Abstract
Purpose
To report a case of spontaneous resolution of a long-standing serous macular detachment associated with an optic disc pit, leading to significant visual improvement.
Case Presentation
A 63-year-old female presented with a 6-month history of blurred vision and micropsia in her left eye. Her best-corrected visual acuity was 6/24 in the left eye, and fundoscopy revealed serous macular detachment associated with optic disc pit, which was confirmed by optical coherence tomography (OCT). The patient was offered vitrectomy as a treatment alternative, but she preferred to be reviewed conservatively. Three years after initial presentation, neither macular detachment nor subretinal fluid was evident in OCT, while the inner segment/outer segment (IS/OS) junction line was intact. Her visual acuity was improved from 6/24 to 6/12 in her left eye, remaining stable at the 6-month follow-up after resolution.
Conclusion
We present a case of spontaneous resolution of a long-standing macular detachment associated with an optic disc pit with significant visual improvement, postulating that the integrity of the IS/OS junction line may be a prognostic factor for final visual acuity and suggesting OCT as an indicator of visual prognosis and the probable necessity of a surgical management.
Key words: Optic disc pit, Macular detachment, Inner segment/outer segment, Optical coherence tomography, Spontaneous resolution
Introduction
Optic disc pit consists of an imperfect closure of the superior edge of the embryonic fissure, leading to an oval, gray-white depression in the optic disc that can be congenital or acquired [1, 2]. It is considered a rare clinical entity with an incidence of about 1 in 10,000, being bilateral in 15% of the cases and most commonly located inferotemporally on the optic disc [2]. Optic disc pits can be asymptomatic, but the majority of them may present macula-related complications such as serous retinal detachment (25–75%) or cystoid macular edema affecting visual acuity [1, 2]. It has also been referred that optic disc pits may result in arcuate scotoma or an enlarged blind spot [2].
Treatment alternatives for optic disc pit include conservative management, laser photocoagulation, macular buckling surgery, vitrectomy with or without internal limiting membrane (ILM) peeling, gas tamponade and the combination of them [3, 4, 5, 6]. Although few cases of spontaneous resolution of macular detachment due to optic disc pit have been reported in children [7, 8] and adults [1, 3, 9, 10, 11, 12, 13, 14], they most commonly result in poor visual outcome, especially if subretinal fluid persists more than 3 months [2, 14]. Herein, we report a rare case of spontaneous resolution of a long-standing (3 years) serous macular detachment associated with an optic disc pit leading to significant visual improvement, which remained stable at the 6-month follow-up.
