Abstract
Residents of environmental justice (EJ) communities may bear a disproportionate burden of environmental health risk, and often face additional burdens from social determinants of health. Accounting for cumulative risk should include measures of risk from both environmental sources and social determinants. This study sought to better understand cumulative health risk from both social and environmental sources in a disadvantaged community in Texas. Key outcomes were determining what data are currently available for this assessment, clarifying data needs, identifying data gaps, and considering how those gaps could be filled. Analyses suggested that the traditionally defined EJ community in Port Arthur may have a lower environmental risk from air toxics than the rest of the City of Port Arthur (although the entire city has a higher risk than the average for the state), but may have a larger burden from social determinants of health. However, the results should be interpreted in light of the availability of data, the definitions of community boundaries, and the areal unit utilized. Continued focus on environmental justice communities and the cumulative risks faced by their residents is critical to protecting these residents and, ultimately, moving towards a more equitable distribution and acceptable level of risk throughout society.
Keywords: cumulative risk, environmental justice, social determinants of health
INTRODUCTION
“Environmental justice” communities, that is, poor and minority communities that bear a disproportionate burden of environmental health risk, are a particular group that is inadequately served by current environmental risk assessment methods (Sexton 1997; IOM 1999; Morello-Frosch and Shenassa 2006; deFur et al.2007). Conventional environmental risk assessment methods historically have focused on individual chemicals from particular sources, with exposures occurring via single pathways and routes. But attention is now shifting to the need to conduct more holistic risk assessments that take into account exposures to both chemical and nonchemical stressors from multiple sources, all of which occur through diverse exposure pathways and routes (Fiscella and Williams 2004; Gee and Payne-Sturges 2004; Callahan and Sexton 2007; NEJAC 2004, 2010; Sexton and Linder 2010; WHO 2010).
Today, there is strong recognition that socioeconomically disadvantaged populations, many of whom are ethnic and racial minorities, have the potential to experience higher rates of morbidity and mortality due to the cumulative effects of exposure to environmental stressors, including chemical agents (e.g., benzene), physical agents (e.g., noise, build environment), biological agents (e.g., disease vectors), and psychosocial agents (e.g., unemployment, lack of access to health care) (Linder et al. 2008; Su et al. 2009). A number of recent studies have shown the importance of taking both environmental chemicals and social determinants of health into account when assessing the cumulative effects of environmental stressors on health, especially in environmental justice and other vulnerable communities (Schulz and Northridge 2004; Morello-Frosch and Lopez 2006; MRC 2009).
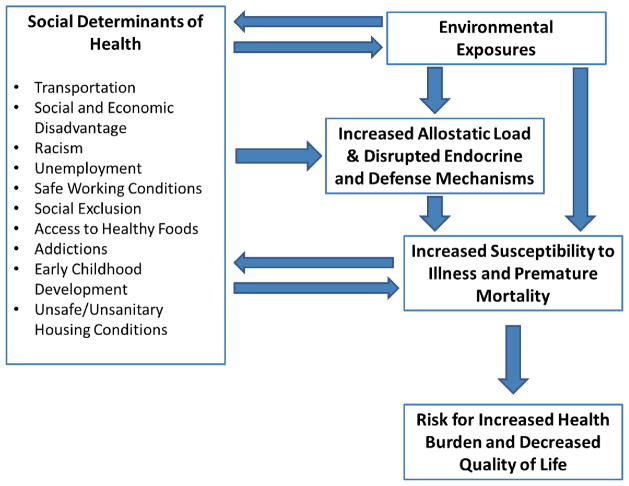
Examining cumulative impacts of sources of environmental risk, in combination with health risks due to adverse social determinants, supports a broader understanding of cumulative risk in environmental justice communities (Payne-Sturges and Gee 2006; Soobader et al. 2006; Linder and Sexton 2011; Sexton and Linder 2011). Overall, social determinants of health are found to be a significant influence on health inequities—the unfair and avoidable differences in health status seen within and between populations (CDC 2010). Social determinants of health play both direct and indirect roles in the health of populations (see Figure 1). Determinants such as social and economic disadvantage, racism, under- and unemployment, unsafe or insecure employment conditions and social exclusion create stressful conditions that serve to increase allostatic load and disrupt the body’s endocrine and defense mechanisms, thereby increasing susceptibility to illness and premature mortality. At the same time, diminished access to healthy foods, addictions, and poor early childhood development conditions also impact a number of physiological functions, including the pathway described above. Many of these determinants and health outcomes create feedback cycles that perpetuate and worsen declines in health outcomes among populations. Adding additional exposures to environmental health threats only serves to further complicate these processes and create even more vulnerable populations (Wilkinson and Marmot 2003).
Figure 1.
Framework for cumulative risk.
