acad Sci U S A. 1991;88:7538–7542. doi: 10.1073/pnas.88.17.7538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Doerschuk CM, Mizgerd JP. Neutrophils in innate immunity. Semin Respir Crit Care Med. 2004;25:33–41. doi: 10.1055/s-2004-822303. [DOI] [PubMed] [Google Scholar]
- Wang S, Voisin MB, Larbi KY, Dangerfield J, Scheiermann C, Tran M, Maxwell PH, Sorokin L, Nourshargh S. Venular basement membranes contain specific matrix protein low expression regions that act as exit points for emigrating neutrophils. J Exp Med. 2006;203:1519–1532. doi: 10.1084/jem.20051210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J, Johnston B, Lee SS, Bullard DC, Smith CW, Beaudet AL, Kubes P. A minimal role for selectins in the recruitment of leukocytes into the inflamed liver microvasculature. J Clin Invest. 1997;99:2782–2790. doi: 10.1172/JCI119468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J, Luo BH, Xiao T, Zhang C, Nishida N, Springer TA. Structure of a complete integrin ectodomain in a physiologic resting state and activation and deactivation by applied forces. Mol Cell. 2008;32:849–861. doi: 10.1016/j.molcel.2008.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]