Abstract
A 69-year-old woman presented with generalized myasthenia gravis and a left orbital cavernous hemangioma (OCH), which elevated the optic nerve and displaced the external eye muscles. Cyclosporine treatment induced a gradual size reduction in the OCH, and consequently contributed to improved external ocular symptoms in combination with immunosuppressant effects.
Key Words: Myasthenia gravis, External ocular symptoms, Orbital cavernous hemangioma, Cyclosporine
Introduction
Myasthenia gravis (MG) is an autoimmune neuromuscular disease leading to fluctuating muscle weakness and fatigue. Fluctuating double vision and ptosis are the hallmarks of external ocular muscle weakness in MG. We report an intraorbital tumor that caused an impairment of the eye movement in a MG patient, which was reduced in size by cyclosporine treatment.
Case Presentation
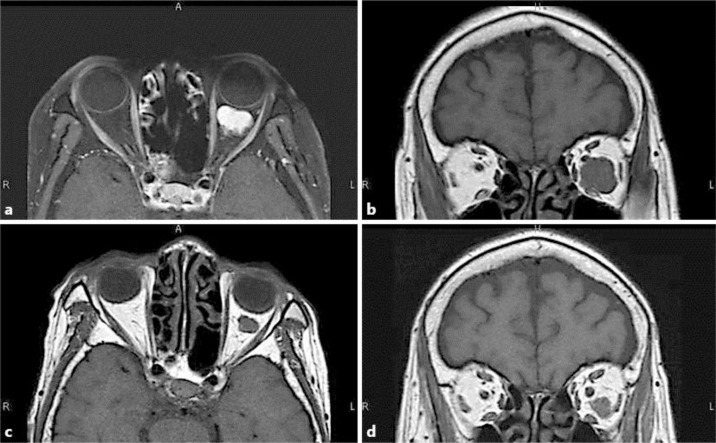
A 69-year-old woman had undergone a thymectomy at the age of 59 years because of a thymoma detected by routine chest X-ray examination. At the time of the thymoma detection, she had not shown any abnormal neurological symptoms. However, she has been suffering from symptoms such as moderate bilateral ptosis, severe diplopia, and muscle weakness after 10 years of thymoma operation, despite no recurrence of the thymoma. The affected muscles were the bilateral external ocular muscles, pharyngeal musculature, neck extensor muscle, deltoid, biceps, triceps, and iliopsoas. In particular, her left eye movement was limited in all directions. The diplopia developed at approximately the same time as the onset of the ptosis, and the extremity muscle weakness occurred during the 6 months following the onset of the external ocular symptoms. MG was diagnosed by the fluctuating symptoms, the waning detected in a repetitive nerve stimulation test on the median nerve, and positive test results for the acetylcholine receptor (AChR) antibody. The patient's quantitative MG score [1] was of 24 points. After plasma exchange treatment, her qualitative MG score improved to 11 points. The AChR antibody titer at the initial visit was 250 μmol/l. The antibody titer decreased to 95 μmol/l after plasmapheresis (PP) treatment. However, improvement of the left external ocular movement (EOM) without ptosis was poor compared to the improvements in the right EOM, dysphagia, and limb muscles weakness. An orbital MRI was performed because the diplopia did not respond to PP or an edrophonium test, and revealed an intraorbital tumor of 3 cm in diameter. The tumor was diagnosed as an orbital cavernous hemangioma (OCH) by the imaging characteristics (fig. 1a, b). It was followed closely without treatment because the patient did not want surgical treatments for the tumor. She was treated with cyclosporine A (CsA) at concentrations from 100 to 150 ng/ml in order to improve the MG symptoms after PP treatment. Her diplopia began to improve thereafter over the course of 6 months. A follow-up MRI showed a reduction in the tumor size. The improvement of the left eye movement was paralleled by a significant reduction of the tumor rather than a change in the AChR antibody titer, although it was further reduced to 72 μmol/l by CsA therapy. On the other hand, continuing CsA therapy at concentrations of 100 to 150 ng/ml increased her systolic blood pressure to 160 mm Hg and decreased her glomerular filtration rate to 45 ml/min. In response to these adverse effect, the CsA concentration was controlled in the range from 75 to 100 ng/ml, which maintained blood pressure within the normal range and a glomerular filtration rate over 50 ml/min. After 7 years, a follow-up MRI was performed and the AChR antibody titer was 5.0 μmol/l. The CsA concentration was kept in the range from 75 to 100 ng/ml, and the tumor was maintained at a size that does not affect the EOM (fig. 1c, d).
Fig. 1.
