Abstract
Introduction: The primary aims of this study were to assess the learning curve effect of robot-assisted radical prostatectomy (RARP) in a large administrative database consisting of multiple U.S. hospitals and surgeons, and to compare the results of RARP with open radical prostatectomy (ORP) from the same settings.
Materials and Methods: The patient population of study was from the Premier Perspective Database (Premier, Inc., Charlotte, NC) and consisted of 71,312 radical prostatectomies performed at more than 300 U.S. hospitals by up to 3739 surgeons by open or robotic techniques from 2004 to 2010. The key endpoints were surgery time, inpatient length of stay, and overall complications. We compared open versus robotic, results by year of procedures, results by case volume of specific surgeons, and results of open surgery in hospitals with and without a robotic system.
Results: The mean surgery time was longer for RARP (4.4 hours, standard deviation [SD] 1.7) compared with ORP (3.4 hours, SD 1.5) in the same hospitals (p<0.0001). Inpatient stay was shorter for RARP (2.2 days, SD 1.9) compared with ORP (3.2 days, SD 2.7) in the same hospitals (p<0.0001). The overall complications were less for RARP (10.6%) compared with ORP (15.8%) in the same hospitals, as were transfusion rates. ORP results in hospitals without a robot were not better than ORP with a robot, and pretreatment co-morbidity profiles were similar in all cohorts. Trending of results by year of procedure showed no differences in the three cohorts, but trending of RARP results by surgeon experience showed improvements in surgery time, hospital stay, conversion rates, and complication rates.
Conclusions: During the initial 7 years of RARP development, outcomes showed decreased hospital stay, complications, and transfusion rates. Learning curve trends for RARP were evident for these endpoints when grouped by surgeon experience, but not by year of surgery.
Introduction
Since 2004, many U.S. and worldwide hospitals have invested in robot-assisted surgery systems for the purpose of improving patient outcomes and decreasing the impact of surgery on work1 and regular activity. The index procedure leading the initial case volume was the robot-assisted radical prostatectomy (RARP), based upon reports from early adopters of advantages ranging from a faster learning curve, ergonomics, less bleeding/transfusion, faster recovery, fewer complications, and possibly functional.2–5 The cost of the systems was substantial in terms of initial purchase, yearly maintenance, and per-case disposables,6,7 yet hospitals and surgeon-advocates justified investment in the systems with the model of increased case volumes and improved outcomes.8 Therefore, there is an ongoing need to measure the benefits of robot-assisted surgery that can be expected across a general population cohort from mixed setting hospitals and surgeons. One such method of study is a population-based study of the learning curve of RARP using an administrative database that can track perioperative outcomes and complication rates.
We identified the Premier Perspective Database as a potential source for a learning curve study, as it includes a broad range of hospitals and surgeons,9–13 and can separately identify the technique of a prostatectomy, unlike many other databases that can only differentiate minimally invasive (robotic or laparoscopic) versus open. We focused our study on the strengths of the administrative database, as derived from the billing coded source data: perioperative parameters, complications, and correlations with surgeon case volume. The dataset is limited, however, to inpatient events immediately following the surgical procedure.
Materials and Methods
The source population was derived from Premier Research Services® (Premier, Inc., Charlotte, NC) Perspective Database, the largest, hospital, clinical, and economic database in the United States, developed to provide outcome quality and resource utilization benchmarking to its subscribers. The service contains inpatient and outpatient hospital-based billing and diagnostic codes from hospital-based clinics from a geographically diverse set of hospitals. The billing data include a date-stamped log of all billed items from procedures, medications, laboratory, diagnostic, and therapeutic services at the individual patient level. To our knowledge, no published studies using this database exist for prostate cancer, although representative studies in thoracic surgery and gynecology, among others, are available, for examples, of questions examined with this resource.10–13 This database allows radical prostatectomy (RP) procedures to be further identified as open radical prostatectomy (ORP), laparoscopic radical prostatectomy (LRP), or RARP, and hospitals can be subcategorized as offering RARP during this time frame or not. Surgeons can be identified in the dataset to assess case volume; however, the queries are blind to surgeries performed before the dates of study, and any activity at non-Premier hospitals.