Case Presentation
A 63-year-old female presented at the outpatients department complaining about blurred vision and micropsia in her left eye for 6 months. She had no other symptoms, no previous ocular history and her general health was unremarkable. On examination, her best-corrected visual acuity was 6/7.5 in the right eye and 6/24 in the left eye. Slit-lamp examination revealed immature cataract in both eyes (+1 nuclear sclerosis), and both anterior segments were normal. Intraocular pressure was normal in both eyes as well. Dilated fundoscopy revealed normal fundus in the right eye and a serous elevation of the macular region in the left eye, for which the patient was referred to the medical retina department for further investigation.
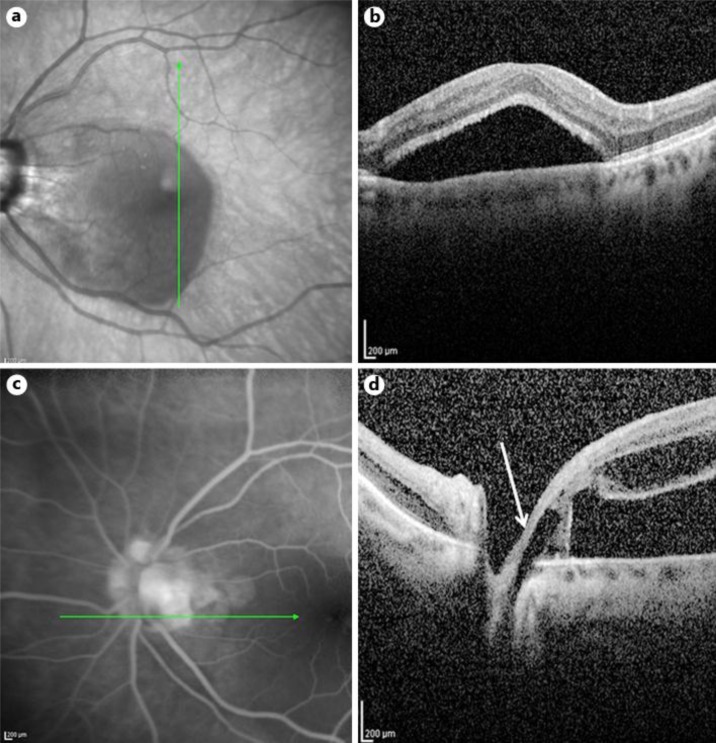
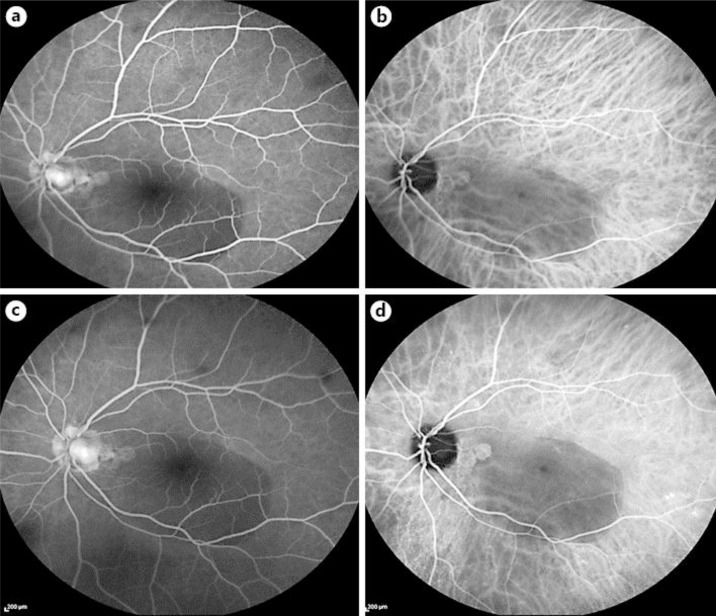
A more detailed fundus examination of the left eye revealed a large optic nerve head and a grey pit at the inferotemporal margin of the optic disc in association with serous macular detachment. Optical coherence tomography (OCT) confirmed the diagnosis of macular schisis communicating nasally with an optic disc pit, showing a hyporeflective area corresponding to the edge of the pit where there was communication with the schisis cavity (fig. 1). Fluorescein angiography (FA) and an indocyanine green angiogram excluded other causes of serous retinal pigment epithelium detachment, showing pooling in the area of serous macular detachment and no leakage from the pit even at the late stage (fig. 2). Additionally, MRI was performed to rule out any other abnormalities related to optic disc pit, but it was totally clear.
Fig. 1.
a, b Infrared photograph and OCT, showing serous macular detachment. c, d Infrared photograph and OCT, showing optic disc pit (arrow) associated with macular schisis.
Fig. 2.
a–d Early-phase FA and indocyanine angiogram and late-phase FA and indocyanine angiogram, showing serous macular detachment.
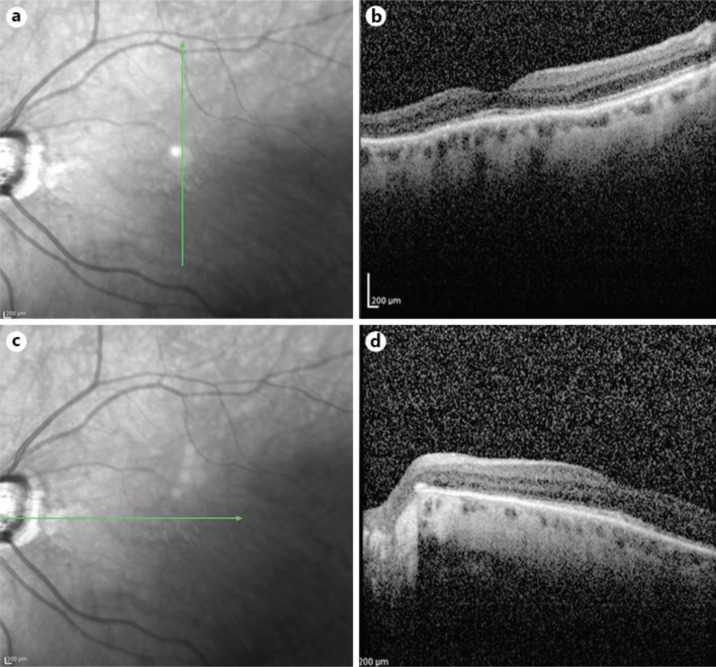
The patient was offered vitrectomy as a treatment alternative, but taking into account the potential risks and benefits of the surgery, she declined and was reviewed routinely on a 4-monthly basis. Interestingly enough, 3 years after initial presentation, neither macular schisis nor subretinal fluid were evident on OCT (fig. 3), and her visual acuity was significantly improved from 6/24 to 6/12 in the left eye, which remained stable at the 6-month follow-up after resolution of macular detachment.
Fig. 3.
a, b Infrared photograph and OCT, showing resolution of macular detachment. c, d Infrared photograph and OCT, showing the closure of the optic disc pit.