Orbital MRI. a, b The MRI was performed when the patient was hospitalized for the first time after PP treatment. a A short T1 inversion recovery axial image with contrast enhancement at the first examination is presented. Well-enhanced masses, 3 cm in diameter, in the left orbit are shown. b T1-weighted coronal image. The mass lifted the optic nerve diagonally forward and right and displaced the inferior rectus muscle inferiorly. A high-intensity lesion was shown in the inferior rectus muscle. c, d The MRI was performed 7 years after the initial visit. T1-weighted axial and coronal images without contrast enhancement. The mass volume decreased in size and the optic nerve returned to its normal position. The intramuscular high-intensity area regressed.
Discussion
OCH is the most common benign neoplasm of the orbit in adults, whereas the prevalence of MG is only 11.8 per 100,000 in Japan [2]. There is no causal relationship between MG and OCH, however, the EOM in this case was affected by OCH. Diplopia is not a life-threatening condition, but it represents a serious problem affecting the quality of life in MG.
To the best of our knowledge, there are no prior reports on the management of OCH discovered in the course of treatment of MG, which is why we considered this case particularly interesting. The clinical course, wherein thymoma preceded the myasthenia symptoms, was atypical. However, in our hospital, we have experienced the same clinical course of MG before [3].
OCH is usually a slow-growing tumor; its pathology is a benign, noninfiltrative, and slowly progressive vascular neoplasm composed of endothelial lined spaces surrounded by a well-delineated fibrous capsule. As for treatment, surgical excision is performed when symptomatic visual impairment occurs because of the involvement of the optic nerve, extraocular muscles, or surrounding vasculature.
In the present case, the tumor gradually reduced in size without surgery; this is an unlikely natural course. This patient was treated with CsA. The vasoconstrictive effects of calcineurin inhibitors such as CsA and tacrolimus are related to interference with the balance of vasoactive substances, including endothelin and nitric oxide. It has been demonstrated that CsA causes both systemic and renal vasoconstriction [4]. Renal vasoconstriction is thought to be caused by the production of endothelin in larger preglomerular arteries, where it acts via the endothelin receptor [5]. Some studies have suggested that CsA impairs vasodilation rather than causing vasoconstriction per se. Studies in isolated rat mesenteric artery resistance vessels showed that CsA impaired vasodilation by reducing nitric oxide [6]. We are convinced that the tumor size reduction was induced by the influence of vasoactive substances, and modified by the effects of CsA on endothelial structures. Vasoconstrictor effects are one of the important adverse effects of CsA that contributed to the tumor reduction in the present case, and resulted in the improvement of the EOM.
The use of CsA and the tumor size reduction were the result of an incidental beneficial reaction. It is needless to say that it is important to clinically examine the orbital MRI when MG patients experiences EOM impairment and is poorly responsive to the combination of immunological therapy with PP.
Disclosure Statement
The authors have no financial conflicts of interest to disclose concerning this case report.
References
- 1.Jaretzki A, 3rd, Barohn RJ, Ernstoff RM, Kaminski HJ, Keesey JC, Penn AS, Sanders DB. Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Neurology. 2000;55:16–23. doi: 10.1212/wnl.55.1.16. [DOI] [PubMed] [Google Scholar]
- 2.Murai H, Yamashita N, Watanabe M, Nomura Y, Motomura M, Yoshikawa H, Nakamura Y, Kawaguchi N, Onodera H, Araga S, Isobe N, Nagai M, Kira J. Characteristics of myasthenia gravis according to onset-age: Japanese nationwide survey. J Neurol Sci. 2011;305:97–102. doi: 10.1016/j.jns.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Wakata N, Fukuya H, Niizuma M, Ishida T, Kinoshita M. Myasthenia gravis developing after discovery of thymoma. Clin Neurol Neurosurg. 1992;94:303–306. doi: 10.1016/0303-8467(92)90178-6. [DOI] [PubMed] [Google Scholar]
- 4.Kaye D, Thompson J, Jennings G, Esler M. Cyclosporine therapy after cardiac transplantation causes hypertension and renal vasoconstriction without sympathetic activation. Circulation. 1993;88:1101–1109. doi: 10.1161/01.cir.88.3.1101. [DOI] [PubMed] [Google Scholar]
- 5.Cavarape A, Endlich K, Feletto F, Parekh N, Bartoli E, Steinhausen M. Contribution of endothelin receptors in renal microvessels in acute cyclosporine-mediated vasoconstriction in rats. Kidney Int. 1998;53:963–969. doi: 10.1111/j.1523-1755.1998.00852.x. [DOI] [PubMed] [Google Scholar]
- 6.Roullet JB, Xue H, McCarron DA, Holcomb S, Bennett WM. Vascular mechanisms of cyclosporin-induced hypertension in the rat. J Clin Invest. 1994;93:2244–2250. doi: 10.1172/JCI117222. [DOI] [PMC free article] [PubMed] [Google Scholar]