Our goal in this study was to obtain a better understanding of the cumulative risk borne by residents in an U.S. Environmental Protection Agency (USEPA)-designated Environmental Justice Showcase Community. In 2010, the USEPA identified one Showcase Community for each of its 10 U.S. regions, selecting communities with multiple, disproportionate environmental health burdens, population vulnerability, and limits to effective participation in decisions with environmental and health consequences (Wilkinson and Marmot 2003). This study focused on the West-Side area of Port Arthur, Texas—the Showcase Community for USEPA Region VI. To better understand cumulative risk from both environmental and social sources in this community, we determined what data were available to conduct this broader assessment, clarified data needs and identified data gaps, and considered how those gaps could be filled. The findings from this assessment provide a starting point for broadening our understanding of how multiple environmental and social factors interrelate to impact the health and quality of life of residents in disadvantaged communities.
METHODS
Setting
Port Arthur, Texas, is a coastal industrial community located along the Texas-Louisiana border. The city has a long legacy of petrochemical refining and associated industries. Port Arthur is currently home to three major refineries with an overall capacity estimated at 809,000 barrels per calendar day in 2011 (roughly 17% of all refined output of Texas and 5% of the entire United States) (USEIA 2012). One refinery is currently undergoing expansion to become the largest refinery in the U.S., as well as to process products carried along the Keystone XL pipeline (Motiva 2012, TransCanada 2012).1 The city is also home to a hazardous waste incineration facility that processes, among other things, hydrolysate, a by-product of nerve gas, as well as PCBs (Ellick 2008; Veolia 2012; The Houston Chronicle 2008; Port of Port Arthur 2012). Additional sources of environmental pollutants are associated with the movement of goods to and from the community through the active marine port as well as major highways and rail lines. The area is also prone to negative impacts from hurricanes and other potential disasters related to being proximate to the Gulf Coast.
Port Arthur has a population of just over 51,000, according to the 2010 census (see Table 1) (BoC 2012a). Twenty-seven percent (27%) were aged 18 years or younger (higher than the national average of 24%), and 13.3% were 65 years old or older (about the national average). Roughly 40% of residents were Black or African-American, one-third (29.6%) of all residents were of Hispanic or Latino descent and 22.8% were White, non-Hispanic. Just under 75% of residents 25 years old or older graduated from high school (compared to the national average of 84.6%), and only 10.9% had a bachelor’s degree or higher (compared to 27.5% nationally). Nearly one-quarter (23.4%) of residents live below the poverty level, and median household income in 2009 was $30,339 (BoC 2012b).
Table 1.
Demographics of Port Arthur, Texas.
| West-Side Neighborhood | City of Port Arthur | |
|---|---|---|
| Population (est.) | 10,024 | 51,885 |
| Population with age 18+ | 25.5% | 27% |
| Population with age 65+ | 13.3% | |
| Black or African-American | 89.6% | 40% |
| Hispanic or Latino | 19.2% | 29.6% |
| White, non-Hispanic | 2.8% | 22.8% |
| % Ages 25+ with High School Diploma | 73.7% | 74.8% |
| % of Households with Incomes At or Below Poverty | 29.2% | 23.4% |
| Median Household Income | $19,900 | $30,339 |
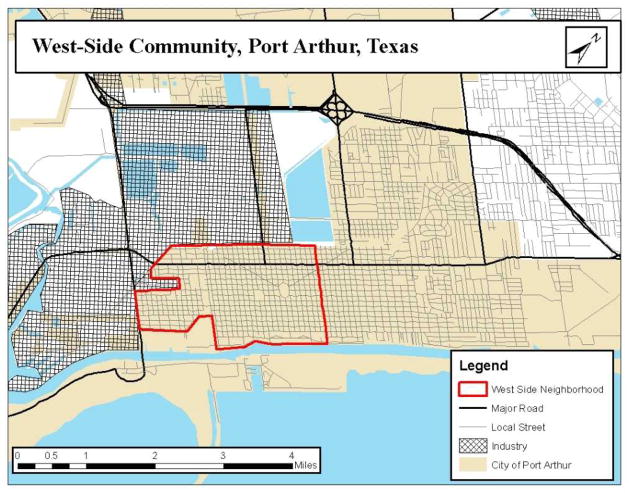
While these demographics describe Port Arthur’s residents as a whole, a particular neighborhood of about 10,000 residents on the west side stands out as an area of public health concern, and is the focus of this study (BoC 2012a). As can be seen in Figure 2, the West-Side neighborhood is surrounded by the petrochemical complex on the north and west sides, and a sea port to the south. A rail line and major highway bisect the community near the eastern edge. While this neighborhood has slightly fewer children than the average of the city (25.5% were aged 18 years old or younger), it is strongly minority: nearly 91.5% of the residents are Black or African-American and another 5% are Hispanic or Latino. Compared to Port Arthur as a whole, the West-Side had a slightly lower proportion of residents aged 25 or older (73.7%) who had a high school education. Nearly 30% live under the federal poverty level, and the median household income estimates for 2009 for the West-Side neighborhood was $19,900 (BoC 2012b).