Discussion
There are previous studies describing the resolution of optic disc pit associated with serous macular detachments without treatment [1, 3, 9, 10, 11, 12, 13, 14]. Sugar [3] reported that 7 out of 8 cases with optic disc pit presented a clinically documented resolution of subretinal fluid, although final visual acuity was most dependent on initial visual acuity. This was in line with Brown et al., [9] who described spontaneous resolution of subretinal fluid in 5 out of 20 cases with optic disc pit, finding that those with a low initial visual acuity had a minimal improvement. Accordingly, Sobol et al. [10] found resolution of subretinal fluid in 4 out of 15 cases with a follow-up between 1 and 16 years, concluding that it is not advisable to allow the retina to remain detached for longer than 3 months due to irreversible changes. Moreover, Bonnet [11] reported resolution of macular detachment in 2 out of 4 cases with optic disc pit, without any intervention in a long-term follow-up of 8–10 years, but without improvement in visual acuity. This is in accordance with Poulson et al., [12] who also described a case of resolution of subretinal fluid after 2 years of follow-up without visual acuity improvement. In addition, a 43-year-old man exhibited similar subretinal fluid regression in a long-term follow-up of 2.5 years, with a visual acuity improvement from 6/60 to 6/18, as Patton et al. [13] described. Vedantham and Ramasamy [1] reported an OCT-resolution of subretinal fluid in parallel with a visual acuity improvement from 6/18 to 6/9 within 1 month after presentation. Finally, Cruzado-Sanchez et al. [14] presented the case of a 38-year-old female with optic disc pit who developed resolution of a serous macular detachment without treatment in 3 months after initial presentation and an improvement in visual acuity from 20/200 to 20/25. Therefore, based on the current literature, spontaneous resolution of macular detachments due to optic disc pit seldom happens, and if a macular detachment is long-standing, i.e., more than 3 months, it most probably results in poor visual outcome [1, 3, 9, 10, 11, 12, 13, 14]. Our case, however, exhibited significant improvement in visual acuity from 6/24 to 6/12 after spontaneous resolution of a long-standing serous macular detachment over a period of 3 years, which remains stable at the 6-month follow-up.
The pathophysiology of the origin of serous macular detachment in optic disc pit remains elusive [2]. Brown et al. [15] proposed that the fluid originates from the vitreous cavity. Other possible fluid sources are the leaky blood vessels at the base of the pit or the orbital space surrounding the dura [2]. Nevertheless, the most common theory included the communication between the subarachnoid and subretinal spaces, through which cerebrospinal fluid can move towards the submacular space [2]. As a result, the spontaneous closure of this communication could be attributed to a flow and pressure reduction at the level of the subarachnoid space, along with the firm adhesion between the neurosensory retina layers and the retina pigment epithelium [2].
Optic disc pit diagnosis is based mainly on fundus examination and OCT, which reveals the dual morphology of the detachment with a schisis cavity and a coexisting outer layer detachment from the retinal pigment epithelium [2]. OCT can also be a helpful tool to assess the integrity of the inner segment/outer segment (IS/OS) junction line as well as the inner layers of the retina [16]. According to Theodossiadis et al., [16] the final visual acuity after surgical treatment of optic disc pit associated with macular detachment was related with the integrity of the IS/OS junction line and with visual acuity immediately after fluid absorption. Another prognostic factor for the final visual acuity may be the time for which the fluid remained in the subretinal space, as it can cause cystoid macular degeneration and irreversible visual impairment [2]. In our case, although the macular detachment was long-standing, the IS/OS junction line was intact, explaining the visual improvement after the resolution of subretinal fluid. As a result, OCT could not only be used for follow-up, but also as an indicator of visual prognosis, the necessity of a surgical management and the potential visual outcome.
As far as treatment modalities for optic disc pit are concerned, a conservative management can be adopted, although it often leads to poor visual outcomes [2, 3]. Laser photocoagulation is another alternative, but it is not widely used today [2, 6]. Theodossiadis [4] proposed a novel technique using macular buckling surgery to treat optic disc pit with promising results. However, the most recent alternative is vitrectomy with or without ILM peeling and gas tamponade with or without endolaser photocoagulation, presenting encouraging results [2, 5, 6].
In conclusion, optic disc pit is a rare clinical entity, which is very commonly associated with macular schisis and detachment, resulting in visual impairment. In these cases, the most widely accepted treatment is vitrectomy with or without ILM peeling, with or without endolaser photocoagulation and gas tamponade. Nevertheless, there are few cases with spontaneous resolution of macular detachment even if visual outcome is poor, especially in long-standing macular detachment. Our case exhibited spontaneous regression of optic disc pit associated with macular detachment after 3 years of follow-up as well as an improvement in visual acuity from 6/24 to 6/12, which remains stable at the 6-month follow-up. Taken as a whole, we postulate that the integrity of the IS/OS junction line may be a prognostic factor for final visual acuity and suggest OCT as an indicator of visual prognosis and probable necessity of surgical management.