The key endpoints of study feasible from the dataset were surgery time (incision to closure, i.e., excluding anesthesia time), inpatient stay, and complications. Surgery time and inpatient stay were objective data points captured by Premier Perspective. Complication rates were derived via inpatient stay diagnosis codes added to the record that would be consistent with a complication in a patient admitted for elective prostate surgery. Key diagnostic codes were queried again based upon a similar study by Shih et al.14 yielding the final categories: medical miscellaneous, anastomotic stricture, surgical miscellaneous, respiratory, cardiac, genitourinary, thromboembolic, wound/bleeding, vascular, transfusion, and mortality. The query methods were identical for all surgical modalities. The data do not permit Clavien-style complication grading,15 but the descriptors of the diagnosis would mostly fall into grades 3–5, that is, major complications. Co-morbidity was assessed by the All Patient Refined Diagnosis Related Groups (APR-DRGs), which is Premier's preferred co-morbidity tool, as it is designed to predict resource demands, rather than mortality.11
Prior to undertaking this study we obtained IRB approval from the MD Anderson Cancer Center and Tulane University Medical School. We requested a complete data set of all RP procedures from 2004 through 2010 (7 full years of data) that were performed at Premier's source hospitals. From that, we identified four useful cohorts for comparison: (1) ORP performed at any Perspective hospital (ORP-All; n=43,964), (2) ORP performed at a Perspective hospital with a robotic system in place at the same time interval (ORP-robotic hospital [RH]; n=30,124), (3) RARP (n=27,348), and (4) LRP (n=733). Given the objectives of this study and the very small size of the LRP cohort, this group was dropped from further analysis.
It is unknown which robotic system models were used for cases included in this study, nor whether this influences outcomes. For future reference, the company notes the following breakdown in systems sold in the United States: 2004, daVinci=92; 2005, daVinci=281+daVinci S=6; 2006, daVinci=292+daVinci S=129; 2007, daVinci=294+daVinci S=300; 2008, daVinci=279+daVinci S=545; 2009, daVinci=231+daVinci S=582+daVinci Si=214; and 2010, daVinci=160+daVinci S=579+daVinci Si=545. Note however, that as time goes by, previously sold systems may later go out of service.
Data analysis
Raw data from querying the Premier database were transferred directly to an independent statistical services contractor, Axistat, Inc. (San Francisco, CA), for analysis. Continuous variables were compared using a Student's t-test while discrete variables were compared using a chi-squared test. Comparisons for trends over time or surgical case volume used the Jonckheere–Terpstra test.16 A p-value of <0.05 was considered statistically significant. Analyses were carried out using SAS version 9.2.1 (SAS Institute, Cary, NC).
Key endpoints of study
The data queries can provide objective reports on length of hospital stay, surgery time, and most any complication that results in a new diagnostic code.
Results
We identified 71,312 RP performed at more than 300 hospitals by up to 3739 surgeons by open or robotic technique (excluding LRP as noted). Table 1 displays the relevant demographic and key endpoints for the three focused cohorts—ORP at non-RH, ORP-RH, and RARP. Within the hospitals with a robot, the mean time for ORP was 3.4 hours (standard deviation [SD]=1.5) and for RARP 4.4 hours (SD=1.7; p<0.0001). The mean length of stay for open was 3.4 days (SD=2.7) and for RARP 2.2 days (SD=1.9; p<0.0001). The overall complication rate was 15.8% for open and 10.6% for robotic (p<0.0001). Specific complication rates, shown in Table 2, were favorable to robotic and statistically significant: stricture 4.8% versus 3.2%, respiratory 2.3% versus 1.4%, cardiac 1.5% versus 0.6%, and blood transfusion 11.5% versus 2.3%. In the combined open cohorts with any discharge complications, they were single in 60% and multiple in 40%. The same analysis for robotic was single in 60% and multiple in 40%.
Table 1.