Figure 2.
Location of the West-Side neighborhood.
In order to more critically examine the potential health concerns and accumulation of risk within this community, it is useful to identify particular health threats arising within the contexts of the geographic and demographic descriptors highlighted above. Specifically, what is the current status of environmental and social determinants of health within the West-Side neighborhood compared to other parts of Port Arthur, as well as Port Arthur as a whole? Among the most visible factors related to health within the West-Side neighborhood is the neighborhood’s close proximity to the surrounding port and petrochemical refining facilities. Potential risks occur both through potential sudden impacts, such as large unpermitted releases (such as those that occur during explosions or other industrial accidents) as well as long-term impacts related to chronic exposures such as through routine releases of toxicants, noise and light pollution, and activities related to goods movement to and from these facilities.
Added to threats to health and quality of life from these environmental exposures is a complex web of locally relevant social determinants of health including lack of access to affordable healthy foods, affordable quality childcare, affordable quality housing, and transportation, as well as relatively high rates of violence and crime, unemployment, vacant and dilapidated property, and economic disinvestment. Each of these determinants has a demonstrated correlation with health status and quality of life (San Francisco Department of Health 2012; Sundquist et al. 2006; Riva et al. 2007).
While the general risks attributed to each of these determinants individually have been documented in the research literature, only recently has research begun to focus on cumulative risk due to combined exposures, as well as the broader impact on population health. This study lays the groundwork for better understanding the multiple sources of health risk and their contributions to cumulative risk within a community by cataloging these various sources of risk due to both exposure to environmental toxics as well as social determinants of health, comparing those findings to nearby and broader populations, and reflecting on the sufficiency of readily available data.
Approach
Indicators
Researchers in partnership with a local non-profit community development and environmental justice advocacy group worked collaboratively to identify local conditions contributing to health risk among West-Side residents, and to develop appropriate indicators. Candidate indicators were identified from an inventory assembled through a literature review, from the Healthy Development Measurement Tool, and through previous experience with cumulative risk assessments (San Francisco Department of Health 2012). Joint community meetings to discuss local priorities and to map key community assets and hazards, combined with secondary data from national- and state-level databases, informed the selection of relevant local indicators of social determinants of health (Pacific Institute 2011). Priority was placed on selecting indicators that were 1) commonly used measures of critical constructs of environmental and social determinants of health and 2) readily available to other communities wishing to replicate this process. Priority was given to indicators readily available from federal databases, with state-level data being given second priority, as state-specific data may not be available in other communities (outside of Texas) seeking to replicate this process. All data were collected at the census tract level. The final inventory of selected indicators included:
-
Environmental Toxics
-
National Air Toxics Assessment (NATA) 2005 (USEPA 2011)
Diesel particulate matter
Cancer risk
Respiratory Risk
Neurological Risk
-
-
Social determinants of health
-
U.S. Census American Community Survey (ACS) 5-year estimates 2005–2009 (BoC 2012b)
Percent living in poverty
Percentage of single parent households
Racial segregation (concentration of minorities)
Median household income
Mean rent as a percentage of income
Percentage of residents who rent
Percentage of housing units that are vacant
Percentage of residents receiving supplemental nutrition assistance program (SNAP) benefits
Percentage of workers without access to a car
-
United States Department of Agriculture (USDA 2011)
Density of food outlets that accept Women, Children, and Infant (WIC) subsidies per population
Density of food outlets that accept SNAP benefits per population
-
Texas Department of Family and Protective Services (2012)
Density of licensed child care centers per population
-
Texas Alcoholic Beverage Commission (2012)
Density of facilities licensed for sales of alcohol intended for offsite consumption per population
-
Limitations of indicators
National Air Toxics Assessment (NATA) exposure models vary across the available years, and therefore should not be used to compare risk levels over time. Further, NATA is typically used to identify areas that may need closer investigation of toxic air emissions, or for planning more refined local assessments, and may not provide an accurate assessment of risk associated with air toxics (USEPA 2012). NATA also is limited in that it examines risk from air pollution only, and omits soil and water contamination, noise pollution, vibration, and other sources of environmental threats to health. Among local residents we communicated with in Port Arthur, the primary environmental source of risk is perceived to be airborne exposures. Therefore, for the purposes of this study, only exposures to air toxics will be considered for environmental risk.