Disclosure Statement
The authors declare that there are no conflicts of interest.
References
- 1.Vedantham V, Ramasamy K. Spontaneous improvement of serous maculopathy associated with congenital optic disc pit: an OCT study. Eye (Lond) 2005;19:596–599. doi: 10.1038/sj.eye.6701540. [DOI] [PubMed] [Google Scholar]
- 2.Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol. 2011;249:1113–1122. doi: 10.1007/s00417-011-1698-5. [DOI] [PubMed] [Google Scholar]
- 3.Sugar HS. Congenital pits in the optic disc and their equivalents (congenital colobomas and coloboma like excavations) associated with submacular fluid. Am J Ophthalmol. 1967;63:298–307. [PubMed] [Google Scholar]
- 4.Theodossiadis GP. Treatment of maculopathy associated with optic disc pit by sponge explant. Am J Ophthalmol. 1996;121:630–637. doi: 10.1016/s0002-9394(14)70628-2. [DOI] [PubMed] [Google Scholar]
- 5.Snead MP, James N, Jacobs PM. Vitrectomy, argon laser, and gas tamponade for serous retinal detachment associated with an optic disc pit: a case report. Br J Ophthalmol. 1991;75:381–382. doi: 10.1136/bjo.75.6.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Georgalas I, Petrou P, Koutsandrea C, Papaconstadinou D, Ladas I, Gotzaridis E. Optic disc pit maculopathy treated with vitrectomy, internal limiting membrane peeling, and gas tamponade: a report of two cases. Eur J Ophthalmol. 2009;19:324–326. doi: 10.1177/112067210901900230. [DOI] [PubMed] [Google Scholar]
- 7.Yuen CH, Kaye SB. Spontaneous resolution of serous maculopathy associated with optic disc pit in a child: a case report. J AAPOS. 2002;6:330–331. doi: 10.1067/mpa.2002.127921. [DOI] [PubMed] [Google Scholar]
- 8.Polunina AA, Todorova MG, Palmowski-Wolfe AM. Function and morphology in macular retinoschisis associated with optic disc pit in a child before and after its spontaneous resolution. Doc Ophthalmol. 2012;124:149–155. doi: 10.1007/s10633-012-9314-5. [DOI] [PubMed] [Google Scholar]
- 9.Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head. II. Clinical studies in humans. Ophthalmology. 1980;87:51–65. doi: 10.1016/s0161-6420(80)35278-0. [DOI] [PubMed] [Google Scholar]
- 10.Sobol WM, Blodi CF, Folk JC, Weingeist TA. Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology. 1990;97:1539–1542. doi: 10.1016/s0161-6420(90)32380-1. [DOI] [PubMed] [Google Scholar]
- 11.Bonnet M. Serous macular detachment associated with optic nerve pits. Graefes Arch Clin Exp Ophthalmol. 1991;229:526–532. doi: 10.1007/BF00203315. [DOI] [PubMed] [Google Scholar]
- 12.Poulson AV, Snead DR, Jacobs PM, Ahmad N, Snead MP. Intraocular surgery for optic nerve disorders. Eye (Lond) 2004;18:1056–1065. doi: 10.1038/sj.eye.6701572. [DOI] [PubMed] [Google Scholar]
- 13.Patton N, Aslam SA, Aylward GW. Visual improvement after long-standing central serous macular detachment associated with an optic disc pit. Graefes Arch Clin Exp Ophthalmol. 2008;246:1083–1085. doi: 10.1007/s00417-008-0824-5. [DOI] [PubMed] [Google Scholar]
- 14.Cruzado-Sánchez D, Luglio Valdivieso H, Lujan Nájar SM. Spontaneous resolution of macular detachment associated with congenital anomalies of the optic nerve: coloboma and optic disc pit (in English, Spanish) Arch Soc Esp Oftalmol. 2013;88:201–203. doi: 10.1016/j.oftal.2012.09.030. [DOI] [PubMed] [Google Scholar]
- 15.Brown GC, Shields JA, Patty BE, Goldberg RE. Congenital pits of the optic nerve head. I. Experimental studies in collie dogs. Arch Ophthalmol. 1979;97:1341–1344. doi: 10.1001/archopht.1979.01020020083020. [DOI] [PubMed] [Google Scholar]
- 16.Theodossiadis GP, Grigoropoulos VG, Liarakos VS, Rouvas A, Emfietzoglou I, Theodossiadis PG. Restoration of the photoreceptor layer and improvement of visual acuity in successfully treated optic disc pit maculopathy: a long follow-up study by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2012;250:971–979. doi: 10.1007/s00417-011-1918-z. [DOI] [PubMed] [Google Scholar]