Demographics and Perioperative Outcomes
| ORP (non-robotic hospitals) | ORP (robotic hospitals) | RARP | P-values* | |
|---|---|---|---|---|
| Cases, n | 13,840 | 30,124 | 27,348 | |
| Hospitals, n | 205 | 142 | 142 | |
| Teaching (%) | 21 | 39 | 39 | 1.00, 0.0003, 0.0003 |
| Surgeons, n | 1228 | 1767 | 744 | |
| Lymphadenectomy, n (%) | 8100 (59) | 17, 911 (60) | 12,371 (45) | <0.0001, <0.001, 0.07 |
| Age (years), Mean ± SD | 63.5 ± 8.2 | 63.0 ± 8.2 | 61.0 ± 7.1 | <0.0001, <0.0001, 0.9986 |
| APR-DRG Severity, n (%) | ||||
| Minor | 8551 (61.8) | 18,745 (62.2) | 17,025 (62.3) | 0.3752 |
| Moderate | 3458 (25.0) | 7816 (26.0) | 7550 (27.6) | 0.3737 |
| Major | 485 (3.5) | 982 (3.3) | 997 (3.7) | 0.1046 |
| Extreme | 93 (0.7) | 193 (0.6) | 132 (0.5) | |
| Unknown | 1253 (9.1) | 2388 (7.9) | 1644 (6.0) | |
| Morbid obesity, n (%) | 94 (0.7) | 263 (0.9) | 231 (0.8) | 0.7127, 0.0730, 0.0354 |
| Surgery time (hours) Mean ± SD | 3.2 ± 1.43 | 3.4 ± 1.5 | 4.4 ± 1.7 | <0.0001, <0.0001,<0.0001 |
| Inpatient LOS (days) Mean ± SD | 3.7 ± 2.7 | 3.4 ± 2.7 | 2.2 ± 1.9 | <0.0001, <0.0001, <0.0001 |
| Overall Complications, n (%) | 2474 (17.9) | 4759 (15.8) | 2892 (10.6) | <0.001, <0.0001, <0.0001 |
Data are for all radical prostatectomy cases performed at Premier hospitals from 2004 to 2010.
p-Values are for RARP vs ORP (robotic hospitals), RARP vs ORP (non-robotic hospitals), and ORP (robotic hospitals vs non-robotic hospitals). Morbid obesity=BMI >35. Surgery time is the “skin-skin” time; that is, it excludes additional room/anesthesia time before and after the procedure.
SD=standard deviation; APR-DRG=All Patient Refined Diagnosis Related Group (APR-DRG) uses diagnostic, therapeutic, and demographic attributes to classify patients with similar resource demands (minor, moderate, major, and extreme); LOS=length of stay; RARP=robot-assisted radical prostatectomy; ORP=open radical prostatectomy; NA=not applicable.
Table 2.
Discharges with a Complication
| Complication, n (%) | ORP (non-robotic hospitals) n=13,840 | ORP (robotic hospitals) n=30,124 | RARP n=27,348 | P-values |
|---|---|---|---|---|
| Medical misc. | 923 (6.7) | 1725 (5.7) | 1147 (4.2) | <0.0001 |
| <0.0001 | ||||
| 0.0675 | ||||
| Anastomotic stricturea | 686 (5.0) | 1450 (4.8) | 870 (3.2) | <0.0001 |
| <0.0001 | ||||
| 0.5166 | ||||
| Surgical misc. | 485 (3.5) | 877 (2.9) | 584 (2.1) | <0.0001 |
| <0.0001 | ||||
| 0.0009 | ||||
| Respiratory | 383 (2.8) | 693 (2.3) | 356 (1.4) | <0.0001 |
| <0.0001 | ||||
| 0.0033 | ||||
| Cardiac | 247 (1.8) | 443 (1.5) | 175 (0.6) | <0.0001 |
| <0.0001 | ||||
| 0.0139 | ||||
| Genitourinary | 169 (1.2) | 379 (1.3) | 250 (0.9) | <0.0001 |
| 0.0005 | ||||
| 0.7451 | ||||
| Thromboembolic | 107 (0.8) | 224 (0.7) | 106 (0.4) | <0.0001 |
| <0.0001 | ||||
| 0.7394 | ||||
| Wound/bleeding | 57 (0.4) | 126 (0.4) | 98 (0.4) | 0.2208 |
| 0.3693 | ||||
| 0.9226 | ||||
| Vascular | 22 (0.2) | 142 (0.5) | 106 (0.4) | 0.1425 |
| <0.0001 | ||||
| <0.0001 | ||||
| Transfusion | 2360 (17.1) | 3449 (11.5) | 638 (2.3) | <0.0001 |
| <0.0001 | ||||
| <0.0001 | ||||
| Mortality | 19 (0.14) | 27 (0.09) | 9 (0.03) | 0.0066 |
| 0.0001 | ||||
| 0.1552 | ||||
| Overall complications | 2474 (17.9) | 4759 (15.8) | 2892 (10.6) | <0.0001 |
| <0.0001 | ||||
| <0.0001 |
Data are for all radical prostatectomy cases performed at Premier hospitals from 2004 to 2010.