Additionally, American Community Survey (ACS) data used in this analysis are averaged across 5 years. In some communities, there may be major population shifts due to disasters or other catastrophes that occur during this period and findings should be interpreted cautiously under those conditions. Some indicators are based on highly formal criteria, and may overlook more informal social and economic structures and processes. For instance, the child care indicator only covers providers that are licensed by the state, and excludes unlicensed operations, including informal care by a family member or neighbors, which can be a significant source of childcare among low to moderate income households, but can also present problems in terms of reliability, safety, and quality (Love et al. 2003). On the other hand, there are many indicators that have been shown to have a negative (or positive) impact on health that are not collected in easily accessible databases, and were not captured here.
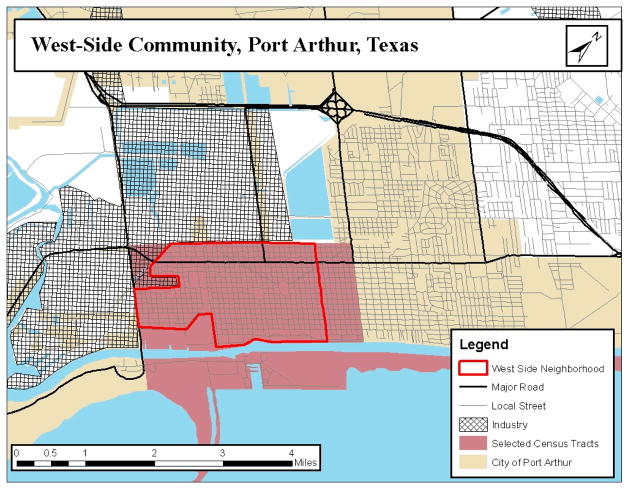
Analysis
Indicator data were collected for all census tracts in the City of Port Arthur from the sources listed above. The City of Port Arthur consists of 20 census tracts, 5 of which largely define the West-Side neighborhood (see Figure 3). Using community partner input, the boundaries of the West-Side neighborhood were drawn and the relevant census tracts were identified. There were some minor differences between the community’s boundary of the West-Side and the selected census tract boundaries, but the census tracts selected account for the entire West-Side neighborhood and extend beyond the eastern boundary by approximately 0.25 mile. Local community partners agreed that the extension beyond the local boundary of the neighborhood was not unreasonable, as this area’s population is similar to the residents within the locally drawn boundary. The selected tracts also include land south of the community, but this mostly rural area is predominantly not used as a residential area and is sparsely populated.
Figure 3.
Selected census tracts in relationship to the boundaries of the West-Side neighborhood.
Summary statistics for the various indicators were generated for each census tract. Statistical comparisons were made between West-Side neighborhood census tracts and the remainder census tracts for the City of Port Arthur using independent sample t-tests. To gain further context, similar t-tests were run for census tracts in Port Arthur compared to other census tracts within Jefferson County. Hotelling’s T2 tests were conducted to account for a cumulative effect of changes in all variables at once. The test was conducted (a) across all variables (both environmental and social), (b) only for the environmental variables, and (c) only for the social determinants variables.
Further, for each indicator, the West-Side neighborhood census tracts were compared to (a) the remainder of the census tracts in the city, (b) the city as a whole, (c) Jefferson County, and (d) the State of Texas, to give a broader base for comparison. Statistical tests for significance were conducted for differences between the West-Side neighborhood and the rest of Port Arthur, but not for comparisons across the city, county, and state, as comparing different ecological levels could be invalid (i.e., potentially introducing an ecological fallacy in comparing census tracts to broader population averages). Geospatial data were collected, stored and manipulated using ArcGIS 9.3 (ESRI 2008). Statistical tests were run using Stata 9.2 (StataCorp 2007).
RESULTS
Summarized in Table 2 are demographic, environmental risk, and social determinant indicators for the West-Side neighborhood, the remainder of the city, Port Arthur as a whole, Jefferson County, and the State of Texas. Data in the table suggest that risk for cancer, neurological conditions, and respiratory health problems experienced by the West-Side neighborhood due to air toxics is lower than the comparable areas in Port Arthur. Cumulative comparisons were found to be statistically significant (Hotelling’s T2: F = 5.5312, p = 0.0061). Individual t-tests also suggest this area experiences higher risks associated with social determinants of health; however, Hotelling’s T2 were not statistically significant for either the social determinants only variables (F = 1.677, p = 0.2248) or the overall model with all variables (F = 2.0328, p = 0.223).
Table 2.