See the “Discussion” section for further clarification, as “anastomotic strictures” during an inpatient stay likely do not represent complications from the radical prostatectomy.
Misc.=miscellaneous; p-values are for RARP vs ORP (robotic hospitals), RARP vs ORP (non-robotic hospitals), and ORP (robotic hospitals vs non-robotic hospitals).
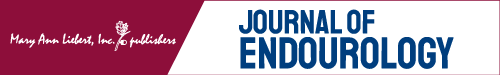
The separate cohort of ORP at non-RHs is also displayed in Tables 1 and 2 to explore the hypotheses that patient selection and/or quality of surgery may be different at these locations. There were fewer teaching hospitals comprising ORP-non-RH versus ORP-RH—21% versus 39% (p=0.0003). The differences in surgery time and LOS are statistically different but not likely clinically meaningful; however, ORP-non-RH had slightly higher complications at 17.9% versus 15.8% for ORP-RH. The array of specific complications (Table 2) shows a similar pattern of higher complications after ORP than RARP, and the highest transfusion rate at 17.1%. Table 1 also shows a Premier Perspective proprietary measure of co-morbidity called the APR-DRGs. The incidences of patients with minor, moderate, major, extreme, and unknown co-morbidity were statistically equivalent between the three cohorts. Complication rates by year of surgery are shown in Figure 1, and demonstrate a consistent trend for lower complication rates for RARP compared with either ORP cohort; however, there is no visible learning curve trend for high complications in year 1 (2004) followed by a decline.
FIG. 1.
Overall complication rates at Premier Perspective Hospitals from 2004 to 2010 during initial hospitalization: robotic, open at robotic hospitals, and open at non-robotic hospitals.
Next, we re-examined the key endpoints by surgeon case volume. There were 226 surgeons in this database who had completed 25 or more robotic cases, 132 surgeons who had completed 50 or more robotic cases, and 67 surgeons who had completed 100 or more cases. Table 3 shows the cohorts of robotic cases performed by surgeons in their first six 25 case increments. The conversion rate declined from 1.13% to 0.18%, the time decreased 5.0 to 3.9 hours, and the complications decreased 11.75% to 8.95%. The ARP-DRG measure was highly consistent within these 25 case increments, indicating fairly consistent patient selection by co-morbidity even in the first 25 cases.
Table 3.
RARP Learning Curve That Groups Initial Surgeon Cases by Groups of 25
| First 25 | Second 25 | Third 25 | Fourth 25 | Fifth 25 | Sixth 25 | |
|---|---|---|---|---|---|---|
| Variable | n=5650 | n=4208 | n=2638 | n=1914 | n=1496 | n=1128 |
| Conversion, n (%) | 64 (1.13) | 20 (0.48) | 11 (0.42) | 6 (0.31) | 3 (0.20) | 2 (0.18) |
| Surgery time, mean (SD) | 5.0 (1.84) | 4.5 (1.45) | 4.3 (1.36) | 4.1 (1.15) | 4.0 (1.02) | 3.9 (1.03) |
| LOS | 2.4 (1.96) | 2.2 (2.02) | 2.1 (1.95) | 2.0 (1.47) | 1.9 (1.32) | 2.0 (2.81) |
| Complications, n (%) | 664 (11.75) | 423 (10.05) | 239 (9.06) | 171 (8.93) | 129 (8.62) | 101 (8.95) |
| ARP-DRG severity | ||||||
| Minor | 3579 (63.4) | 2659 (63.1) | 1708 (64.8) | 1221 (63.8) | 992 (66.3) | 731 (64.8) |
| Moderate | 1589 (28.1) | 1247 (29.6) | 759 (28.8) | 568 (29.7) | 399 (26.7) | 309 (27.4) |
| Major | 272 (4.8) | 185 (4.4) | 86 (3.7) | 58 (3.0) | 44 (2.9) | 32 (2.8) |
| Extreme | 38 (0.7) | 16 (0.4) | 17 (0.6) | 5 (0.3) | 1 (0.1) | 3 (0.3) |
We then performed an additional query of the more extreme comparison of surgeons with <25 total RARP cases versus >25 (unlimited case volume for a surgeon, n=3236 cases vs 24,112). In comparing the sixth cohort of 25 cases, versus 25 and up, there were no significant improvements in conversions, operative time, or length of stay; however, total complications improved further to 5.7%—a demonstration of how results become affected by including surgeons who have “exited” the learning curve at some point.