Results of indicator analysis and selected independent samples t-tests.
| Indicator | West-Side Neighborhood | Rest of Port Arthur | City of Port Arthur | Jefferson County | State of Texas |
|---|---|---|---|---|---|
| Population (est.) | 12,028 | 39,857 | 51,885 | 254,759 | 23,819,042 |
| NATA Environmental Risk Measures | |||||
| Air toxicant risk | |||||
| Diesel Particulate Matter | .095453 | .1163001 | 0.1090036 | 0.1703616 | N/A |
| Health Risks | |||||
| Cancer Risk | .0000476* | .0000552 | 0.0000525 | 0.0000576 | 0.0000002 |
| Respiratory Risk | 1.443836* | 1.924338 | 1.756162 | 2.285726 | .0100898 |
| Neurological Risk | .0497525* | .0544296 | 0.0527926 | 0.0632285 | .00028223 |
| Social Determinants of Health | |||||
| Percent living in poverty | 28.9%* | 18.7% | 22.3% | 20.0% | 16.8% |
| Percentage of single parent households | 17.4%* | 10.7% | 13.0% | 12.1% | 12.8% |
| Percent minority | 94.3%* | 50.9% | 66.1% | 48.9% | 47.8% |
| Median household income | $21,634.71* | $36,602.77 | $31,363.95 | $39,496.95 | $48,199 |
| Rent as a percentage of income | 35.2%* | 27.9% | 30.5% | 30.31% | 29.4% |
| Percentage of residents who rent | 38.9% | 32.5% | 34.8% | 36.5% | 33.1% |
| Percentage of housing units that are vacant | 18.0% | 14.0% | 15.4% | 13.0% | 11.8% |
| Percentage receiving SNAP benefits | 27.6%* | 18.7% | 21.8% | 17.9% | 9.9% |
| Percentage without a vehicle | 12.2%* | 2.1% | 5.6% | 3.8% | 2.6% |
| # of WIC outlets / 1000 population | 0 | 0.10 | 0.08 | 0.08 | 0.01 |
| # of snap outlets / 1000 population | 1.58 | 1.15 | 1.25 | 0.89 | 0.70 |
| # of licensed child care providers / 1000 | 0.33 | 0.38 | 0.37 | 0.34 | 0.44 |
| # of alcohol vendors / 1000 population | 1.16 | 1.53 | 1.45 | 1.39 | 1.15 |
- Difference between the West-Side neighborhood and the rest of Port Arthur was statistically significant at the p = 0.05 level for individual t-test
N/A - not available
According to these data, the West-Side neighborhood may face lower relative risks than the rest of the city for three measures of risk related to air toxics, with statistically significant differences estimated for three of the four indicators. These findings may be a result of a number of factors, many of which potentially stem from the methodology behind NATA modeling, with data sources not being concentrated geographically at such a local level. Also, the prevailing wind from the south likely tends to push environmental toxicants released by the petrochemical industry away from the community. However, the cumulative impacts of the social determinants, as well as the impacts of these variables combined with environmental sources of risk, cannot be statistically demonstrated in the results of this study.
This community may shoulder relatively heavier burdens compared to the rest of the city in regard to social determinants of health. High levels of low income households are indicated by relatively higher proportions of persons living below the federal poverty level, rent overburdened households, single parent households, and decreased median household income.
There are significantly more residents receiving SNAP benefits in the West-Side neighborhood relative to the rest of Port Arthur. And while the difference technically is not statistically significant, access to vendors carrying healthy, affordable foods (i.e., large grocery stores, supermarkets and other facilities accepting W.I.C. benefits) is essentially non-existent within the West-Side neighborhood. Residents must travel upwards of 4 miles in many instances to reach a store selling a variety of healthy and affordable foods, a problem compounded by the significantly higher portion of West-Side without access to a vehicle. This deficit related to nutritional intake is partially addressed locally by an increase in vendors that accept SNAP benefits, which increases access to affordable but not necessarily a range of healthful food. Examples include convenience stores, which typically have higher prices than supermarkets and a limited range of healthful options.2
Finally, there are relatively fewer licensed childcare providers in the West-Side neighborhood. Given the larger proportion of single parent households in this community, having access to affordable, quality childcare is essential for parents seeking opportunities for gaining and maintaining employment, workforce development training activities, or other activities related to improving the family’s overall position. Without licensed child-care, parents may be forced to rely on unregulated informal childcare, which raises questions in relation to safety, reliability, and quality, among other issues.
DISCUSSION
While the environmental and health risk indicators derived from NATA data showed the West-Side neighborhood to be better off relative to the rest of the City of Port Arthur, the city as a whole, and the county, these differences were small compared to state level data, suggesting that the region as a whole is quite similar, and at potentially higher risk than Texas averages (see Table 2) (USEPA 2011). And while some localized areas may have higher burdens than others, much of the entire county appears to be affected by the local petrochemical industry and activities related to the port and goods movement.