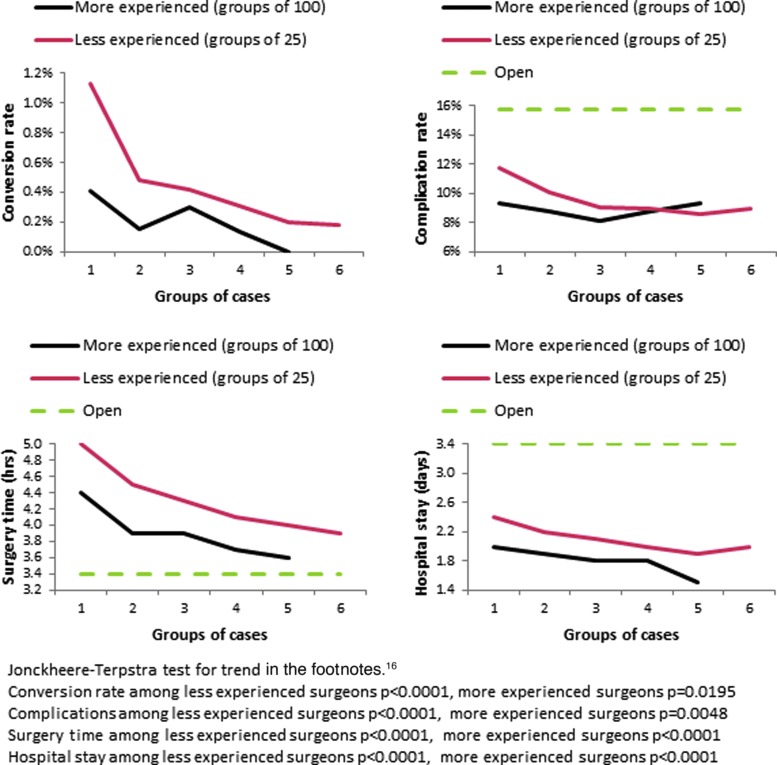
Figure 2 shows another view of the learning curve for RARP, where the more experienced surgeons' outcomes are plotted in multiples of 100 (black lines) versus less-experienced surgeons plotted in multiples of 25 (red line)—both series starting with the surgeons' first cases in the dataset.
FIG. 2.
Learning curve for surgeons by experience level, grouped into bundles of 25 (red) or 100 (black) cases: conversion rates, complication rates, surgery time, and hospital stay.
Discussion
Administrative databases offer prostate surgery outcomes, investigators, large volumes of cases, and events that are linked to definable billing/diagnostic codes, and require minimal additional expert interpretation. These databases may require a cost to access the data, but the investigators can quickly move to data analysis and interpretation. Therefore, endpoints, such as surgical time, hospital stay, and several Clavien grade 3–5 complications, are well captured with this method, and there is the added benefit of studying large numbers of surgeons and hospital settings. On the other hand, cancer control and quality of life endpoints that require additional follow-up, expert interpretation, and/or patient reported outcomes require a more costly research effort/infrastructure, and most of our knowledge of these outcomes derives from voluntary reporting from high-volume experts and early adopters.