The most significant local differences found relate rather to social determinants of health, especially rates of poverty and minority concentration. Specifically, residents living in close proximity to large industrial facilities and near routes related to goods movement were also likely to have relatively lower access to healthy foods, live in an area facing more concentrated poverty, and be more racially segregated, among other disadvantages. While the cumulative differences in these variables were not shown to be statistically significant, there are a number of potential reasons for this. First, the sample size of this study was relatively small, with Port Arthur having 20 census tracts. Second, while there were differences between the West-Side neighborhood and the rest of the city, as stated earlier, this comparison does not account for the overall status of the city relative to state- and nation-wide averages.
While the findings related to concentrated poverty, availability of transportation, and racial segregation, suggest that the residents of the West-Side neighborhood may be carrying a higher health risk than their fellow Port Arthur residents due to social determinants of health; the relatively lower level of risk among West-Side residents in relation to environmental risks was not expected. These findings could be a result of four potential sources of bias. First, the comparatively small sample size suggests that the variability measured in these 20 census tracts may not have been sufficient to meet statistical significance. Second, the relative contributions to cumulative risk by each variable is likely not equal. For example, the risk posed by air emissions may be a different magnitude than the risk posed by density of childcare providers. This suggests that a weighting system might make an important contribution to accurate modeling of cumulative risk in communities. Also, the degree of risk may not have a linear relationship with distance or density (depending on the indicator). Third, the indicators utilized were limited to available secondary data. There are additional environmental and social sources of risk that could not be accounted for using only large publically available databases of secondary data. Two examples include additional sources of data related to environmental risk (e.g., soil and water pollution, etc.) and crime data, as well as a variety of factors that may be more difficult to quantify, such as social cohesion within a community. Finally, the defined boundary of the environmental justice community may be too geographically narrow, and risk accumulations may be occurring in this community on broader scales, such as across the entire city. Further examination of the surrounding area and its relationship with different definitions of the community boundary is needed.
Lower levels of environmental health risk for the fence line community of the West-Side neighborhood was an unexpected finding that warrants further investigation. Specifically, questions remain about the relative differences sources of health risk (particularly from air toxics) observed in the Westside Neighborhood compared to the rest of the City versus the apparently elevated estimates of risk from air toxics in the general region as a whole.
It is also possible that the findings may in fact be a result of data limitations, the finding reinforces the notion that, the limited data available to researchers through secondary sources needs to be expanded and standardized. In particular, more robust measures of air, water and soil exposures as well as social determinants of health and health outcomes at more refined geographic resolutions would yield a more refined analysis of environmental risk, if collected and made publicly available. The collection of such data through database sources is important because although primary data collection can fill information gaps, and local knowledge will serve an important function in identifying community priorities and guiding researchers down useful paths of inquiry, primary data collection is expensive and time-consuming, and potentially leads to studies with little external validity.
Finally, traditional statistical models may be too limited in their capacity to assess cumulative risk from these multiple sources. The relationships between the indicators and their impacts on cumulative health risk may potentially be linear or non-linear. Additional models of assessment may need to be applied to help in answering the questions around cumulative risk. Possible applications include the use of health impact assessments, as well as application of systems thinking methodologies, such as system dynamics modeling, agent based modeling, and other simulation techniques (Health Impact Project 2013; OBSSR 2013).
Overall, the findings of this study suggest that assessing cumulative risk without incorporating social determinants of health can underestimate a community’s risk, even in an environmental justice community. More locally refined data related to environmental and social sources of risk, as well as health outcomes and health status. Further, additional research on clearly defining boundaries of environmental justice communities is needed. Continued focus on environmental justice communities and the cumulative risks faced by their residents is critical to protecting these residents and, ultimately, moving towards a more equitable distribution and acceptable level of risk throughout society. With continued growth of industries associated with toxic emissions, as well as the development of new sources of products that potentially have even more toxic byproducts (such as the increased interest in refining bituminous sand for petroleum production), several fence line communities, and their surrounding neighbors, may be facing increased risk in the near future. Gaining broader understanding as to the sources and magnitude of this risk burden from environmental and social sources, as well as their interactions with each other, is essential to developing long-term effective solutions to the issues affecting these communities, and, ultimately, moving towards a more equitable distribution and acceptable level of risk throughout society.
Acknowledgments
The authors acknowledge Dr. Jonathon Ward for his initial insights into the work that led to the development of this manuscript. Also, special acknowledgement goes to Sayali Tarlekar for her valued assistance in helping develop this manuscript. The authors also acknowledge the thoughtful and constructive feedback from three anonymous journal reviewers in further strengthening this manuscript. Finally, we acknowledge the members of Community In-Power and Development Association (CIDA), Inc. for their sharing of valuable knowledge and insight about the West-Side neighborhood. This work was supported, in part, by National Institute on Minority Health and Health Disparities award 1RC2MD004783-01.
Footnotes
The Keystone XL Pipeline Project is a proposed 36-inch-diameter crude oil pipeline, beginning in Hardisty, Alberta, and extending south to Steele City, Nebraska, with ultimate connections to petrochemical refineries in the Midwest, as well as along the U.S. Gulf Coast. Along with transporting crude oil from Canada, the Keystone XL Pipeline will also support the significant growth of crude oil production in the United States from producers in the Bakken region of Montana and North Dakota. This pipeline will allow Canadian and American oil producers more access to the large refining markets found in the American Midwest and along the U.S. Gulf Coast.
SNAP: The Supplemental Nutrition Assistance Program. A U.S. federal government program that serves as a domestic safety net by providing financial and educational support to protect lower income Americans from hunger.
WIC: The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides additional U.S. federal government grants to U.S. states and territories for supplemental foods, health care referrals, and nutrition education specifically for low-income pregnant, breastfeeding, and non-breastfeeding postpartum women, and to infants and children up to age five who are found to be at nutritional risk.
AUTHORS’ DECLARATION STATEMENT
The authors declare that they have no conflicts of interest in the conduct and publication of this investigation.
References
- BoC (US Bureau of the Census) United States Census 2012 Web site. 2012a Available at http://2010.census.gov/2010census/
- BoC. American Community Survey. US Census Bureau Web site. 2012b Available at http://www.census.gov/acs/www/
- Callahan M, Sexton K. If cumulative risk assessment is the answer, what is the question? Environ Health Perspect. 2007;115(5):799–806. doi: 10.1289/ehp.9330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention) Establishing a Holistic Framework To Reduce Inequities In HIV, Viral Hepatitis, STDs, and Tuberculosis in the United States. 2010 Available at: http://www.cdc.gov/socialdeterminants.
- deFur PL, Evans GW, Cohen Hubal EA, et al. Vulnerability as a function of individual and group resources in cumulative risk assessment. Environ Health Perspect. 2007;115(5):817–24. doi: 10.1289/ehp.9332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EIA (US Energy Information Administration) 2012 Web site. Available at http://www.eia.gov/neic/rankings/refineries.htm.
- Ellick A. Tons of PCBs may come calling at a down-at-the-heels Texas City. The New York Times. 2008 Available at http://www.nytimes.com/2008/06/19/us/19PCB.html.
- ESRI. ArcGIS. Redlands, CA, USA: 2008. Version 9.3. [Google Scholar]
- Fiscella K, Williams DR. Health disparities based on socioeconomic inequalities: implications for urban health care. Academic Med. 2004;79(12):1139–47. doi: 10.1097/00001888-200412000-00004. [DOI] [PubMed] [Google Scholar]
- Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112(17):1645–50. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Toward Environmental Justice: Research, Education, and Health Policy Needs. National Academy Press; Washington, DC, USA: 1999. [PubMed] [Google Scholar]
- Linder SH, Sexton K. Conceptual models for cumulative risk assessment. Am J Public Health. 2011;101(1):S74–S81. doi: 10.2105/AJPH.2011.300318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linder SH, Marko D, Sexton K. Cumulative cancer risk from air pollution in Houston: disparities in risk burden and social disadvantage. Environ Sci Technol. 2008;42(12):4312–22. doi: 10.1021/es072042u. [DOI] [PubMed] [Google Scholar]
- Love JM, Harrison L, Sagi-Schwartz A, et al. Child care quality matters: how conclusions may vary with context. Child Dev. 2003;74(4):1021–33. doi: 10.1111/1467-8624.00584. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Lopez R. The riskscape and the color line: examining the role of segregation in environmental health disparities. Environ Res. 2006;102:181–96. doi: 10.1016/j.envres.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Shenassa ED. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ Health Perspect. 2006;114(8):1150–53. doi: 10.1289/ehp.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NEJAC (National Environmental Justice Advisory Council) Report submitted to the Office of Environmental Justice. US Environmental Protection Agency; Washington, DC, USA: 2004. Ensuring Risk Reduction in Communities with Multiple Stressors: Environmental Justice and Cumulative Risks/Impacts. [Google Scholar]
- NEJAC. Report submitted to the Office of Environmental Justice. US Environmental Protection Agency; Washington, DC, USA: 2010. Nationally Consistent Environmental Justice Screening Approaches. [Google Scholar]
- NRC (National Research Council) Science and Decisions: Advancing Risk Assessment. National Academies Press; Washington, DC, USA: 2009. [PubMed] [Google Scholar]
- OBSSR (Office of Behavioral and Social Sciences Research, National Institutes of Health) Systems Science. 2013 Available at http://obssr.od.nih.gov/scientific_areas/systems_science.