The key questions posed by our study are whether or not learning curve trends can be detected in a large administrative dataset and how RARP outcomes have compared with ORP outcomes in the first 7 years of RARP adoption. For the RARP learning curve question, the data demonstrate improvements in conversion rates, complications, surgery time, and hospital stay (Fig. 2) when looking at surgeon volume. In particular, complication rates start in the 12% range initially, and decline to the 8% range within the first 100 cases, and may decline further in the extended case volume (>100 cases) to under 6%. Surgery time and hospital stay time also improve noticeably in the first 100 cases, and additional improvements beyond 100 cases. By contrast, the year of surgery did not demonstrate noteworthy trends to suggest that our techniques of training and instruction are improving with time. Our experiences living through the era of study, 2004–2010, would suggest to us that this was mostly an era of surgeons learning in the post-graduate career using brief hands-on training courses, a few proctored cases, and then straight to live-case learning. By contrast, learning curve studies moving forward will have a growing influence from surgeons who learned robotics as part of formal surgical residency/fellowship,17 extended post-graduate training,18 and/or have access to surgical simulation.19
Aside from the influence of the learning curve, the available comparisons between RARP and ORP demonstrate equivalent to favorable outcomes for RARP. As patients do not wish to suffer complications under any circumstance, the reduction in RARP complications would add value to their evaluation as to which technique to choose. For example, inpatient mortality rates were the lowest for robotic—0.03% versus 0.09%–0.14% for ORP (Table 2). In a formal cost-effectiveness study, the reduced complications and hospital stay would certainly factor into the total analysis. Currently the cost reporting within the Premier hospital network is not yet uniform enough to add such an analysis to our study, although some authors have included one despite the limitations.20
Our study has strengths and limitations worth highlighting. The data source includes a large catchment of surgeries from multiple hospitals and surgeons, thereby closely correlating with generalizable results of surgery. The data capture was prospective, and performed/monitored by an independent third party (Premier, Inc.). Premier undertakes an extensive multistep data validation and correction process, which includes more than 95 quality assurance checks. Once the validations are complete, the data are transferred to Premier's warehouse where they are maintained for health service research. In our study, the requested data were delivered directly to a third party analytics firm (Axistat, Inc.) for final production of tables and statistics for the investigators.
The limitations of this study include the lack of cost figures, functional outcomes, pathologic endpoints, and disease-free status, and therefore is only a partial analysis of comparative effectiveness. The other extreme of study strength is a well-conducted single-institution study such as Di Pierro et al.18 that can capture a full array of endpoints and show RARP with better positive surgical margins, major complications, urinary continence, and erectile function.
As with all non-randomized study designs, there may exist unknown patient selection differences between the open and RARP cohorts. We were particularly concerned with the influences of patient selection and quality of surgery between open surgeries performed at hospitals with versus without a robot. However, we found that the overall complication rate was lower for ORP in robotic versus non-RHs. The co-morbidity assessment was also identical across the cohorts (Table 1). These findings would argue against the conclusion that lower complications in RARP were due to selecting the healthiest patients. It is common knowledge that most surgeons attempting his/her initial RARP cases would select ideal surgical candidates; however, as Table 3 demonstrates in the ARP-DRG ratios, such selection is not even visible in the first 25 cases versus subsequent ones. As noted in the methods, this database is limited to inpatient events, and therefore does not capture additional complications that may occur at different rates in the outpatient setting. In addition, the learning curve analysis may be effected in that open surgery was always assumed to be an established technique in this time period, whereas robotic case learning curves were built on the estimated technology installation date.
It is also noteworthy that although administrative databases may provide large sample sizes of patients and a representative cross-section of surgeons, the data capture is mostly designed for hospital administration clients, rather than clinical outcome research, and in some cases may lack expert refinement in data capture. As an example, we designed our study, requested the data, and began our analysis, only to find anastomotic stricture rates of 3.2%–5.0%. However, for an inpatient data study, this would make little sense, as patients develop strictures weeks to months later, and not in the initial hospital stay. When we looked at each of 26 individual diagnostic codes used to define “anastomotic stricture,” we could only conclude that the events represented a mix of surgeons managing pre-existing strictures at the time of RP, or coders picking up on certain language elements of the documentation and adding these codes in ways that would have been revised by a clinician or researcher. Examples may include a complex bladder neck reconstruction from a large gland/median lobe, or lower urinary tract obstructive symptoms. All other complication categories such as the “vascular” category (23 separate codes) are consistent with inpatient care, such as carotid artery occlusion or major vein thrombosis with embolism. These examples point to possible biases in comparing studies based upon administrative data capture versus physician/researcher-based interpretation of events and capture.
Our study is consistent with several others with respect to comparing open versus robotic prostatectomy.21,22 Our dataset showed <1% use of LRP in this era, and we can probably assume that the LRP influence is also minimal in other studies from the United States.23 Hu et al.23 also showed that minimally invasive radical prostatectomy had fewer complications and shorter hospitalization, but higher anastomotic strictures and salvage therapy rates, unless higher surgeon volume was considered. This also points to the importance of the learning curve and training efforts. Sharma et al.24 looked at the learning curve of two surgeons for RARP in 500 cases. There was no open cohort, but improvements were seen throughout the series in several endpoints such as operative time. Agarwal et al.25 looked at comprehensive complications after RARP and found an overall rate of 9.8%. Of 368 complications in 326 patients, 81.3% occurred within 30 days, 4.6% from 31 to 90 days, and 14.1% after 90 days (driven by anastomotic stricture and lymphocele formation). Our study found 10.6% complications during initial inpatient stay, and therefore a comparable comprehensive complication study would show a higher rate, but by comparing a larger population of surgeons versus a single high-volume center.
Conclusions
During the initial 7 years of robotic RP development, an administrative database study of large numbers of patients and surgeons undergoing open and robotic RP demonstrated fewer complications, shorter length of stay, and reduced transfusion rates for robotic cases. Learning curve trends for robotics were evident for these endpoints when grouped by surgeon experience, but not by year of surgery.
Abbreviations Used
- APR-DRGs
All Patient Refined Diagnosis Related Groups
- LOS
length of stay
- LRP
laparoscopic radical prostatectomy
- ORP
open radical prostatectomy
- RARP
robot-assisted radical prostatectomy
- RH
robotic hospital
- RP
radical prostatectomy
- SD
standard deviation
Disclosure Statement
Funding for access to the Premier Database, and Axistat services: Intuitive Surgical. Authorship funding (J.W.D. and R.T.): none. Primary authorship: J.W.D. Data analysis: J.W.D. and U.K. Article editing and approval: J.W.D., J.G., U.K., and R.T.
References
- 1.Epstein AJ, Groeneveld PW, Harhay MO, et al. Impact of minimally invasive surgery on medical spending and employee absenteeism. JAMA Surg 2013;148:641–647 [DOI] [PubMed] [Google Scholar]
- 2.Ahlering TE, Skarecky D, Lee D, et al. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: Initial experience with laparoscopic radical prostatectomy. J Urol 2003;170:1738–1741 [DOI] [PubMed] [Google Scholar]
- 3.Patel VR, Tully AS, Holmes R, et al. Robotic radical prostatectomy in the community setting—the learning curve and beyond: Initial 200 cases. J Urol 2005;174:269–272 [DOI] [PubMed] [Google Scholar]
- 4.Menon M, Tewari A, Baize B, et al. Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: The Vattikuti Urology Institute experience. Urology 2002;60:864–868 [DOI] [PubMed] [Google Scholar]
- 5.Tewari A, Srivasatava A, Menon M, et al. A prospective comparison of radical retropubic and robot-assisted prostatectomy: Experience in one institution. BJU Int 2003;92:205–210 [DOI] [PubMed] [Google Scholar]
- 6.Binder J, Brautigam R, Jones D, et al. Robotic surgery in urology: Fact of fantasy? BJU Int 2004;94:1183–1187 [DOI] [PubMed] [Google Scholar]
- 7.Lotan Y, Cadeddu JA, Gettman MT. The new economics of radical prostatectomy: Cost comparison of open, laparoscopic and robot assisted techniques. J Urol 2004;172:1431–1435 [DOI] [PubMed] [Google Scholar]
- 8.Scales CD Jr, Jones PJ, Eisenstein EL, et al. Local cost structures and the economics of robot assisted prostatectomy. J Urol 2005;174:2323–2329 [DOI] [PubMed] [Google Scholar]