- Payne-Sturges DC, Gee GC. National environmental health measures for minority and low-income populations: tracking social disparities in environmental health. Environ Res. 2006;102:154–71. doi: 10.1016/j.envres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- Port Arthur Crude Expansion Project. Motiva Port Arthur Refinery Expansion Project Web site. 2012 Available at http://www.motivaexpansionproject.com/default.aspx.
- Port Arthur International Public Port Website. 2012 Available at http://www.portofportarthur.com/
- Riva M, Gauvin L, Barnett T. Toward the next generation of research into small area effects on health: a synthesis of multilevel investigations published since July 1998. J Epidemiol Community Health. 2007;61:853–61. doi: 10.1136/jech.2006.050740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- San Francisco Department of Health. Indicator Master List. Healthy Development Measurement Tool Web site. 2012 Available at http://www.thehdmt.org/master_list.php.
- Schulz A, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Ed Behavior. 2004;31(4):455–71. doi: 10.1177/1090198104265598. [DOI] [PubMed] [Google Scholar]
- Sexton K. Sociodemographic aspects of human susceptibility to toxic chemicals: do class and race matter for realistic risk assessment? Environ Toxicol Pharmacol. 1997;4:261–9. doi: 10.1016/s1382-6689(97)10020-5. [DOI] [PubMed] [Google Scholar]
- Sexton K, Linder SH. The role of cumulative risk assessment in decisions about environmental justice. Int J Environ Res Public Health. 2010;7(11):4037–49. doi: 10.3390/ijerph7114037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton K, Linder SH. Cumulative risk assessment for combined health effects from chemical and nonchemical stressors. Am J Public Health. 2011;101(1):S81–S88. doi: 10.2105/AJPH.2011.300118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soobader M, Cubbin C, Gee GC, et al. Levels of analysis for the study of environmental health disparities. Environ Res. 2006;102:172–80. doi: 10.1016/j.envres.2006.05.001. [DOI] [PubMed] [Google Scholar]
- StataCorp. STATA 9.2. College Station, TX, USA: 2007. [Google Scholar]
- Su JG, Morello-Frosch R, Jesdale BM, et al. An index for assessing demographic inequalities in cumulative environmental hazards with application to Los Angeles, California. Environ Sci Technol. 2009;43(20):7626–34. doi: 10.1021/es901041p. [DOI] [PubMed] [Google Scholar]
- Sundquist K, Theobald H, Yang M, et al. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006;62(8):2061–71. doi: 10.1016/j.socscimed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- Texas Alcoholic Beverage Commission. 2012 Web site. Available at http://www.tabc.state.tx.us/
- Texas Department of Family and Protective Services. 2012 Web site. Available at http://www.dfps.state.tx.us/Child_Care/Search_Texas_Child_Care/CCLNET/Source/CPA/ppSearchTXChildCare2.aspx.
- The Health Impact Project. About HIA. 2013 Available at http://www.healthimpactproject.org/hia.
- The Houston Chronicle. Unwanted imports: USEPA should delay PCB shipment plan. 2008 Available at http://www.chron.com/opinion/editorials/article/Unwanted-imports-USEPA-should-delay-PCB-shipment-1775559.php.
- The Pacific Institute. CSSJ brings community mapping workshops to Texas. 2011 Available at http://pacinst.org/publications/online_update/april_2011_online_update.htm#LETTER.BLOCK10.
- TransCanada. About the Project: The Keystone XL Pipeline. 2012 Available at http://http://keystone-xl.com/about/the-project/
- USDA (United States Department of Agriculture) 2011 Web site. Available at http://www.fns.usda.gov/fns/
- USEPA (US Environmental Protection Agency) 2005 National-Scale Air Toxics Assessment. US Environmental Protection Agency Web site. 2011 Available at http://www.epa.gov/nata2005/
- USEPA. Environmental Showcase Communities. 2012 Available at http://www.epa.gov/compliance/ej/grants/ej-showcase.html.
- USEPA. EPA updated National Air Toxics Assessment. 2012 Press Release. Available at http://yosemite.epa.gov/opa/admpress.nsf/d0cf6618525a9efb85257359003fb69d/64fcbc524c0f836c85257850004fe436!OpenDocument.
- Veolia Environmental Services. Port Arthur, TX, VEOLIA Environmental Services Web site. 2012 Available at http://www.veoliaes.com/en/locations/port-arthur.html.
- WHO (World Health Organization) Urban HEART: Urban Health Equity Assessment and Response Tool. WHO Center for Health Development; 2010. [Google Scholar]
- Wilkinson R, Marmot M. WHO Publications, Kobe, Japan. Social Determinants of Health: The Solid Facts. 2. World Health Organization; 2003. Available at http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf. [Google Scholar]