- 9.Ouriel K, Kaul AF, Leonard MC. Clinical and economic outcomes in thrombolytic treatment of peripheral arterial occlusive disease and deep venous thrombosis. J Vasc Surg 2004;40:971–977 [DOI] [PubMed] [Google Scholar]
- 10.Swanson SJ, Meyers BF, Gunnarsson CL, et al. Video-assisted thoracoscopic lobectomy is less costly and morbid than open lobectomy: A retrospective multiinstitutional database analysis. Ann Thorac Surg 2012;93:1027–1032 [DOI] [PubMed] [Google Scholar]
- 11.Pasic RP, Rizzo JA, Fang H, et al. Comparing robot-assisted with conventional laparoscopic hysterectomy: Impact on cost and clinical outcomes. J Minim Invasive Gynecol 2010;17:730. [DOI] [PubMed] [Google Scholar]
- 12.Shaw AD, Bagshaw SM, Goldstein SL, et al. Major complications, mortality, and resource utilization after open abdominal surgery, 0.9% saline compared to Plasma-Lyte. Ann Surg 2012;255:255.:821. [DOI] [PubMed] [Google Scholar]
- 13.Wright JD, Herzog TJ, Neugut AL, et al. Comparative effectiveness of minimally invasive and abdominal radical hysterectomy for cervical cancer. Gynecol Oncol 2012;127:11–17 [DOI] [PubMed] [Google Scholar]
- 14.Shih YC, Ward JF, Pettaway CA, et al. Comparative effectiveness, cost, and utilization of radical prostatectomy among young men within managed care insurance plans. Value Health 2012;15:367–375 [DOI] [PubMed] [Google Scholar]
- 15.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lunneborg CE. Jonckheere-Terpstra Test. Encyclopedia of Statistics in Behavioral Science. New Jersey: John Wiley & Sons, Inc., 2005 [Google Scholar]
- 17.Leroy TJ, Theil DD, Duchene DA, et al. Safety and peri-operative outcomes during learning curve of robot-assisted laparoscopic prostatectomy: A multi-institutional study of fellowship-trained robotic surgeons versus experienced open radical prostatectomy surgeons incorporating robot-assisted laparoscopic prostatectomy. J Endourology 2010;24:1665–1669 [DOI] [PubMed] [Google Scholar]
- 18.Di Pierro GB, Baumeister P, Stucki P, et al. A prospective trial comparing consecutive series of open retropubic and robot-assisted laparoscopic radical prostatectomy in a centre with limited caseload. Eur Urol 2011;59:1–6 [DOI] [PubMed] [Google Scholar]
- 19.Lallas CD, Davis JW. Robotic surgery training with commercially available simulation systems in 2011: A current review and practice pattern survey from the society of urologic robotic surgeons. J Endourol 2012;26:283–293 [DOI] [PubMed] [Google Scholar]
- 20.Wright JD, Ananth CV, Lewin SN, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA 2013;309:689–698 [DOI] [PubMed] [Google Scholar]
- 21.Cathcart P, Murphy DG, Moon D, et al. Perioperative, functional and oncological outcomes after open and minimally invasive prostate cancer surgery: Experience from Australasia. BJU Int 2011;107Suppl 3:11–19 [DOI] [PubMed] [Google Scholar]
- 22.Trinh QD, Sammon J, Sun M, et al. Perioperative outcomes of robot-assisted radical prostatectomy with open radical prostatectomy: Results from the nationwide inpatient sample. Eur Urol 2012;61:679–685 [DOI] [PubMed] [Google Scholar]
- 23.Hu JC, Wang Q, Pashos CL, et al. Utilization and outcomes of minimally invasive radical prostatectomy. J Clin Oncol 2008;26:2278–2284 [DOI] [PubMed] [Google Scholar]
- 24.Sharma NL, Papadopoulos A, Lee D, et al. First 500 cases of robotic-assisted laparoscopic radical prostatectomy from a single UK centre: Learning curves of two surgeons. BJU Int 2010;108:739–748 [DOI] [PubMed] [Google Scholar]
- 25.Agarwal PK, Sammon J, Shandari A, et al. Safety profile of robot-assisted radical prostatectomy: A standardized report of complications in 3317 patients. Eur Urol 2011;59:684–698 [DOI] [PubMed] [Google Scholar]